Abstract
Introduction
Little is known about the association between problem-gambling severity and psychiatric disorders among American-Indian/Alaska-Native (AI/AN) individuals. Thus, we examined these factors among a nationally representative sample of AI/AN and other American adults in the USA.
Method
Using the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) data, we conducted separate Wald tests and multinomial logistic regression analyses comparing AI/AN to black/African American, white/Caucasian, and all other racial/ethnic groups, respectively.
Results
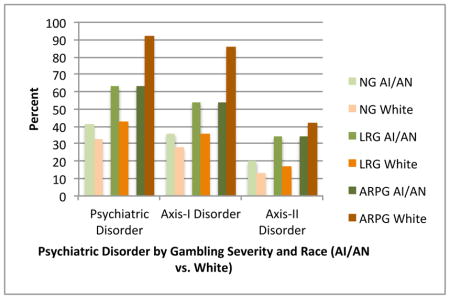
Relative to other American adults, AI/AN adults were least likely to report non-/low-frequency gambling (NG: AI/AN 66.5%, white/Caucasian 70.5%, black/African American 72.8%, other racial/ethnic group 72.3%) and most likely to report low-risk gambling (LRG: AI/AN 30.1%, white/Caucasian 26.5%, black/African American 23.4%, other racial/ethnic group 24.7%). The association between at-risk/problem-gambling (ARPG) and any past-year Axis-I disorder was stronger among AI/AN versus other American adults. Although ARPG and LRG were associated with multiple past-year Axis-I and lifetime Axis-II psychiatric disorders in both AI/AN and other American adults, LRG was more strongly associated with both Axis-I disorders (particularly major depression, generalized anxiety disorder and nicotine dependence) and Cluster-B Axis-II (particularly antisocial personality disorder) disorders in AI/AN versus other American adults.
Discussion
A stronger association between problem-gambling severity and past-year psychiatric disorders among AI/AN relative to other American adults suggests the importance of enhancing mental health and problem-gambling prevention and treatment strategies that may help AI/AN individuals.
Keywords: American Indian/Alaska Native, Gambling, Psychiatric Disorders, Comorbidity
Graphical Abstract
Introduction
There are 5.2 million American-Indian/Alaska-Native (AI/AN) individuals living in the USA, and the US Census shows a 39% increase in AI/AN individuals since 2000 (Norris et al., 2012). As descendants of the indigenous people, AI/AN individuals are a diverse population with more than 500 federally recognized tribes in the USA. These individuals have experienced intergenerational trauma, discrimination and racism, which have accumulated into emotional and psychological suffering. Relative to the general population, AI/AN individuals are disproportionately affected by mood, anxiety, and substance-use disorders (Beals et al., 2005, Gone and Trimble, 2012), as well as interpersonal violence (Gone and Trimble, 2012, Oetzel and Duran, 2004), child maltreatment (Duran et al., 2004), and suicide (Gone and Trimble, 2012).
Rates of disordered gambling, including pathological gambling (PG; endorsement of 5 or more criteria of the Diagnostic and Statistical Manual of Mental Disorders [DSM-IV]) and problem gambling (PrG; which typically employs a lower threshold than PG) among AI/AN individuals are also high. A review of the extant literature on gambling among AI/AN individuals in 2001 found PrG rates of 5.8–19% and PG rates of 6.6–22% (Wardman et al., 2001). These rates are two to five times higher than the PrG rates and four to 16 times higher than the PG rates found among non-AI/AN American adults (Wardman, el-Gudebaly, 2001). Since publication of this review, three studies have examined disordered gambling among AI/AN adults. The first study examined PG rates among 3,007 residents in New Mexico by oversampling American-Indian individuals and found that the PG rate among American-Indian residents was higher (2.2%) than that of non-American-Indian residents (0.9%) (Volberg and Bernhard, 2006). The second study showed that the PG rate among American-Indian veterans sampled from southwest and north central regions of the USA was higher than the PG rate detected among Hispanic veterans from the same region (9.9% vs. 4.3%) (Westermeyer et al., 2005). The third study showed that in the USA, PrG rates among American-Indian individuals were higher than in the general population (18% vs. 8%) (Patterson-Silver Wolf et al., 2014). In sum, the studies-to-date show varied rates of disordered gambling among AI/AN adults depending on the sample; however, the overall disordered gambling rates are uniformly higher than those of non-AI/AN groups.
Prior studies have described that the high prevalence estimates of psychiatric problems, including addictive behaviors such as disordered gambling, among AI/AN individuals is not inherently attributable to “race” per se, but reflects a consequence of pervasive and systematic exposure to poverty, racism and discrimination, and historical and social trauma that members of this group have experienced through generations (Brave Heart et al., 2011, Whitesell et al., 2012). Historical trauma includes multigenerational forced assimilation, such as removal from native lands, coerced placement of children into boarding schools, and laws prohibiting indigenous practices (Brave Heart, Chase, 2011, Duran et al., 1998, Evans-Campbell, 2008, Whitesell, Beals, 2012). These traumatic experiences may have both specific and cumulative effect on the mental health of AI/AN individuals (Brave Heart, Chase, 2011, Duran, Duran, 1998). For instance, social factors such as experiencing racial discrimination has been associated with problematic gambling among Aboriginal populations (Currie et al., 2013). Specifically, experiencing racial discriminations led to subjective distress among AI/AN individuals, leading to engagement in problematic gambling to escape negative emotional reactions to these experiences.
