Abstract
Aim
Periodic leg movements in sleep (PLMS) are generally evaluated by the number of events per hour during sleep, but this is an unstable measure with marked nightly variability and also fails to assess the basic periodicity that essentially characterizes these movements. The inter-movement interval (IMI) evaluates a putative biological process producing the period of PLMS. By contrast, the actual number of PLMS reflects the expression of this biological process that would likely be affected by multiple factors, particularly those disrupting sleep. Thus, this study tests the hypothesis that measurement of IMI duration should be more stable over nights in comparison to any measure based on counting the number of movements. IMI approximates a log-normal distribution. This study, therefore, tests the hypothesis that the means of the log IMI are more stable from night 1 (N1) to night 2 (N2) sleep recordings compared with measures of the number of PLMS.
Methods
PLMS/h and IMI were measured for two consecutive nights of full sleep recordings for 29 restless legs syndrome (RLS) patients not being treated and 22 healthy controls without RLS. N1–N2 difference between nights was measured as percent of average for the nights.
Results
Mean log IMI showed little nightly variability (mean ± SD for RLS: 3.6% ± 3.7, controls: 7.1% ± 7.0) significantly less p < 0.001) in comparison to PLMS/h (mean ± SD for RLS: 43.2 ± 37.1, controls: 63.7 ± 40.8). The IMI nightly variability was also significantly better than that for the periodicity index. IMI also varied considerably between individuals.
Conclusion
Mean log IMI is a remarkably stable measure across nights within a subject and shows differences between subjects that may have clinical and biological significance. Because of this consistency, the mean log IMI should be considered as one standard measure of PLMS alongside the PLMS index.
1. Introduction
Periodic leg movements in sleep (PLMS) are a consistently observed phenomenon in restless legs syndrome (RLS) [1] that also occur in adults with increasing age [2] and for some other disorders, for example, narcolepsy [3]. The customary primary measure of PLMS is the number of periodic leg movements (PLM) per hour of sleep (PLMS/h), often referred to as PLMS index (PLMSI). The periodic limb movements (PLM) during wake are also often reported as number per hour of wake time (PLMW/h) during the recording period. Large variability in these measures within patients and between nights, however, significantly compromises clinical utility of these measures [4], particularly in patients with RLS [5] Thus, the PLMSI from a sleep study cannot be considered a reliable measure, particularly if it is taken from the first night's recording, as is commonly done in clinical practice.
The search for better and more stable measurements of PLMS has been greatly advanced by Ferri's work emphasizing the time between onsets of consecutive movements referred to as the inter-movement interval (IMI). He introduced the periodicity index (PI) as the proportion of all IMI that are periodic, that is, three or more consecutive IMI that are each ≥10 and ≤90 s [6]. By shifting focus away from number of movements, he has reframed the measurement of PLMS in terms of the periodicity of the events, and suggested that, in order to understand the biology of PLMS, research should focus on accurately identifying ture PLMS and assessing their periodicity and occurrence relative to other leg movements.
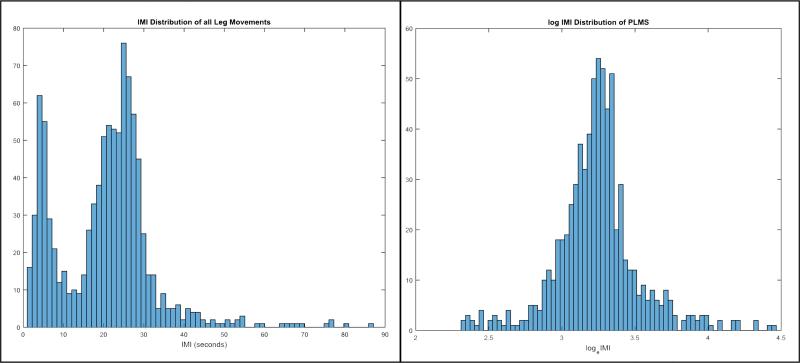
IMI is itself of particular interest for measuring PLMS because it represents the inherent period of an underlying biology producing these repetitive movements. The PLMS biology producing these often remarkably patterned movements presumably differs between individuals possibly reflecting disease state but would likely be relatively stable over short periods of time when there are no significant biological changes. IMI may, therefore, reflect a significant property of a putatively stable biological process producing the PLMS, while the actual number of PLM, in contrast, may reflect factors that affect expression of this underlying biological process. If IMI reveals the inherent periodicity of a biological process, then it should be reasonably stable over several nights while, in contrast, any measure based on counting the number of PLM (e.g., PLMS/h) or IMI (e.g., PI) may vary considerably depending on factors affecting expression of these periodic events, for example, noise or novel environment disrupting sleep. As IMI of PLMS (defined to range from 5 to 90 s) shows a unimodal strongly right-skewed distribution approximating a lognormal [7], the central tendency and variance would be best Q4 measured by the mean and standard deviation of the log IMI (see Fig. 1).
