STRUCTURED ABSTRACT
Objectives
We aimed to determine the correlation between coronary artery calcium (CAC) scores on 3mm ECG-gated computed tomography (CT) scans and standard 6mm chest CT scans, and to compare relative strength of associations of CAC on each scan type with mortality risk.
Background
Coronary artery calcification predicts cardiovascular disease (CVD) and all-cause mortality, and is typically measured on ECG-gated 3mm CT scans. Patients undergo standard 6mm chest CTs for various clinical indications much more frequently, but CAC is not usually quantified. To better understand the usefulness of standard chest CTs to quantify CAC, we conducted a case-control study among persons who had both scan types.
Methods
Between 2000–03, 4,544 community-living individuals self- or physician-referred for “whole body” CT scans, had 3mm ECG-gated CTs and standard 6mm chest CTs, and were followed for mortality through 2009. In this nested case-control study, we identified 157 deaths and 494 controls frequency matched (1:3) on age and gender. The Agatston method quantified CAC on both scan types. Unconditional logistic regression determined associations with mortality, accounting for CVD risk factors.
Results
Participants were 68±11 years old and 63% male. The Spearman correlation of CAC scores between the two scan types was 0.93 (p<0.001); median CAC scores were lower on 6mm CTs compared to 3mm CTs (22 vs.104 Agatston units, p<0.001). Adjusted for traditional CVD risk factors, each SD higher CAC score on 6mm CTs was associated with 50% higher odds of death (OR=1.5; 1.2–1.9), similar to 50% higher odds on the 3mm ECG-gated CTs (OR=1.5, 1.1–1.9).
Conclusions
CAC scores on standard 6mm chest CTs are strongly correlated with 3mm ECG-gated CTs and similarly predict mortality in community-living individuals. Chest CTs performed for other clinical indications may provide an untapped resource to garner CVD risk information without additional radiation exposure or expense.
Keywords: Coronary artery calcium, Chest Computed Tomography, Mortality, Epidemiology
INTRODUCTION
Coronary artery disease (CAD) is the leading cause of mortality in the United States.(1) Detection of coronary artery calcification (CAC) is a strong predictor of CAD, cardiovascular events, and all-cause mortality,(2, 3) above and beyond the Framingham risk score.(2, 4) CAC is usually quantified on dedicated 3mm sliced computed tomography (CT) scans that are ECG gated, so as to minimize motion artifact from the beating heart and provide relatively fine cuts through the coronary arteries. These scans are done frequently in research settings, but uncommonly in clinical practice because most insurance providers do not cover the cost of the scan for preventive medicine and because the US Preventive Task Force currently does not recommend preventive CAC screening in individuals without a history of CAD.(5, 6) Standard chest CT scans are used for numerous clinical indications including lung cancer screenings, evaluation for pulmonary embolism, adenopathy, pleural diseases, and pneumonia, among others. Calcium within the coronary arteries can be easily recognized on these scans,(7) and prior studies have evaluated CAC on lung CTs for CAD screening in smokers at high risk for lung cancer.(8, 9) However, CAC screening may be most useful in persons at intermediate risk for CAD,(2) where presence and severity of CAC may modify the approach to preventive strategies such as use of statins and other interventions. In comparison to the approximate 600,000 3mm ECG-gated CT scans done in the US annually, it is estimated that over 7.1 million 6mm lung CT scans are done annually for other clinical indications.(10) While several studies have demonstrated agreement between 3mm ECG-gated CTs and standard chest CTs in their measurement of CAC (7, 9, 11), whether standard chest CTs can predict outcomes in the general population, and whether results are similar to 3mm EBCT scan data, despite the wider cuts and absence of ECG gating, is unknown.
To better understand the usefulness of standard chest CTs for this purpose, we conducted a case-control study among persons who had both scan types when they were seen in 2000–2003 and who were followed for mortality for approximately 8 years thereafter.
METHODS
Study Population and Study Design
Study participants were recruited through a San Diego cardiovascular imaging clinic between 2000 and 2003, where 4544 community-living individuals who were mostly asymptomatic were self-referred or referred by primary care physicians for “whole body” CT scans. Participants were followed for mortality through 2009, during which 173 participants died. Using a nested case-control study design, each death (case) was frequency matched on gender and age within 1 year with 3 surviving controls, resulting in 518 controls, and totaling 691 participants.(12) Following the selection of cases and matching controls, we further excluded any participant who had undergone any angioplasty, stent, or bypass revascularization procedure (n=41), which resulted in a total of 651 participants – 157 deaths and 494 controls. Five of the oldest cases did not have age matches within 1 year. Thus, controls for these five cases were within 3 to 5 years of the ages of these 5 cases. A 3mm ECG-gated CT was obtained and scored for CAC at the time of the initial visit. A 6mm standard chest CT was also obtained and read for general lung pathology, but was not scored for CAC at the time of the baseline visit. Our case-control design, nested within a prospective cohort study allowed us a targeted approach to retrieve chest CTs and re-read them for CAC without significant loss of statistical power. All participants provided informed consent and the study was approved by the University of California, San Diego Human Research Protections Program.