The role of gambling is particularly complex within the contemporary AI/AN communities because of economic ties to casinos that exist on some AI/AN reservations. Approximately, 240 of the 562 AI/AN tribes in 28 states operate some level of gambling facilities (National Indian Gaming Commission, 2011). Gambling facilities allowed on native lands offer opportunity for economic growth as well as positive social change by providing job opportunities and decreasing rates of poverty (Evans and Topoleski, 2002, Gerdes et al., 1997). The Indian Gaming Regulatory Act (Public Law 100-497-Oct 17, 1988 100th Congress Sec 2701) mandates that profits from gambling operations on reservations (1) fund tribal government operations or programs, (2) provide for the general welfare of the Indian Tribe and its members, (3) promote tribal economic development, (4) donate to charitable organizations, (5) help fund operations of local government agencies, or (6) be used when the above are adequately provided for a revenue allocation plan. The potential economic benefits made possible by gambling facilities are particularly important for AI/AN communities because their poverty rates double those of the general population, and the poverty rates are even higher for individuals living on reservations and rural locations (DeVoe and Darling-Churchill, 2008). However, despite the opportunity for positive economic growth and social benefits, the outcome is controvertible. Economic analyses show that casinos on reservations increase employment and health benefits and decrease poverty rates; however, the increase in economic growth appears to be driven by non-AI/AN employment (Evans and Topoleski, 2002). Furthermore, AI/AN communities surrounding casinos experience higher bankruptcy and reports of crimes (Evans and Topoleski, 2002). There is also a concern that the increased number of gambling facilities may increase the risk for gambling-related pathology. Thus, an examination of disordered gambling among AI/AN groups continues to be an important public-health objective.
Despite the unique role of gambling enterprises on native lands, relatively few studies have examined the prevalence and patterns of disordered gambling in the context of other psychiatric disorders among AI/AN individuals in the USA. This examination is important given that population studies have shown high rates of co-occurrence of psychiatric disorders with disordered gambling (Chou and Afifi, 2011, Lorains et al., 2011, Petry et al., 2005).
The few existing studies examining psychiatric comorbidity with disordered gambling among AI/AN groups indicate that AI/AN individuals with PG may experience higher rates of comorbidity relative to non-AI/AN individuals. For example, AI/AN adults receiving treatment for alcohol dependence were more likely to also have PG (22%) compared to white/Caucasian adults receiving similar alcohol-related treatment (7.3%) (Elia and Jacobs, 1993). Another study showed that the prevalence of lifetime Axis-I disorder among AI/AN and Hispanic veterans with PG was 70% compared to 46% among those without PG (Westermeyer, Canive, 2005). Given these studies findings that show comorbidity between problem-gambling severity and psychiatric disorders in samples of AI/AN individuals, there is a need to examine this association among a nationally representative sample of AI/AN individuals to assess whether these high associations detected in previous studies are not artifact of sampling limitation. An important shortcoming of the literature examining AI/AN individuals is that sampling is limited to rural reservations and specific tribes, which limits the generalizability of the findings (Atkins et al., 2013). Additionally, comparative analyses examining AI/AN groups with other ethnic/racial groups have been generally difficult because of the small sample size and reliance on convenience samples.
In this study, we sought to examine the associations between problem-gambling severity and psychiatric disorders among AI/AN and other American adults using the data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study. We hypothesized that (1) AI/AN relative to other American adults would display higher rates of problem-gambling severity, (2) problem-gambling severity would be associated with psychiatric disorders in all Americans, including AI/AN adults, and (3) these associations would be stronger among AI/AN relative to other American adults.
Methods
Participants
We analyzed the data from the NESARC (2001–2002). Detailed methods are described elsewhere (e.g., Grant et al., 2004, Grant et al., 2003b). In brief, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the US Census Bureau sampled a nationally representative group of US citizens and non-citizens aged 18 and older. Respondents were interviewed in their homes by trained research staff. The NESARC study over-sampled Hispanic and African American households, as well as individuals aged 18 to 24, to allow for sufficient statistical power to perform meaningful statistical analyses on these populations. Multi-stage cluster sampling identified respondents by first sampling Census sampling units, followed by households, and then household members. Although individuals residing in jails, prisons, or hospitals were not included, members of group living environments, such as group homes, shelters, dormitories, and facilities for housing workers were sampled. Weights have been calculated to adjust for standard errors for these over-samples, the cluster sampling strategy, and non-responses (Grant, Moore, 2003b). The final sample size was 43,093 (response rate of 81%). All participants provided written consent prior to the study. The current study was exempt from a formal Institutional Review Board review because NESARC is publicly accessible, de-identified data (http://pubs.niaaa.nih.gov/publications/NESARC_DRM/NESARCDRM.htm).
Measures
Sociodemographics variables included gender, race (American-Indian/Alaska-Native, white/Caucasian), age, education level (less than high school, high school, some college, college graduate or higher), and marital status (married, formerly married, never married), employment status (full time, part time, not working), and income.
