Abstract
Background
Orofacial clefts (OFCs) are common birth defects that may impose a large burden on the health and psychosocioeconomic well-being of affected individuals and families. The current study aims to identify qualitative factors that affect the quality of life (QOL) of family caregivers of children with OFCs.
Methods
A mixed method study in which family caregivers of OFCs children were consecutively recruited from cleft clinics over a 3-month period. Quantitative data was analyzed using SPSS version 17 and FGD by framework analysis.
Results
A total of 107 caregivers participated in the entire study and 24 caregivers participated in the focus group discussions. About 50% of the children had cleft lip and palate (CLP), 28% with cleft lips only (CL) and 23.4% with cleft palate only (CP). Poor access to specific information and lack of empathy of professionals affected the quality of life and delivery of family centered care.
Conclusions
To improve the quality of life of family caregivers, individual focused counseling sessions should be organized for caregivers soon after birth. This will provide an opportunity to discuss laid out plans for supportive care. It will also as an avenue to address arising social issues by health professionals and counselors.
Keywords: Orofacial clefts, Quality of life, Focus Group discussion, Nigeria
Background
Orofacial defects (OFCs) commonly known as clefts are common birth defects that may impose a large burden on the health, quality of life (QOL), psychosocial and socioeconomic well-being of affected individuals, families and the society (Wehby and Cassell, 2010; Zahid and Ohaeri, 2010). There are about 170,000 children born with cleft lips or palate every year (Smile Train, 2012). OFCs are known to result in structural and functional limitations affecting speech, hearing, and mastication early in life (Covinsky et al.,1994; Nackashi et al., 2002; Kramer et al., 2009). OFCs have a significant impact on the QOL of affected individuals and can cause substantial morbidity risks which may also reduce quality of life throughout the life span (Locker et al., 2005; Broder et al., 2012). Morbidity risks can be profound in less developed settings where early systematic paediatric care may not be commonly accessible (Wehby and Cassell, 2010). Several of the effects of OFCs are said to extend through adulthood resulting in increased mortality and morbidity. This may then result in significant healthcare use and costs for the individual, family and caregiver (Christensen et al., 2004; Wehby and Cassell, 2010).
The effect of diseases and complex traits like OFCs and the course of treatment on the family play an important role in a child's adaptation. Sometimes several members of the family take care of the dependent relative, but it is more common for the burden of care to be carried by a single person i.e. the main caregiver (Bendo et al., 2012). This care affects the caregiver significantly in physical, mental, social and economic aspects. It produces an overload of tasks that usually changes the functional dynamics of the family (Alexih et al., 2002; Glozman, 2004).
The functioning and well-being of the family caregivers depend on the child's situation (Ylven et al., 2006; Rodríguez-Sánchez et al., 2011; Northouse et al., 2012).
QOL is rapidly becoming a model for measuring outcomes in clinical trials, cost effectiveness analysis and clinical practice (Becker et al., 2000). It is a worldwide health indicator that provides information on the physical, psychological and social dimensions of an individual’s life which are not captured in the clinical instruments (Glozman, 2004; Haberstroh et al, 2010). QOL of parents of chronically ill children is now very important as the mortality rates decrease and survival rates increase (Epstein et al., 2005). It is important for health care professionals to be aware of these changes and for them to have effective tools to assess the impact of these demands on the caregivers (Yaffe et al., 2002). However, little is known about the QOL of caregivers of children with clefts in developing countries such as Nigeria. In order to provide responsive and adequate support to caregivers and to improve the outcomes of children with orofacial clefts, the current study aims to identify qualitative factors that affect the QOL of family caregivers.
Methods
Study sites
Ethical approval for this study was obtained from the Health Research and Ethics Committee of the Lagos University Teaching Hospital (IRB number ADM/DCST/HREC/887). Written informed consent was obtained from each respondent on each questionnaire indicating their willingness to participate in the study. There were no names printed on the questionnaires and the respondents were assured of the confidential nature of the study.
