Abstract
Objective:
The aim of this research was to assess the effect of mouth rinses with and without alcohol on the hardness of dental nano-filled composite.
Methods:
The micro-hardness of fifty circular disk shaped specimens of 7 mm x 2 mm were measured after 14 days. Specimens were immersed into alcohol containing (Listerine and Colgate Perioguard) and alcohol-free (Prodent and Sensodyne Oral antiseptic) mouth rinse solutions. Artificial saliva served as the control. Vickers Micro-hardness was measured with a 30gram load for 30 seconds dwell time by using a diamond indenter. Significant differences were represented by p<0.05, whereas highly significant difference represented by p<0.01. The level of significance (p) was calculated with the help of repeated measure ANOVA. For multiple comparisons, Tukey’s multiple comparison test was used.
Results:
Statistical analysis revealed highly significant difference between specimens immersed in artificial saliva (control) and Listerine (p<0.01). Whereas significant difference were observed between control and Colgate Periogard (p<0.05). However, no significant difference was observed on comparing Prodent and Sensodyne Oral antiseptic mouth rinses with control group(p>0.05). Control specimens depicted highest value of micro-hardness(60.5746 ± 3.2703) compared to the lowest value seen in specimens immersed in Listerine solvent(54.4687 ± 1.0937).
Conclusion:
Alcohol containing mouth rinsing solutions have more deleterious effect on hardness of nano composites as compared to alcohol-free mouth rinses.
KEY WORDS: Hardness, Microscopy, Mouth rinses, Nano-filled composite
INTRODUCTION
Dental composite is a material of choice for direct restorations.1,2 The chemical action of organic solvents associated with lack of good mechanical and physical properties which makes it liable to suffer from dissolution and degradation in the oral cavity. This leads to surface roughness and decreased hardness of the material.1
Although the initial hardness of the polymerized composite material is sufficient to withstand the masticatory load yet the degradation process that initiates immediately in the oral cavity make the composite material vulnerable to dissolution followed by disintegration. The deterioration of a composite material is an intricate process dependent on the filler quantity, matrix type and the coupling agent used in the material. The action of food and organic solvents, water uptake by the matrix3, thermal changes, mechanical cycling and the characteristics of the oral cavity are some of the factors that influence surface degradation, crack propagation and hardness of the material.4 The surface integrity of composite material is directly related to clinical longevity of the composite material.5,6
In recent years, the use of mouth rinses has increased tremendously to thwart action against plaque, caries and periodontal diseases.7 It is an effective method for oral hygiene maintenance.8 These mouth rinses contain water, antimicrobial agents, detergents, emulsifiers and organic acids and in some cases alcohol.9 Changing the concentration of these substances alter the oral pH.10 Studies have shown influence of alcohol containing mouth rinses on the surface roughness and hardness of the composites.8,10,11 On the contrary there are studies claiming to have no adverse effect of alcohol mouth rinses on the hardness of the composite material12 and assert that micro hardness value depends on the material itself rather than the rinsing solutions used.11
Surface hardness is an important physical property which correlates well with the mechanical properties such as abrasion resistance and compressive strength of the material.13 It is assumed that clinical longevity and aesthetic of the restoration is very much dependent on this property.13 Therefore our objective of the study was to investigate the effect of commonly available mouth rinses on the surface hardness of the nano-filled composite material.
METHODS
The composite resin used for preparing 50 circular disk shaped specimens of 7 mm x 2 mm thickness each was Te- Econom Plus (IvoclarVivadent, UK). Teflon mold was used in fabricating the specimens. Mylar strip (Dentart, Polidental, Sao Paulo, Brazil) having dimensions of 10 × 120 × 0.05 mm was placed over the top and bottom of the mold and pressed from top with a microscope slide 22 × 22 mm (BDH borosilicate glass) to form a flat surface of the specimen. Light curing unit Quartz Tungsten Halogen (401™ Demetron Research Corporation, Danbury, CT, USA) with light intensity of 550 W/cm2 was held rigidly and placed 1.0 mm over the glass slide for 40 seconds to polymerize the specimens. Sof-Lex (3M ESPE, USA)and Sof-Lex discs were used to polish specimens to get a clinical finish. These fabricated specimens were placed in distilled water for 24 hours for post irradiation hardness. After 24 hours specimens were dried with absorbing paper and ready for immersion into the control and experimental solutions.
