Abstract
Background
Breast cancer is the second leading cause of cancer mortality among women in the developed world. Mammography screening is especially important for African Americans because they experience a greater mortality (OR=1.38) than Caucasians despite having a lower incidence of breast cancer.
Purpose
The purpose of this study was to compare the effects of two interventions with usual care on mammography adherence among African American women.
Methods
A subsample of African American women (n=244) aged 41-65 years who had not had a mammogram in the last 15 months and no history of breast cancer were randomly assigned to receive: 1) mailed interactive DVD, 2) computer-tailored telephone counseling, or 3) usual care.
Results
The DVD intervention was 5 times more effective than usual care for promoting mammography screening at 6 months follow-up among women who earned less than $30,000 (OR= 5.3). Compared to usual care, neither the DVD nor phone produced significant effects for women with household incomes >$30,000.
Conclusion
Use of a mailed DVD for low-income African American women may be an effective way to increase mammography adherence.
Keywords: Randomized intervention, mammography adherence, African-American, Interactive DVD, controlled trial, health disparities
BACKGROUND
Breast cancer is the most common cancer and the second leading cause of cancer mortality among women in the developed world [1-3]. In 2013, an estimated 232,340 new cases of breast cancer and 39,620 breast cancer deaths were expected to occur in the United States of America. The 2006-2010 incidence rates across all racial/ethnic groups declined or remained stable, with a slight increase (0.2% per year) among African American women [4, 5]. Although the incidence of breast cancer across all age groups is lower in African American women as compared to Caucasian women (121.4/100,000 v.127.4/100,000) [6-8], the incidence for ages 45 and younger is highest among African American women as compared to Caucasian women [7]. Additionally, African Americans have a higher breast cancer mortality rate than their Caucasian counterparts (30.8/100,000 v. 22.1/100,000). In summary, breast cancer in African American women is characterized by occurrence at an early age, less favorable clinical outcome, and a more aggressive tumor phenotype [6-8].
Although race plays an important role in breast cancer mortality, studies have found that income also impacts breast cancer outcomes. The incidence of breast cancer is higher among high income women compared to low income women [9, 10], but the mortality rate is reversed. Low income women have higher mortality rates of breast cancer compared to high income women [4]. Race and socio-economic disparity can partly be attributed to barriers that impede access to timely, high-quality medical care [5]. However, it is clear that both race and income affect mammography rates.
Early detection remains our most important strategy for addressing breast cancer disparities, as evidenced by prospective studies showing mortality reduction benefit [11-14]. Breast cancer mortality can be reduced by up to 49% for women who were screened compared to those who were not screened [14] and population screening rates have been associated with early diagnosis [15]. Late stage diagnosis complicates the outcome because few and less effective treatment choices are available [1, 5]. Mammography screening rates among African American women (73%) and Caucasian women are equivalent, but remains below the 81% healthy people 2020 objective [16-19] and is lowest among African American women living below 200% of the poverty level [20]. In 2008, 51% of women living below the poverty level threshold, including women earning less than $30,000, were adherent to mammography screening compared to 73% of higher-income women [1]. Therefore, low-income African American women are a priority for increasing mammography screening.
Overall, tailored interventions have been used and documented to be effective in increasing mammography adherence [21]. Fewer tailored interventions have been tested among African American women. These studies have shown tailoring to be effective in increasing mammography screening rates among African American women [22-28]. A major question about differences in intervention efficacy must be answered before we can begin translation to this population. In our previous work, when all races were included (n=1681) we found a significant interaction between intervention and household income, such that the DVD was more effective (OR=1.51; 95% C.I. 1.08-2.13) than usual care for women with household incomes less than $75,000 [29]. The role of socioeconomic status and intervention efficacy within the African American population remains understudied; only a few researchers have assessed the relationship between income and mammography adherence. It is under this premise that we conducted a subset analysis of African American women (n=244) enrolled in a randomized controlled trial to increase mammography adherence. Specific research questions included:
What are the differences in mammography adherence among African American women who received a mailed tailored DVD intervention, a tailored telephone counseling intervention, or usual care?
Does intervention effectiveness vary by household income?
METHODS
Sample and Recruitment
The sample of 244 African American women was recruited from two locations: a large health maintenance organization in the Midwest and a large insurance plan in North Carolina. Two sites were important to increase sample size as well as enhance generalizability of the interventions across states and in two types of insurances-managed care and a traditional insurance plan. The study was approved by institutional review boards at Duke and Indiana Universities. This controlled study was registered in a public registry, clinicaltrials.gov, registration number NCT00287040.