Fig. 1.
IMI distribution from a single patient. On the left side, all IMI are displayed, regardless of whether they take place during a PLMS run. Notice the two distinct peaks, which have been noted elsewhere by Ferri [7] as comprising two distinct lognormal distributions, separated by a dip at 10 s. The graph on the right is, firstly, a distribution of only IMI occurring in runs of PLMS, with a minimum IMI of 10 s, to isolate the second peak. Secondly, it is displayed on a logarithmic scale to better illustrate the near-normal distribution of IMI when expressed logarithmically.
The two aims of this study were (1) to test the hypothesis that average variability from the first to the second night would be significantly less for mean log IMI in comparison to either PLMS/h or PI, and (2) to explore the first to second night variability of IMI compared with another commonly reported feature of PLM, that is, duration of PLMS.
2. Methods
2.1. Subjects
Data from two consecutive nights of standard polysomnogram (PSG) recordings conducted on 37 RLS and 30 control subjects, who were participating in an ongoing RLS study, that had been approved by the Hopkins Institutional Review Board for research involving human subjects, were available for analysis. The PSG recordings and sleep stage scoring followed the standards set by the American Academy of Sleep Medicine with bilateral anterior tibialis muscle electromyogram (EMG) recordings on a separate channel for each leg [8]. Full respiratory measures including oximetry, nasal and oral air pressure, and thoracic and abdominal respiratory effort were obtained on the first night recording only. Subjects who had apnea/hypopneas with desaturations ≥4% on the first night of PSG, occurring more often in comparison to 15/h during sleep, were excluded. Using the clinical version of the validated Hopkins Telephone Diagnostic Interview for RLS, an RLS expert diagnosed the subjects as having RLS or non-RLS through a clinical interview [9]. All RLS subjects who were on medications for their disease stopped RLS medications for at least 12 days before the first night sleep study. RLS patients had been screened to include only those with an average PLMS index >15/h over 5 days of home recording with the PAM-RL activity meter [10]. Conversely, control subjects were included only if they had an average PLMS index <10/h for 5 consecutive days, recorded the same as the RLS subjects. Besides RLS, both control and RLS subjects were clinically screened to exclude those with significant mental health or sleep disorders.
Subjects were excluded by visual analyses of the PSG if the data from any time during either N1 or N2 from either leg showed high levels of EMG noise or unstable thresholds clearly indicating loss of recording integrity. Subjects were excluded prior to the data analyses for this study, thus excluding eight RLS patients and eight controls leaving 51 (29 RLS, 22 control) subjects included in this study.
2.2. Scoring of PLM
PSG data were extracted from REMLOGIC European data format into MATLAB data structure, to be scored by the validated MATPLM1 auto-detection program (sensitivity: 95.3%, specificity: 91.7%) [11]. MATPLM1 strictly applies World Association of Sleep Medicine (WASM) criteria in order to score periodic leg movements (PLMs). The automatic scoring was visually inspected and records with significant recording problems, for example, noise, electrocardiogram (EKG) artifact, were rejected before data analyses.
