Abstract
Purpose
To investigate whether telephone-based continuing care (TEL) is a promising alternative to traditional face-to-face counseling for clients in treatment for substance abuse.
Methods
Patients with alcohol and/or cocaine dependence who had completed a 4-week intensive outpatient program were randomly assigned through urn randomization into one of three 12-week interventions: standard continuing care (STD), in-person relapse prevention (RP), or telephone-based continuing care (TEL). This study performed cost, cost-effectiveness, and cost-benefit analyses of TEL and RP compared to STD, using results from the randomized clinical trial with two years of follow up (359 participants). In addition, the study examined the potential moderating effect of baseline patient costs on economic outcomes.
Results
The study found that TEL was less expensive per client from the societal perspective ($569) than STD ($870) or RP ($1,684). TEL also was also significantly more effective, with an abstinence rate of 57.1% compared to 46.7% for STD (p<0.05). Thus TEL dominated STD, with a highly favorable negative incremental cost-effectiveness ratio (−$1,400 per abstinent year). TEL also proved favorable under a benefit-cost perspective.
Conclusions
TEL proved to be a cost-effective and cost-beneficial contributor to long-term recovery over two years. Because TEL dominated STD care interventions, wider adoption should be considered.
Keywords: Alcohol and cocaine dependence, continuing care alternatives, telephone-based continuing care, relapse prevention
1. Introduction
Under the Affordable Care Act, treatment of substance abuse disorders is integrated more closely with general medical services and can receive increased funding through Medicaid expansion (Buck, 2011; Dentzer, 2011). These provisions incentivize both public and private health care payers to identify and implement initiatives to control health costs and improve quality comparable to those for general health care. Adding economic analyses to successful clinical trials may be able to identify approaches that meet these important goals (Emanuel et al., 2012).
Because substance abuse disorders are chronic, relapsing disorders, long-term continuing treatment or aftercare is recommended to reduce the risk of relapse and expensive hospitalization (American Society of Addiction Medicine, 2001). Despite the proven benefits of continuing care programs for substance abuse disorders and other chronic conditions, many patients either do not attend any continuing care, or stop attending after a few sessions (Donovan, 1998; Hawkins and Catalano, 1985; McKay, 2007, 2009; McLellan et al., 2000; O’Brien and McLellan, 1996). Telephone-based continuing care (TEL) is a promising alternative to traditional face-to-face counseling sessions. TEL may be more flexible, less burdensome, and less embarrassing for the patient, and more easily structured by the provider than traditional modalities. All these advantages could improve treatment adherence and health outcomes. By reducing patient travel expenses and time and facility overhead, TEL should also reduce costs.
The telephone has proven to be a viable therapeutic tool in the treatment of several chronic disorders including alcoholism (Connors et al., 1992; Foote and Erfurt, 1991; McKay et al., 2010), panic disorder (Swinson et al., 1995), obsessive-compulsive disorder (Baer et al., 1993), depression (Baer et al., 1995) and congestive heart failure (Jerant et al., 2001). It has also been found to improve outcomes in smoking cessation (Lichtenstein et al., 1996; Stoffelmeyr et al., 2003) and cardiac rehabilitation (Bambauer et al., 2005), and reduces costs for patients in fair or poor overall health (Wasson et al., 1992).
To our knowledge, this report provides the first economic evaluation of telephone counseling in substance abuse treatment. It builds on the results from a randomized trial of telephone-based continuing care for alcohol and other drugs (AOD; McKay et al., 2005a, 2005b, 2004). That trial found that telephone-based counseling is an effective form of continuing care for patients with AOD who are progressing reasonably through their initial phases of care, compared to standard continuing care (STD) or in-person relapse prevention (RP). However, the effect of this modality on health care costs is a key factor in its adoption. Because the public sector funded an estimated 83% of substance abuse treatment in 2014 (Levit et al., 2008), if TEL proves inexpensive, it could become an important tool towards controlling health costs.
1 METHODS
1.1 2.1 Overview
This economic analysis of TEL entails four steps. First, the costs of each continuing care intervention are calculated, with and without the inclusion of societal costs for patients’ time and travel expenses. Second, cost-effectiveness analyses (CEAs) are presented in which TEL and RP are compared to STD. Third, benefit-cost analyses are presented in which the three continuing care interventions are compared on costs related to the consequences of substance use, investment costs, and income from employment during the follow-up. Fourth, regression analysis is used to examine the potential moderating effect of baseline patient costs on economic outcomes based on findings from our earlier study (McKay et al., 2005a, 2005b), hypothesizing that patients who were less costly during the baseline period would see the greatest economic advantages from TEL.
1.1.1 2.2 Enrollment
Patients with alcohol and/or cocaine dependence who had completed a 4-week intensive outpatient program (IOP) were screened for participation in this randomized clinical trial (McKay et al., 2005a). Subjects were enrolled at two program sites in Philadelphia, Pennsylvania: The Philadelphia Veterans Affairs Medical Center (VA; 48% of enrollees) and a clinical research unit within the University of Pennsylvania’s Presbyterian Medical Center (Presbyterian; 52% of enrollees). All participants met Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for being cocaine and/or alcohol dependent, and completed four weeks of IOP treatment. Most participants were male (83%) and non-white (89%). All procedures were approved by the institutional review boards at the University of Pennsylvania and Brandeis University and the participant flow has been previously reported (McKay et al., 2005a, 2005b, 2004).