Coronary Artery Calcification Imaging and Scoring
CT scans were performed using an Imatron C-150 scanner (San Francisco, California), which is an electron-beam CT (EBCT) scanner with a high resolution detector system. We used the standard single-section mode, which involves an image acquisition time of 100msec and 3mm section thickness. The 3mm ECG-gated CT scans were electrocardiographically triggered at 40% or 65% of the [0-9]-[a-z] interval, depending on the participant’s heart rate, and resulted in 1.0 and 1.3 mSv of radiation for women and men, respectively.(13) For the 6mm chest CT scans, subjects were scanned from the sternal notch to base of the diaphragm without ECG gating. Radiation exposure for this type of scan, as presented in lung cancer screening literature for low-dose CT scan screening is approximately 1.5 mSv.(14) Methods for scoring CAC follow those described by Agatston et al. on both scan types. (15) The 3mm ECG-gated scans were read at the time of scan acquisition, while the 6mm scans were read for CAC in 2012. Readers were blinded to participant clinical data and to their 3mm CT CAC score.
Mortality
In 2009, we linked the data with the Social Security Death Index (SSDI) to identify individuals who had died in the intervening period. Potential deaths identified by the SSDI were cross-referenced with their patient clinical records to confirm identity.
Covariates
Height and weight were measured at clinic visits, and body mass index (BMI) was calculated (in kg/m2). Age and sex were obtained through self-report, and a questionnaire was used to obtain a participant’s medical history including smoking status (never, former, or current), prevalent hypertension, and cholesterol medication use. Non-fasting serum lipid and glucose levels were obtained via finger-stick using the Cholestec LDX system. Diabetes was defined as serum glucose > 200 mg/dL, or the use of glucose-lowering medications. Dyslipidemia was defined as total to high-density lipoprotein (HDL) cholesterol ratio > 5, or the use of cholesterol-lowering medication. Systolic and diastolic blood pressures were obtained from a trained technician after the participant rested for 5 minutes. Hypertension was defined as systolic blood pressure > 140 mmHg, diastolic blood pressure > 90 mmHg, or the use of anti-hypertensive medications.
Statistical Analysis
We evaluated differences in demographics and traditional CVD risk factors in cases and controls using t-tests or Wilcoxon Rank Sum tests for continuous variables and chi-square tests or Fisher’s exact tests for categorical variables. We evaluated the correlation of CAC scores on the two scan types using Spearman correlations for continuous CAC scores, given skewed distributions, and Kappa statistics for categorical CAC scores. We also performed a Bland-Altman analysis to determine the bias and limits of agreement between the 3mm ECG-gated CT and the 6mm standard chest CT scans.(16) Next, we used unconditional logistic regression to examine associations of each scan type with mortality. Initial models were unadjusted. Subsequent models adjusted for demographics and traditional CVD risk factors (age, gender, diabetes, hypertension, dyslipidemia, BMI, smoking, and family history of CVD). We evaluated each CAC score as both a continuous and categorical variable. For analysis using a continuous CAC score, we added 1 to each CAC score (such that zero scores were not excluded from the analysis) and natural log transformed the distribution (Ln[CAC +1]) to approximate a normal distribution of CAC scores. We used standardized coefficients to compare strength of association per standard deviation of LnCAC+1 across the two scan types. For analysis using a categorical CAC score, we categorized patients into 4 groups according to standard 3mm Agatston CAC score cut-points, which facilitated comparisons across scan types.(17)
In evaluating the 6mm Agatston scores, 34% had Agatston scores of zero, whereas 24% had scores of zero using the 3mm CT scans. Using standard cut-points proposed by Detrano and colleagues, we defined 4 categories of CAC for both 3mm ECG-gated and 6mm chest CT scans: CAC=0, CAC=1–100, CAC=101–300, and CAC>300.(17) All analyses were conducted using Stata version 11.0SE (Stata Corp., College Station, TX) and SAS version 9.4 (SAS Corp, Cary, NC), and p-values < 0.05 were considered statistically significant.
RESULTS
The 651 participants in this study had mean age of 68 years, and 63% were male. Cases and controls had similar BMI, total cholesterol, HDL cholesterol, and use of lipid lowering medications. However, a greater proportion of cases had diabetes and hypertension, were former or current smokers, and had a family history of CVD. Cases also had higher median CAC scores on both the 3mm CT and 6mm CT scans compared to controls at baseline (Table 1). Race/ethnicity was not required to obtain a CT scan, thus it was provided by 199 individuals in this study. Of these 199 individuals with reported ethnicity, 100% (43) of deaths occurred in Caucasians. This subsample of 199 included 0.6% Asian, 12% Hispanic and 2% Other – the remaining 85% were Caucasian.
