Abstract
Management of pediatric epilepsy requires complex coordination of care. We hypothesized that an improved seizure management care plan would reduce healthcare utilization and improve outcomes. We conducted a cohort study with historical controls of 120 epilepsy patients before and after implementation of a “Seizure Action Plan.” We evaluated for differences in healthcare utilization including emergency department visits, hospitalizations, clinic visits, telephone calls, and the percentage of emergency department visits that resulted in hospitalization in patients who did or did not have a Seizure Action Plan. We found that there was no decrease in these measures of healthcare utilization, and in fact the number of follow-up clinic visits was increased in the group with Seizure Action Plans (4.2 versus 3.3, p 0.006). However, the study was underpowered to detect smaller differences. Our study suggests that pediatric epilepsy quality improvement measures may require alternative approaches to reduce healthcare utilization and improve outcomes.
Keywords: Epilepsy, quality improvement, hospitalizations
INTRODUCTION
Management of a child presenting with seizures is a complex process involving medical, social, and educational components. The process involves acute medical care, education of the family about medications, instructions for what to do if there is a seizure, implementation of potentially complicated medication regimens, and instructions for follow-up. Families are often worried and upset when their child is admitted to the hospital, and education and instructions for treatment may not always be correctly understood. Management of epilepsy and other chronic conditions falls heavily on the patient/family and their ability to adhere to medication regimens and understand their disease, including the need to understand potentially complicated plans in case of breakthrough seizures.1 However, physicians may have unrealistic expectations that patients and families have adequate ability and resources to assume responsibility for management of their disease.2
Improved care for pediatric epilepsy patients, even in the absence of novel therapies, offers a potential for improving health outcomes and reducing healthcare utilization. Unexpected readmissions for seizures are the fourth most common reason for readmissions at children’s hospitals.3 Increased education of patients and families has been shown to improve understanding of epilepsy and appropriate anti-epileptic medication use.4 Certain strategies such as pre-hospital use of intranasal midazolam for a prolonged breakthrough seizure, have been demonstrated to reduce hospital admissions.5
Recent Cochrane reviews on patients with chronic medical conditions have concluded that patient/family-centered education programs can lead to improvements in ratings of health and symptoms, with reductions in hospital admissions.6, 7 For patients with epilepsy, studies have shown that educational programs significantly improved self-management behaviors.8 However, there are contrary examples; for example, use of Asthma Action Plans did not decrease frequency of ED visits and hospitalizations.9
These findings led us to consider whether a detailed plan for children with epilepsy and their families might reduce health care utilization. We hypothesized that a written “Seizure Action Plan” (SAP) would minimize confusion about when to seek healthcare for seizures; reduce emergency department visits; and reduce in-patient admissions for seizure exacerbations. The SAP would include a list of current anti-epileptic medications and their dosages, instructions for use of rescue medications when necessary, instructions for break-through seizures, and a specific follow-up plan. Our goal was to provide families and patients with clear instructions that would be readily available to them. We studied whether implementation of SAPs was associated with a change in the number of emergency department visits and subsequent admissions for seizures, and decreased need for families to contact us with questions.
METHODS
This study was approved by the Institutional Review Boards for the University of Utah and for Primary Children’s Hospital. We performed a cohort study with historical controls of patients with seizures before and after implementation of a seizure action plan (SAP). The study was performed at Primary Children’s Hospital (PCH), which provides primary pediatric care for the urban Wasatch Front region, and is also the sole tertiary children’s hospital within a 5 state catchment area for patients from Utah, Wyoming, Idaho, Nevada and Montana. Patients were identified from the Electronic Data Warehouse (EDW) maintained by PCH and Intermountain Healthcare, using a computerized search of International Classification of Disease, 9th Edition, Clinical Modification (ICD-9-CM, referred to subsequently as ICD-9) diagnosis codes, and confirmed by manual chart review. A total of 120 patients were analyzed; 60 consecutive patients prior to implementation of the SAP from January 1, 2007 through December 31, 2008; and 60 consecutive patients after implementation of the SAP from January 1, 2010 through December 31, 2011. Each patient was followed for outcomes for 18 months after the index presentation. There was no overlap of patients in the SAP and no SAP groups.