1.1.2 2.3 Interventions
Participants were randomly assigned with urn randomization into one of three 12-week interventions: STD, RP, or TEL. STD consisted of 12 weeks of twice weekly two-hour group sessions. RP consisted of 12 one-hour individual sessions and 12 two-hour group sessions, also provided over 12 weeks. TEL consisted of one individual one-hour face-to-face session, four one-hour group support sessions, and eleven 20-minute telephone counseling sessions provided over 12 weeks. Table 1 compares the three intervention arms (TEL, RP and STD) on counselor contacts, contact time, outcomes after two years and the cost-effectiveness of interventions. Further details about the interventions are presented elsewhere. (McKay, 2005; McKay et al., 2004)
Table 1.
Comparison of intervention arms: inputs, outcomes, and cost-effectiveness
| Item | STD (N=122) | RP (N=135) | TEL (N=102) |
|---|---|---|---|
| (a) Number of planned counselor contacts per client (with actual numbers in parentheses) | |||
| Individual sessions | 0.0 (0.1) | 12.0 (7.2) | 1.0 (1.0) |
| Group sessions | 24.0 (14.1) | 12.0 (7.1) | 4.0 (4.3) |
| Telephone sessions | 0.0 (0.0) | 0.0 (0.0) | 11.0 (5.7) |
| Total | 24.0 (14.2) | 24.0 (14.3) | 16.0 (11.0) |
| (b) Planned contact time per client | |||
| Client hours | 56.6 | 50.0 | 17.8 |
| Counselor hours | 6.0 | 16.0 | 5.3 |
| (c) Outcomes per client, 2 years | |||
| Effectiveness: Average % abstinent each quarter | 46.7% | 51.7% | 57.1% |
| Incremental effectiveness | Reference | 5.0% | 10.4% |
| 95% confidence interval | n.a. | [−3.2%; 13.2%] | [0.1%; 20.7%] |
| Program cost | $511 | $1,363 | $454 |
| Value of client time and travel | $359 | $322 | $115 |
| Societal cost | $870 | $1,684 | $569 |
| (d) Incremental cost | |||
| Program cost over 2 years | Reference | $852 | −$57 |
| Program cost per year | Reference | $426 | −$29 |
| Societal cost over 2 years | Reference | $814 | −$301 |
| Societal cost per year | Reference | $407 | −$151 |
| (e) Cost-effectiveness (perspective) | |||
| ICER (program) | Reference | $8,500 | −$300 |
| 95% confidence interval | [$3,200; infinity] | [−$30,700; −$100] | |
| ICER (societal) | Reference | $8,100 | −$1,400 |
| 95% confidence interval | [$3,100; infinity] | [−$161,900; −$700] | |
Notes: STD denotes standard continuing care program; RP denotes relapse prevention program; TEL denotes continuing care delivered over the telephone program; n.a. denotes not applicable. Incremental (Incr.) effectiveness uses STD as the reference. ICER denotes incremental cost-effectiveness ratio (incremental cost per abstinent year) compared to reference category (STD). Statistical significance of incremental effectiveness of RP, based on RP vs. STD contrast, is 0.24; that of TEL, based on TEL vs. STD contrast, is 0.047 (McKay et al., 2005a). Costs are in 2005 prices.
2.4 Effectiveness measures
Participants were followed for two years through interviews conducted by study technicians not involved in the interventions, and results were validated against biological samples. Average abstinence rates from drugs and alcohol by the study arm were calculated by averaging across clients and assessment periods.
2.5 Cost analysis
Following CEA guidelines for the health sector, the cost analysis represents treatment program costs at a societal level. It combines institutional (costs borne by the health system) and client levels (travel expenses and opportunity costs of treatment time borne by a patient; Gold et al., 1996; Popovici et al., 2008).
Intervention program unit costs were derived for each of the three arms based on year 2005 prices using components of two well-established cost methods in the substance abuse treatment costing instruments 1) the Treatment Cost Analysis Tool (TCAT) and 2) the Substance Abuse Treatment Service Cost Analysis Program (SASCAP; Beaston-Blaakman et al., 2007; Flynn et al., 2009; Zarkin et al., 2004). As a cost-accounting tool for application in both program studies and clinical trials, the TCAT examines personnel and non-personnel costs from the institutional perspective and incorporates important reliability checks to verify cost data. Using the SASCAP labor cost allocation methodology as a guide, personnel time data were captured retrospectively via individual interviews with therapists and supervisors to allocate personnel costs to each of the three intervention arms.
To ensure that they would be available for scheduled sessions, therapists did not overbook; thus their time was based on scheduled sessions. To reflect the staffing of typical clinics rather than research settings, therapists’ total paid time (including planned contact time, documentation, receiving supervision, meetings, absences, and unused slots to accommodate clients’ schedules) was estimated as twice their planned direct client contact time. Clients’ time in treatment, waiting, and travel were based on actual sessions attended and valued at the then applicable Pennsylvania minimum wage ($5.65/hour; Labor Law Center Blog, 2006). Clients’ travel expenses averaged $2.75 per round trip (bulk tickets on Philadelphia public transport).
1.1.3 2.6 Cost-effectiveness analysis (CEA)
CEA relates the incremental opportunity cost of implementing a treatment program to the incremental change in some non-monetary outcome of interest. For this study, we used abstinence from drugs and alcohol as the outcome, as it was the goal of treatment and generally leads to secondary benefits. We calculated the cost-effectiveness ratio for TEL using equation (1), with an analogous formula for RP:
| (1) |
2.7 Cost-benefit analysis (CBA)
2.7.1 Data collection for quantities
Cost-benefit analyses required estimating quantities of resources consumed or generated by clients and their unit costs. Data for the quantities were based on research interviews with clients at intake into the aftercare study and six follow-up periods (months 3, 6, 9, 12, 18, and 24). Many of the quantities came from the Addiction Severity Index (ASI; French, 2000, 2001; French et al., 2002) which was administered at each participant’s interview.