This study was carried out at the cleft clinics of the three public tertiary health institutions located in Lagos State. The hospitals are: the Lagos University Teaching Hospital (LUTH), the Lagos State University Teaching Hospital (LASUTH) and the National Orthopaedic Hospital, Igbobi (NOHI). These hospitals were chosen to allow for a relatively wide catchment area in order to accommodate patients from the different geographical zones of Lagos state. All three hospitals offer free surgical management of OFCs sponsored the Smile Train- a US based Non-governmental Organization. The cleft clinics in these tertiary hospitals are run by consultants who are trained and certified on the same standard protocols for management of clefts. Only respondents who were family caregivers of orofacial cleft children (OFC), related to the participating child and had been residing with the family prior to the birth of the participating child were included. In addition, only a family caregiver who directly cared for the participating child most part of each day for a minimum of four weeks prior to the study period was included. We excluded family caregivers of children with orofacial clefts who had any other birth defects, chronic conditions or other abnormalities. Family caregivers of children less than one month of age or more than five years (60 months) of age were also excluded from this study.
Data collection
Data was obtained using quantitative tools adapted from the work of Stein and Jessop, 2003 to assess the quality of life of family caregivers. The questionnaire has five sections (i.e. A to E). Section A was socio-demographic details of the caregiver and index child, section B obtained information on the clinical history of child, section C obtained history on social support during care, section D was the Impact on Family Scale (IOFS) (Stein and Jessop, 2003) which was applied to measure the subjectively perceived quality of life in affected families. The IOFS is related to five dimensions which are (1) Financial impacts (assesses changes in the financial status of the family, (2) Social relationships (the disruption of social interaction, (3) Personal impacts (assesses the psychological burden experienced by the primary caregiver; (4) Coping strategies or mastery as employed by the family (5) Impact on siblings (assesses the quality of interaction within the family unit). We excluded impact on siblings from the final analysis because not all children had siblings and those who did were of varying numbers. The questionnaire was translated and back translated in Yoruba by staff of the Department of linguistics at the Obafemi Awolowo University, Ife, Osun State.
The qualitative tool was adapted from focus group discussion (FGD) guide previously described by Blitz-Lindeque (2006). The FGD was conducted at a place and time chosen as convenient by the participants. The family caregivers had been approached during the process of interviewing them for the questionnaires. This was done personally by the principal investigator of the study (TA). The mode of discussions was explained to all caregivers approached and possible interview venues were suggested to them. The caregivers who consented were chosen based on their similar family size (less than four children) and depending on the type of cleft the index child had. This was done to increase homogeneity within each group.
Focus Group Discussion
Three focus group discussions were carried out with the family caregivers. First session was conducted for family caregivers of children with cleft lip, second for family caregivers of children with cleft palate and the third for family caregivers of children with both cleft lip and palate. The sessions for each group consisted of eight participants selected during the study period. Two of those invited for the discussion declined because they were going to be indisposed on the date of the interview. Thus, we had 22 respondents in total for the FGD. Ikeja (the Lagos Sate Capital) was chosen since it was a central location for the discussants. Some of them had to come from Badagry, Epe and Ikorodu towns in Lagos. The outdoor hallway from the cleft clinical area in LASUTH, Ikeja was the meeting place for the interviews. Monday and Wednesday were chosen for the interviews since none of the participating hospitals including LASUTH have clinics on those days which are relatively quiet and peaceful.
The first two groups of discussants came on Monday at separate times of the day. The family caregivers of children with CL had a discussion in the morning from 10am and the family caregivers of children with CP had the afternoon session from 1pm. The third group of family caregivers of children with CLP had their FGD on Wednesday morning from 11am. All the participants were sent text messages (sms) 5 days prior to the date as reminders for the focus group discussions. They were also called individually 2 days before the dates. The participants were seated in a circle with the principal investigator of the study (TW) and a research assistant who recorded the responses. The FGD was tape recorded and the research assistant wrote down the verbal responses and noted non-verbal actions or sounds made by the discussants. Each session lasted for about one hour and they were entertained with light refreshments afterwards.
Data entry and analysis
Quantitative data was entered into Microsoft excel and the Statistical Package for Social sciences (SPSS) version 17 was used for data analysis. The socio-demographic, socioeconomic and medical factors were presented in the form of frequency tables. Analysis of the qualitative data was conducted using framework analysis as described by Rabiee (2004).