Patients were included in the study if they were admitted to PCH with a seizure during the study time period; and had a discharge diagnosis of seizure or epilepsy (ICD-9 345.xx or 780.xx). Diagnosis was also confirmed at the time of chart review. The timeframe dates for controls (no SAP, “nSAP”) group was 1/2007–12/2008; and was 1/2010–12/2011 for the SAP group. Patients were excluded from the study for febrile seizures, seizures provoked by illness or trauma, non-epileptogenic seizures, patients admitted electively for video EEG monitoring, patients with epilepsy admitted for diagnostic evaluation solely, and patients who underwent epilepsy surgery during the study period.
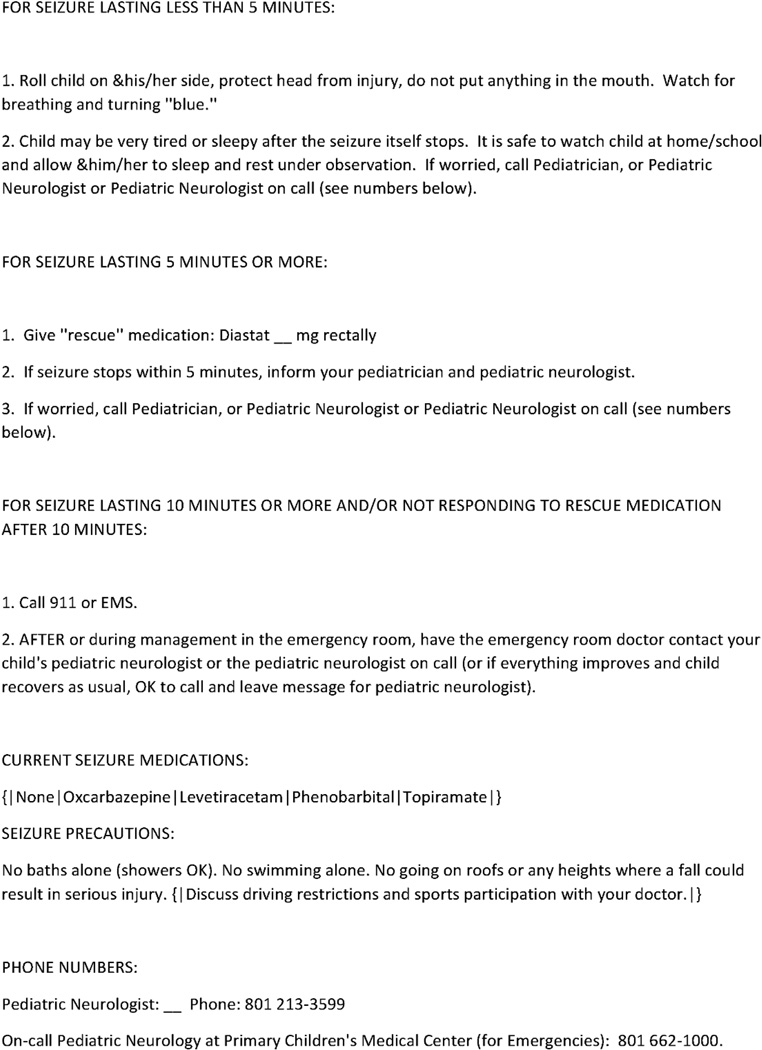
The SAP was designed to provide families and patients with information that might be forgotten or difficult to remember, and that would be helpful in a situation of breakthrough seizures or for determining timing of follow-up (Figure 1). The template for the SAP, which included name and date of birth, was automatically generated by the electronic medical record system, and patient-specific details were filled out by the clinician. SAPs were discussed either one-on-one with a family, or sometimes in a larger group of medical personnel, at the time of discharge. SAP introduction to families was not scripted; and discussion of SAPs at follow-up clinic visits was left to the discretion of the individual clinician. For the analyses included in this manuscript only SAPs used for hospitalized patients were included. SAPs for patients who presented initially in the outpatient setting were not included in order to maintain a potentially less heterogenous population for analysis. Discussion about the SAP in follow-up was left to the discretion of the clinician.
FIGURE 1.