Economic outcomes were created using the interview data and were classified into costs of adverse consequences (resources consumed during the study period), economic benefits (resources generated during the study period), and investments (resources consumed in activities with anticipated impacts mostly beyond the study period). Economic costs of adverse consequences consisted of the economic value of days experiencing medical or psychological problems, jail days or days involved in illegal activities, plus self-reported expenditures on drugs or alcohol. Self-reported income from legal employment was used as the primary measure of current economic benefits. Expenses for inpatient substance abuse, mental health, or medical treatment reported in the post-IOP period were considered investments; they generally reflected attention to previously neglected or deferred problems, and were expected to generate improvements primarily beyond the time horizon of the study.
2.7.2 Derivation of unit costs
Dollar values were assigned to each resource using methods developed by French and colleagues specifically for the ASI (French, 2000, 2001; French et al., 2002). Standard resource categories include personnel, supplies and materials, contracted services, buildings and facilities, equipment and other operating costs as well as time, travel and waiting costs for clients.
For example, in a comprehensive study from 2002, each day of inpatient medical treatment was valued at $1,460.50 based on the average daily expenses of metropolitan community hospitals in Pennsylvania. A day of residential treatment ($90.69) was the average value from published and unpublished data on all residential treatment programs that completed the Drug Abuse Treatment Cost Analysis Plan (DATCAP; French et al., 2002). Quantities were then multiplied by inflation-adjusted unit costs to obtain total economic values.
2.7.3 Transformations of outcome variables
Due to the rarity and skewness in high costs of certain consequences (where most participants had low or zero values, a few had high values), we took three steps. First, we combined six of the consequences (jail days; days engaged in illegal activities; days experiencing psychological problems; days experiencing medical problems; spending on alcohol; and spending on drugs) into a single aggregate burden cost variable, and the investment components (inpatient medical, addiction, and psychological treatment stays) into overall investments. Second, to allow us to combine costs of different types of consequences while reducing random variation, we recoded each of the individual and aggregated variables to the medians of the three categories (zero, below the median, or above the median). Third, we transformed each individual and aggregate cost variable (x) using the started natural log transformation (i.e., ln(x + 1)). Thus our dependent variables were: (1) Log cost of consequences: defined as log of aggregate cost burden. (2) Log income: the log of monthly income during follow-up months; and (3) Log investment: a categorized aggregate version of log investment costs. For consistency with costs, all economic data related to income, investments and consequences were converted to 2005 dollars based on the US GDP deflator (U.S. Department of Commerce. Bureau of Economic Analysis).
2.7.4 Statistical analysis
Descriptive statistics and bivariate analyses were run for each of the individual (i.e., subject-level) and grouped variables (i.e., treatment condition, time period, and program). Next, regression analyses were conducted where our dependent variables were the two economic outcomes, both measured on started log scales. In addition to the treatment conditions (STD; RP; or TEL), we identified two of the three main effect independent variables: SEQUENCE (the time-period variable), and PROGRAM (program location: VA or Presbyterian Hospital). To test the moderating effects, we also included the baseline value of the corresponding economic value on the same scale (linear or started log), and an interaction term between TXCOND and the baseline value. We used the SAS PROC MIXED procedure with fixed effects, repeated measures, and clustering on subjects.
Following the standard principles of cost-effectiveness analysis (Gold et al., 1996), we used the status quo as our standard reference case. Accordingly, as STD represents our reference case, intervention costs, economic costs and benefits of RP and TEL were all calculated relative to STD. As moderator analyses in the main trial showed that the effectiveness of TEL depended on measures of client severity, we conducted moderator analyses using the severity measure most relevant for each cost-offset analysis, namely the baseline value of the dependent variable.
Sensitivity analyses examined the effects of statistical variation in estimated effectiveness and economic outcomes.
3. Results
3.1 Effectiveness and costs by arm
Table 1 section (c) shows average values of costs and effectiveness by arm. TEL produced higher abstinence rates overall during the 24-month follow-up than STD (p< 0.05) and were somewhat higher in TEL than in RP, although not significantly so (McKay et al., 2005a, 2005b, 2004) The moderator analysis found that TEL was more effective for clients who met the majority of the initial goals of their IOP (80% of the sample). However, STD, with its greater group support, was most effective for the 20% of patients who failed to achieve the majority of those goals (McKay, 2005; McKay et al., 2005b).
Over the two-year study period, from the perspectives of both treatment program costs and societal costs, TEL was the least expensive intervention ($454 and $569, respectively). Not surprisingly, time and travel costs were considerably lower in the TEL condition as clients did not have to travel to the clinic for most aspects of treatment.
3.2 Cost-effectiveness analysis
TEL was the most cost-effective approach from both the program and societal perspectives (see Table 1, sections (d) and (e)). Clients in TEL were 10.4 percentage points more likely to remain abstinent than those in STD, a significant difference (p<0.05; McKay et al., 2005a). From the program perspective, the incremental cost per participant per program year was −$29 (i.e., it was less expensive than STD), giving a negative (and thus very favorable) incremental cost-effectiveness ratio of −$300 per incremental abstinent year. From the societal perspective, TEL was also both less costly and more effective than the STD program. The net cost per program year was negative (−$151). The incremental cost-effectiveness ratio was an extremely favorable negative number (−$1,400 per abstinent year). Thus TEL dominated STD on both program and societal perspectives.