Axis-I and Axis-II diagnostic categories were determined by trained lay interviewers using a structured diagnostic interview, the Alcohol Use Disorder and Associated Disability Interview Schedule-DSM-IV version (AUDADIS-IV) (American Psychiatric Association, 2000, Grant et al., 2003a). The AUDADIS-IV has demonstrated good reliability and validity for detecting psychiatric disorders in a community sample (Grant, Dawson, 2003a). The NESARC data contain past-year measures of DSM-IV Axis-I diagnostic variables for mood disorders (major depression, dysthymia, mania, hypomania), anxiety disorders (panic disorder with or without agoraphobia, social phobia, simple phobia, generalized anxiety disorder), and substance-use disorders (alcohol abuse/dependence, drug abuse/dependence, nicotine dependence), and lifetime measures for DSM-IV Axis-II cluster-A (paranoid, schizoid), cluster-B (histrionic, antisocial), and cluster-C (avoidant, dependent, obsessive-compulsive) personality disorders.
Problem-Gambling Groups were determined based on the 10 DSM-IV diagnostic inclusionary criteria for pathological gambling and gambling-related items on the AUDADIS-IV as previously done (Barry et al., 2011a, b, Desai and Potenza, 2008). We classified participants as either (1) non-gambling/low-frequency gambling (NG; i.e., reporting not gambling more than five times per year in their lifetime), (2) low-risk gambling (LRG; i.e., reporting gambling more than five times in a year and endorsing 0 to 2 inclusionary criteria for pathological gambling in the previous year), (3) at-risk, problem or pathological gamblers (ARPG; i.e., reporting three or more inclusionary criteria of pathological gambling in the previous year).
Data Analysis
We conducted all analyses using Stata 13.1 (StataCorp, 2013). All analyses accounted for the NESARC sampling design and were weighted to generate nationally representative estimates. To compare the associations between problem-gambling severity and psychiatric disorders between AI/AN and other American adults, we compared AI/AN groups to three separate groups of American adults (i.e., black/African American, white/Caucasian, all other ethnicity/race other than AI/AN). The analyses comparing AI/AN to black/African American adults had a sample size of 8679, AI/AN to white/Caucasian had a sample size of 24,599, and AI/AN to all other racial/ethnic categories had a sample size of 42,027. Participants who reported race and provided valid gambling data were included in the analyses.
First, we conducted a Wald test to assess whether problem-gambling severity (i.e., NG, LRG, ARPG) differed by race (e.g., AI/AN vs. white/Caucasian). Second, we conducted Wald tests (for categorical variables) or mean comparisons (for continuous variables) to assess bivariate associations between problem-gambling severity and sociodemographic characteristics (i.e., gender, marital status, education, employment, income, age) stratified by race. Third, we conducted Wald tests to examine bivariate associations between NESARC-calculated weighted percentages of psychiatric disorders by race and problem-gambling-severity groups. Fourth, we fit a series of logistic regression models with each psychiatric disorder (see Table 2 and 3 for the list of disorders) as a separate dependent variable, problem-gambling severity, race, and the interaction between race and problem-gambling severity as the independent variables, and sociodemographic variables as the covariates.
Table 2.
Bivariate associations between psychiatric disorders and gambling severity, by race
| American-Indian/Alaska-Native (n=679) | White/Caucasian (n=23,920) | |||||||
|---|---|---|---|---|---|---|---|---|
| NG (n=461; 66.59% | LRG (n=190; 30.14%) | ARPG (n=28; 3.37%) | p | NG (n=17,022; 70.51%) | LRG (n=6230; 26.50%) | ARPG (n=676; 2.99%) | p | |
| % | % | % | % | % | % | |||