A sample Seizure Action Plan to be provided to a patient/family upon discharge from the hospital.
Data collected included demographic data including age, gender, ethnicity, and diagnosis; and outcomes data including the number of emergency department (ED) visits, number of hospitalizations for seizures, number of pediatric neurology follow-up clinic visits, number of phone calls to the pediatric neurology offices which was recorded as the number of “Message Logs” entered into the electronic medical record (message logs are the nurse-entered record of phone calls), length of index hospitalization and number of anti-epileptic drugs (AEDs) at discharge. Outcomes data were collected for each patient for the 18-month period following the index admission. Data was managed using REDCap (Research Electronic Data Capture) hosted at the University of Utah.10
Statistical Analysis
De-identified patient data was entered into the REDCap database, including demographic information, number of AEDs, number of emergency department visits, number of neurology clinic follow-up visits, number of phone calls to the pediatric neurology offices, and number of hospitalizations for seizures. Comparison was made of outcomes from patients who did not receive a SAP, to patients who did receive one. Descriptive statistics were used to characterize the study cohort. The two-proportion z-test was used to calculate p-values of demographic data. Wilcoxon Rank-Sum tests were used to compare outcomes; p values were two-sided. We used SAS University Edition (SAS Institute, Inc., Cary, NC) for analyses.
RESULTS
The total study cohort of 120 patients included 60 control patients from 2007–2008, prior to seizure action plan (SAP) implementation (the no seizure action plan group, “nSAP”), and 60 patients from 2010–2011, after SAP implementation (“SAP” group) (Table 1). In the SAP cohort there were more males (p 0.029) and a higher percentage of children who were on 4 or more AEDs (p 0.028). Otherwise demographics of the two cohorts were similar, including age, ethnicity, length of hospitalization, and discharge diagnosis.
TABLE 1.
Patient characteristics and demographics. nSAP = prior to implementation of Seizure Action Plan (2007–2008); SAP = after implementation of Seizure Action Plan (2010–2011). N=60 for each group. First number listed is absolute number followed by percentage (out of 60) in parentheses. Highlighted values indicate those that are statistically significant. “Discharge Diagnosis” is based on the primary ICD-9 code used. AED, anti-epileptic drug.
| Characteristic | nSAP (%) | SAP (%) | p value |
|---|---|---|---|
| Age (years) | |||
| 0–2 | 17 (28%) | 16 (26%) | 0.84 |
| 3–18 | 43 (72%) | 44 (74%) | |
| Gender (male) | 25 (42%) | 37 (62%) | 0.029 |
| Race/Ethnicity | |||
| Non-Hispanic White | 38 (63%) | 47 (78%) | 0.25* |
| Non-Hispanic Black | 0 (0%) | 0 (0%) | |
| Hispanic/Latino | 8 (13%) | 7 (12%) | |
| Asian | 1 (2%) | 0 (0%) | |
| Pacific Islander | 2 (3%) | 1 (2%) | |
| Middle Eastern | 0 (0%) | 1 (2%) | |
| Other/Unknown | 11 (18%) | 4 (7%) | |
| Insurance (Medicaid) | 21 (36%) | 18 (30%) | 0.70 |
| Hospital Length of Stay (days) | 0.67** | ||
| 0–1 | 21 (35%) | 19 (32%) | |
| 2–3 | 24 (40%) | 25 (42%) | |
| 4–6 | 9 (15%) | 13 (22%) | |
| >7 | 6 (10%) | 3 (5%) | |
| Discharge Diagnosis (from initial hospitalization) | 0.28^ | ||
| Intractable Epilepsy | 25 (42%) | 30 (50%) | |
| Grand Mal Status | 19 (32%) | 21 (35%) | |
| Other Convulsions | 16 (27%) | 9 (15%) | |
| Number of AEDs at Discharge | 0^^ | ||
| 0 | 5 (8%) | 3 (5%) | |
| 1 | 25 (42%) | 22 (37%) | |
| 2 | 20 (33%) | 16 (27%) | |
| 3 | 9 (15%) | 12 (20%) | |
| 4 or more | 1 (2%) | 7 (12%) |
7×2 chi-square test.