The women were included if they were: aged 41–65 years, could read English, and had no previous breast cancer or bilateral mastectomies. Women were included if they did not have a mammogram during the last 15 months; a cut off that was consistent with US annual screening guidelines at the time of enrollment [30]. For these women, the cost of mammography was covered with no co-pay or out-of-pocket funds thus eliminating cost as a confounding variable.
Women who met the inclusion criteria were mailed introductory letters with a brief study description and instructions for opting out of contact. Those who did not want to be contacted could opt out by calling a toll-free number within two weeks of receiving the letter. Women who did not opt out were called by research assistants (RAs) who used a standard protocol and a computerized tracking system. The RAs explained the study and assessed their interest in participating. Verbal consent was sought from women willing to participate in the study, and baseline data collected during this call or during another scheduled phone call. Women who consented to participate were mailed the written Health Insurance Portability and Accountabitlity Act (HIPAA) form to allow the researchers to access their medical records. Thereafter, the women were randomly assigned to one of the three groups: 1) mailed tailored interactive DVD, 2) tailored telephone counseling, or 3) usual care.
This paper's analysis is based on a sample derived from the original study (n=1,681) where power had been predetermined. The original study was a random sample of women from urban health care centers according to the distribution of Caucasians and African Americans, representative of those in the Health care system and were needing a mammography. A total of 1,681 sample size was calculated and would yield adequate power to detect clinically significant effects, as well as detect an overall difference of 10% in mammography adherence among any of the three groups. Simple random assignment to the three groups was performed with a computer using a random number generator (SQL randomizing code). The allocation assignment was concealed by the computer program until interventions were assigned. The investigators generated the random allocation sequence, enrolled the participants (in collaboration with The Center for Survey Research, Indiana University) and assigned participants to interventions.
Measurements
Data were collected on the phone by trained interviewers at three time points: baseline (T1), 4 weeks [intervention groups only] (T2), and six months (T3). Time 2 measurements assessed satisfaction with the intervention, thus usual care was not included in T2 assessment. Intervention groups received either the mailed DVD, or phone intervention. The usual care group completed surveys at baseline and 6 months but received no intervention. Details of recruitment and data collection have been discussed elsewhere [29, 31].
Demographics, insurance information, medical history, personal experience, media exposure and family history were assessed at baseline using standard questions. Key demographic questions included age, race, religious background, education, marital status, occupation, and number of children. Participants were queried regarding any mammography recommendations or counseling outside of the study protocol. Perceived barriers, perceived benefits, perceived risk of breast cancer, breast cancer fear, cancer fatalism and self-efficacy for mammography were measured using scales that are reliable and have been validated [32]. For example, barrriers included two subscales reflecting logistic and perceived barriers. Perceived barriers included a 10-item subscale with an internal consistency coefficient of .88 and test-retest coefficient was.86. Logistical Barriers included an 11-item subscale including barriers that are logistical in nature such as transportation, costs, time etc.
Outcome. Mammography adherence (the outcome variable) was computed as a combined score using both medical records and six-month self-report data. Women were classified as being adherent if either self-report or medical records indicated they had a mammogram between baseline and six months. These outcome data were 97% complete for mammography adherence with only 3% missing. A validation test of self-reported and medical records was conducted and the overall kappa coefficient of agreement was 0.82.
Development, Tailoring and Implementation of Interventions
The development of tailored interventions was framed by the Health Belief and Transtheoretical Models (TTM) previously associated with promoting mammography use [32-47]. The messages contained in both the DVD and phone counseling were tailored on: 1) perceived and actual risk; 2) perceived benefits, 3) barriers, 4) self-efficacy; and 5) knowledge. Intervention content has been explained in detail elsewhere [31].
Tailoring was done by first asking participants to respond to a question about each of the beliefs as well as provide demographic information using the arrow keys on the DVD remote. Message responses were selected based on algorithms built into the DVD program. There were more than 36 combinations of messaging. By answering the questions throughout the program, messages specific to the individual woman's beliefs were delivered. For example, If an individual did not believe there was benefit to screening, a message about the benefits of early screening would be delivered.
The DVD began with a narrator introducing the program. Four women characters representing different demographic profiles, including an African American woman, delivered the intervention messages. All women viewed an animation of breast cancer developing and spreading throughout the body which illustrated metastasis. Women who never had a mammogram were shown a video of the mammography process starting with an appointment. Finally, women were queried and received messages about individual barriers that would prevent them from receiving a mammogram. The DVD program ended with the narrator encouraging viewers to make a mammography appointment.