Specimens were randomly divided into five groups. Each group containing 10 specimens (n=10). The active ingredients of the control are displayed in Table-I and the experimental groups are displayed in Table-II with their respective pH. The specimens were immersed in 10 ml of respective solutions. The specimens of group 1 (control) were stored in artificial salivaat 37±3°C in an incubator (Sanfa DNP-9052, China) for 14 days. Likewise, specimens of group 2 were stored in Listerine (alcohol containing); group 3 in Colgate Periogard (alcohol containing); group 4in Prodent (alcohol free); and group 5 in Sensodyne Oral Antiseptic (alcohol free)respectively.
Table-I.
Showing different ingredients of Artificial Saliva along with pH
| S. No. | Solvent | Ingredients | pH |
|---|---|---|---|
| 1 | Artificial Saliva | Sodium chloride (NaCl) 0.400 g; Potassium chloride (KCl) 0.400 g; Calcium chloride monohydrate (CaCl2H2O) 0.795g; Sodium dihydrogen phosphate (NaH2PO4) 0.69 g; Disodium sulphide hydrate (Na2Sx9H20) 0.005 g; Urea 1.0 g | 6.9 |
Table-II.
Showing the active components of different mouth rinsing solutions with their pH andalcoholic content.
| Mouth rinse | Manufacturer | Components | Indications/Treatment | pH | Alcohol Content |
|---|---|---|---|---|---|
| Listerine | Johnson & Johnson Instrustiral Ltd., Soa Paulo, Brazil | Eucalyptol 0.092%, Menthol 0.042%, Methyl Salicylate 0.060, Thymol 0.064%, Water, Sorbitol, Alcohol, Poloxamer 407, Flavor, Benzoic acid, Stem extract, Sodium Benzoate | Antiplaque, Mild Anti gingivitis effect. | 4.3 | 21.6% |
| Colgate Periogard | Colgate Palmolive Industria e ComercioLtda, Soa Paulo, Brazil | 0.12% Chlorhexidinegluconate,Water, Alcohol, Glycerin, PEG-40 sorbitandiisostearate, flavor, Sodium saccharin. | Antimicrobial, Anti fungal, Broad spectrum antiseptic, Bactericidal against Gram +ve and Gram –ve, Denture stomatitis. | 5.6 | 11.6% |
| Prodent | Platinum PhamaceuticalsPvt Ltd, Pakistan | Potassium nitrate 1% | Dentinal hypersentivity, Anti inflammatory and bleeding gums. | 6.2 | Alcohol free |
| Sensodyne Oral antiseptic | Glaxo Smith Kline, Rio de Janeiro, Brasil | Cetylpyridinium chloride 0.05%, Sodium fluoride 226 ppm F, Water, Glycerine, Sorbitol 70%, Poloxamer 338, PEG-60, Hydrogenated castor oil, Sodium benzoate, Flavouring, Methylparaben, Sodium saccharin, Sodium Phosphate, Disodium Phosphate | Antiplaque, Sensitive teeth, Halitosis. | 6.1 | Alcohol free |
Scanning Electron Microscopy (SEM) Analysis
Surface changes were observed using the scanning electron microscopy (SEM) at 20 kV accelerating voltage. The specimens were mounted on aluminum stubs, sputter-coated with gold and examined with a scanning electronic microscope (JEOL-JSM; 6460LV, Tokyo, Japan).