3.3 Cost-benefit analysis
3.3.1 Pattern over time
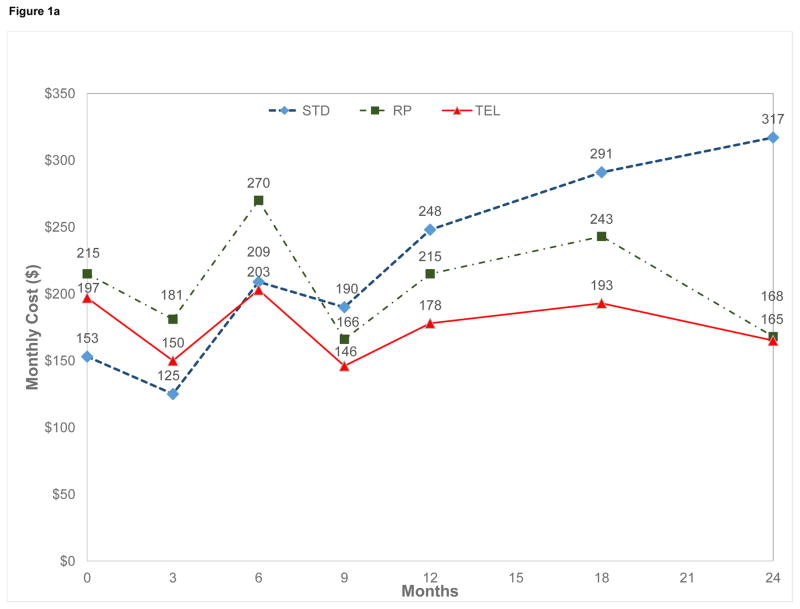
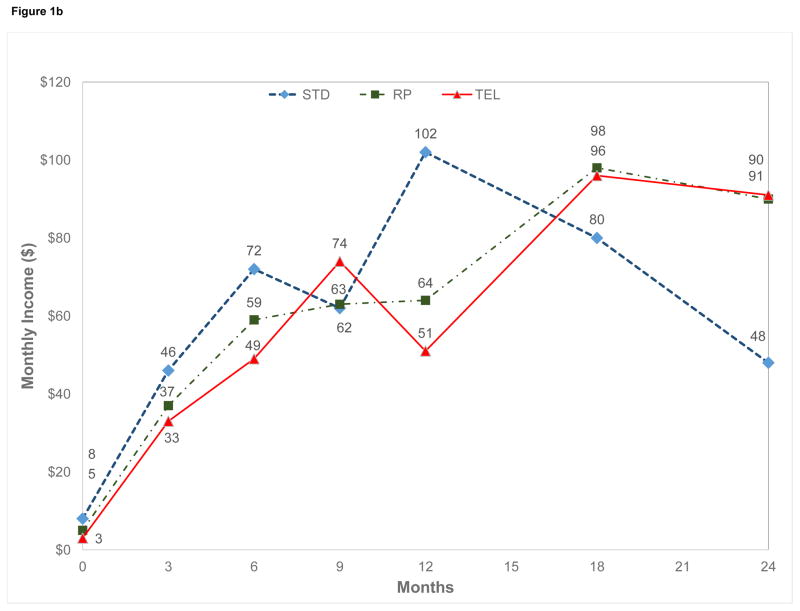
Figure 1(a) shows the geometric mean of the cost of adverse consequences per month by treatment arm for all participants. The cost of consequences fell for all groups from baseline to 3 months (the end of the intensive period of continuing care) and fluctuated over the remainder of the follow-up period. For TEL and RP, costs at 24 months are approximately those of the baseline level, while in STD, the costs of consequences exceed those of the baseline level.
Figure 1.
Means of dependent variables by arm (geometric mean of monthly amount per participant) (a) Cost of adverse consequences. (b) Income of participants
Neither income from employment (Figure 1(b)) nor average monthly investments of $2.90 for STD, $1.94 for RP and $2.61 for TEL (data not shown) showed significant main or interaction effects. Nevertheless, income from employment rose and investments in treatment fell in all treatment conditions as clients left controlled environments and transitioned through continuing care.
3.3.2 Regression results on costs of consequences
Regression results (using PROC MIXED) in Table 2 shows that STD was significantly higher than TEL in costs of consequences after controlling for baseline values (excess risk 3.79, p < 0.01). Although RP also tended to have more costs of consequences than TEL, the difference was not statistically significant after controlling for other covariates. As predicted, higher baseline costs were strongly associated with higher costs of consequences with an elasticity of 0.17 (STD), 0.27 (RP), or 0.40 (TEL). That is, for every 10% increase in baseline costs of consequences, the costs of consequences at follow-up rose by about 2%, 3%, or 4%, respectively.
Table 2.
Regression results for costs of consequences (log scale, with TEL as reference)
| Independent variables* | Co-efficient (β) | Excess risk, Exp(β)-1 | t-statistic | Statistical significance |
|---|---|---|---|---|
| STD | 1.57 | 3.79 | 2.59 | < 0.01 |
| RP | 0.78 | 1.19 | 1.26 | n.s. |
| Log baseline costs of consequences | 0.40 | 0.50 | 4.76 | <0.0001 |
| Log baseline costs of consequences x STD | −0.23 | −0.21 | −2.18 | <0.05 |
| Log baseline costs of consequences x RP | −0.13 | −0.12 | −1.18 | n.s. |
Notation: STD denotes standard continuing care program; RP denotes relapse prevention program, TEL denotes telephone-based continuing care program (reference). n.s. denotes not statistically significant, log denotes natural logarithm. Regressions were run with SAS procedure PROC MIXED.