The telephone intervention was developed using the same tailoring variables. Messages used in the interactive DVD and the telephone intervention were kept as consistent as possible so that intervention content varied only by media delivery. The main differences between the two interventions were that in the DVD program, women were able to view illustrations and the message was delivered by an African American woman, which could not be attained via telephone. The telephone intervention was delivered by counselors who were graduate students. The students (RAs) were trained to deliver tailored content that reflected each woman's responses to questions (counseling sessions were recorded for quality control). To ensure consistency, all the RAs were rigorously trained and followed a telephone script. All phone interviews were recorded and one of the investigators evaluated a sample of the recordings using a check-list. To keep both content and time consistent for each participant, the interveners were trained to politely terminate attempts at extraneous dialogue. An analysis of the average length of time women spent using the interactive DVD was 10 minutes while women in the telephone intervention took, on average, 11.3 minutes. Usual Care.
Women randomized to the usual care group did not receive any intervention. Usual care varied depending on location but ranged from nothing to a post-card reminder when it was time to schedule a mammogram. These women would receive standard care from their health care providers.
Statistical Strategy
All statistical analyses were conducted using SAS (version 9.3). Chi square distribution test and ANOVA statistics were performed to compare frequency distributions and means of covariates by intervention arms. We used binary logistic regression analysis adjusted for various demographic and other theoretical variables to test the effect of the intervention on mammography adherence (see results section and Table 2). In addition, we tested interactions between the intervention and baseline covariates for potential moderating effects. P-values less than .05 were considered statistically significant. To satisfy the 10 participants/parameter rule, we have reported the binary logistic regression model adjusting only for demographic variables (age, education, and income) as well as doctor recommendation and the woman's stage of change (pre-contemplation vs contemplation). However, as a sensitivity analysis, we also ran binary logistic regression models while adjusting for all demographic factors and TTM construct scale scores. Variables associated with mammography adherence and their effect sizes were very similar in both models.
Table 2.
Logistic Regression Model of Mammography Adherence Behavior
| Intervention Effect | |
| DVD vs usual care | 1.64 (0.80-3.39) |
| Telephone vs usual care | 1.24 (0.61-2.50) |
| Covariates | |
| Baseline Stage (Contemplation vs. Pre-Contemplation) | 8.78 (2.91-26.52) |
| Age | 1.03 (0.99-1.07) |
| Education 4 yrs. college or more | 1.06 (0.48-2.36) |
| Married | 0.61 (0.34-1.09) |
| Media source | 1.10 (0.93-1.29) |
| Doctor recommendation | 3.16 (1.32-7.58) |
| Household income (>75K vs <30K) | 1.78 (0.57-5.56) |
| Household income (30-75K vs <30K) | 1.39 (0.68-2.83) |
*Groups that were significant are bolded
RESULTS
Sample
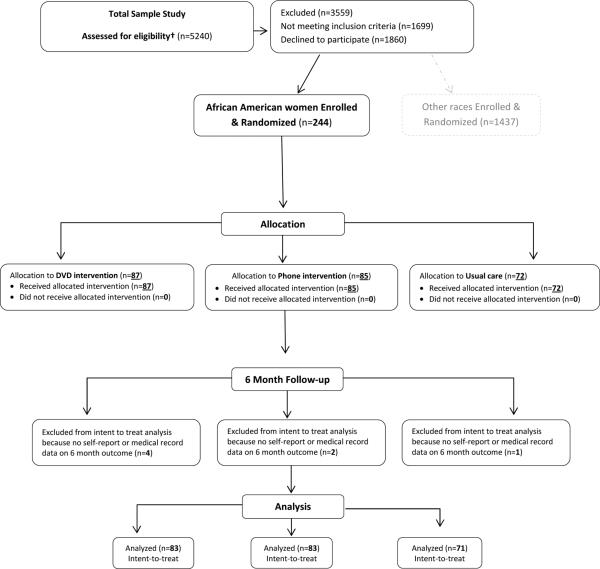
A total of 244 women were randomly assigned to: DVD (n=87), telephone (n=85), or usual care group (n=72). Randomization was effective in rendering groups similar in age, demographic variables, TTM constructs, and intention to have a mammogram (Table 1). However, more women in the telephone group were currently employed (94%) compared to the usual care group (81%). There were no significant mean differences for any of the belief constructs by intervention group.
Table 1.