Wilcoxon signed-rank test.
3×2 chi-square test.
7×2 chi-square test.
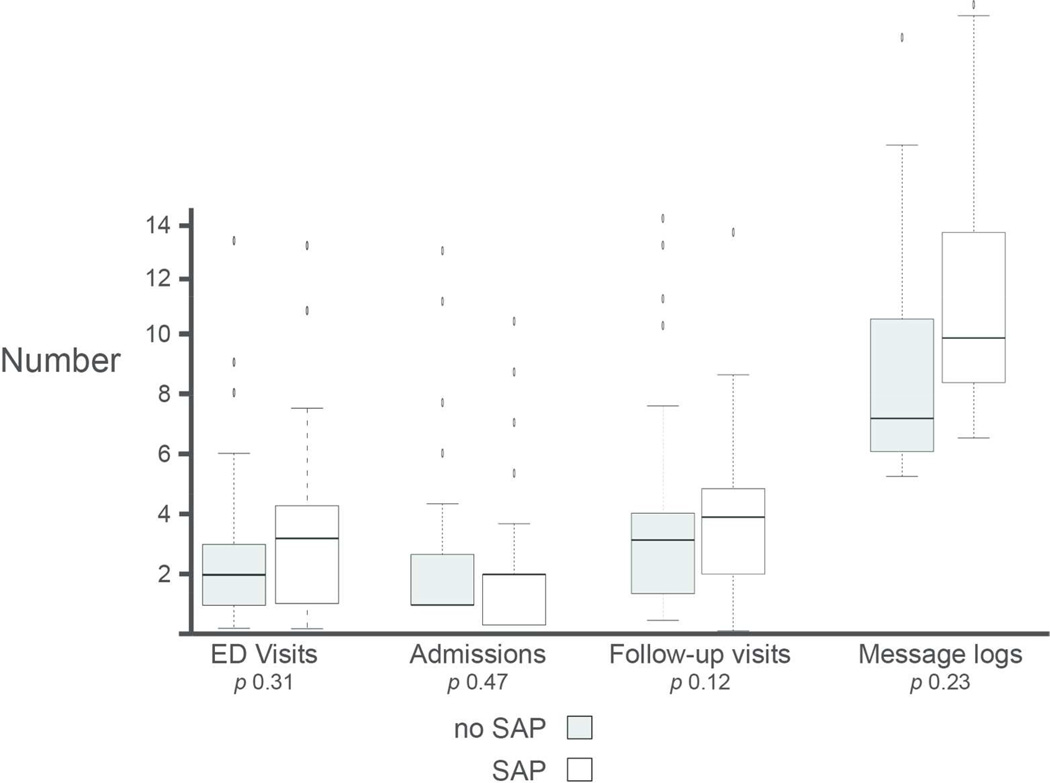
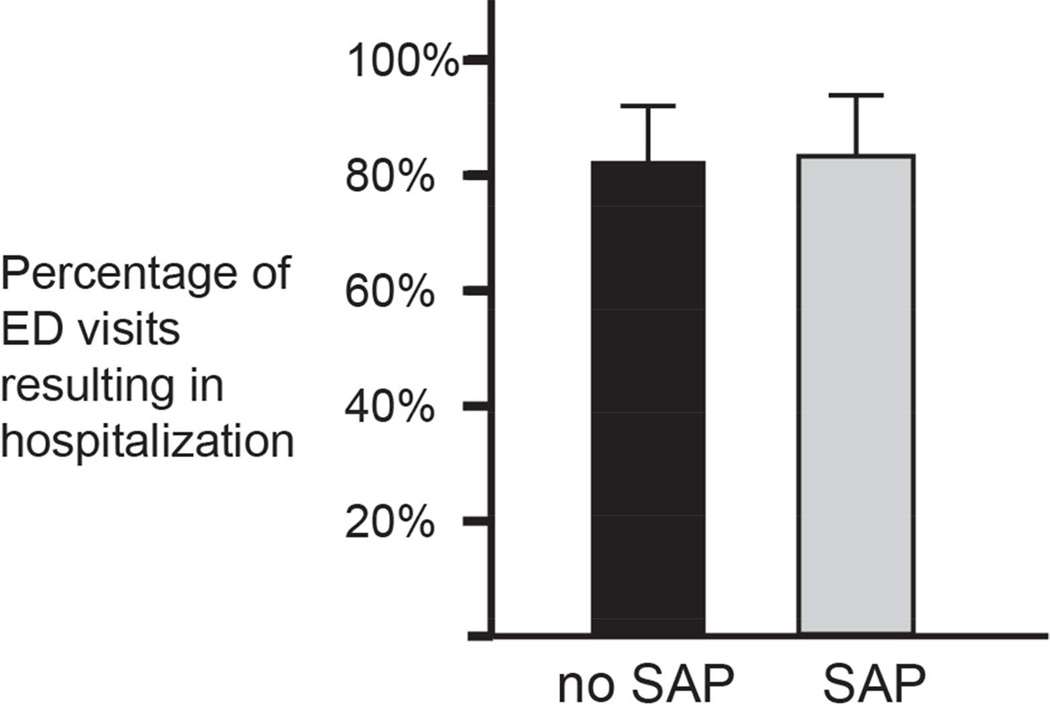
The SAP included a list of current AEDs and dosages, instructions for use of rescue medications when necessary, instructions for break-through seizures, and a specific follow-up plan (Figure 1). To determine whether use of a SAP reduced health care utilization we measured several outcomes, including number of ED visits, number of hospital admissions, number of pediatric neurology clinic visits, number of phone calls to the pediatric neurology offices (Figure 2), and the percentage of ED visits that resulted in hospitalization (Figure 3). There were no statistically significant differences in these outcomes between the SAP and nSAP groups (Table 2), except that the number of follow-up clinic visits was increased in the group with Seizure Action Plans (4.2 versus 3.3, p 0.006).
FIGURE 2.
Number of ED visits, hospital admissions, neurology clinic follow-up visits and telephone messages (“message logs”) before (No SAP) and after (SAP) implementation of a Seizure Action Plan, each group compared over 18 months. There were no statistically significant differences in outcomes between the groups. Box plots (25th and 75th percentiles); center line, median; whiskers, 1.5 interquartile range.
FIGURE 3.
Percentage of ED visits that result in hospital admission before (No SAP) and after (SAP) implementation of a Seizure Action Plan. There was no statistical difference between the groups, p= 0.99. Error bars, binomial proportion confidence interval (95% confidence interval).