2.3. PLMS features and variability measures
The MATPLM1 program was used to calculate PLM index, IMI, and PLM durations for all of sleep and separately for each sleep stage using the WASM criteria [11]. PI is defined for IMI in sleep as the number in a series of at least 3 with IMI ≥10 and ≤90 s divided by the total number of IMI in sleep. For the results in the body of this paper, PLMS must have an IMI ≥5 s and ≤90 s, but recent research has indicated that PLMS may be better characterized by an IMI minimum of 10 s [6], and so results from PLMS so calculated are included in supplementary tables (Tables S1 and S2 available online). Except for the PI, the PLMS sequences are defined ignoring IMI <minimum.
N1–N2 variability for each measure was calculated for each subject by dividing the absolute N1–N2 difference by the mean of the two nights and multiplying this number by 100 to return a percentage.
2.4. Statistics
Variability of the different measures was compared using a two-sided Wilcoxon signed-rank test. To test the primary hypothesis, the percentage variability for mean log IMI was compared with PLMS/h and PI. Hierarchical testing was used. The statistical tests of the percentage variability were made in the following order: mean log IMI versus PLMS/h, mean log IMI versus PI. Statistical significance was set at p < 0.05 for each step in the evaluation. Testing continued in this order until statistical significance was not established or all tests had been used. Controls and RLS patients were tested separately.
3. Results
3.1. Subjects
Data were analyzed for 29 RLS (average age: 58.8 ± 9.4, 59% female) and 22 control (average age: 59.5 ± 8.9, 64% female) subjects. The average (±SD) severity of RLS as measured by the International RLS Severity Scale [12], when patients were off treatment for at least 11 days, was 25.8 ± 5.6 (range 16–39).
3.2. PLMS features and N1–N2 variability
The N2 average values of PLMS features for RLS patients and controls are presented in Table 1 to describe the PLM features of these subjects for sleep, wake during sleep period, and each sleep stage. Table 2 similarly presents the average percentage N1–N2 error for the PLM features for sleep, wake, and each sleep stage.
Table 1.
Average ± SD of the PLMS features from RLS patients and controls for wake during sleep period, sleep, and each stage of sleep, collected from Night 2 of recording.
| Wake | Sleep | REM | S1 | S2 | S3 | |
|---|---|---|---|---|---|---|
| RLS (n = 29) | ||||||
| PLM Index | 89.92 (44.80) | 96.55 (63.62) | 88 80 (70 20) | 103.52 (71.12) | 103.26 (68.65) | 73.14 (60.23) |
| Mean IMI | 21.79 (4.52) | 25.28 (6.91) | 26.60 (8.59) | 24.17 (7.22) | 26.17 (7.73) | 29.66 (12.49) |
| Median IMI | 16.76 (4.59) | 23.15 (7.49) | 21.32 (8.52) | 22.16 (7.96) | 24.26 (7.82) | 28.33 (12.72) |
| Mean log IMI | 2.80 (0.20) | 3.06 (0.28) | 3.04 (0.32) | 3.00 (0.32) | 3.11 (0.31) | 3.25 (0.37) |
| Mode log IMI | 1.87 (0.47) | 2.51 (0.54) | 2.09 (0.47) | 2.13 (0.62) | 2.49 (0.64) | 2.64 (0.75) |
| STD log IMI | 0.71 (0.11) | 0.52 (0.11) | 0.62 (0.10) | 0.55 (0.16) | 0.48 (0.14) | 0.41 (0.19) |