Table 1.
Participant Characteristics by Case-Control Status
| Characteristics | Case | Controls | P-value |
|---|---|---|---|
| (n=157) | (n=495) | ||
|
|
|||
| Age, years | 67.74 ± 11.71 | 67.84 ± 10.76 | 0.92 |
| Body Mass Index | 26.68 ± 4.66 | 26.84 ± 4.22 | 0.70 |
| Total Cholesterol | 203.5 ± 42.51 | 201.9 ± 40.03 | 0.67 |
| HDL Cholesterol | 52.45 ± 17.92 | 51.79 ± 16.90 | 0.70 |
| Female | 67 (43%) | 186 (38%) | 0.26 |
| Diabetes | 13 (8%) | 16 (3%) | 0.01 |
| Hypertension | 64 (41%) | 188 (38%) | 0.53 |
| Lipid Medication Use | 9 (6%) | 38 (8%) | 0.41 |
| Smoking Status | |||
| Never Smoked | 70 (45%) | 269 (54%) | 0.03 |
| Former Smoker | 67 (43%) | 195 (39%) | 0.47 |
| Current Smoker | 20 (13%) | 32 (6%) | 0.01 |
| CVD Family History | 43 (27%) | 87 (18%) | 0.01 |
| 3mm EBCT CAC Score (Median; 25th, 75th Percentile) | 210 (14, 608) | 84 (0, 484) | 0.01 |
| 6mm Chest CT CAC Score (Median; 25th, 75th Percentile) | 55 (0, 230) | 15 (0, 146) | 0.00 |
Used Wilcoxon-Rank Sum Test to determine differences between cases and controls.
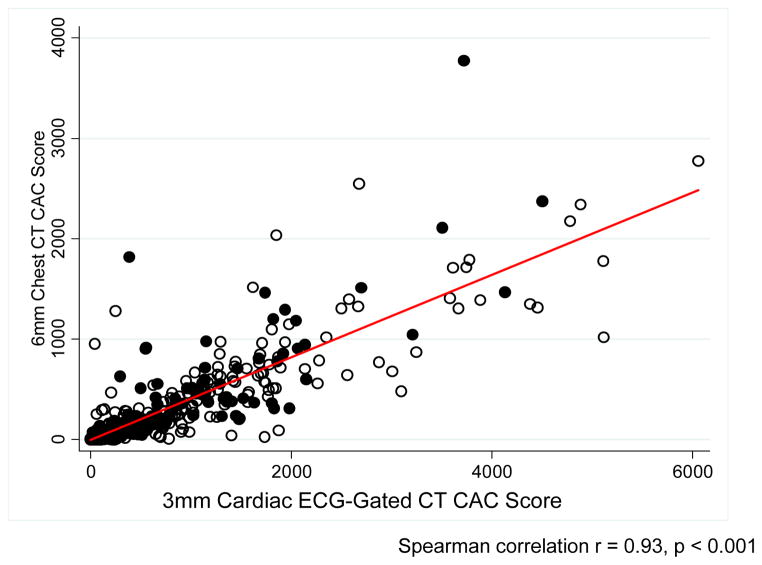
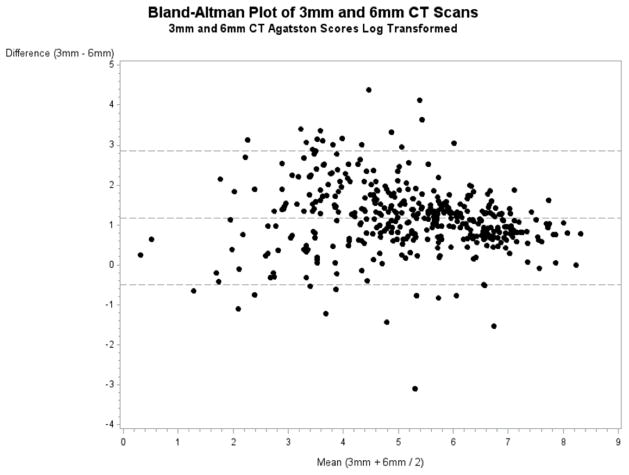
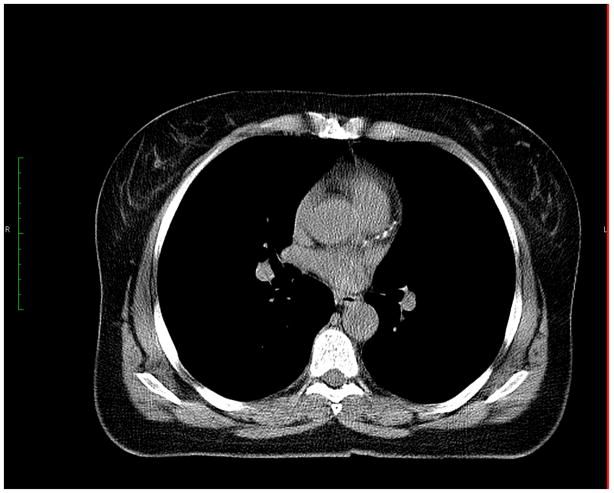
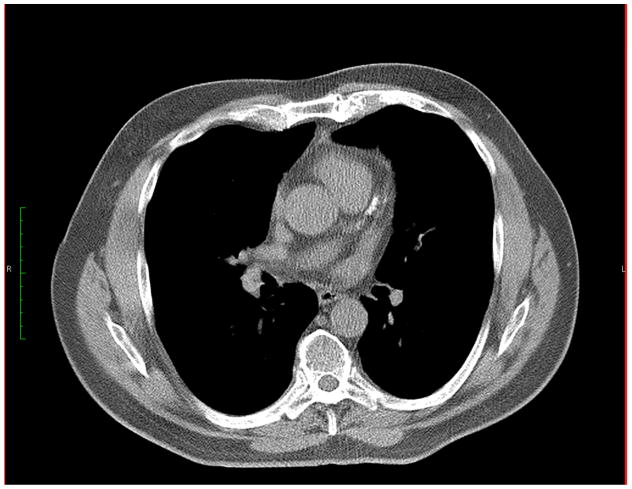
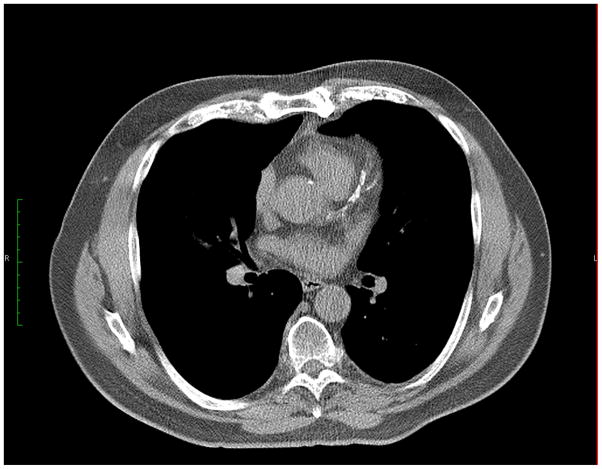
The correlation between CAC scores on the 3mm ECG-gated CT and the 6mm standard chest CT was 0.93 (p < 0.001; Figure 1). However, the median CAC scores were significantly lower on the 6mm CT scan than on the 3mm ECG-gated scan (22 vs. 104 Agatston units, respectively, p < 0.001). The Kappa statistic for agreement between CAC score categories on