Vickers Micro-hardness Test
Micro-hardness was measured for all the 50 specimens by using a 50gram load for 30 seconds dwell time. A square base pyramid shaped diamond micro indenter of136° was used. Each specimen was indented 3 times at different places and a mean value was obtained for each disk. Micro-hardness values of the specimens were recorded using Vickers micro hardness tester (MMT – X7 Matsuzuwa, Japan).
Statistical Analysis
Data was entered in Statistical Package for Social Sciences (SPSS) version 19. Descriptive analysis was executed in the form of mean ± standard deviation for surface micro-hardness. p<0.05 were considered to be significant. Significant differences were represented by p<0.05, whereas highly significant difference represented by p<0.01. The level of significance (p) was calculated with the help of repeated measure ANOVA. For multiple comparisons, Tukey’s multiple comparison test was used.
RESULTS
Statistical analysis of the data revealed highly significant difference (p<0.01) between the control and Listerine group while a significant difference was observed when control was compared to Colgate Periogard. However, no significant differences were observed on comparing Prodent and Sensodyne Oral antiseptic with control. Control specimens demonstrated highest value of micro-hardness, however, on the other hand specimens immersed in the Listerine solution were found to have the lowest micro-hardness values. Furthermore, Colgate Periogard demonstrated a reduction in micro-hardness which was also significant from control. Whereas, no significant change was observed for specimens in Prodent or in Sensodyne Oral Antiseptic solutions. Actual p values of treatment versus control and mean values of micro hardness test with their respective standard deviations are presented in Table-III.
Table-III.
Showing the mean and standard deviation values of Vickers micro-hardness testing.
| Groups | Immersing Medium | Mean ± SD | p-value |
|---|---|---|---|
| 1 | Artificial Saliva | 60.5746 ± 3.2703 | Control |
| 2 | Listerine | 54.4687 ± 1.0937 | 2.58683E-05 |
| 3 | Colgate Periogard | 58.0366 ±0.53798 | 0.026236797 |
| 4 | Prodent | 60.0057 ± 0.81027 | 0.599905294 |
| 5 | Sensodyne Oral antiseptic | 59.8782 ± 0.90889 | 0.524650214 |
The SEM micrographs examination revealed presence of micro cracks and voids in the specimens of control and experimental groups (Fig.1). A surface alteration can be observed in micrographs (A-C) of control group. The most evident porosity and cracks were observed in the micrographs (D-F) of Listerine group. The results of this study proved that alcohol containing mouth rinses have significant effect on the hardness values.
Fig.1.
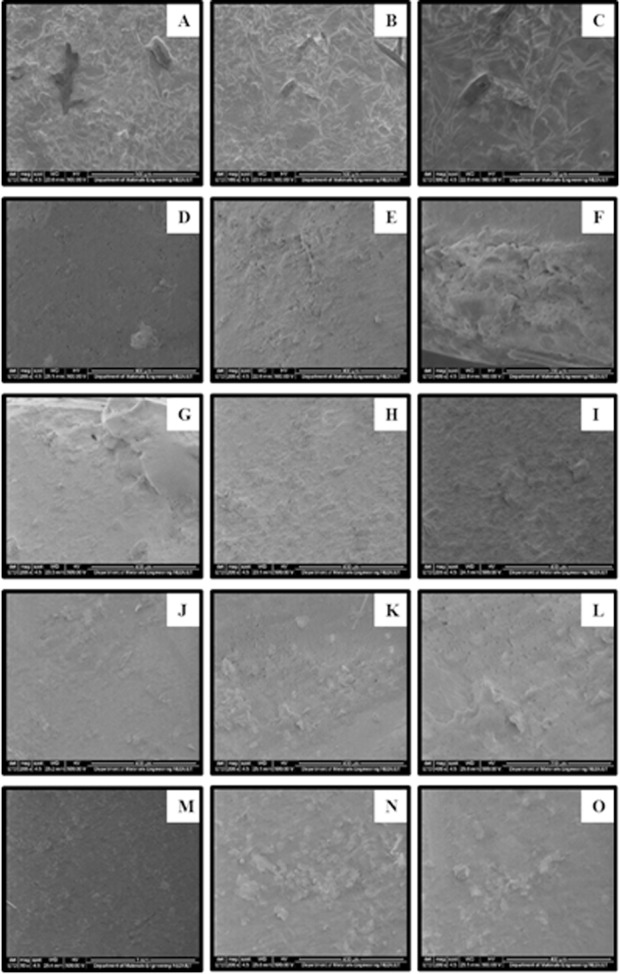
SEM micrographs of nano-filled composite specimens (A-C) specimen immersed in Artificial Saliva at 100 x, 200 x and 300 x respectively, (D-F) specimen immersed in Listerine at 100 x, 200 x and 300 x respectively, (G-I) specimen immersed in Colgate Periogard at 100 x, 200 x and 300 x respectively, (J-L) specimen immersed in Prodent at 100 x, 200 x and 300 x respectively, (M-O) specimen immersed in Sensodyne Oral Antiseptic at 100 x, 200 x and 300 x respectively.