Earlier models tested the following independent variables, but dropped them from the final model because they proved to be not statistically significant: Treatment condition x Log baseline cost of consequences, Log income, Log baseline income, Treatment condition x Log baseline income, Baseline investment, Treatment condition x Log baseline investment, Program, Treatment condition, and Sequence
The interaction between baseline costs of consequences and the treatment condition variable allowed us to estimate whether baseline costs of consequences moderated the effects of the interventions. This analysis, shown in equation (2) with standard errors below each coefficient, was designed to mirror the moderator analyses done in our previous reports (McKay et al., 2005a, 2005b).
| (2) |
Here FU denotes natural log of monthly costs of costs of adverse consequences at follow up, BL denotes natural log of monthly costs of costs of adverse consequences at baseline, STD is a dummy variable (1 if subject is in STD, otherwise 0), RP is a dummy variable (1 if subject is in RP, otherwise 0), and TEL is the reference group. The numbers in parentheses are the standard errors of the coefficients.
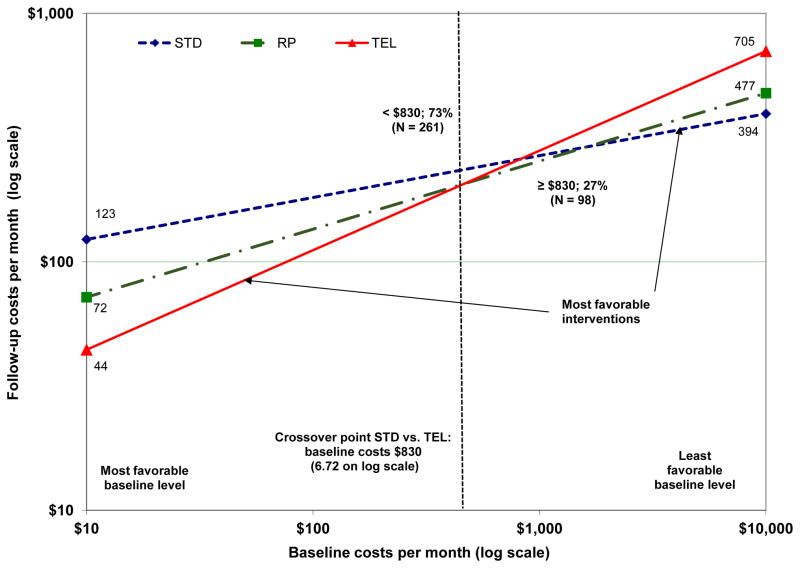
The significant interaction term for STD (compared with TEL) of −0.2330 (p < 0.05) means that costs of consequences increased more slowly in STD with higher baseline costs than they did for clients in TEL. Illustrated graphically (see Figure 2), TEL was associated with lower costs of consequences for the majority (73%) of clients who had baseline costs of consequences below $830. On the other hand, STD resulted in lower costs of consequences for clients with over $830 in baseline costs
Figure 2.
Cost of consequences by group as a function of baseline values group (geometric mean of monthly amounts per participant)
For participants with very low baseline costs (i.e., $10 per month), monthly costs of consequences under TEL were $79 less than those in STD (i.e., $44 vs. $123, respectively). Over 12 months, the savings in costs of consequences were $948.
As with the costs of adverse consequences, a significant positive relationship was found between the baseline and follow-up measures of income and investments. Specifically, regressions with these independent variables showed that for every 10% increase in baseline employment income, income from employment was 32% higher (p < 0.10) during follow-up. Similarly, for each 10% increase in investment costs reported at baseline, there was an increase of 7% (p < 0.05) in investment costs at follow-up. Unlike the costs of consequences, however, these positive relationships to baseline values were independent of participants’ treatment group assignment.
4. Discussion
The strengths of this study are design features that address many of the limitations of previous research and meet recently recommended standards for economic evaluation of continuing care (Popovici et al., 2008). The use of random assignment protects against selection bias. The long-term (24-month) follow-up period is suitable for a continuing care intervention. Program costs and benefits were assessed with validated instruments (Flynn et al., 2009; Shepard et al., 2012). Treatment sites and participants’ socio-demographic characteristics generalize to other publicly funded settings. Enrollment was sufficient for both main and subgroup analyses. Unit costs came from credible external sources. The combination of economic frameworks (cost, CEA and CBA) provides numerous perspectives for policy makers on the economic impact of the interventions.
The study found that continuing care delivered over the telephone was less expensive, more cost-effective, and more cost-beneficial than standard clinic-based group counseling continuing care. From the program perspective, TEL was the least expensive of the three interventions because the sessions were shorter. It proved least expensive from the societal perspective as well, because it entailed less time commitment for sessions as well as for travel. Travel costs may be a particularly salient issue for lower income, disabled or rural patients. The flexibility offered by TEL would be an advantage to clients who recently became employed or who had parenting responsibilities. An additional benefit to some clients was reduction in stigma due to the greater privacy offered by TEL. These are among the many ways that TEL can help clients maintain treatment involvement over long time intervals, a powerful contributor to long-term recovery (Dennis and Scott, 2007; McKay, 2009; McLellan et al., 2000).