the 3mm ECG- gated CT compared to the 6mm standard chest CT was 0.41, and the weighted Kappa statistic was 0.62, indicating moderate to substantial agreement between the two scans using the cut-points specific to the 3mm ECG- gated CT scans. Bland-Altman analysis presents a mean bias of 3.23, with limits of agreement between 0.6 and 17.3, as shown in Figure 2, suggesting that Agatston scores on 3mm ECG- gated CT scans were, on average, approximately 323% higher than Agatston scores on the 6mm standard chest CT scan.(16) As illustrative examples of the difference in sensitivity, Figure 3 presents CAC measured on 3mm ECG-gated CT (CAC=372.09) and 6mm chest CT (CAC=116.58) at approximately the same location within an individual. In a participant with more advanced CAC, Figure 4 presents 2 consecutive slices within the same individual where CAC measured on 3mm ECG-gated CT totaled to 3212.75 and CAC measured on 6mm chest CT totaled to 1044.00. Both examples demonstrate that, while CAC is present and quantifiable on both the 3mm and 6mm scans, the clarity and amount of CAC scored by the Agatston method is higher using a 3mm ECG-gated CT scan.
Figure 1. Scatter Plot Agatston CAC Score on 6mm Chest CT and 3mm Cardiac ECG-Gated CT Scans.
Spearman Correlation r = 0.93, p < 0.001
● = Cases (n=157)
○ = Controls (n=494)
Figure 2. Bland-Altman Plots for Agreement Between 3mm ECG-Gated CT Scans and 6mm Standard Chest CT Scans.
*Log transformed mean bias (center line) was 1.17 (±0.855), which back transforms to 3.23, with limits of agreement ranging from 0.6 to 17.3 (top and bottom dashed lines).