Results
Quantitative data
A total of 107 caregivers of OFC children participated in the quantitative part of the study. Almost 50% of the children had CLP, 28% with CL and 23.4% with CP. A large proportion (82.2%) of the diagnosis of the cleft was made at delivery with just 6.5% diagnosed prenatally. A total of 11.2% of the diagnosis of cleft was made during neonatal period and infancy. Majority of caregivers (95.3%) had no known positive family history of clefts up to their second generation of parents.
About 66.4% of respondents named the doctor and 16.8% named the nurse as the main source of care-giving information. Others got their information from co-caregivers (9.3%) and via the internet (7.5%). Most of the OFC caregivers (93.5%) did not have any healthcare worker home visit to assist with care and about 38% of respondents had no family support. In 31.8% of respondents, family support was from the index child’s aunt/uncle (), grandparents (25.2%) and from an older sibling (4.7%) (Table 1).
Table 1.
Caregiving support for OFC family caregivers
| Freq n=107 | (%) | |
|---|---|---|
| Most helpful source of care giving information reported | ||
| Doctor | 71 | 66.4 |
| Nurse | 18 | 16.8 |
| Co-caregiver | 10 | 9.3 |
| Internet | 8 | 7.5 |
| Home visits by healthcare worker | ||
| Yes | 7 | 6.5 |
| No | 100 | 93.5 |
| Person who gave significant family support (relative to child) | ||
| None | 41 | 38.3 |
| Grand Parent | 27 | 25.2 |
| Aunt / Uncle | 34 | 31.8 |
| Sibling | 5 | 4.7 |
| Caregivers satisfaction with professionals support | ||
| Yes | 103 | 96.3 |
| No | 4 | 3.7 |
| Caregivers satisfaction with Family support | ||
| Yes | 64 | 59.8 |
| No | 43 | 40.2 |
The socio-demographic characteristics of respondents showed that most of the respondents were between 25–34 years of age and 63.6% had a mean age of 31.1±5.5 years. Majority (92.5%) of the respondents were mothers of the children (Table 2).
Table 2.
Socio-demographic and socio-economic characteristics of respondents
| OFC caregivers n=107 Freq |
% | |
|---|---|---|
| Age (years) | ||
| 15 – 24 | 10 | 9.3 |
| 25 – 34 | 68 | 63.6 |
| 35 – 44 | 29 | 27.1 |
| Mean ± SD | ||
| Sex | ||
| Male | 6 | 5.6 |
| Female | 101 | 94.4 |
| Marital Status | ||
| Married | 99 | 92.5 |
| Unmarried/separated | 8 | 7.5 |
| Relationship to child | ||
| Father | 6 | 5.6 |
| Mother | 99 | 92.6 |
| Others | 2 | 1.8 |
| Ethnicity | ||
| Yoruba | 58 | 54.2 |
| Igbo | 43 | 40.2 |
| Hausa | 3 | 2.8 |
| Others | 3 | 2.8 |
| Religion | ||
| Christianity | 76 | 71.0 |
| Islam | 31 | 29.0 |
| Education | ||
| None | 6 | 5.6 |
| Primary | 15 | 14.0 |
| Secondary | 48 | 44.9 |
| Tertiary | 38 | 35.5 |
| Income/month | ||
| (naira) | 9 | 8.4 |
| Above 100,000 | 20 | 18.7 |
| 50,000 – 99,999 | 37 | 34.6 |
| 20,000 – 49,999 | 41 | 38.3 |
| Below 20,000 | ||
| Occupation | 3 | 2.8 |
| Snr. Professionals | 13 | 12.1 |
| Intmd. Professionals | 42 | 39.3 |
| Skilled | 28 | 26.2 |
| Semiskilled | 21 | 19.6 |
| Unskilled |
The financial dimension was positively correlated to the social dimension (0.521) and personal dimension (0.330) (Table 3). The social impact was positively correlated to the personal impact (0.527). The social impact had a strong negative correlation with the coping impact (−2.92) (Table 3). All these correlation coefficients in the matrix were statistically significant (p<0.05). The personal impact was also positively correlated with the social impact (0.527) with statistical significance (p<0.05) (Table 3).