| Mean duration | 3.25 (0.69) | 2.85 (0.69) | 2.15 (0.58) | 2.76 (0.86) | 3.03 (0.71) | 2.92 (0.99) |
| Median duration | 2.77 (0.82) | 2.75 (0.88) | 1.88 (0.62) | 2.64 (0.90) | 2.91 (0.92) | 2.86 (1.09) |
| Control (n = 22) | ||||||
| PLM Index | 36.61 (24.67) | 7.85 (7.51) | 19.10 (15.25) | 17.14 (15.08) | 5.38 (5.87) | 3.46 (3.92) |
| Mean IMI | 24.37 (5.40) | 34.86 (9.20) | 32.52 (10.24) | 41.72 (16.23) | 43.29 (15.03) | 19.00 (8.61) |
| Median IMI | 17.42 (6.89) | 29.96 (13.17) | 25.98 (13.26) | 38.77 (17.95) | 41.26 (17.64) | 14.96 (10.15) |
| Mean log IMI | 2.86 (0.24) | 3.25 (0.35) | 3.16 (0.38) | 3.49 (0.50) | 3.52 (0.46) | 2.68 (0.50) |
| Mode log IMI | 1.73 (0.13) | 1.86 (0.44) | 1.90 (0.58) | 2.81 (0.91) | 2.34 (0.91) | 2.04 (0.80) |
| STD log IMI | 0.79 (0.11) | 0.78 (0.10) | 0.83 (0.10) | 0.70 (0.17) | 0.71 (0.13) | 0.73 (0.18) |
| Mean duration | 3.06 (0.69) | 1.81 (0.58) | 1.63 (0.41) | 1.90 (1.21) | 1.77 (0.80) | 1.80 (0.90) |
| Median duration | 2.33 (0.96) | 1.35 (0.68) | 1.17 (0.36) | 1.66 (1.25) | 1.35 (0.77) | 1.55 (0.97) |
Table 2.
Average ± SD of percentage variability* from N1 to N2 of PLMS features from RLS patients and controls for wake during sleep period, sleep, and each stage of sleep.
| Wake | Sleep | REM | S1 | S2 | S3 | |
|---|---|---|---|---|---|---|
| RLS (n = 29) | ||||||
| PLM Index | 32.64 (28.07) | 44.01 (36.88) | 51.16 (47.72) | 53.74 (48.70) | 45.08 (45.99) | 101.64 (67.42) |
| Mean IMI | 12.92 (l0.52) | 12.65 (12.39) | 16.41 (20.60) | 22.16 (21.82) | 13.11 (12.11) | 32 34 (28 67) |
| Median IMI | 16.26 (l5.00) | 13.00 (15.81) | 26.03 (24.12) | 24.90 (23.44) | 12.52 (15.50) | 36.51 (32.34) |
| Mean log IMI | 4.31 (3.64) | 4.13 (4.45) | 6.16 (6.99) | 8.38 (7.32) | 4.27 (4.66) | 10.71 (9.75) |
| Mode log IMI | 19.69 (19.14) | 20.63 (20.65) | 23.77 (15.48) | 19.42 (16.41) | 28.63 (23.76) | 21.18 (19.05) |
| STD log IMI | 10.55 (8.48) | 13.50 (7.89) | 17.20 (16.77) | 23.23 (16.65) | 17.87 (11.54) | 33.60 (19.64) |
| Mean duration | 11.09 (17.56) | 16.57 (18.12) | 22.94 (16.96) | 15.73 (10.72) | 16.23 (21.82) | 23.68 (22.27) |
| Median duration | 16.47 (25.68) | 19.17 (20.66) | 20.07 (17.49) | 21.18 (22.87) | 14.77 (18.66) | 29.85 (28.95) |
| Control (n = 22) | ||||||
| PLM Index | 64.79 (42.29) | 59.37 (41.53) | 57.56 (38.77) | 66.59 (45.46) | 73.35 (56.71) | 62.91 (43.87) |
| Mean IMI | 23.85 (15.86) | 21.61 (20.77) | 19.09 (13.49) | 37.54 (35.62) | 29.91 (33.37) | 58.29 (26.47) |
| Median IMI | 37.52 (27.25) | 42.07 (36.43) | 36.61 (27.25) | 54.47 (43.42) | 42.87 (39.47) | 74.11 (22.55) |
| Mean log IMI | 9.73 (6.23) | 8.82 (8.81) | 6.16 (5.60) | 12.81 (12.10) | 10.97 (11.71) | 21.71 (7.84) |
| Mode log IMI | 8.14 (9.55) | 7.74 (7.43) | 7.43 (6.07) | 23.62 (25.52) | 18.25 (20.97) | 22.64 (24.26) |
| STD log IMI | 9.94 (7.63) | 12.15 (14.00) | 12.02 (11.97) | 58.35 (47.19) | 24.31 (28.63) | 28.67 (4.25) |
| Mean duration | 16.33 (15.46) | 20.73 (14.07) | 22.67 (15.77) | 22.74 (17.59) | 40.03 (29.94) | 27.23 (10.13) |
| Median duration | 32.63 (22.00) | 17.79 (12.72) | 24.05 (12.91) | 37.42 (25.38) | 32.40 (29.38) | 16.73 (15.78) |
Percentage variability = absolute difference N1–N2/average of N1, N2.