Participant Characteristics and Baseline Beliefs by Group (N=244)
| Characteristics/Beliefs | DVD Group (N = 87) | Telephone Group (N = 85) | Usual care Group (N = 72) | |
|---|---|---|---|---|
| Mean (SD) | P value | |||
| Age | 51.3 (7.4) | 51.7 (7.7) | 50.6 (6.7) | 0.6161 |
| Number of media sources | 3.2 (1.8) | 3.4 (1.8) | 3.3 (1.8) | 0.8831 |
| Constructs | ||||
| Barriers | 43.7 (9.82) | 45.6 (11.66) | 43.1 (9.51) | 0.2841 |
| Benefits | 16.6 (2.34) | 16.2 (2.48) | 16.2 (2.22) | 0.5556 |
| Fatalism | 24.9 (6.44) | 24.8 (5.8) | 24.8 (5.55) | 0.9940 |
| Fear | 24.6 (7.43) | 22.45 (8.0) | 23.1 (7.0) | 0.1446 |
| Knowledge | 5.2 (1.41) | 5.2 (1.05) | 5.6 (1.12) | 0.0623 |
| Optimism | 16.9 (3.76) | 17.1 (4.0) | 16.4 (3.58) | 0.5482 |
| Susceptibility | 13.2 (3.91) | 13.1 (3.33) | 12.9 (2.82) | 0.8904 |
| Self-Efficacy | 41.1 (4.88) | 40.4 (5.04) | 40.8 (4.47) | 0.6872 |
| n (%) | ||||
| Education: ≥ 4 year college degree | 17 (19.5) | 14 (16.5) | 23 (31.9) | *0.0512 |
| Doctor ever suggested a mammograms | 73 (83.9) | 69 (81.2) | 61 (84.7) | 0.8189 |
| Married or living with a partner | 53 (60.9) | 46 (54.1) | 40 (55.6) | 0.6394 |
| Currently working for pay | 79 (90.8) | 80 (94.1) | 58 (80.6) | 0.0206 |
| Household income | ||||
| <$30,000 | 27 (31.8) | 23 (27.4) | 17 (23.6) | 0.3494 |
| $30,000 - $75,000 | 50 (58.8) | 48 (57.1) | 40 (55.6) | |
| >75,000 | 8 (9.4) | 13 (15.5) | 15 (20.8) | |
| Mammography stage (baseline) | ||||
| Pre-contemplation | 19 (21.8) | 10 (11.8) | 12 (16.7) | 0.2098 |
| Contemplation | 68 (78.2) | 75 (88.2) | 60 (83.3) | |
| Site | ||||
| Duke University | 26 (29.9) | 35 (41.2) | 22 (30.6) | 0.2246 |
| Indiana University | 61 (70.1) | 50 (58.8) | 50 (69.4) | |
| Mammography Adherence (outcome) | 34 (41.0) | 35 (42.2) | 25 (35.2) | 0.6491 |
Groups that were significantly different are bolded
Research Question 1
Analyses unadjusted for covariates across groups showed that overall mammography uptake increased similarly among all three groups – 41% for DVD, 42% for telephone counseling, and 35% for usual care (p=.6491). Logistic regression testing intervention efficacy in increasing mammography adherence while adjusting for baseline demographic characteristics (Table 2) showed neither the DVD (OR=1.64; 95% CI 0.80-3.39) nor Telephone (OR = 1.24; 95% C.I. 0.61-2.50) intervention was more efficacious when compared to usual care.
However, two covariates were associated with having a mammogram: baseline stage-change (pre-contemplation vs contemplation) and physician recommendation. Women who were in the contemplation stage had a higher odds (OR = 8.8) of adherence compared to those in the pre-contemplation stage. Women who had mammography recommended by their physicians were 3.2 times more likely to have a mammogram compared to women who did not have a recommendation.
Research Question 2
The second research question sought to determine whether intervention efficacy to increase mammography adherence varied by income group. The DVD intervention was more effective than usual care for African American women with the lowest household incomes (< $30,000), but not for those with higher household incomes (Table 3). African Americans with household incomes of less than $30,000 who received the DVD were 5 times more likely to be adherent at 6 months, compared to women in usual care (Table 3). The Telephone intervention was not effective for African American women at any of the three income levels.
Table 3.
Pre-planned Test of Intervention Efficacy on Mammography adherence among African American Household income groups
| ≤30K | |
| DVD vs Telephone | 1.38 (0.39-4.88) |
| DVD vs Usual care | 5.34 (1.12-25.42) |
| Telephone vs Usual care | 3.87 (0.81-18.52) |
| 30-75K | |
| DVD vs Telephone | 0.99 (0.41-2.42) |
| DVD vs Usual care | 0.99 (0.39-2.51) |
| Telephone vs Usual care | 1.00 (0.40-2.51) |
| ≥75K | |
| DVD vs Telephone | 2.78 (0.39-19.93) |
| DVD vs Usual care | 1.68 (0.25-11.36) |
| Telephone vs Usual care | 0.60 (0.11-3.40) |
*Groups that were significant are bolded
DISCUSSION
The findings from analyses of this African American subgroup yielded important insights into applicability of a tailored mammography intervention delivered via DVD. When considering all income groups neither the DVD nor telephone intervention was effective in increasing mammography adherence among African American women. These findings are similar to the full dataset (n=1,681) that included Caucasian women [29]. However, household income demonstrated a moderating effect on the DVD intervention in the full dataset which led us to investigate this moderating effect in African American women. African American women with household incomes of $30,000 or below who received the DVD intervention were 5 times more likely to get a mammogram than those in the control group. For the middle and upper income groups the odds ratios were not significant for DVD compared to usual.