Table 3.
Correlation matrix between the dimensions of the quality of life score among respondents
| Quality of Life (No. of items) |
Financial | Social | Personal | Coping |
|---|---|---|---|---|
| Financial- (4) | 1 | 0.521* | 0.330* | 0.03 |
| Social (15) | 0.521 | 1 | 0.527* | −2.92* |
| Personal- (5) | 0.330* | 0.527* | 1 | −0.073 |
| Coping- (3) | 0.03 | −0.292* | −0.073 | 1 |
p value <0.05
There were statistically significant positive correlations between correlation coefficients of the following dimensions: financial (0.696), social (0.909) and personal (0.693 with the QOL total scores (Table 4). The coping dimension was weakly correlated with the QOL score and not statistically significant.
Table 4.
Correlation between quality of life score and the dimensions among respondents
p value <0.05
r = Pearson’s correlation coefficient
The social impact score was inversely correlated with the duration of breast feeding (−0.190) and the period in time when the cleft was diagnosed (Table 5). These correlation coefficients were statistically significant. The other dimensions had weak positive and negative correlations with the factors of duration of breastfeeding, age of child and period in which the cleft was diagnosed (Table 5).
Table 5.
Correlation between quality of life score and characteristics of respondents
| Duration child breastfed | Age of child | Time cleft diagnosed | |
|---|---|---|---|
| Quality of Life (No of Items) | |||
| Financial Impact (4) | 0.049 | 0.013 | −0.010 |
| Social impact (15) | −0.190** | 0.004 | −0.203* |
| Personal Impact (5) | −0.025 | −0.026 | −0.074 |
| Coping Impact (3) | 0.030 | −0.025 | −0.022 |
p-value <0.05
p-value <0.01
Qualitative Data
Three focus group discussions (FGD) were carried out with caregivers of children with clefts i.e. CP, CL and CLP. The findings from the focus group discussion are highlighted in four categories i.e. reaction to birth of a cleft child, information about care process and service delivery, challenges of caregiving and coping mechanisms and five subcategories which are: access to information, experience of service delivery toward family centered care, financial challenges, social challenges and emotional challenges (Figure 1).
Figure 1.
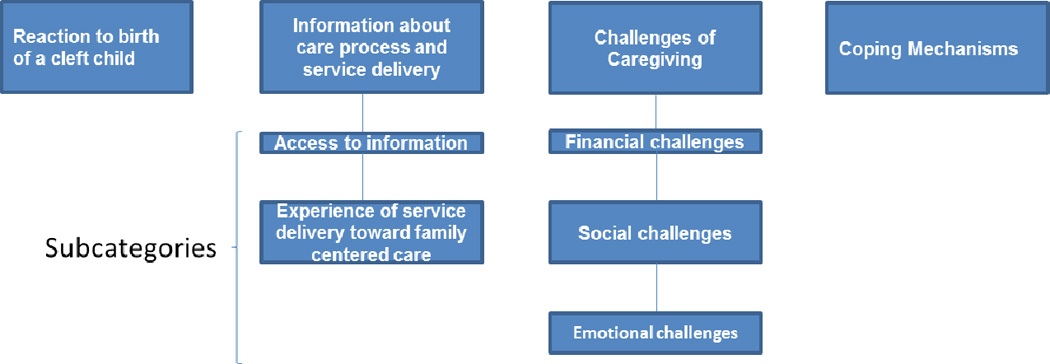
Showing findings from the Focus Group Discussions (FGD) highlighted in four categories and five subcategories.
Reaction to birth of a cleft child
The discussants gave expressions such as ‘shock’, ‘sad’ … when they first set eyes on their newborn. Some were even afraid and used a Yoruba word ‘abami’ which means “alien” to describe the baby. The second discussants in the CP focus discussion group and fifth discussant in the CL focus discussion group were more aware of occurrence of clefts and thus had less severe reactions.