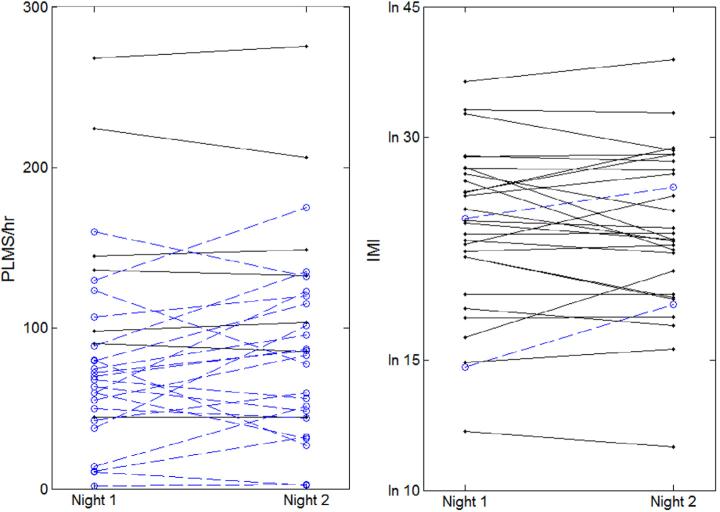
Table 3 displays the average values for Night 2, the N1–N2 percent error, and the results of the Wilcoxon test comparing each metric's error to that of the log IMI. Each step of the hierarchical testing was statistically significant, revealing that mean log IMI varies significantly less than PLMS index and PI. Fig. 2 illustrates the relatively high N1–N2 variability for PLMS index and PI compared with log IMI.
Table 3.
Hierarchical statistical analyses* of IMI compared with PLMS/h and PI.
| Night 2 Values | % Error Night 1–Night 2 | p, vs. Mean log IMI | |
|---|---|---|---|
| RLS (n = 29) | |||
| PLMS Index | 96.55 (63.62) | 44.01 (36.88) | 0.0000063 |
| PI | 0.67 (0.23) | 24.25 (32.45) | 0.00015 |
| mean log IMI | 3.06 (0.29) | 4.11 (4.54) | |
| Control (n = 22) | |||
| PLMS Index | 7.85 (7.51) | 59.37 (41.53) | 0.00042 |
| PI | 0.21 (0.13) | 52.22 (49.16) | 0.0010 |
| mean log IMI | 3.25 (0.35) | 8.82 (8.81) |
Logs are for natural log with base e.
All statistical tests showed significant differences for p < 0.05, by Wilcoxon sign-rank test.
Fig. 2.
N1 to N2 values for each RLS patient. These are presented with lines connecting data from the same subject on each night. The dotted lines indicate changes from N1 to N2 that are >10% of the average of the two nights. The data presented are for PLMS/h in the left panel and mean log IMI in the right panel.