Results from analyses using only the African American sample were compared to results using both Caucasian and African American women. For the original study which included Caucasians, women in both the lowest (<$30,000) and middle income ($30,000-$75,000) groups revealed significant intervention effects for DVD. Therefore, the low and middle income groups were combined yielding an odds ratio of 1.5 (95% C.I; 1.03-2.27) [29]. In the African American sample, the DVD's significant intervention effect was only significant for those in the lowest income group (<$30,000). However, efficacy of the DVD in the lowest household income group was much greater in African American women (OR=5.3) than in the larger study (OR= 1.2). These results are consistent with other studies that have shown that tailored interventions have been effective for low income African American populations [22-28, 48]. In fact, in the first-ever tailored mammography intervention study published two decades ago [49] tailoring was more effective only for African Americans and those with lower incomes. But, the five-fold effect size (OR=5.3) we found in the lowest-income subgroup of African American women is exceptional. Post hoc power analysis indicated that we detected a very large effect size with only 35% statistical power (2-sided test) which is great.
The large odds ratio for DVD vs usual care in the African American sample has important implications for increasing mammography rates in this at risk population. Studies have shown that African American women with lower incomes are generally less likely to be screened [50]. Several factors may explain the moderating effect of income. We wondered whether women's reactions to the DVD intervention might help explain the differences in intervention effect by income and therefore conducted additional analysis with some of the process outcomes data [31]. We found a suggestion that low income women paid the most attention to the DVD content (pvalue=0.0373). A full 100% of the lowest income women reported having no trouble paying attention to the DVD compared to 97% of the middle income group and 75% of those with the highest incomes (75%). This additional attention may have maximized their learning about breast cancer and persuasion about benefits of mammography adherence and subsequently alleviated their fears and barriers encouraging them to go on to actually getting a mammogram.
Employment status was different between the intervention groups and usual care. In the usual care group, 81% of the women reported that they worked for pay compared to the DVD (91%) and Telephone (94%) intervention groups. Women who worked, especially those with higher household incomes, reported having less time available to get a mammogram, both at baseline and follow up, a barrier which may have prevented them receiving a mammogram, partially explaining why the intervention was not effective for the women who had a higher household income. We did not adjust for work for pay in the logistic models because income was in the model and was correlated with work for pay.
Varying education levels may also partially explain why the intervention was more effective among the lowest income group. There were fewer women with a four year college education in the low income group (1.5%) compared to the middle (19.6%) and high (72.7%) income group. Having a low education has been associated with lower health literacy, less knowledge about screening, and higher barriers making the messages in the DVD important or relevant for them [50-52]. The DVD was developed to overcome the problem of low health literacy as well as barriers to mammography associated with low health literacy. A tailored program was delivered in narrative format which could have resulted in greater understanding of the importance of screening. Additionally, the lowest income group had a higher mean barrier score (45) at baseline compared to the middle (43.1) and high income groups (42.9), perhaps providing more opportunity for the intervention to reduce barriers and lead to behavior change.
Other reasons why the DVD was the most effective in low income women may be intrinsic to the DVD as a mode of communication. Engagement in the intervention is an important factor in intervention efficacy. Communication theory- has demonstrated that interventions that engage users are more likely to have an effect [51]. The DVD was interactive and further analysis did reveal that women who received the DVD felt the intervention related more to them (88%) when compared to those receiving Telephone intervention (74%). The DVD with its combination of audio and video may have been a more effective communication channel. The mechanism in which the video may have motivated the women may be through increased literacy and fear. For example, perhaps when women watched the animation of the cancer development process and metastasis, this may have evoked fear and led the women to seek a mammogram. The use of narratives also have been found to be effective in increasing intention to get a mammogram among low income African American women [52]. The DVD also has the advantage of potentially being used several times and shared among family and friends which potentially increases its impact.
Limitations: Generalizing the results of this study is limited to the women similar to those who agreed to participate. Also, this was sub-sample generated from a larger study that was randomly selected; the study was not designed to recruite African American women only. Although participants were randomly assigned to the intervention groups, the usual care group had significantly higher education levels. Also, fewer women in the usual care group were currently working for pay compared to women in the telephone group. As is common in intervention studies, loss to follow-up occurred, however, mammography adherence information was collected based on either self-report or medical records. As a result, 97% complete data were attained for this primary outcome, overcoming the problem of lost information due to attrition.