| Any psychiatric disorder | 41.57 | 63.00 | 91.82 | <0.001 | 32.82 | 42.64 | 63.58 | <0.001 |
| Any Axis-I disorder | 36.13 | 54.06 | 85.85 | <0.001 | 27.86 | 36.12 | 53.84 | <0.001 |
| Any mood disorder | 14.41 | 16.86 | 27.01 | 0.083 | 9.43 | 9.16 | 16.31 | <0.001 |
| Depression | 11.23 | 15.25 | 17.81 | 0.080 | 7.65 | 6.73 | 11.12 | <0.001 |
| Dysthymia | 3.51 | 1.43 | 4.81 | 0.018 | 1.84 | 1.93 | 2.63 | 0.1748 |
| Mania | 2.45 | 2.63 | 6.36 | 0.602 | 1.55 | 1.89 | 3.25 | <0.001 |
| Hypomania | 2.29 | 1.26 | 5.44 | <0.001 | 1.04 | 1.24 | 2.92 | <0.001 |
| Any anxiety disorder | 14.05 | 18.64 | 26.47 | 0.046 | 11.24 | 12.87 | 21.2 | <0.001 |
| Panic disordera | 5.07 | 4.30 | 4.46 | 0.736 | 2.25 | 2.08 | 7.30 | <0.001 |
| Social phobia | 4.07 | 2.25 | 9.23 | 0.087 | 2.96 | 3.16 | 5.27 | <0.001 |
| Specific phobia | 7.33 | 10.18 | 16.22 | 0.011 | 7.05 | 8.61 | 14.44 | <0.001 |
| Generalized-Anxiety disorder | 1.56 | 4.98 | 6.03 | <0.001 | 2.16 | 2.35 | 3.10 | 0.044 |
| Any substance-use disorder | 22.88 | 39.44 | 67.08 | <0.001 | 15.81 | 24.06 | 39.93 | <0.001 |
| Alcohol abuse/dependence | 9.37 | 14.84 | 33.85 | 0.003 | 7.26 | 11.72 | 24.29 | <0.001 |
| Drug abuse/dependence | 2.93 | 3.17 | 10.85 | 0.108 | 1.34 | 1.83 | 4.37 | <0.001 |
| Nicotine dependence | 17.99 | 32.99 | 56.14 | <0.001 | 12.14 | 18.36 | 32.72 | <0.001 |
| Any Axis-II disorder | 19.93 | 34.27 | 42.35 | <0.001 | 13.41 | 17.00 | 34.01 | <0.001 |
| Cluster Ab | 11.73 | 16.91 | 15.56 | 0.120 | 5.11 | 5.89 | 14.04 | <0.001 |
| Schizoid PD | 5.06 | 9.58 | 8.60 | 0.092 | 2.52 | 3.22 | 7.18 | <0.001 |
| Paranoid PD | 9.50 | 14.04 | 13.71 | 0.120 | 3.45 | 3.73 | 10.67 | <0.001 |
| Cluster Bc | 8.42 | 19.16 | 14.96 | <0.001 | 4.17 | 6.10 | 14.67 | <0.001 |
| Antisocial PD | 5.92 | 18.85 | 13.10 | <0.001 | 2.95 | 4.77 | 11.30 | <0.001 |
| Histrionic PD | 2.98 | 0.30 | 12.12 | <0.001 | 1.61 | 1.80 | 5.76 | <0.001 |
| Cluster Cd | 10.99 | 14.21 | 27.12 | 0.054 | 9.13 | 11.00 | 20.34 | <0.001 |
| Dependent PD | 0.64 | 0.29 | 0.00 | 0.004 | 0.55 | 0.46 | 0.80 | 0.032 |
| Avoidant PD | 3.70 | 4.47 | 2.58 | 0.752 | 2.60 | 1.83 | 5.92 | <0.001 |
| Obsessive-Compulsive PD | 9.22 | 11.22 | 24.54 | 0.143 | 7.59 | 9.85 | 17.13 | <0.001 |
Note. NG=no gambling or low-frequency gambling, LRG=low-risk gambling, ARPG=at-risk, problem, or pathological gambling, PD=personality disorder. Sample sizes were based on the raw data, while percentages, means, and tests of significance accounted for the sampling design and were weighted to generate nationally representative estimates. Frequencies were compared using Wald tests, and means were compared using regression modeling.
With or without agoraphobia
Schizoid or paranoid personality disorder
Antisocial or histrionic personality disorder
Dependent, avoidant, or obsessive-compulsive personality disorder
Table 3.
Adjusted associations between psychiatric disorders and gambling severity, by race
| American Indian/Alaska Native (n=679) | White/Caucasian (n=23,920) | Interaction OR (American- Indian/Alaska-Native vs. White/Caucasian) | ||||
|---|---|---|---|---|---|---|
| LRG vs. NG | ARPG vs. NG | LRG vs. NG | ARPG vs. NG | LRG vs. NG | ARPG vs. NG | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Any psychiatric disorder | 2.59 (2.10, 3.19) | 14.19 (8.88, 22.68) | 1.67 (1.61, 1.73) | 3.52 (3.30, 3.75) | 1.56 (1.27, 1.91) | 4.20 (2.87, 6.15) |
| Any Axis-I disorder | 2.40 (1.93, 2.98) | 9.96 (6.08, 16.32) | 1.64 (1.58, 1.71) | 2.98 (2.73, 3.26) | 1.40 (1.14, 1.72) | 3.39 (2.22, 5.17) |
| Any mood disorder | 1.41 (1.02, 1.96) | 1.93 (0.84, 4.41) | 1.17 (1.09, 1.25) | 1.98 (1.77, 2.23) | 1.17 (0.82, 1.67) | 1.05 (0.51, 2.17) |
| Major depression | 1.68 (1.20, 2.37) | 1.57 (0.64, 3.83) | 1.06 (0.99, 1.15) | 1.64 (1.40, 1.91) | 1.55 (1.05, 2.28) | 1.01 (0.45, 2.30) |
| Dysthymia | 0.46 (0.24, 0.87) | 1.60 (0.32, 8.04) | 1.25 (1.08, 1.44) | 1.50 (1.07, 2.12) | 0.34 (0.17, 0.65) | 0.92 (0.20, 4.29) |