Figure 3. Illustrative Example of the Difference in Sensitivity between 3mm ECG-Gated CT Scans and 6mm Chest CT Scans in a Single Slice within an Individual.
A. 3mm ECG-gated CT (Agatston CAC Score = 372.09)
B. 6mm Chest CT (Agatston CAC Score = 116.58)
Figure 4. Illustrative Example of the Difference in Sensitivity between 3mm ECG-Gated CT Scans and 6mm Chest CT Scans in Two Consecutive Slices within an Individual.
A.1, A.2 Two consecutive slices from 3mm ECG-gated CT within an individual (Agatston CAC Score = 3212.75)
B.1, B.2 Two consecutive slices from 6mm Chest CT within an individual (Agatston CAC Score = 1044.00)
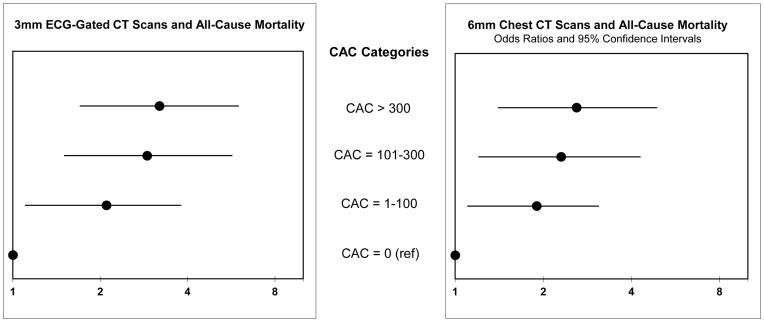
Table 2 shows the associations of CAC scores on the two scan types with mortality. When evaluating CAC on the 6mm chest CT scans, compared to the CAC=0 reference, there was a graded relationship of higher CAC score with odds of mortality such that those with CAC scores between 1 and 100 had 1.9-fold higher odds of mortality, between 101 and 300 had 2.3 fold higher odds of mortality, and those with CAC greater than 300 had 2.6-fold higher odds for mortality in models adjusted for demographics and traditional CVD risk factors. In comparison, with the 3mm ECG-gated scans, compared to the CAC=0 reference, participants with CAC scores between 1 and 100 had 2.1-fold higher odds of mortality, between 101 and 300 had 2.9-fold higher odds of mortality, and those greater than 300 had 3.2-fold higher odds of mortality in adjusted models. These associations have been plotted in Figure 5. When CAC scores were evaluated as a continuous variable, each SD higher CAC score on the 6mm chest CTs was associated with 1.5-fold higher odds of mortality. Similarly, each SD higher score on the 3mm ECG-gated scans was associated with 1.5-fold higher odds of mortality. All of these results were statistically significant.
Table 2.
Association of 6mm Standard Chest CT vs. 3mm ECG-Gated EBCT CAC scores with All-Cause Mortality
| 6mm Non-Gated Chest CT | |||||
|
| |||||
| Agatston Score Range | < 1.0 | 1–100 | 101–300 | > 300 | Continuous Model Per SD Ln [CAC +1] |
| # Deaths/# Controls | 41/192 | 53/152 | 29/70 | 34/80 | |
| Unadjusted OR (95% CI) | 1.00 (Ref) | 1.6 (1.0, 2.6) | 1.9 (1.1, 3.4) | 2.0 (1.2, 3.4) | 1.3 (1.1, 1.6) |
| p-value | 0.037 | 0.018 | 0.01 | 0.002 | |
| Adjusted* OR (95% CI) | 1.00 (Ref) | 1.9 (1.1, 3.1) | 2.3 (1.2, 4.3) | 2.6 (1.4, 4.9) | 1.5 (1.2, 1.9) |
| p-value | 0.017 | 0.009 | 0.004 | 0.001 | |
|
| |||||
| 3mm ECG-Gated EBCT | |||||
|
| |||||
| Agatston Score Range | <1.0 | 1–100 | 101–300 | >300 | Continuous Model Per SD Ln [CAC +1] |
| # Deaths/# Controls | 26/139 | 35/120 | 31/77 | 65/158 | |
| Unadjusted OR (95% CI) | 1.00 (Ref) | 1.6 (0.9, 2.7) | 2.2 (1.2, 3.9) | 2.2 (1.3, 3.7) | 1.3 (1.1, 1.6) |
| p-value | 0.122 | 0.011 | 0.002 | 0.005 | |
| Adjusted* OR (95% CI) | 1.00 (Ref) | 2.1 (1.1, 3.8) | 2.9 (1.5, 5.7) | 3.2 (1.7, 6.0) | 1.5 (1.1, 1.9) |
| p-value | 0.022 | 0.002 | 0.000 | 0.002 | |
Adjusted for age, sex, diabetes, hypertension, hyperlipidemia, BMI, smoking, and family history of CVD.