Conclusion
The tailored DVD intervention was very effective in promoting receipt of a mammogram with African American women whose household income was $30,000 or less. The DVD, once produced, can be easily disseminated to women in need of mammography. Therefore, it can be an inexpensive method to promote mammography adherence in the most economically vulnerable population in the African American community. Indeed, our preliminary analyses indicates that the DVD was 3-times less expensive ($6.84/person) than the telephone ($22.50/person) intervention. Since women with low household incomes report low mammography screening rates, the findings of this study have significant translational potential. In addition, moving women forward to contemplating having a mammography and receipt of a physician recommendation are paramount to increasing mammography adherence in all women. Further research in larger studies is needed to explore the role of household income in promoting mammography adherence in African American women. Lastly, it will be important to conduct comparative studies between racial groups on the efficacy of tailored interventions in increasing mammography adherence.
Fig 1. Consort Flow Diagram for African American Sample obtained from larger study.
This diagram shows the number of women who were eligible, those allocated to each intervention group-DVD, Telephone and Usual Care and those who were analyzed. †No race data was collected from those who were eligible; race data is only available for those who consented to participate and enrolled in the study.
Acknowledgements
Funding for this research was provided by the Institute for Nursing Research at the National Institutes of Health [grant number R01 NR008434]/ Clinical Trials Number NCT000287040. In addition, Wambui is a predoctoral fellow funded by the Training in Research for Behavioral Oncology and Cancer Control Program – R25 (PI: Champion). Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number R25 CA117865-07S1 and K05CA175048. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
COI & Ethical Adherence:
Wambui Gathirua-Mwangi, Patrick Monahan, Timothy Stump, Susan Rawl, Celette Skinner and Victoria Champion declare they have no conflict of interest.
All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation. The research complies with ethical guidelines and was approved by the research ethics committee at Duke and Indiana Universities.
REFERENCES
- 1.DeSantis C, Siegel R, Bandi P, Jemal A. Breast cancer statistics, 2011. CA Cancer J Clin. 2011;61:409–18. doi: 10.3322/caac.20134. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 3.Miller JW, King JB, Joseph DA, Richardson LC, Centers for Disease C. Prevention. Breast cancer screening among adult women--Behavioral Risk Factor Surveillance System, United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:46–50. [PubMed] [Google Scholar]
- 4.American Cancer Society . Breast Cancer Facts & Figures 2013-2014. American Cancer Society, Inc.; Atlanta: 2013. [Google Scholar]
- 5.DeSantis C, Naishadham D, Jemal A. Cancer statistics for African Americans, 2013. CA Cancer J Clin. 2013;63:151–66. doi: 10.3322/caac.21173. [DOI] [PubMed] [Google Scholar]
- 6.Danforth DN., Jr Disparities in breast cancer outcomes between Caucasian and African American women: a model for describing the relationship of biological and nonbiological factors. Breast Cancer Res: BCR. 2013;15:208. doi: 10.1186/bcr3429. Jr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Newman LA. Breast cancer in African-American women. Oncologist. 2005;10:1–14. doi: 10.1634/theoncologist.10-1-1. [DOI] [PubMed] [Google Scholar]
- 8.Sturtz LA, Melley J, Mamula K, Shriver CD, Ellsworth RE. Outcome disparities in African American women with triple negative breast cancer: a comparison of epidemiological and molecular factors between African American and Caucasian women with triple negative breast cancer. BMC Cancer. 2014;14:62. doi: 10.1186/1471-2407-14-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Borugian MJ, Spinelli JJ, Abanto Z, Xu CL, Wilkins R. Breast cancer incidence and neighbourhood income. Health Rep. Jun. 2011;22:7–13. [PubMed] [Google Scholar]
- 10.Dano H, Andersen O, Ewertz M, Petersen JH, Lynge E. Socioeconomic status and breast cancer in Denmark. Int J Epidemiol. 2003;32:218–24. doi: 10.1093/ije/dyg049. [DOI] [PubMed] [Google Scholar]
- 11.Amirikia KC, Mills P, Bush J, Newman LA. Higher population-based incidence rates of triple-negative breast cancer among young African-American women : Implications for breast cancer screening recommendations. Cancer. 2011;117:2747–53. doi: 10.1002/cncr.25862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith RA. The value of modern mammography screening in the control of breast cancer: understanding the underpinnings of the current debates. Cancer Epidemiol Biomarkers Prev. 2014;23:1139–46. doi: 10.1158/1055-9965.EPI-13-0946. [DOI] [PubMed] [Google Scholar]