| Mania | 1.02 (0.38, 2.73) | 2.39 (0.64, 8.91) | 1.47 (1.27, 1.71) | 2.05 (1.41, 2.99) | 0.80 (0.38, 1.68) | 1.27 (0.32, 5.13) |
| Hypomania | 0.98 (0.61, 1.57) | 3.24 (1.61, 6.52) | 1.47 (1.23, 1.77) | 2.58 (1.94, 3.42) | 0.47 (0.30, 0.73) | 0.55 (0.26, 1.14) |
| Any anxiety disorder | 1.58 (1.13, 2.20) | 2.98 (1.21, 7.30) | 1.37 (1.29, 1.44) | 2.42 (2.15, 2.72) | 1.17 (0.88, 1.55) | 1.04 (0.46, 2.36) |
| Panic disorder | 0.88 (0.49, 1.58) | 1.06 (0.11, 10.01) | 1.13 (1.00, 1.28) | 3.89 (3.19, 4.74) | 0.82 (0.53, 1.26) | 0.26 (0.03, 2.17) |
| Social phobia | 0.60 (0.15, 2.45) | 2.65 (1.17, 5.97) | 1.22 (1.07, 1.39) | 1.89 (1.55, 2.29) | 0.50 (0.13, 1.95) | 1.28 (0.63, 2.63) |
| Specific phobia | 1.68 (1.30, 2.18) | 2.83 (1.10, 7.24) | 1.47 (1.36, 1.59) | 2.60 (2.27, 2.97) | 1.12 (0.89, 1.40) | 1.13 (0.39, 3.25) |
| Generalized-anxiety disorder | 3.84 (2.14, 6.89) | 6.99 (2.22, 22.02) | 1.30 (1.17, 1.44) | 1.58 (1.14, 2.19) | 2.85 (1.67, 4.84) | 2.81 (0.94, 8.41) |
| Any substance-use disorder | 2.34 (1.89, 2.89) | 6.39 (2.73, 14.98) | 1.81 (1.72, 1.91) | 3.18 (2.88, 3.51) | 1.30 (1.03, 1.63) | 1.89 (0.85, 4.20) |
| Alcohol abuse/dependence | 1.92 (1.18, 3.12) | 3.75 (2.36, 5.94) | 1.81 (1.69, 1.94) | 3.55 (3.11, 4.05) | 1.02 (0.64, 1.62) | 1.05 (0.62, 1.80) |
| Drug abuse/dependence | 1.20 (0.82, 1.76) | 4.50 (1.64, 12.32) | 1.71 (1.51, 1.94) | 2.74 (2.05, 3.65) | 0.84 (0.52, 1.13) | 0.87 (0.26, 2.84) |
| Nicotine dependence | 2.36 (1.95, 2.86) | 5.18 (2.24, 12.13) | 1.77 (1.67, 1.87) | 3.21 (2.88, 3.58) | 1.37 (1.09, 1.73) | 1.58 (0.71, 3.54) |
| Any Axis-II disorder | 2.12 (1.65, 2.74) | 2.30 (0.98, 5.37) | 1.39 (1.33, 1.47) | 2.19 (2.92, 3.49) | 1.57 (1.23, 2.02) | 0.86 (0.36, 2.01) |
| Cluster Ab | 1.65 (1.06, 2.56) | 1.04 (0.59, 1.85) | 1.28 (1.19, 1.37) | 2.94 (2.61, 3.30) | 1.28 (0.81, 2.03) | 0.42 (0.24, 0.72) |
| Schizoid PD | 2.01 (1.15, 3.52) | 1.41 (0.70, 2.84) | 1.36 (1.24, 1.51) | 2.92 (2.43, 3.50) | 1.52 (0.84, 2.77) | 0.58 (0.29, 1.19) |
| Paranoid PD | 1.62 (0.96, 2.72) | 1.13 (0.61, 2.12) | 1.25 (1.14, 1.36) | 3.22 (2.78, 3.74) | 1.39 (0.82, 2.38) | 0.41 (0.23, 0.74) |
| Cluster Bc | 2.61 (1.92, 3.55) | 1.57 (0.56, 4.37) | 1.55 (1.43, 1.68) | 3.28 (2.88, 3.74) | 1.77 (1.33, 2.36) | 0.41 (0.15, 1.14) |
| Antisocial PD | 3.89 (2.68, 5.65) | 2.04 (0.69, 6.05) | 1.63 (1.48, 1.80) | 3.22 (2.79, 3.73) | 2.40 (1.71, 3.39) | 0.50 (0.16, 1.53) |
| Histrionic PD | 0.09 (0.05, 0.15) | 4.61 (1.15, 18.46) | 1.32 (1.18, 1.48) | 3.52 (2.86, 4.34) | 0.08 (0.05, 0.14) | 1.07 (0.35, 3.23) |
| Cluster Cd | 1.38 (0.99, 1.91) | 2.32 (0.99, 5.42) | 1.31 (1.22, 1.40) | 2.57 (2.25, 2.95) | 1.08, 0.77, 1.51) | 1.18 (0.46, 3.07) |
| Dependent PD | 0.57 (0.07, 4.98) | ---e | 1.06 (0.86, 1.29) | 1.46 (0.84, 2.55) | 0.50 (0.06, 3.97) | ---e |
| Avoidant PD | 1.40 (0.74, 2.66) | 0.59 (0.08, 4.07) | 0.83 (0.74, 0.94) | 2.36 (1.89, 2.95) | 1.69 (0.88, 3.23) | 0.26 (0.03, 1.98) |
| Obsessive-Compulsive PD | 1.20 (0.82, 1.77) | 2.45 (1.00, 5.97) | 1.38 (1.28, 1.48) | 2.57 (2.23, 2.96) | 0.93 (0.63, 1.38) | 1.34 (0.49, 3.67) |
Note. NG=no gambling or low-frequency gambling, LRG=low-risk gambling, ARPG=at-risk, problem, or pathological gambling. Sample sizes were based on the raw data, while percentages, means, and tests of significance accounted for the sampling design and were weighted to generate nationally representative estimates. Odds ratios and 95% confidence intervals were calculated using logistic regression. All analyses controlled for gender, marital status, education, employment, income, and age.
With or without agoraphobia
Schizoid or paranoid personality disorder
Antisocial or histrionic personality disorder
Dependent, avoidant, or obsessive-compulsive personality disorder
Omitted because there were zero American-Indian/Alaska-Native respondents with ARPG and dependent personality disorder.