Figure 5. Forest Plots of Odds Ratios and 95% Confidence Intervals for the Associations between 3mm ECG-Gated CT Scans and Mortality and 6mm Chest CT Scans and Mortality.
*Adjusted for age, sex, diabetes, hypertension, hyperlipidemia, BMI, smoking, and family history of CVD
DISCUSSION
In this population of free-living individuals who self-referred or were referred by their primary care physicians for “whole body” CT scans, CAC scores on standard 6mm chest CTs were strongly correlated to those on the 3mm ECG-gated CT scans specifically designed for CAC measurement. Scores on either scan type were strongly associated with all-cause mortality, and the relative strength of association was similar irrespective of the scan type.
CAC screening has been considered useful for prevention of CVD because it can further risk-stratify persons who are considered intermediate risk for incident CVD events by the Framingham risk score. Several investigators have reported that standard chest CT scans used for lung cancer screening can also detect and quantify CAC.(3, 4, 9, 11, 18, 19) Our study confirms these results, and extends them to a community-living population for the first time. Moreover, to our knowledge, this is the first study to compare the correlation and relative strengths of association of CAC on the standard chest CT and the 3mm ECG-gated CT with mortality.
Our results may have important implications for preventive cardiology clinical practice. In 2007, approximately 7.1 million chest CT scans were performed in the US, compared to 600,000 CT scans for calcium scoring, presumably using 3mm ECG-gated CTs.(10) There is concern that radiation exposure from CT scans may increase cancer risk.(20, 21) In addition, many health insurance plans do not cover the expense of CT scanning for CAC measurement for preventive care purposes. Given that chest CTs are done frequently for numerous other clinical indications, many individuals may already have scans that can be scored for CAC, which may guide preventive cardiology care. Thus, if our results are confirmed, health care providers may consider utilizing previously obtained CT scans to assess CAC while avoiding the potential risks and expense of repeat CT scans designed specifically for CAC measurement.
Currently, CAC observed on standard chest CT scans is not routinely reported by radiologists, and use of the Agatston method is even less common. For example, Williams et al. reported that CAC on chest CTs was recorded in the final radiology report in only 44% of patients with known CAC.(22) Jacobs and colleagues demonstrated that, by using simple visual grading to measure CAC on standard chest CT, CAC was strongly associated with future CVD events.(23) Thus, by simple visual grading system evaluated by others,(23, 24) or by the Agatston method used here, the detection of CAC on standard chest CT has prognostic implications. As it has important implications for preventive care, we believe it should be systematically reported.
The median CAC scores on the 6mm CT scans were substantially lower on average than on the 3mm CT scans. This may be because there are fewer slices to evaluate and score on the 6mm scan. With fewer slices, there may also be volume averaging in plaque based on interpolation algorithms from slice to slice. Also, small plaques may be missed between 6mm cuts. Therefore, 6mm chest CT scans may be less sensitive for low levels of CAC, and the good prognosis provided by a 3mm ECG-gated scan showing zero CAC may not be as robust for a 6mm chest CT with zero CAC. Absence of any CAC on an ECG-gated 3mm scan has been associated with low risk for incident CVD, and relatively standard CAC cut-points (for example, 0–100; 101–300; and > 300) have been used frequently in prior studies. In this study, we have extended these cut-points to 6mm standard chest CT scans, which were similarly associated with mortality risk, but the implication of a specific CAC score may differ across scan types. For example the median 6mm standard chest CT scan CAC scores were 3, 46, and 286 in individuals in the 3mm CT scan CAC categories of 1–100, 101–300, and >300, respectively. Establishing applicable cut-points for Agatston CAC scores on 6mm standard chest CT scans warrant further development. However, our data suggest that lower CAC scores on 6mm chest CT scans may underestimate the CAC burden compared to 3mm ECG-gated CT scores.
This study has important limitations. Our study population was mostly older non-Hispanic white adults, many of whom self-referred for “whole body” CT scans for preventive care. Such individuals may be particularly motivated to prevent chronic diseases. Future studies in other settings are required to confirm these findings. As discussed previously, although the associations of either scan type with mortality were similar, there are absolute differences in the CAC scores across scan types, which may impact sensitivity to detect low level CAC and will influence specific cut-points. Thus, specific CAC values should be interpreted with knowledge about the scan type.