Table 2.
Outcomes in SAP and nSAP groups. Numbers (mean; median in parentheses) (as displayed in Figures 2 and 3) for healthcare utilization before and after implementation of seizure action plan are provided. Subgroup analysis only included patients on 3 or fewer anti-epileptic drugs (AEDs). Outcomes and corresponding p value shown.
| Outcomes | Initial Analysis | Subgroup Analysis (patients on <4 AEDs) |
||||
|---|---|---|---|---|---|---|
| nSAP n=60 |
SAP n=60 |
p-value | nSAP n=59 |
SAP n=53 |
p-value | |
| ED Visits | 2.5(2) | 3.0(3) | 0.17 | 2.5(2) | 3.0(3) | 0.16 |
| Admissions | 1.8(1) | 2.0(2) | 0.37 | 1.8(2) | 1.9(2) | 0.65 |
| F/up visits | 3.3(3) | 4.2(4) | 0.006 | 3.4(3) | 4.0(4) | 0.029 |
| Message Logs | 11.7(7) | 14.1(10) | 0.10 | 11.9(12) | 13.3(13) | 0.30 |
| % ED Visits that resulted in hospitalization | 81.7% | 81.9% | 0.99 | 82.0% | 75.7% | 0.43 |
Because of the difference in baseline demographics between the SAP and nSAP groups, with more SAP patients on 4 or more AEDs, we performed a subgroup analysis on the 59 nSAP patients compared to the 53 SAP patients who were on fewer than 4 AEDs (shown in Table 2). In this subgroup analysis there also were no significant differences identified between the SAP and nSAP groups. Of note, the number of males compared to females, which showed a statistically significant difference in the original analysis, was not significant in the subgroup analysis.