All analyses comparing AI/AN to black/African American, white/Caucasian, and all other racial/ethnic groups yielded comparable results so we provided the results comparing AI/AN and white/Caucasian to allow for direct comparisons with other NESARC publications that have also used white/Caucasian as a reference group (e.g., Barry et al., 2011a, b; Desai and Potenza, 2008). All results comparing AI/AN to black/African American and all other racial/ethnic groups are reported in the supplemental materials unless stated otherwise.
Results
A Wald test demonstrated a significant difference in the distribution of problem-gambling severity between AI/AN and white/Caucasian adults (Wald F=3.83, p=0.03). Among white/Caucasian adults, 70.5% were NG, 26.5% were LRG, and 3.0% were ARPG. In comparison, among AI/AN adults, 66.5% were NG, 30.1% were LRG, and 3.4% were ARPG. AI/AN status was associated with 21% greater odds of LRG (vs. NG) compared to white/Caucasian (OR=1.21, 95% CI=1.06, 1.38). The association between racial group and ARPG (vs. NG) was similar to the effect size found between racial group and LRG (vs. NG), but non-significant (OR=1.20, 95% CI=0.87, 1.64).
There was a significant difference between racial groups in education (Wald F=20.87, p<0.001): AI/AN adults were more likely to have less than a high-school education (19.9% vs. 11.2%, p<0.05) and less likely to have a college degree or greater education (16.4% vs. 27.5%, p< 0.05). AI/AN adults also had lower incomes than white/Caucasian adults (Wald F=36.76, p<0.001): AI/AN adults were more likely to be in the lowest income category ($0–$19,999; 29.7% vs. 18.4%, p<0.05), and less likely to be in the highest income category ($70,000+; 28.7% vs. 15.4%, p<0.05). On average, AI/AN adults were 1.65 years younger than white/Caucasian adults (M=45.36, SD=14.56 vs. M=47.01, SD=15.98; t=−4.67, p< 0.05). There was no difference between AI/AN and white/Caucasian adults in gender (Wald F=1.06, p=0.31), working status (Wald F=1.94, p=0.15), and marital status (Wald F=1.80, p=0.17).
Table 1 displays bivariate associations between sociodemographic characteristics and problem-gambling severity, stratified by AI/AN and white/Caucasian groups. Sociodemographics varied by problem-gambling-severity groups for all variables among both AI/AN and white/Caucasian groups, although among the AI/AN group not all differences reached statistical significance (p-values ranged from <0.001 to 0.094). Among both racial groups, the most pronounced differences were observed between NG and ARPG groups, where ARPG adults were more likely to be male (AI/AN: 60.0% vs. 41.8%; white/Caucasian: 64.2% vs. 43.6%) and less likely to be married (AI/AN: 44.0% vs. 65.3%; white/Caucasian: 58.5% vs. 63.6%). ARPG adult were also younger than NG adults (AI/AN: M=39.92, SD=15.34 vs. M =44.74, SD=15.17; white/Caucasian: M=44.01, SD=14.46 vs. M=46.49, SD=16.37).
Table 1.
Bivariate associations between sociodemographic characteristics and gambling severity, by race
| American Indian/Alaska Native (n=679) | White/Caucasian (n=23,920) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NG (n=461; 66.49% | LRG (n=190; 30.14%) | ARPG (n=28; 3.37%) | p | NG (n=17,022; 70.51%) | LRG (n=6230; 26.50%) | ARPG (n=676; 2.99%) | p | |||||||
| n or mean | % or SD | n or mean | % or SD | n or mean | % or SD | n or mean | % or SD | n or mean | % or SD | n or mean | % or SD | |||
| Gender | <0.001 | <0.001 | ||||||||||||
| Male | 187 | 41.84 | 98 | 56.13 | 15 | 60.04 | 6,782 | 43.55 | 3,376 | 58.12 | 402 | 64.21 | ||
| Female | 274 | 58.16 | 92 | 43.87 | 13 | 39.96 | 10,240 | 56.45 | 2,846 | 41.88 | 274 | 35.79 | ||
| Education | 0.061 | <0.001 | ||||||||||||
| Less than high school | 95 | 19.72 | 37 | 19.82 | 7 | 23.16 | 2,041 | 11.43 | 678 | 10.50 | 98 | 13.20 | ||
| High school | 146 | 31.60 | 59 | 31.61 | 12 | 51.94 | 4,908 | 29.27 | 1,956 | 31.73 | 227 | 35.09 | ||
| Some college | 133 | 30.71 | 66 | 34.07 | 8 | 21.99 | 5,099 | 30.54 | 2,030 | 32.78 | 227 | 33.31 | ||
| College + | 87 | 17.97 | 28 | 14.50 | 1 | 2.91 | 4,974 | 28.75 | 1,558 | 24.99 | 124 | 18.39 | ||
| Employment | 0.065 | <0.001 | ||||||||||||
| Full time | 222 | 49.14 | 93 | 49.87 | 13 | 52.17 | 8,334 | 51.07 | 3,243 | 58.15 | 369 | 52.37 | ||
| Part time | 51 | 10.42 | 23 | 12.96 | 6 | 21.56 | 1,859 | 11.46 | 614 | 10.67 | 70 | 11.12 | ||
| Other | 188 | 40.44 | 74 | 37.17 | 9 | 26.27 | 6,829 | 37.47 | 2,365 | 31.18 | 237 | 36.51 | ||
| Marital Status | <0.001 | <0.001 | ||||||||||||
| Married | 251 | 65.30 | 108 | 64.42 | 13 | 44.02 | 9,192 | 63.56 | 3,583 | 67.50 | 340 | 58.50 | ||
| Previously married | 115 | 17.26 | 56 | 23.84 | 5 | 14.37 | 4,522 | 17.62 | 1,666 | 18.05 | 173 | 17.85 | ||
| Never married | 95 | 17.44 | 26 | 11.74 | 10 | 41.61 | 3,308 | 18.81 | 973 | 14.44 | 163 | 23.64 | ||
| Income | 0.094 | |||||||||||||