“I screamed when I first saw my baby. I later accused the nurse that she switched the baby with another woman’s baby and I was just shouting and crying on and on….wondering why this happened to me” - discussant four from the CLP group.
“As a pharmacist, I had heard of cleft, so when the doctor told me he had a cleft palate. I was sad and tears just flowed as I sobbed ” – discussant two from the CP group.
Discussant eight of CL group reported mixed feelings toward the baby; she was happy to have a baby alive as it was her first child after three years of miscarriages but also with feelings of ‘despair’ that the baby had a birth defect. “I wasn’t really prepared for my first live child to have a problem. I felt he was ugly but he was still my baby…….nothing else was wrong apart from the split lip”- discussant eight from the CL group.
Information about care process and service delivery
Access to information
Most of the discussants said they were informed by the doctors of the baby’s birth defect, who simply said “it was a minor thing and could be repaired”. Discussant five of CP group said “the doctor didn’t even tell me what to do to care for her or that we will be coming to the hospital every week”. Discussants one and six from the CLP group and discussant three of CL group made similar statements. Discussant seven from the CP group said “breastfeeding was a problem and no information on how to go about it was given”.
“The Doctor didn’t tell me my baby would choke on milk and it would come out of his nose. I was afraid when this happened. I didn’t know how to breastfeed and my baby was losing weight very fast. I complained at the health center but they said I should keep trying. Four weeks after his birth, a friend told me to try and cut open the bottle “teat” - Discussant seven from the CP
Discussants three from the CP, two and eight from the CLP made similar statements to affirm poor access to adequate and correct information which made caring for the baby difficult.
Experience of service delivery toward family centered care
Poor access to services was highlighted especially in the rural areas. Also, the health workers were reported not to show empathy most times and this increased the emotional strain. Most respondents said no health worker or social worker visited them to improve home care. Two discussants i.e. discussant three from the CP and discussant five from the CLP said “they were visited at home by a health worker from a non-governmental organization”. The hospital processes were said to be “tiresome and complex”.
“The nurse on duty sent me with a referral letter and no information. I cried all the way to the hospital carrying my baby in the four hour journey. I got there and the first words the nurse I met said was to come back the next week, clinic had closed. I was very sad” - Discussant one from the CLP group.
“My husband and I have been coming here and they haven’t told us when the surgery will be and how much it will cost. We don’t know how many times this baby will enter theatre and if she will be normal after. “We were just asked to go for several laboratory tests and coming back to the clinic” - Discussant five from the CL group.
Most were however happy at the outcome of repair. They desired more access to information especially earlier at birth, more support groups and possibly help lines.
“I knew I didn’t have a perfect baby, I hoped the doctors knew what they were doing and now that it is healing, I’m happy; I can live my life now”- Discussant six from the CP group.
Challenges of Caregiving
Several hidden challenges were discussed by the participants mostly relating to finances, social and emotional aspects.
Financial challenges
‘I spend 1,500 naira ($7.50) to come for appointment and go home every week and I’m not selling market three months now since I delivered…… ” - Discussant four in the CL group.
‘I have to buy two cans of food (infant formula) every week because this baby cannot suck breast. It is too expensive…..’ - Discussant one from the CLP group.
Social challenges
“We have to leave home at 5am and travel every week from Epe to Ikeja (117km) for hospital checkup just because of this one child. The other children are suffering because of this child‘’ - Discussant four from the CL group.
‘’My life is just about hospital and taking care of this baby since she was born. I don’t have time to visit my friends like I used to and I don’t even want them to come and visit me, so they don’t see her until the surgery is done..” - Discussant eight from the CLP group.
Emotional challenges
“I am very ashamed; I can’t take him out till the repair is done. My mother-in-law said he is a bastard and I should throw him away. My neighbor’s always whisper when they see me, they keep finding reasons to come into my house and greet our baby. My husband only understands and comforts me, but it has not been easy”- Discussant six from the CLP group.
Coping Mechanisms
Most were still adjusting to the family acceptance of the child. They had to stop working and could not attend social functions even for those that mattered to them.