DISCUSSION
The ideal restorative material is the one that functions in the same manner as our natural teeth do under different masticatory loads with changing oral environment. Besides, these materials should closely resemble in appearance with that of the natural teeth.14 The quest for new material with these ideal properties has already begun. Nano-filled composites are the newest addition to the pantheon of composite filling materials; emerged as suitable alternatives to overcome limitations that other types of composites have.15 Nano-filled composites are considered to be the material of choice because of their improved physical and mechanical properties are not found in other types of composites.15 This study involved one of these type of new composite material (Te Econom Plus) to evaluate the micro hardness which is considered an important property for the longevity of the composite material.
To evaluate the effect of alcoholic mouth rinses on the micro hardness of nano composite, this study involved two different commercially available mouth rinses; and their effect on nano composites were compared with alcohol free mouth rinses. The results of this study found that alcohol concentration has a direct influence on one of the physical property ofthe material i.e. hardness (Table-III). The reason could be the low pH of organic solvents like alcohol which have the tendency to damage polymer chain. Alcohol can penetrate into the polymeric chain and thereby causing the release of unreacted monomers.16,17 Alcohol has the affinity to penetrate the polymer chain and damage it in no time. The low pH of alcohol mouth rinses catalysis the ester groups from dimethacrylate monomers present in the composite which leads to destruction of the polymer chain.17 This is followed by hydrolytic degradation of the composite material.12
Continual storage of specimens for 14 days in different mouth rinsing solutions significantly decreased the micro hardness of the composite material in every group. This surface change can be observed with SEM micrographs (Fig 1). Matrix cracking and its propagation in a resin material is attributed to water uptake process. This vicious circle of a composite material starts initially with the swelling of a composite material and leads to interfacial debonding and dislodgment of filler particles over the period of time.18 This hydrolytic degradation mechanism aggravates if fillers have metallic ions present in them.19 The fillers such as barium and zinc are electropositive in nature and have affinity to react with water. Loss of these elements into water perturbs the charge balance of silica network. Silica network reestablishes the charge balance with the penetration of hydrogen ions. This process results into breakage of (Si-O-Si) bonds leading to softening of the composite resin with aging time.19 The results of this study justified this hydrolytic degradation mechanism. The presence of barium fillers in the nano-filled composite we used further testified the results and degradation process in all the groups.
The results of our study are consistent with the previous studies of Miranda et al.10 who found decreased values of micro-hardness due to alcohol presence; Almeida et al.8 who observed severe degradation of nano-filled composite due to mouth rinses; and Jyothi et al.20 work which found significant reduction in mean VHN (Vickers micro hardness number) of specimens immersed in alcohol based mouth rinses. SEM micrographs further validate this effect on the hardness of the nano-filled composites.