| $0–19,999 | 159 | 31.06 | 57 | 27.42 | 9 | 24.54 | 4,156 | 19.89 | 1,184 | 14.35 | 151 | 17.77 | <0.001 | |
| $20,000–34,999 | 100 | 20.24 | 45 | 21.27 | 7 | 31.05 | 3,460 | 18.80 | 1,306 | 18.83 | 144 | 19.87 | ||
| $35,000–69,999 | 137 | 32.26 | 63 | 37.68 | 7 | 34.63 | 5,393 | 33.33 | 2,167 | 36.42 | 208 | 31.77 | ||
| ≥$70,000 | 65 | 16.44 | 25 | 13.64 | 5 | 9.78 | 4,013 | 27.98 | 1,565 | 30.40 | 173 | 30.58 | ||
| Age | 44.74 | 15.17 | 47.35 | 15.92 | 39.92 | 15.34 | 0.007 | 46.49 | 16.37 | 49.73 | 14.96 | 44.01 | 14.46 | <0.001 |
Note. NG=no gambling or low-frequency gambling, LRG=low-risk gambling, ARPG=at-risk, problem, or pathological gambling. Sample sizes were based on the raw data, while percentages, means, and tests of significance accounted for the sampling design and were weighted to generate nationally representative estimates. Frequencies were compared using Wald tests, and means were compared using regression modeling.
Table 2 displays bivariate associations between psychiatric disorders and problem-gambling severity, stratified by AI/AN and white/Caucasian groups. Among AI/AN adults, differences in psychiatric disorder frequencies by problem-gambling severity reached significance at p<0.05 for “any psychiatric disorder”, “any Axis-I disorder”, “any Axis-II disorder,” “any anxiety disorder,” “any substance-use disorder,” Cluster-B personality disorder, and the following specific disorders: dysthymia, hypomania, specific phobia, generalized anxiety, alcohol use disorder, nicotine dependence, antisocial personality disorder, histrionic personality disorder, and dependent personality disorder. Among the white/Caucasian (Table 2), black/African American (Supplemental Table 2), and all other racial/ethnic adults (Supplemental Table 4), differences reached significance at p<0.05 for “any psychiatric disorder”, “any Axis-I disorder”, “any Axis-II disorder,” “any anxiety disorder,” “any substance-use disorder,” and all individual disorders, with the exception of Dysthymia only among white/Caucasian adults. There was a general trend whereby those in the LRG group had greater frequencies of psychiatric disorders than the NG group, and ARPG had the highest frequencies. For example, among the AI/AN group, 41.57% of the NG group had any psychiatric disorder, compared to 63.00% of the LRG group and 91.82% of the ARPG group. The corresponding estimates for the white/Caucasian group were as follows: NG 32.82%, LRG 42.64%, and ARPG 63.58%.
Table 3 displays adjusted associations between psychiatric disorders and problem-gambling severity, stratified by AI/AN and white/Caucasian. The table also includes tests of whether the strengths of the associations between problem-gambling severity and psychiatric diagnoses differed between racial groups. There were notable findings. First, higher rates of psychiatric disorders among those in the LRG and ARPG groups compared to the NG group tended to remain significant after adjustment for sociodemographic covariates. Second, although both LRG and ARPG were associated with any psychiatric diagnosis compared to NG for all race groups, problem-gambling severity was more strongly associated with “any psychiatric diagnosis” for the AI/AN group (OR=14.19) than the white/Caucasian group (OR=3.52), black/African American group (OR=4.46), and all other race group (OR=3.79). Furthermore, problem-gambling severity was also more strongly associated with “any Axis-I disorder” for the AI/AN group (OR=9.96) compared to the white/Caucasian group (OR=2.98), black/African American group (OR=4.68), and all other race groups (OR=3.31). Additionally, the association between LRG (versus NG) and “any Axis-II disorder” was stronger in AI/AN (OR=2.12) than in white/Caucasian adults (OR=1.39), black/African American group (OR=1.52), and all other race groups (OR=1.66). Third, in the case of LRG but not ARPG, the findings appeared to be driven by specific groups of disorders or individual disorders. Specifically, the stronger relationship between LRG and Axis-I disorders in AI/AN versus all American adults were linked to major depression (AI/AN OR=1.68, white/Caucasian OR=1.06, black/African/American OR=1.32, all other race group OR=1.44, n/s), generalized-anxiety disorder (AI/AN OR=3.84, white/Caucasian OR=1.30, black/African/American OR=2.72, all other race group OR=2.52), and nicotine dependence (AI/AN OR=2.36, white/Caucasian OR=1.77, black/African/American OR=1.69, all other race group OR=1.37). The stronger relationship between LRG and Axis-II disorders in AI/AN versus American adults appeared linked to Cluster-B disorders (OR=2.61 vs. OR=1.55 AI/AN OR=2.61, white/Caucasian OR=1.55, black/African/American OR=2.14, all other race group OR=1.55), and specifically antisocial personality disorder (AI/AN OR=3.89, white/Caucasian OR=1.63, black/African/American OR=2.20, all other race group OR=1.90).