Discussant three from the CLP group said ‘I avoided my family even during my sister’s wedding. I kept telling them I was on my way then made up excuses later ….….. I can’t let them see my child like this’.
Discussant two from the CL group spoke of hiding her child in fear of the stigma. Six other discussants from the CL group and five discussants from the CLP asserted the same with affirmative phrases like ‘yes o’, ‘eeh hen’, ‘it’s true’ while nodding their heads.
Some statements made included:
‘Covering the baby’s face and head while I’m backing him has helped me to go out occasionally. I tell them he is sleeping…’ - Discussant five from the CLP group.
“We couldn’t do any naming ceremony for this baby, I just gave her a name at the hospital during clinic file registration” - Discussant seven from the CL group.
Discussion
The quality of life of children with orofacial clefts is a priority in current research. However, it is now imperative to consider the quality of life of caregivers. It is also essential to strengthen caregivers with a resultant effect of good health outcomes for the affected child and family as a whole in the spirit of true rehabilitation. In the current study, we examined the factors associated with QOL of family caregivers of children with OFC in Nigeria. The factors associated with a good quality of life for family caregivers were exclusive breastfeeding and an increased duration of breastfeeding. The type of cleft was a significant factor associated with the quality of life of OFC caregivers. Income, exclusive breastfeeding and professional support were found to be significant predictors for a better quality of life too. The family functioning was also found to be a significant predictor of better quality of life.
Those with higher family functioning scores had lower impact scores. Other studies have also shown a significant positive relationship between quality of life and the family functioning found for both the global score and the four dimensions of quality of life (Juniper et al., 1996; Alecxih et al., 2002; Lierde and Dhaeseleer, 2002). Family functioning was also found to be inversely related to the social impact and the coping impact and this was also statistically significant. This was also reported by a similar study where social support was the dimension least influenced by family functioning (Prahbhjot and Pratibha; 2005). The social impact was inversely correlated to the duration of breastfeeding and found to be the most significant predictor of the quality of life score.
Breastfeeding has been shown to be a factor that also positively influences the wellbeing of mothers (Kramer et al., 2007). Women who were breastfeeding reported significantly better physical health, more hours of sleep, lesser rates of depression and more energy when compared with those who mixed fed or formula fed their babies (Kramer et al., 2007; Kathleen et al., 2011). Children with OFCs struggle to create intraoral pressure in order to suck directly from the breast (Ibrahim et al., 2008). In the current study, a number of women reported difficulty breastfeeding their babies and were provided little or no information on how to go about breast feeding. This will lead to undue stress coupled with the shock of having a child with OFCs and inevitably affect the coping mechanisms of these women and their QOL.
A variety of services can help support family and other informal caregivers. Supportive services that are designed to support caregivers include information and assistance services, technology, education and training, support groups and counseling, respite care, and financial support. The current healthcare set-up in Nigeria and indeed most developing countries makes this a difficult task. There is great emphasis on meeting the surgical needs of the affected child and little is done to support other services such as speech, dental and psychosocial support. Furthermore, there are no existing structures to support the family caregivers since there is an overwhelming need to support the affected child. The limited available financial resource is a contributing factor too. Currently, surgical support to cleft families is funded by non-governmental organizations in Nigeria and most part of Africa. Nonetheless, there are advocacy groups and women organizations in Nigeria that can be trained to support cleft families. The current situation where health workers are expected to provide surgical and other ancillary support is not sustainable. From our FDG, it is obvious that there is a need for trained family advocacy groups to support families. These groups should liaise with the healthcare providers in order to obtain all the necessary information and training.
During the long trips to the hospital, there was an additional financial commitment towards transportation and lack of care for the other children in the family. Furthermore, family dynamics have been reported to be affected due to disagreements, conflicts and even violence among members (Fadden et al., 1987). Some family members or relatives leave to avoid taking care of the patient. We observed similar trends in some of the families we interviewed; where most caregivers had negative experiences and feelings of stigmatization from close relatives and within their community. Poor access to specific information tailored to meet the needs of each caregiver and lack of empathy of professionals were some additional barriers observed in this study. A situation where families visited the hospital without knowing the treatment plan or cost is not encouraging, considering the emotional state of families with OFCs.