Exploratory analyses revealed several potentially relevant differences. N1–N2 variability for all types of sleep for RLS patients and controls showed overall least variability for both mean log IMI (4.1% and 8.8%, respectively), standard deviation of log IMI (12.1% and 13.5%), and mean linear IMI (12.7 and 21.6%). Duration variability can be compared with linear IMI for all sleep and across all sleep stages (Wilcoxon tests show no statistically significant differences), but has greater variability than that of log IMI. The percentage error of PI was not significantly less than PLMS/h in RLS patients (mean ± SD, respectively: 24.3 ± 32.5 and 44.0 ± 36.9, p > 0.06), nor controls (respectively: 52.2 ± 49.2 and 59.4 ± 41.5, p > 0.64). Sleep stage effects were observed for mean and standard deviation log IMI with slightly shorter means (7%) but much larger standard deviations (42%) for RLS patients in wake, rapid eye movement (REM), and stage 1 in comparison to stage 2 or 3 sleep.
A similar pattern was observed for controls except for stage 3 sleep. The percentage error for log IMI was also less for stage 2 sleep in comparison to the other sleep stages for RLS patients but not for controls.
The results using the PLMS criterion of ≥10 rather than 5 s minimum IMI showed the same effects with the stability between nights being generally marginally better (see Tables S1 and S2 in online supplement).
4. Discussion
This study supports what is already well known about the instability of PLMS/h between two nights. The log IMI shows remarkably low variability between nights, in both RLS patients and controls. This supports our hypothesis that the IMI provides a reliable, stable measure of an important feature of PLMS. As IMI has an approximate log normal distribution, the mean provides a relatively unbiased estimate of the period of the process producing the PLMS (see Fig. 1). This period appears stable between nights for a subject but markedly variable across subjects (see Table 1 and Fig. 2). This may provide not only a more stable measure of PLMS but also more importantly a stable endophenotype of the biology producing these periodic events.
Therefore, log IMI is stable for both RLS and control subjects, suggesting that IMI stability is independent of number of events and current disease state. Thus, the defining feature of PLMS, the periodicity of the process producing the movement, can be reliably measured for any person from one night's sleep recording. Measuring IMI is often neglected in sleep studies because of the burden on a visual scorer to track the length of events. However, the significance of IMI in characterizing PLM is such that it warrants the effort to calculate it. At present, there are validated, automated systems available for PLM detection [11,13] that not only significantly reduce technician time for scoring records but also increase accuracy of the scoring and can automatically offer the IMI measurements.
The relation between sleep stages and mean log IMI values in this study are similar to those reported by Nicolas et al. for the mode of linear IMI, that is, shorter for REM and stage 1 compared with stage 2 or SWS [2]. The sleep-stage effect on N1–N2 stability for IMI differs for controls and RLS, with stage 2 providing the most stable measure for RLS patients but not controls (Table 2). This, however, is complicated by the relatively small number of events in specific sleep stages for controls. Furthermore, the standard deviation of the log IMI in a single night shows significant differences across sleep stages in RLS subjects: Particularly, stages 2 and 3 have significantly smaller standard deviations compared with stage 1 and REM sleep. Although more investigation is warranted to find the association between sleep architecture and PLMS, it seems from these initial findings that events during sleep, particularly during stage 1 and REM, disrupt the normal periodic expression, leading to a wider range of IMI times, but not a major change in the inherent period for the individual.
The overall variability of IMI is significantly lower from N1 to N2 compared with other measures of PLMS, particularly PLMS index and periodicity index. This is particularly true of the log IMI measures. The greatest night-to-night variability across multiple nights is generally considered to be that from N1 to N2, thus the stability of mean log IMI can reasonably be assumed to persist for >2 nights. A single night's recording appears sufficient to establish a baseline mean of log IMI of PLMS for a person. Any changes in this measure that appears over time may, therefore, reflect changes in the underlying biological process independent of changes affecting sleep status. Differences between people in their mean log IMI may also have clinical and biological relevance, although this has yet to be investigated.
The stability over nights of mean log IMI is so striking in RLS patients (mean: 4.1%, range 0.5–12%) and in controls with PLMS (mean 8.8%, range 0.3–33%) that it should be considered as a likely major defining feature of PLMS. The measure of the PLMS period (mean log IMI) combined with the measure of the expression of this period (the PLMS index), serve to provide a better characterization of a patient's disease state and current sleep status. These measures may facilitate research into the factors affecting PLMS and the periodicity-driving processes involved.