In conclusion, despite the absence of ECG gating and wider slice thickness, CAC scores on standard 6mm chest CTs are highly correlated with those on 3mm ECG-gated CT scans, and are similarly associated with mortality risk in community-living individuals. Most insurance providers do not routinely cover the expense of 3mm ECG-gated scans for CAC scoring, and conversely approximately 7 million chest CT scans are done annually in the US for other clinical indications.(10) Persons who have chest CTs for other clinical indications may benefit from systematic reading of CAC to garner additional information on CVD risk without the added expense and radiation exposure required for dedicated 3mm ECG-gated scans.
Clinical Perspectives.
Competency in Medical Knowledge
Standard chest CT scans are often not read for CAC severity by radiologists when reading scans obtained for other clinical indications. We show that detection of CAC on standard chest CT scans is closely correlated with CAC on the ECG-gated CT scans, and similarly predicts mortality. Therefore, chest CT scans obtained for various clinical indications can also inform CVD risk through measurement of CAC.
Translational Outlook
While similarly predictive of events, a CAC score on a standard chest CT was lower than on an ECG-gated CT on the same individual. Future studies are required to determine applicable cut-points for CAC scores on standard CT scans relative to the ECG-gated CT.
Acknowledgments
FUNDING SOURCES: Funding for this project comes from National Institutes of Health, National Heart, Lung, and Blood Institute R01HL116395, American Heart Association Established Investigator Award EIA18560026, American Heart Association Fellow to Faculty Award 0475029N, and K23DK091521.
The authors would like to thank the participants of this study, the clinic staff who received and examined these participants, and Julie Denenberg for her assistance and organization.
ABBREVIATIONS
- CAD
Coronary Artery Disease
- CAC
Coronary Artery Calcium
- CT
Computed Tomography
- ECG
Electrocardiogram/Electrocardiography
- EBCT
Electron Beam Computed Tomography
- CVD
Cardiovascular Disease
- HDL
High Density Lipoprotein
- SD
Standard Deviation
Footnotes
DISCLOSURES: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jan M. Hughes-Austin, Email: jhughesaustin@ucsd.edu.
Arturo Dominguez, III, Email: a4dominguez@ucsd.edu.
Matthew A. Allison, Email: mallison@ucsd.edu.
Christina L. Wassel, Email: cwassel@pitt.edu.
Dena E. Rifkin, Email: drifkin@ucsd.edu.
Cindy G. Morgan, Email: cindymorgansd@gmail.com.
Michael R. Daniels, Email: mrdaniels@ucsd.edu.
Umaira Ikram, Email: ikramumaira@hotmail.com.
Jessica B. Knox, Email: jbknox@ucsd.edu.
C. Michael Wright, Email: cmichael.wright@gmail.com.
Michael H. Criqui, Email: mcriqui@ucsd.edu.
Joachim H. Ix, Email: joix@ucsd.edu.
References
- 1.Thomas KL, Honeycutt E, Shaw LK, Peterson ED. Racial differences in long-term survival among patients with coronary artery disease. Am Heart J. 2010 Oct;160(4):744–51. doi: 10.1016/j.ahj.2010.06.014. Comparative Study Research Support, Non-U.S. Gov’t. [DOI] [PubMed] [Google Scholar]
- 2.Polonsky TS, McClelland RL, Jorgensen NW, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. Jama. 2010 Apr 28;303(16):1610–6. doi: 10.1001/jama.2010.461. Research Support, N.I.H., Extramural. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shemesh J, Henschke CI, Shaham D, et al. Ordinal scoring of coronary artery calcifications on low-dose CT scans of the chest is predictive of death from cardiovascular disease. Radiology. 2010 Nov;257(2):541–8. doi: 10.1148/radiol.10100383. Research Support, Non-U.S. Gov’t. [DOI] [PubMed] [Google Scholar]
- 4.Shaw LJ, Raggi P, Callister TQ, Berman DS. Prognostic value of coronary artery calcium screening in asymptomatic smokers and non-smokers. Eur Heart J. 2006 Apr;27(8):968–75. doi: 10.1093/eurheartj/ehi750. [DOI] [PubMed] [Google Scholar]
- 5.O’Malley PG, Greenberg BA, Taylor AJ. Cost-effectiveness of using electron beam computed tomography to identify patients at risk for clinical coronary artery disease. Am Heart J. 2004 Jul;148(1):106–13. doi: 10.1016/j.ahj.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 6.Force USPST. Final Recommendation Statement: Coronary Heart Disease: Screening Using Non-Traditional Risk Factors. 2014 Available from: http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/coronary-heart-disease-screening-using-non-traditional-risk-factors.