The limitations of this study include the limited number of individuals available for the study, the fact that this sample may not be representative of Nigeria since it was only conducted in Lagos. Furthermore, the experiences of these families may be limited to developing countries only and not reflective of similar families in developed countries. There is also the possibility of other respondents agreeing with what was said as a limitation of the current study. Nonetheless, this study focuses on the plight of caregivers in developing countries which may have an impact on cleft children and outcomes.
To improve the quality of life of family care givers, individual focused counseling sessions should be organized for caregivers soon after birth. This will provide valuable opportunities for the professionals to discuss laid out plans for supportive care. It will also serve as an avenue to address arising social issues by health professionals and counselors. Family advocacy groups should be trained to provide support services to clefts families since there are limited social services and resources for counselling. In the absence of these levels of support, the quality of life of family caregivers may negatively affect the outcomes for children with OFCs in Nigeria and other developing countries.
Acknowledgement
We are particularly grateful to all the families that participated voluntarily in this research, the research assistant that helped with the focused group discussions and staff of the Lagos University Teaching Hospital, Lagos State University Teaching Hospital and the National Orthopaedic Hospital, Igbobi. We are also grateful to Paul Casella for editing the manuscript. This project was supported by NIDCR K99/R00 DE022378 (AB), Robert Wood Johnson Foundation (AB) Grant number 72429 and Lagos University Teaching Hospital Fellowship Training Funds (TA).
Footnotes
List of abbreviations
CL, CLP, CP, FGD, LASUTH, LUTH, NOHI and QOL
Conflict of Interest:
Authors declare that there are no conflicts of interest.
Author’s contribution
TA, AB and WLA conceived and designed the project. ATO and BO supervised TA to conduct the project; TA conducted the data collection and FGD. TA, KL and AB wrote the manuscript. All authors critically revised the manuscript.
REFERENCES
- 1.Alecxih L, Zeruld S, Olearczyk B. National Family Caregiver Support Program: Selected Issue briefs. Washington DC: US Department of health and human services, Administration on aging; 2002. Characteristics of caregivers based on the survey of income and program participation. [Google Scholar]
- 2.Becker MA, Shaw BR, Reib LM. Quality of Life Assessment Manual. Madison, WI: University of Wisconsin– Madison, Quality of Life Assessment Team; 2000. Available online: http://www.fmhi.usf.edu/institute/pubs/pdf/mhlp/qol.pdf. [Google Scholar]
- 3.Bendo CB, Paiva SM, Viegas CM, Vale MP, Varni JW. The PedsQLTM Oral Health Scale: Feasibility, reliability and validity of the Brazilian Portuguese version. Health and quality of life outcomes. 2012;42 doi: 10.1186/1477-7525-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berger ZE, Dalton LJ. Coping With a Cleft: Psychosocial Adjustment of Adolescents With a Cleft Lip and Palate and Their Parents. Cleft Palate-Craniofacial Journal. 2009;46:435–443. doi: 10.1597/08-093.1. [DOI] [PubMed] [Google Scholar]
- 5.Blitz-Lindeque J. How to assess family function. South African Family Practice Manual. (2nd ed.) 2006:384–385. [Google Scholar]
- 6.Broder HL, Wilson-Genderson M, Sischo L. Health disparities among children with cleft. Am J Public Health. 2012;102:828–830. doi: 10.2105/AJPH.2012.300654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christensen K, Juel K, Herskind AM, Murray JC. Long term follow up study of survival associated with cleft lip and palate at birth. BMJ. 2004;328:1405–1408. doi: 10.1136/bmj.38106.559120.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Covinsky KE, Goldman L, Cook EF. The impact of serious illness on patients’ families. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of Treatment. JAMA. 1994;272:1839–1844. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- 9.Epstein I, Stinson J, Stevens B. The effects of camp on health related quality of life in children with chronic illness: A review of the literature. Journal of Pediatric Oncology Nursing. 2005;22:89–103. doi: 10.1177/1043454204273881. [DOI] [PubMed] [Google Scholar]