Viewing the results of present data confirmed that alcohol containing mouthrinses showed major influence on micro-hardness values when compared with control. The limitation of our study was to create a dynamic oral environment that cannot be exactly and entirely replicated by in vitro laboratory conditions.21 Further studies need to be conducted to access longer exposure times using artificial saliva and other solvents in order to mimic the clinical oral condition. Also other properties such as tensile testing and colour stability may be conducted to provide more specific data about the effects of pH and alcohol concentration of various solvents on esthetic restorative materials.22
CONCLUSION
We can conclude from this in vitro study that:
The surface hardness values of the nano composites are differently affected by the mouth rinse solutions
Degradation was observed in all the specimens during this study.
Alcohol containing mouth rinses showed more reduction in micro hardness values of nano-composite as compared to alcohol free mouth rinses.
ACKNOWLEDGMENTS
We extend sincere appreciation to the Deanship of Scientific Research, King Saud University for funding/supporting this research through Research Group No-IRG 14-31.
Footnotes
Declaration of interest: The authors have no conflict of interest regarding any part in this research.
Source of funding: Mentioned in acknowledgements.
Authors’ contribution
Aftab Ahmed Khan: writing major part of the manuscript, statistical work and proof reading. Adel Zia Siddiqui: Designing of the study, manuscript writing and final references. Syed Fareed Mohsin: Contributed in collecting relevant references and manuscript writing. Abdulaziz A. Al Kheraif: Critical review and final editing of manuscript.
REFERENCES
- 1.Yanikoğlu N, Duymuş ZY, Yilmaz B. Effects of different solutions on the surface hardness of composite resin materials. Dent Mater J. 2009;28:344–351. [PubMed] [Google Scholar]
- 2.Tabatabaei SH, Sabaghi A. The effect of three mouthwashes on micro leakage of a composite resin-An in vitro study. J Am Sci. 2013;9:13–19. [Google Scholar]
- 3.da Silva EM, Almeida GS, Poskus LT, Guimaraes JG. Relationship between the degree of conversion, solubility and salivary sorption of a hybrid and a nanofilled resin composite: Influence of the light-activation mode. J Appl Oral Sci. 2008;16:161–166. doi: 10.1590/S1678-77572008000200015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beun S, Glorieux T, Devaux J, Vreven J, Leloup G. Characterization of nanofilled compared to universal and microfilled composites. Dent Mater. 2007;23:51–59. doi: 10.1016/j.dental.2005.12.003. doi: 10.1016/j.dental.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Ilie N, Hickel R. Resin composite restorative materials. Aus Dent J. 2011;56(Suppl1):59–66. doi: 10.1111/j.1834-7819.2010.01296.x. doi: 10.1111/j.1834-7819.2010.01296.x. [DOI] [PubMed] [Google Scholar]
- 6.Hamouda IM. Effects of various beverages on hardness, roughness, and solubility of esthetic restorative materials. J EsthetRestor Dent. 2011;23:315–322. doi: 10.1111/j.1708-8240.2011.00453.x. doi: 10.1111/j.1708-8240.2011.00453.x. [DOI] [PubMed] [Google Scholar]
- 7.Feres M, Gursky LC, Faveri M, Tsuzuki CO, Figueiredo LC. Clinical and microbiological benefits of strict supragingival plaque control as part of the active phase of periodontal therapy. J ClinPeriodontol. 2009;36:857–867. doi: 10.1111/j.1600-051X.2009.01471.x. doi: 10.1111/j.1600-051X.2009.01471.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Almeida GS, Poskus LT, Guimarães JG, da Silva EM. The effect of mouthrinses on salivary sorption, solubility and surface degradation of a nanofilled and a hybrid resin composite. Oper Dent. 2010;35:105–111. doi: 10.2341/09-080-L. doi: 10.2341/09-080-L. [DOI] [PubMed] [Google Scholar]