Under the cost-effectiveness framework, we found TEL dominated the alternatives by being less costly and more effective in terms of abstinent years. Because dominance by one treatment over two others is a rare occurrence in economic evaluations, wider adoption of TEL should be considered. Historically, the treatment of addictions has tended to follow an acute care model. For example, some insurance policies limit the number of outpatient sessions covered and do not currently reimburse telephone-based treatment. Such practices inhibit recovery, because longitudinal studies show that more than half of patients in publicly funded treatment programs require multiple episodes over a number of years before they can reach sustained recovery (Dennis and Scott, 2007; McKay, 2009; McLellan et al., 2000). Developing methods to verify and reimburse providers for telephone counseling could help make this service financially viable for fee-for-service treatment providers.
Under the cost-benefit framework, we found that TEL produced lower consequence costs, but no difference in investment costs. TEL, like some screening interventions in general health, might have sensitized participants to their existing problems and induced additional utilization. Our analysis of investment costs did not find any such increases compared to STD, but our study design did not permit a comparison to no treatment.
As studies of the economic cost of alcohol and drug abuse found that productivity loss is one of their greatest economic burdens, more effective counseling might have been expected to increase participant productivity. In fact, income from employment in TEL was not significantly higher than other arms. This finding may reflect the chronic nature of these clients’ substance abuse, as well as their poor job prospects. Thus, participants had limited legal income immediately prior to treatment. Nevertheless, it is encouraging that within each of the treatment conditions, legal income improved over the course of the evaluation.
The presence of significant differences among treatment arms on adverse consequences contrasts with the lack of such differences on income. Because substance use outcomes were better in TEL than in STD (McKay, 2005; McKay et al., 2004), and the fact that clients have little employment experience (and thus little income), this difference is plausible. The average costs of adverse consequences were substantially greater than income in the period immediately following treatment. Not surprisingly, regardless of treatment, clients with greater income at baseline had higher income during follow-up. Likewise, the clients who had higher costs of adverse consequences at baseline continued to have more of the same types of costs at follow-up.
Although there were no significant differences among the three treatment groups, the costs associated with all types of health care tended to decline after baseline. This pattern is consistent with previous studies (Holder and Blose, 1992; Hunkeler et al., 2001; Parthasarathy and Weisner, 2005). One theory is that an exacerbation in alcohol and/or drug-related health problems may have motivated some clients to seek treatment, so lower costs after treatment reflect, in part, regression to the mean.
The cost-effectiveness findings suggest that the RP was the most expensive of the three programs ($1,363), probably because of its greater reliance on longer individual face-to-face treatment sessions (i.e., typically 45–60 minutes per session). The STD program costs less because it was more oriented toward group therapy. Although RP has sometimes proved more efficacious than other approaches (Irvin et al., 1999), this study found no such advantage. Based on findings from cognitive-behavioral therapy (Carroll, 1996), the use of a technology-based version of RP might reduce the costs of this approach in the future.
One limitation of the current study is that it did not include a no-treatment control group, which meant we could not compute an overall benefit-cost ratio relative to a no-treatment arm. However, a no-treatment group would not have been ethically permissible. Moreover, the group counseling continuing care in this study is standard care, or treatment as usual in most addiction treatment programs. An additional limitation is that the economic outcomes used in the cost-benefit analyses on the types of services received and consequences experienced were based on self-report. However, patient self-reports on substance use in this study were corroborated from biological samples and collaterals, and unit costs of medical services and consequences came from external sources. Additionally, self-report measures, such as the ASI, have been widely used and validated both for effectiveness and outcome studies (French et al., 2002).
TEL is an example of a technological advance that has the potential to expand access to AOD treatment to formerly underserved populations (Strecher, 2007; Bewick et al., 2008; Riper et al., 2007; Scott and Dennis, 2009; Stead et al., 2007). By contributing to lower costs, reduced stigma, and better treatment access, telephone counseling could potentially benefit the 19.3 million Americans aged 12 and over who needed but did not receive substance abuse treatment according to the latest available data (Dawson et al., 2005; Substance Abuse and Mental Health Services Administration (SAMHSA), 2012). In the future, smart phone apps may help facilitate, guide and document communication. The integration of substance abuse treatment into general health care provides an opportunity for learning and sharing in both directions. Innovative approaches to health care delivery, such as telephone counseling, deserve evaluation and implementation for a variety of health conditions.
Telephone continuing care achieved greater abstinence than standard groups
Shorter sessions made telephone continuing care less costly than standard groups
Avoiding travel time and expenses, telephone continuing care saved clients money
Telephone continuing care is cost-effective and should be more widely disseminated
Telephone provides support to clients who otherwise might not get continuing care
Footnotes
Conflict of Interest
The authors have no conflicts of interest to declare.