Supplementary Material
Acknowledgments
This study was supported in part by a grant from the National Institute of Neurological Disorders and Stroke number NS075184. Sleep data acquisition and scoring were provided by The Center for Interdisciplinary Sleep Research and Education (CISRE) at Johns Hopkins University.
Footnotes
Conflict of interest
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: http://dx.doi.org/10.1016/j.sleep.2015.10.004.
Appendix: Supplementary material
Supplementary data to this article can be found online at doi:10.1016/j.sleep.2015.10.004.
References
- 1.Montplaisir J, Boucher S, Poirier G, et al. Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: a study of 133 patients diagnosed with new standard criteria. Mov Disord. 1997;12:61–5. doi: 10.1002/mds.870120111. [DOI] [PubMed] [Google Scholar]
- 2.Nicolas A, Michaud M, Lavigne G, et al. The influence of sex, age and sleep/wake state on characteristics of periodic leg movements in restless legs syndrome patients. Clin Neurophysiol. 1999;110:1168–74. doi: 10.1016/s1388-2457(99)00033-4. [DOI] [PubMed] [Google Scholar]
- 3.Dauvilliers Y, Pennestri MH, Petit D, et al. Periodic leg movements during sleep and wakefulness in narcolepsy. J Sleep Res. 2007;16:333–9. doi: 10.1111/j.1365-2869.2007.00601.x. [DOI] [PubMed] [Google Scholar]
- 4.Sforza E, Haba-Rubio J. Night-to-night variability in periodic leg movements in patients with restless legs syndrome. Sleep Med. 2005;6:259–67. doi: 10.1016/j.sleep.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Hornyak M, Kopasz M, Feige B, et al. Variability of periodic leg movements in various sleep disorders: implications for clinical and pathophysiologic studies. Sleep. 2005;28:331–5. [PubMed] [Google Scholar]
- 6.Ferri R, Fulda S, Manconi M, et al. Night-to-night variability of periodic leg movements during sleep in restless legs syndrome and periodic limb movement disorder: comparison between the periodicity index and the PLMS index. Sleep Med. 2013;14:293–6. doi: 10.1016/j.sleep.2012.08.014. [DOI] [PubMed] [Google Scholar]
- 7.Ferri R, Manconi M, Lanuzza B, et al. Age-related changes in periodic leg movements during sleep in patients with restless legs syndrome. Sleep Med. 2008;9:790–8. doi: 10.1016/j.sleep.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 8.Iber C, Ancoli-Israel S, Chesson A, et al. The AASM manual for the scoring of sleep and associated events. rules, terminology and technical specifications. American Academy of Sleep Med; Westchester, IL: 2007. [Google Scholar]
- 9.Hening WA, Allen RP, Washburn M, et al. Validation of the Hopkins telephone diagnostic interview for restless legs syndrome. Sleep Med. 2008;9:283–9. doi: 10.1016/j.sleep.2007.04.021. [DOI] [PubMed] [Google Scholar]
- 10.Sforza E, Johannes M, Claudio B. The PAM-RL ambulatory device for detection of periodic leg movements: a validation study. Sleep Med. 2005;6:407–13. doi: 10.1016/j.sleep.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Huang AS, Skeba P, Yang MS, et al. MATPLM1, a MATLAB script for scoring of periodic limb movements: preliminary validation with visual scoring. Sleep Med. 2015 doi: 10.1016/j.sleep.2015.03.008. doi:10.1016/j.sleep.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The International Restless Legs Syndrome Study Group Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med. 2003;4:121–32. doi: 10.1016/s1389-9457(02)00258-7. [DOI] [PubMed] [Google Scholar]
- 13.Moore H, Leary E, Lee S-Y, et al. Design and validation of a periodic leg movement detector. PLoS ONE. 2014;9:e114565. doi: 10.1371/journal.pone.0114565. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.