- 9.Colucci V, Dos Santos CD, Do Amaral FL, Corona SA, Catirse AB. Influence of NaHCO3 powder on translucency of microfilled composite resin immersed in different mouthrinses. J EsthetRestor Dent. 2009;21:242–248. doi: 10.1111/j.1708-8240.2009.00269.x. doi: 10.1111/j.1708-8240.2009.00269.x. [DOI] [PubMed] [Google Scholar]
- 10.Miranda DA, Bertoldo CES, Aguiar FHB, Lima DANL, Lovadino JR. Effects of mouthrinse on Knoop hardness and surface roughness of dental composites after different immersion times. Brazilian Oral Res. 2011;25:168–173. doi: 10.1590/s1806-83242011000200012. [DOI] [PubMed] [Google Scholar]
- 11.Festuccia MSCC, Garcia LFR, Cruvinel DR, Pires-de-Souza FCP. Color stability, surface roughness and microhardness of composites submitted to mouthrinsing action. JAppl Oral Sci. 2012;20:200–205. doi: 10.1590/S1678-77572012000200013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Moraes Porto IC, das Neves LE, de Souza CK, Parolia A, Barbosa dos Santos N. A comparative effect of mouthwashes with different alcohol concentrations on surface hardness, sorption and solubility of composite resins. Oral Health Dent Manag. 2014;13:502–506. [PubMed] [Google Scholar]
- 13.Erdemir U, Yildiz E, Eren MM, Ozel S. Surface hardness evaluation of different composite resin materials: influence of sports and energy drinks immersion after a short-term period. J Appl Oral Sci. 2013;21:124–131. doi: 10.1590/1678-7757201302185. doi: 10.1590/1678-7757201302185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Palaniappan S, Bharadwaj D, Mattar DL, Peumans M, Van Meerbeek B, Lambrechts P. Three-year randomized clinical trial to evaluate the clinical performance and wear ofa nanocomposite versus a hybrid composite. Dent Mater. 2009;25:1302–1314. doi: 10.1016/j.dental.2009.06.001. doi: 10.1016/j.dental.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Camargo PHC, Satyanarayana KG, Wypych F. Nanocomposites: Synthesis, structure, properties and new application opportunities. Mat Res. 2009;12:1–39. doi: 10.1590/S1516-14392009000100002. [Google Scholar]
- 16.Sarret DC, Coletti DP, Peluso AR. The effects of alcoholic beverages on composite wear. Dental Materials. 2000;16:62–67. doi: 10.1016/s0109-5641(99)00088-3. [DOI] [PubMed] [Google Scholar]
- 17.Rehman A, Amin F, Abbas M. Diametral tensile strength of two dental composites when immersed in ethanol, distilled water and artificial saliva. J Pak Med Assoc. 2014;64(11):1250–1254. [PubMed] [Google Scholar]
- 18.abo el Naga A, Yousef M. Evaluation of Different Restorative Materials after Exposure to Chlorhexidine. J Am Sci. 2012;8:628–631. [Google Scholar]
- 19.Martos J, Osinaga PWR, Oliveira E, Castro LAS. Hydrolytic degradation of composite resins: effects on the microhardness. Mater Res. 2003;6:599–604. doi: 10.1590/S1516-14392003000400029. [Google Scholar]
- 20.Jyothi K, Crasta S, Venugopal P. Effect of five commercial mouth rinses on the microhardness of a nanofilled resin composite restorative material: An in vitro study. JConservDent. 2012;15:214–217. doi: 10.4103/0972-0707.97938. doi: 10.4103/0972-0707.97938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanan SM, Mohammed AK. The effect of mouth rinses on surface micro hardness of two esthetic restorative materials. Iraqi National JNursSpecialities. 2012;25:101–108. [Google Scholar]
- 22.Urbano CD, Abrahao ALS, Lancellotti AC, Menezes-Oliveira MAHD, Calabrez S, Goncalves LDS. Effect of mouthrinses on the surface roughness of nano-filled composite. Braz Dent Sci. 2014;17:92–97. [Google Scholar]