Contributors
DSS and JM came up with the concept of the paper. MD, MN, and APB performed the statistical analysis. MN wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Society of Addiction Medicine. Patient Placement Criteria for the Treatment of Substance-Related Disorders. 2. ASAM; Chevy Chase, MD: 2001. [Google Scholar]
- Baer L, Brown-Beasley MW, Sorce J, Henriques AL. Computer assisted telephone administration of a structured interview for obsessive-compulsive disorder. Am J Psychiatry. 1993;150:1737–1738. doi: 10.1176/ajp.150.11.1737. [DOI] [PubMed] [Google Scholar]
- Baer L, Jacobs DG, Cukor P, O’Laughlen J, Coyle JT, Magruder KM. Automated telephone screening survey for depression. JAMA. 1995;273:1943–1944. [PubMed] [Google Scholar]
- Bambauer KZ, Aupont O, Stone P, Locke SE, Mullan MG, Colagiovanni J, McLaughlin TJ. The effect of a telephone counseling intervention on self-rated health of cardiac patients. Psychosom Med. 2005;67:539–545. doi: 10.1097/01.psy.0000171810.37958.61. [DOI] [PubMed] [Google Scholar]
- Beaston-Blaakman A, Shepard D, Horgan C, Ritter G. Organizational and client determinants of cost in outpatient substance abuse treatment. J Ment Health Policy Econ. 2007;10:3–13. [PubMed] [Google Scholar]
- Bewick BM, Truster K, Barkham M, Hill AJ, Cahill J, Mulhern B. The effectiveness of web-based interventions designed to reduce alcohol consumption - a systematic review. Prev Med. 2008;47:17–26. doi: 10.1016/j.ypmed.2008.01.005. [DOI] [PubMed] [Google Scholar]
- Buck JA. The looming expansion and transformation of public substance abuse treatment under The Affordable Care Act. Health Aff (Millwood) 2011;30:1402–1410. doi: 10.1377/hlthaff.2011.0480. [DOI] [PubMed] [Google Scholar]
- Carroll KM. Relapse prevention as a psychosocial treatment: a review of controlled studies. Exp Clin Psychopharmacol. 1996;4:46–54. [Google Scholar]
- Connors GJ, Tarbox AR, Faillace LA. Achieving and maintaining gains among problem drinkers: Process and outcome results. Behav Ther. 1992;23:449–474. [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- Dennis M, Scott CK. Managing addiction as a chronic condition. Addict Sci Clin Pract. 2007;4:45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dentzer S. Substance abuse and other substantive matters. Health Aff (Millwood) 2011;30:1398. doi: 10.1377/hlthaff.2011.0811. [DOI] [PubMed] [Google Scholar]
- Donovan DM. Continuing care: promoting the maintenance of change. In: Miller WR, Heather N, editors. Treating Addictive Behaviors. 2. Plenum; New York, NY: 1998. pp. 317–336. [Google Scholar]
- Emanuel E, Tanden N, Altman S, Armstrong S, Berwick D, de Brantes F, Calsyn M, Chernew M, Colmers J, Cutler D, Daschle T, Egerman P, Cocher B, Milstein A, Lee EO, Podesta JD, Reinhardt U, Rosenthal M, Sharfstein J, Shotell S, Stern A, Orszag PR, Spiro T. A systematic approach to containing health care spending. N Engl J Med. 2012;367:949–954. doi: 10.1056/NEJMsb1205901. [DOI] [PubMed] [Google Scholar]
- Flynn PM, Broome KM, Beaston-Blaakman A, Knight DK, Horgan CM, Shepard DS. Treatment cost analysis tool (TCAT) for estimating costs of outpatient treatment services. Drug Alcohol Depend. 2009;100:47–53. doi: 10.1016/j.drugalcdep.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foote A, Erfurt JC. Effects of EAP follow-up on prevention of relapse among substance abuse clients. J Stud Alcohol. 1991;52:241–248. doi: 10.15288/jsa.1991.52.241. [DOI] [PubMed] [Google Scholar]
- French MT. Benefit-cost analysis of residential and outpatient addiction treatment in the State of Washington. Eval Rev. 2000;24:609–634. doi: 10.1177/0193841X0002400603. [DOI] [PubMed] [Google Scholar]
- French MT. Economic evaluation of alcohol treatment services. In: Galanter M, editor. Recent Developments in Alcoholism. Volume 15, Services Research in the Era of Managed Care. Kluwer Academic/Plenum Publishers; NewYork: 2001. pp. 209–228. [DOI] [PubMed] [Google Scholar]
- French MT, Salomé HJ, Sindelar JL, McLellan A. Benefit-cost analysis of addiction treatment: methodological guidelines and empirical application using the DATCAP and ASI. Health Serv Res. 2002;37:433–455. doi: 10.1111/1475-6773.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-Effectiveness in Health and Medicine. Oxford University Press; New York: 1996. [Google Scholar]
- Hawkins JD, Catalano RF. The role of continuing care in drug abuse treatment. Int J Addiction. 1985;20:917–945. doi: 10.3109/10826088509047759. [DOI] [PubMed] [Google Scholar]
- Holder HD, Blose JO. The reduction in health care costs associated with alcoholism treatment: a 14 year longitudinal study. J Stud Alcohol. 1992;53:293–302. doi: 10.15288/jsa.1992.53.293. [DOI] [PubMed] [Google Scholar]
- Hunkeler EM, Hung YY, Rice DP, Weisner C, Hu T. Alcohol consumption patterns and health care costs in an HMO. Drug Alcohol Depend. 2001;64:181–190. doi: 10.1016/s0376-8716(01)00119-3. [DOI] [PubMed] [Google Scholar]
- Irvin JE, Bowers CA, Dunn M, Wang MC. Efficacy of relapse prevention: a meta analytic review. J Consult Clin Psychiatry. 1999;67:563–570. doi: 10.1037//0022-006x.67.4.563. [DOI] [PubMed] [Google Scholar]
- Jerant AF, Azari R, Nesbitt TS. Reducing the cost of frequent hospitalizations for congestive heart failure: a randomized trial of a home telecare intervention. Med Care. 2001;39:1234–1245. doi: 10.1097/00005650-200111000-00010. [DOI] [PubMed] [Google Scholar]