- 13.Weedon-Fekjaer H, Romundstad PR, Vatten LJ. Modern mammography screening and breast cancer mortality: population study. BMJ. 2014;348:g3701. doi: 10.1136/bmj.g3701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tabar L, Yen MF, Vitak B, Chen HH, Smith RA, Duffy SW. Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet. Apr. 2003;361:1405–10. doi: 10.1016/S0140-6736(03)13143-1. [DOI] [PubMed] [Google Scholar]
- 15.Sassi F, Luft HS, Guadagnoli E. Reducing racial/ethnic disparities in female breast cancer: screening rates and stage at diagnosis. Am J Public Health. 2006;96:2165–72. doi: 10.2105/AJPH.2005.071761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sadler GR, Ko CM, Cohn JA, White M, Weldon RN, Wu P. Breast cancer knowledge, attitudes, and screening behaviors among African American women: the Black cosmetologists promoting health program. BMC Public Health. 2007;7:57. doi: 10.1186/1471-2458-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Calvocoressi L, Kasl SV, Lee CH, Stolar M, Claus EB, Jones BA. A prospective study of perceived susceptibility to breast cancer and nonadherence to mammography screening guidelines in African American and White women ages 40 to 79 years. Cancer Epidemiol Biomarkers Prev. 2004;13:2096–105. [PubMed] [Google Scholar]
- 18.Ochoa-Frongia L, Thompson HS, Lewis-Kelly Y, Deans-McFarlane T, Jandorf L. Breast and cervical cancer screening and health beliefs among African American women attending educational programs. Health Promot Pract. 2012;13:447–53. doi: 10.1177/1524839910385900. [DOI] [PubMed] [Google Scholar]
- 19. [August, 2014];CDC. Healthy People. 2014 http://www.healthypeople.gov/2020/data/disparities/summary/Chart/4055/3,
- 20.Documet PI, Green HH, Adams J, Weil LA, Stockdale J, Hyseni Y. Perspectives of African American, Amish, Appalachian And Latina women on breast and cervical cancer screening: implications for cultural competence. J Health Care Poor Underserved. 2008;19:56–74. doi: 10.1353/hpu.2008.0018. [DOI] [PubMed] [Google Scholar]
- 21.Sohl SJ, Moyer A. Tailored interventions to promote mammography screening: a meta-analytic review. Prev Med. 2007;45:252–61. doi: 10.1016/j.ypmed.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fouad MN, Partridge E, Dignan M, et al. Targeted intervention strategies to increase and maintain mammography utilization among African American women. Am J Public Health. 2010;100:2526–31. doi: 10.2105/AJPH.2009.167312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Russell KM, Champion VL, Monahan PO, et al. Randomized trial of a lay health advisor and computer intervention to increase mammography screening in African American women. Cancer Epidemiol Biomarkers Prev. 2010;19:201–10. doi: 10.1158/1055-9965.EPI-09-0569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katz ML, Tatum CM, Degraffinreid CR, Dickinson S, Paskett ED. Do cervical cancer screening rates increase in association with an intervention designed to increase mammography usage? J Womens Health (Larchmt) 2007;16:24–35. doi: 10.1089/jwh.2006.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paskett E, Tatum C, Rushing J, et al. Randomized trial of an intervention to improve mammography utilization among a triracial rural population of women. J Natl Cancer Inst. 2006;98:1226–37. doi: 10.1093/jnci/djj333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Avis NE, Smith KW, Link CL, Goldman MB. Increasing mammography screening among women over age 50 with a videotape intervention. Prev Med. 2004;39:498–506. doi: 10.1016/j.ypmed.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 27.Erwin DO, Spatz TS, Turturro CL. Development of an African-American role model intervention to increase breast self-examination and mammography. J Cancer Educ. 1992;7:311–9. doi: 10.1080/08858199209528188. [DOI] [PubMed] [Google Scholar]
- 28.Champion VL, Skinner CS, Menon U, Seshadri R, Anzalone DC, Rawl SM. Comparisons of tailored mammography interventions at two months postintervention. Ann Behav Med. 2002;24:211–8. doi: 10.1207/S15324796ABM2403_06. [DOI] [PubMed] [Google Scholar]
- 29.Smith RA, Saslow D, Sawyer KA, et al. American Cancer Society guidelines for breast cancer screening: update 2003. CA Cancer J Clin. 2003;53:141–169. doi: 10.3322/canjclin.53.3.141. [DOI] [PubMed] [Google Scholar]