- 10.Fadden G, Bebbington P, Kuipers L. The burden of care: The impact of funtional psychiatric illness on the patient's family. Br J Psychiatr. 1987;150:285–292. doi: 10.1192/bjp.150.3.285. [DOI] [PubMed] [Google Scholar]
- 11.Glozman J. Quality of life of caregivers. Neuropsychology review. 2004;14:183–197. doi: 10.1007/s11065-004-8158-5. [DOI] [PubMed] [Google Scholar]
- 12.Haberstroh J, Hampel H, Pantel J. Optimal management of Alzheimer's disease patients: Clinical guidelines and family advice. Neuropsychiatr Dis Treat. 2010;6:243–253. doi: 10.2147/ndt.s7106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ibrahim A, Ijekeye FO, Asuku ME. Tessier cleft numbers 7 and 30: case report and literature review. Nigerian Journal of Plastic Surgery. 2008;4:52–57. [Google Scholar]
- 14.Johansson B, Ringsberg KC. Parents’ experiences of having a child with cleft lip and palate. Journal of Advanced Nursing. 2004;47:165–173. doi: 10.1111/j.1365-2648.2004.03075.x. [DOI] [PubMed] [Google Scholar]
- 15.Kendall-Tackett K, Cong Z, Hale TW. The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. Clinical Lactation. 2011;(2–2):22–26. 2011. [Google Scholar]
- 16.Kramer FJ, Baethge C, Sinikovic B, Schliephake H. An analysis of quality of life in 130 families having small children with cleft lip/palate using the impact on family scale. International Journal of Oral and Maxillofacial Surgery. 2007;36:1146–1152. doi: 10.1016/j.ijom.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 17.Kramer FJ, Gruber R, Fialka F, Sinikovic B, Hahn W, Schliephake H. Quality of life in school-age children with Orofacial Clefts and their families. Journal of Craniofacial Surgery. 2009;20:2061–2066. doi: 10.1097/SCS.0b013e3181be8892. [DOI] [PubMed] [Google Scholar]
- 18.Locker D, Jokovic A, Tompson B. Health-related quality of life of children aged 11 to 14 years with orofacial conditions. Cleft Palate Craniofac J. 2005 May;42(3):260–266. doi: 10.1597/03-077.1. [DOI] [PubMed] [Google Scholar]
- 19.Nackashi JA, Dedlow RE, Dixon-Wood V. Cleft lip and palate from origin to treatment. NY: Oxford University Press; 2002. Health care for children with cleft lip and palate: comprehensive services, and infant feeding; pp. 127–158. [Google Scholar]
- 20.Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients: meta-analysis of randomized trials. Cancer J Clin. 2010;60:317–339. doi: 10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rabiee F. Focus-group interview and data analysis. Proceedings of the Nutrition Society. 2004;63:655–660. doi: 10.1079/pns2004399. [DOI] [PubMed] [Google Scholar]
- 22.Rodríguez-Sánchez E, Pérez-Peñaranda A, Losada-Baltar A, Pérez-Arechaederra D, Gómez-Marcos M, Patino-Alonso M, et al. Relationships between quality of life and family function in caregiver. BMC Family Practice. 2011;12:1–7. doi: 10.1186/1471-2296-12-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smile Train. Changing the world one smile at a time. [Accessed July 2012]; Available at http://www.smiletrain.org. [Google Scholar]
- 24.Wehby G, Cassell C. The impact of orofacial clefts on quality of life and health care use and cost. Oral Dis. 2010;16:3–10. doi: 10.1111/j.1601-0825.2009.01588.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ylvén R, Björck-Åkesson E, Granlund M. Literature review of positive functioning in families with children with a disability. Journal of policy and practice in intellectual disabilities. 2006;3:253–270. [Google Scholar]
- 26.Zahid MA, Ohaeri JU. Relationship of family caregiver burden with quality of care and psychopathology in a sample of Arab subjects with schizophrenia. BMC Psychiatry. 2010;10:71–75. doi: 10.1186/1471-244X-10-71. [DOI] [PMC free article] [PubMed] [Google Scholar]