- Labor Law Center Blog. Pennsylvania (PA): Minimum Wage Posters; 2006. [Accessed 9 November 2015]. Available at: http://blog.laborlawcenter.com/2006/09/19/pennsylvania-pa-minimum-wage-posters/ [Google Scholar]
- Levit KR, Kassed CA, Coffey RM, Mark TL, Stranges EM, Buck JA, Vandivort-Warren R. Future funding for mental health and substance abuse: increasing burdens for the public sector. Health Aff (Millwood) 2008;27:w513–522. doi: 10.1377/hlthaff.27.6.w513. [DOI] [PubMed] [Google Scholar]
- Lichtenstein E, Glasgow RE, Hando HA, Ossip-Klein DJ, Boles S. Telephone counseling for smoking cessation: rationales and meta-analytic review of evidence. Health Educ Res. 1996;11:243–257. doi: 10.1093/her/11.2.243. [DOI] [PubMed] [Google Scholar]
- McKay JR. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100:1594–1610. doi: 10.1111/j.1360-0443.2005.01208.x. [DOI] [PubMed] [Google Scholar]
- McKay JR. Lessons learned from psychotherapy research. Alcohol Clin Exp Res. 2007;31:48S–54S. doi: 10.1111/j.1530-0277.2007.00493.x. [DOI] [PubMed] [Google Scholar]
- McKay JR. Continuing care research: what we have learned and where we are going. J Subst Abuse Treat. 2009;36:131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Lynch K, Shepard DS, Pettinati HM. The effectiveness of telephone-based continuing care for alcohol and cocaine dependence: 24 month outcomes. Arch Gen Psychiatry. 2005a;62:199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Morgenstern J, Forman RF, Pettinati HM. Do patient characteristics and initial progress in treatment moderate the effectiveness of telephone based continuing care for substance use disorders? Addiction. 2005b;100:216–226. doi: 10.1111/j.1360-0443.2005.00972.x. [DOI] [PubMed] [Google Scholar]
- McKay JR, Shepard DS, Ratichek S, Morrison R, Koppenhaver J, Pettinati HM. The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12 month outcomes. J Consult Clin Psychol. 2004;72:967–979. doi: 10.1037/0022-006X.72.6.967. [DOI] [PubMed] [Google Scholar]
- McKay JR, Van Horn DHA, Oslin DW, Lynch KG, Ivey M, Ward K, Drapkin ML, Becher JR, Coviello DM. A randomized trial of extended telephone based continuing care for alcohol dependence: within-treatment substance use outcomes. J Consult Clin Psychol. 2010;78:912–923. doi: 10.1037/a0020700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- O’Brien CP, McLellan AT. Myths about the treatment of addiction. Lancet. 1996;347:237–240. doi: 10.1016/s0140-6736(96)90409-2. [DOI] [PubMed] [Google Scholar]
- Parthasarathy S, Weisner CM. Five-year trajectories of health care utilization and cost in a drug and alcohol treatment sample. Drug Alcohol Depend. 2005;80:231–240. doi: 10.1016/j.drugalcdep.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Popovici I, French MT, McKay JR. Economic evaluation of continuing care interventions in the treatment of substance abuse: recommendations for future research. Eval Rev. 2008;32:547–569. doi: 10.1177/0193841X08316311. [DOI] [PubMed] [Google Scholar]
- Riper H, Kramer J, Smit F, Conijn B, Schippers GP. Web-based self-help for problem drinkers: a pragmatic randomized trial. Addiction. 2007;103:218–227. doi: 10.1111/j.1360-0443.2007.02063.x. [DOI] [PubMed] [Google Scholar]
- Scott CK, Dennis ML. Results of two randomized clinical trials evaluating the impact of quarterly recovery management check-ups with adult chronic substance abuser. Addiction. 2009;104:959–971. doi: 10.1111/j.1360-0443.2009.02525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepard DS, Zeng W, Strickler G, Lwin AK, Cros M, Garner B. The Brief Treatment Cost Analysis Tool (TCAT-Lite) for substance abuse treatment: reliability and application. Alcohol Treat Q. 2012;30:377–339. doi: 10.1080/07347324.2012.719425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stead LF, Perera R, Lancaster T. A systematic review of interventions for smokers who contact quitlines. Tob Control. 2007;16:i3–i8. doi: 10.1136/tc.2006.019737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoffelmeyr B, Wadland WC, Pan W. An examination of the process of relapse prevention therapy designed to aid smoking cessation. Addict Behav. 2003;28:1351–1358. doi: 10.1016/s0306-4603(02)00250-2. [DOI] [PubMed] [Google Scholar]
- Strecher V. Internet methods for delivering behavioral and health-related interventions. (eHealth) Annu Rev Clin Psychol. 2007;3:53–76. doi: 10.1146/annurev.clinpsy.3.022806.091428. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: 2012. NSDUH Series H-44 Publication No. SMA12-4713. [Google Scholar]
- Swinson R, Fergus K, Cox B, Wickwire K. Efficacy of telephone-administered behavioral therapy for panic disorder with agoraphobia. Behav Res Ther. 1995;33:465–469. doi: 10.1016/0005-7967(94)00061-n. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Commerce. Bureau of Economic Analysis. [Accessed 9 November 2015];Current Dollar and “Real” Gross Domestic Product (GDP) Tables. 2015 Available at: http://www.bea.gov/
- Wasson J, Gaudette C, Whaley F, Sauvigne A, Baribeau P, Welch HG. Telephone care as a substitute for routine clinic follow-up. JAMA. 1992;267:1788–1793. [PubMed] [Google Scholar]
- Zarkin GA, Dunlap LJ, Homsi G. The substance abuse services cost analysis program (SASCAP): a new method for estimating drug treatment services costs. Eval Prog Plan. 2004;27:35–43. [Google Scholar]