DISCUSSION
We found that a SAP had no effect in decreasing healthcare utilization in pediatric epilepsy patients. We did not find any statistically significant decreases in emergency department utilization, hospital admissions, or telephone messages between the two groups. In fact, we observed that the number of follow-up clinic visits was increased in the group with SAPs (4.2 versus 3.3, p 0.006). Nor did we find a difference in the percentage of ED visits that resulted in hospitalization. Our study is one of the first that we are aware of to attempt to improve pediatric epilepsy patient care by reducing healthcare utilization.14
We compared different outcome measures in patients with epilepsy who did or did not have a SAP. In the comparison between groups there was no decrease in utilization in patients who had a SAP. For example, the number of emergency department visits in the no SAP group was 2.5 visits, compared to 3 in the SAP group. Since we found a statistically significant higher percentage of SAP patients who were taking four or more anti-epileptic medications (p 0.028), we also performed a subgroup analysis of the two groups for those patients on fewer than four anti-epileptic medications. Even for the subgroup analysis there was no decrease in utilization by the SAP group. For example, clinic visits were 3.4 in the no SAP group and 4 in the SAP group.
Pediatric epilepsy patients have significant medical costs,11 and there is significant variation across institutions in how care for these patients is delivered.12 Some studies have shown that increased education can improve understanding of epilepsy 4 and that lay-education programs can improve health and reduce hospitalizations. 2, 3 Interestingly, however, our findings mirror a Joint Commission study of Asthma Action Plans, in which there was the unexpected finding that implementation of Asthma Action Plans did not decrease frequency of ED visits and hospitalizations.9 Other studies of pediatric asthma patients have found that adolescent patients or patients with public insurance had higher readmission rates.13 Thus, there may be unexpected and/or unrecognized clinical and social factors to uncover in order to design methods to reduce epilepsy healthcare utilization.
Limitations to this study include that is was conducted retrospectively; and that the patient cohorts were collected during different time epochs. There was a potential bias in that patients in the control (nSAP) group were on fewer overall medications, suggesting that the patients in the nSAP group had less severe epilepsy. However, even when we performed a sub-group analysis consisting of only patients on 3 or fewer AEDs, our results still showed no difference in outcomes between SAP and nSAP groups. Further, a Fisher’s exact test comparing the proportion of patients on three or more AEDs versus two or fewer, in the SAP and nSAP, shows no statistical difference (two-tailed p=0.25).
It is possible that we have not identified the appropriate outcome measures, and that ED visits and hospitalizations are not the best reflections of SAP efficacy. Also, our cohort of 60 patients and a follow-up of 18 months may not have been sufficient to detect more subtle differences, and our post-hoc power analysis revealed a power of only 3–7%. Further, examining hospital admissions, if we assumed an 80% power and significance level of 5%, the effect size is only 0.14 (Cohen’s d), indicating near complete overlap of the SAP and nSAP groups. Thus, our work provides important direction for future research, suggesting that significantly larger patient cohorts will be necessary.
This study did not address whether there was improved education as a result of implementation of the SAP. While assumed to be true, simply providing the SAP document may not have resulted in “adequate” education to affect outcomes. SAPs were not discussed in a standardized fashion when introduced to families; and discussion of SAPs at follow-up clinic visits was left to the discretion of the individual clinician. This variability could potentially obscure the utility of SAPs.
In conclusion, we found no significant change in healthcare utilization following the implementation of the SAP. Potential future studies to reduce pediatric epilepsy healthcare utilization could include a more standardized provision of the SAP; changes in the format (for example, larger fonts or uses of bright colors) of the SAP; or inclusion of on-line links to information on epilepsy. For example, we have developed a “Medical Home Portal” that provides on-line information for families on commonly diagnosed neurological conditions including epilepsy.15 Another approach for a revised SAP might include an explicit flow diagram, instructing parents to call the on-call provider for any seizure. While this would likely result in an increase in phone calls, we could determine if this intervention might reduce emergency department and admission rates. Other SAPs have also been developed, for example by the Epilepsy Foundation16 and by many school districts; but their efficacy has not been evaluated. Future studies could also examine family perception of complexity of disease management, and on perceived stress associated with the diagnosis of epilepsy and management. Studies such as these can lead towards identification of factors necessary to improve pediatric epilepsy patient health.