- 7.Kirsch J, Buitrago I, Mohammed TL, Gao T, Asher CR, Novaro GM. Detection of coronary calcium during standard chest computed tomography correlates with multi-detector computed tomography coronary artery calcium score. Int J Cardiovasc Imaging. 2012 Jun;28(5):1249–56. doi: 10.1007/s10554-011-9928-9. Comparative Study. [DOI] [PubMed] [Google Scholar]
- 8.Jacobs PC, Gondrie MJ, van der Graaf Y, et al. Coronary artery calcium can predict all-cause mortality and cardiovascular events on low-dose CT screening for lung cancer. AJR Am J Roentgenol. 2012 Mar;198(3):505–11. doi: 10.2214/AJR.10.5577. Multicenter Study Randomized Controlled Trial Research Support, Non-U.S. Gov’t. [DOI] [PubMed] [Google Scholar]
- 9.Takx RA, de Jong PA, Leiner T, et al. Automated coronary artery calcification scoring in non-gated chest CT: agreement and reliability. PLoS One. 2014;9(3):e91239. doi: 10.1371/journal.pone.0091239. Research Support, Non-U.S. Gov’t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berrington de Gonzalez A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009 Dec 14;169(22):2071–7. doi: 10.1001/archinternmed.2009.440. Research Support, Non-U.S. Gov’t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim YK, Sung YM, Cho SH, Park YN, Choi HY. Reliability analysis of visual ranking of coronary artery calcification on low-dose CT of the thorax for lung cancer screening: comparison with ECG-gated calcium scoring CT. Int J Cardiovasc Imaging. 2014 Dec;30(Suppl 2):81–7. doi: 10.1007/s10554-014-0507-8. [DOI] [PubMed] [Google Scholar]
- 12.Rothman K, Greenland S. Modern Epidemiology. 2. Philadephia: Lippincott-Raven Publishers; 1998. Matching; pp. 147–61. [Google Scholar]
- 13.Hunold P, Vogt FM, Schmermund A, et al. Radiation exposure during cardiac CT: effective doses at multi-detector row CT and electron-beam CT. Radiology. 2003 Jan;226(1):145–52. doi: 10.1148/radiol.2261011365. Comparative Study. [DOI] [PubMed] [Google Scholar]
- 14.Aberle DR, Berg CD, Black WC, et al. The National Lung Screening Trial: overview and study design. Radiology. 2011 Jan;258(1):243–53. doi: 10.1148/radiol.10091808. Multicenter Study Randomized Controlled Trial Research Support, N.I.H., Extramural. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990 Mar 15;15(4):827–32. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 16.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999 Jun;8(2):135–60. doi: 10.1177/096228029900800204. Review. [DOI] [PubMed] [Google Scholar]
- 17.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008 Mar 27;358(13):1336–45. doi: 10.1056/NEJMoa072100. Research Support, N.I.H., Extramural. [DOI] [PubMed] [Google Scholar]
- 18.Wu MT, Yang P, Huang YL, et al. Coronary arterial calcification on low-dose ungated MDCT for lung cancer screening: concordance study with dedicated cardiac CT. AJR Am J Roentgenol. 2008 Apr;190(4):923–8. doi: 10.2214/AJR.07.2974. Research Support, Non-U.S. Gov’t. [DOI] [PubMed] [Google Scholar]
- 19.Arcadi T, Maffei E, Sverzellati N, et al. Coronary artery calcium score on low-dose computed tomography for lung cancer screening. World J Radiol. 2014 Jun 28;6(6):381–7. doi: 10.4329/wjr.v6.i6.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brenner DJ. Radiation risks potentially associated with low-dose CT screening of adult smokers for lung cancer. Radiology. 2004 May;231(2):440–5. doi: 10.1148/radiol.2312030880. Research Support, U.S. Gov’t, Non-P.H.S. [DOI] [PubMed] [Google Scholar]
- 21.Linet MS, Slovis TL, Miller DL, et al. Cancer risks associated with external radiation from diagnostic imaging procedures. CA Cancer J Clin. 2012 Feb 3; doi: 10.3322/caac.21132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams KA, Sr, Kim JT, Holohan KM. Frequency of unrecognized, unreported, or underreported coronary artery and cardiovascular calcification on noncardiac chest CT. J Cardiovasc Comput Tomogr. 2013 May-Jun;7(3):167–72. doi: 10.1016/j.jcct.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 23.Jacobs PC, Gondrie MJ, Mali WP, et al. Unrequested information from routine diagnostic chest CT predicts future cardiovascular events. Eur Radiol. 2011 Aug;21(8):1577–85. doi: 10.1007/s00330-011-2112-8. Multicenter Study Research Support, Non-U.S. Gov’t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blair KJ, Allison MA, Morgan C, et al. Comparison of ordinal versus Agatston coronary calcification scoring for cardiovascular disease mortality in community-living individuals. Int J Cardiovasc Imaging. 2014 Apr;30(4):813–8. doi: 10.1007/s10554-014-0392-1. Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t. [DOI] [PMC free article] [PubMed] [Google Scholar]