- 30.Champion VL, Rawl SM, Bourff SA, et al. Randomized trial of DVD, telephone, and usual care for increasing mammography adherence. J Health Psychol. 2014 doi: 10.1177/1359105314542817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Skinner CS, Buchanan A, Champion V, et al. Process outcomes from a randomized controlled trial comparing tailored mammography interventions delivered via telephone vs. DVD. Patient Education and Counseling. 2011;85:308–12. doi: 10.1016/j.pec.2010.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Champion VL, Monahan PO, Springston JK, Zollinger TW, Saywell RM, Jr., Maraj M. Measuring mammography and breast cancer beliefs in African American Women. J Health Psychol. 2008;13:827–37. doi: 10.1177/1359105308093867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prochaska JJ, Spring B, Nigg CR. Multiple health behavior change research: an introduction and overview. Prev Med. 2008;46:281–5. doi: 10.1016/j.ypmed.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Champion VL, Huster G. Effect of interventions on stage of mammography adoption. J Behav Med. 1995;18:169–87. doi: 10.1007/BF01857868. [DOI] [PubMed] [Google Scholar]
- 35.Champion VL, Ray DW, Heilman DK, Springston JK. A tailored intervention for mammography among low-income African-American women. Journal of Psychosocial Oncology. 2000;18:1–13. [Google Scholar]
- 36.Champion VL, Skinner CS. Differences in perceptions of risk, benefits, and barriers by stage of mammography adoption. J Womens Health. 2003;12:277–86. doi: 10.1089/154099903321667618. [DOI] [PubMed] [Google Scholar]
- 37.King ES, Rimer BK, Seay J, Balshem A, Engstrom PF. Promoting mammography use through progressive interventions: Is it effective? Am J Public Health. 1994;84:104–6. doi: 10.2105/ajph.84.1.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Skinner CS, Arfken CL, Sykes RK. Knowledge, perceptions, and mammography stage of adoption among older urban women. Am J Prev Med. 1998;14:54–63. doi: 10.1016/s0749-3797(97)00008-1. [DOI] [PubMed] [Google Scholar]
- 39.Champion VL. The relationship of selected variables to breast cancer detection behaviors in women 35 and older. Oncol Nurs Forum. 1991;18:733–9. [PubMed] [Google Scholar]
- 40.Vernon SW, Laville EA, Jackson GL. Participation in breast screening programs: a review. Soc Sci Med. 1990;30:1107–18. doi: 10.1016/0277-9536(90)90297-6. [DOI] [PubMed] [Google Scholar]
- 41.Schechter C, Vanchieri CF, Crofton C. Evaluating women's attitudes and perceptions in developing mammography promotion messages. Public Health Rep. 1990;105:253–7. [PMC free article] [PubMed] [Google Scholar]
- 42.Lierman LM, Kasprzyk D, Benoliel JQ. Understanding adherence to breast self-examination in older women. West J Nurs Res. 1991;13:46–66. doi: 10.1177/019394599101300104. [DOI] [PubMed] [Google Scholar]
- 43.Rimer BK, Davis SW, Engstrom PF, Myers RE, Rosan JR. Some reasons for compliance and noncompliance in a health maintenance organization breast cancer screening program. Compliance Health Care. 1988;3:103–14. [PubMed] [Google Scholar]
- 44.Taplin SH, Montano DE. Attitudes, age, and participation in mammographic screening: a prospective analysis. J Am Board Fam Pract. 1993;6:13–23. [PubMed] [Google Scholar]
- 45.Rimer BK, Halabi S, Sugg Skinner C, et al. Effects of a mammography decision-making intervention at 12 and 24 months. Am J Prev Med. 2002;22:247–57. doi: 10.1016/s0749-3797(02)00417-8. [DOI] [PubMed] [Google Scholar]
- 46.Champion VL, Springston JK, Zollinger TW, et al. Comparison of three interventions to increase mammography screening in low income African American women. Cancer Detect Prev. 2006;30:535–44. doi: 10.1016/j.cdp.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 47.Avis NE, Smith KW, Link CL, Goldman MB. Increasing mammography screening among women over age 50 with a videotape intervention. Prev Med. 2004;39:498–506. doi: 10.1016/j.ypmed.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 48.Champion VL, Springston JK, Zollinger TW, et al. Comparison of three interventions to increase mammography screening in low income African American women. Cancer Detect Prev. 2006;30:535–44. doi: 10.1016/j.cdp.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 49.Skinner CS, Strecher VJ, Hospers H. Physicians' recommendations for mammography: do tailored messages make a difference? Am J Public Health. 1994;84:43–9. doi: 10.2105/ajph.84.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Irvin VL, Kaplan RM. Screening mammography & breast cancer mortality: meta-analysis of quasi-experimental studies. PloS one. 2014;9:e98105. doi: 10.1371/journal.pone.0098105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jensen JD, King AJ, Carcioppolo N, Davis L. Why are Tailored Messages More Effective? A Multiple Mediation Analysis of a Breast Cancer Screening Intervention Journal of Communication. 2012;62:851–68. doi: 10.1111/j.1460-2466.2012.01668.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kreuter MW, Holmes K, Alcaraz K, et al. Comparing narrative and informational videos to increase mammography in low-income African American women. Patient Educ Couns. 2010;81:S6–14. doi: 10.1016/j.pec.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]