Acknowledgements
We thank R. Larson for acquisition of the data.
Funding
JLB was supported by the March of Dimes Research Foundation; and NIH DP2 MH100008.
Ethical Approval
This study was approved by the University of Utah and Primary Children’s Medical Center Institutional Review Boards.
Footnotes
Author Contributions
LR performed data collection and analysis and is responsible for the integrity of the data and accuracy of analysis and the manuscript. All authors were involved in study conception and design, editing, and approved the final version of the manuscript.
Conflicts of Interest
The authors state that they have no conflicts of interest.
REFERENCES
- 1.Bertsche A, Dahse AJ, Neininger MP, et al. Ambulatory care of children treated with anticonvulsants - pitfalls after discharge from hospital. Klin Padiatr. 2013;225(5):277–282. doi: 10.1055/s-0033-1345174. [DOI] [PubMed] [Google Scholar]
- 2.Nolte S, Osborne RH. A systematic review of outcomes of chronic disease self-management interventions. Qual Life Res. 2013;22(7):1805–1816. doi: 10.1007/s11136-012-0302-8. [DOI] [PubMed] [Google Scholar]
- 3.Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309(4):372–380. doi: 10.1001/jama.2012.188351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen C, Lee DS, Hie SL. The impact of pharmacist's counseling on pediatric patients' caregiver's knowledge on epilepsy and its treatment in a tertiary hospital. Int J Clin Pharm. 2013;35(5):829–834. doi: 10.1007/s11096-013-9817-5. [DOI] [PubMed] [Google Scholar]
- 5.Holsti M, Sill BL, Firth SD, et al. Prehospital intranasal midazolam for the treatment of pediatric seizures. Pediatr Emerg Care. 2007;23(3):148–153. doi: 10.1097/PEC.0b013e3180328c92. [DOI] [PubMed] [Google Scholar]
- 6.Foster G, Taylor SJ, Eldridge SE, Ramsay J, Griffiths CJ. Self-management education programmes by lay leaders for people with chronic conditions. Cochrane Database Syst Rev. 2007;(4):CD005108. doi: 10.1002/14651858.CD005108.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Effing T, Monninkhof EM, van der Valk PD, et al. Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007;(4):CD002990. doi: 10.1002/14651858.CD002990.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Aliasgharpour M, Dehgahn Nayeri N, Yadegary MA, Haghani H. Effects of an educational program on self-management in patients with epilepsy. Seizure. 2013;22(1):48–52. doi: 10.1016/j.seizure.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Morse RB, Hall M, Fieldston ES, et al. Hospital-level compliance with asthma care quality measures at children's hospitals and subsequent asthma-related outcomes. JAMA. 2011;306(13):1454–1460. doi: 10.1001/jama.2011.1385. [DOI] [PubMed] [Google Scholar]
- 10.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cramer JA, Wang ZJ, Chang E, et al. Healthcare utilization and costs in children with stable and uncontrolled epilepsy. Epilepsy Behav. 2014;32:135–141. doi: 10.1016/j.yebeh.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 12.Standridge SM, Horn PS. Variations in hospitalization outcomes in children admitted with seizures between 2003 and 2006. J Child Neurol. 2012;27(7):898–906. doi: 10.1177/0883073811436325. [DOI] [PubMed] [Google Scholar]
- 13.Kenyon CC, Melvin PR, Chiang VW, et al. Rehospitalization for childhood asthma: timing, variation, and opportunities for intervention. J Pediatr. 2014;164(2):300–305. doi: 10.1016/j.jpeds.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Patel AD. A case series using a care management checklist to decrease emergency department visits and hospitalizations in children with epilepsy. J Child Neurol. 2014;29(2):243–246. doi: 10.1177/0883073813500851. [DOI] [PubMed] [Google Scholar]
- 15.Norlin C, Romeo A, Rocha R. Developing a web site to support the implementation of medical home. AMIA Annu Symp Proc. 2007;11:563–567. [PMC free article] [PubMed] [Google Scholar]
- 16. https://www.epilepsy.com/sites/core/files/atoms/files/seizure-action-plan-pdf_0.pdf.