Discussion
We assessed the associations between problem-gambling severity and psychiatric conditions among American-Indian/Alaska-Native (AI/AN) and other Americans using a nationally representative sample in the USA. As hypothesized, problem-gambling severity was higher among AI/AN adults relative to other American adults, but this difference was more evident at the low-risk gambling (LRG) severity level and did not extend to at-risk, problematic gambling (ARPG).
We also observed that problem-gambling severity was associated with many psychiatric disorders in both AI/AN and other American adults. However, the number of statistically significant associations between problem-gambling severity and psychiatric disorders were greater among other American respondents than AI/AN ones. It is likely that sample size is an important consideration in this regard, with some of the associations among AI/AN adults failing to show statistical significance due to small cell sizes as comparison to those for other American group. Therefore, future studies with larger AI/AN samples are needed. Despite the small cell sizes, we detected stronger associations between having any psychiatric disorder and LRG and ARPG among AI/AN adults than among American adults, even after controlling for demographic covariates. Specific psychiatric disorders, particularly major depression, generalized-anxiety disorder, nicotine dependence and antisocial personality disorder seem important to consider as they relate to problem-gambling severity in AI/AN groups. As problem/pathological gambling has shown genetic and/or environmental links to major depression (Potenza et al., 2005), generalized anxiety disorder (Giddens et al., 2011), nicotine dependence (Xian et al., 2014) and antisocial personality disorder (Slutske et al., 2001), identifying the specific factors influencing these particular relationships in AI/AN (as well as white/Caucasian) individuals is important.
Our findings also underscore the need for research approaches to identify improved intervention strategies for AI/AN individuals to reduce the disproportionate burden of psychiatric concerns in this group. Specifically, development of historical trauma interventions that can alleviate psychological suffering and unresolved grief to improve behavioral health of AI/AN individuals may have be relevant and important for AI/AN individuals given the role of historical trauma in current and cumulative effect on their mental health (Brave Heart, Chase, 2011). Furthermore, interventions based on framework that focuses on strengths of the indigenous groups, such as culture-specific stress-coping strategies that include a development of positive ethnic identity through enculturation (a process in which individuals identify with their culture and participate in their traditional ethnic cultural practices (Zimmerman et al., 1996)), as well as engagement in cultural traditional healing practices (Buchwald et al., 2000) could also have utility.
The finding that ARPG rates among AI/AN adults were comparable to the rates of American adults is inconsistent with existing studies that found that AI/AN have disproportionately elevated rates of disordered gambling (Patterson-Silver Wolf, Welte, 2014, Volberg and Bernhard, 2006, Wardman, el-Gudebaly, 2001, Westermeyer, Canive, 2005). This finding suggests that while more problematic gambling exists in certain AI/AN communities, it is not pervasive within all AI/AN communities. The higher problem and pathological gambling rates reported in other studies may be due to sampling differences and the use of different measures to assess disordered gambling. Alternatively, the findings of this study may point to the unique protective cultural factors that buffer AI/AN individuals from severe disordered gambling or perhaps represent a positive social and economic benefits received by these individuals as a result of gambling facilities. However, we did not assess these factors in this study and future studies should continue to assess the role of gambling on mental health in AI/AN communities.
Despite the comparable ARPG rates between AI/AN and white/Caucasian groups, we found that AI/AN respondents were more likely to engage in LRG than were other American respondents. Furthermore, LRG was more strongly associated with any psychiatric disorder among AI/AN compared to other American respondents. We also found that the association between any psychiatric disorder and no gambling or low frequency group among AI/AN individuals was higher than in other American adults, suggesting greater experiencing of psychiatric concerns independent of elevated problem-gambling severity. Together, the findings underscore the need to expand the focus of gambling treatment and research to include not only problem or pathological gambling but also on lesser levels of problem-gambling severity (low or “none”) when considering the psychiatric needs of AI/AN individuals. Future studies should examine whether low levels of gambling may exacerbate psychiatric conditions among AI/AN individuals and examine how gambling-related interventions may affect psychiatric conditions. Finally, studies should examine the extent to which psychiatric conditions may lead to risky or problematic gambling and the impact that this may have on quality of life, particularly among AI/AN individuals.
The current findings should be interpreted in light of limitations. First, we classified AI/AN respondents as a homogenous group; however, AI/AN groups are heterogeneous with varying tribal affiliations with different cultural norms. Second, even though the NESARC captured a representative sample of US adults in terms of age, geographic location, military, and community housing settings, it did not capture whether AI/AN individuals lived on or off reservations and their tribal affiliations. Living on a reservation has been shown to be associated with PG (Hewitt, 1994). Residential and workplace locations may be determinants of disordered gambling among AI/AN individuals and should be assessed in future studies. Third, despite the use of large nationally representative data, the interaction analyses for specific disorders may have been underpowered to detect significant differences by AI/AN vs. race groups due to relatively small sample sizes for AI/AN respondents. However, the comparable associations between problem-gambling severity and psychiatric disorders observed across AI/AN and three different comparison groups (i.e., black/African American, white/Caucasian, all other racial/ethnic group) further strengthen our study findings that showed stronger associations between problem-gambling severity groups and psychiatric disorders among AI/AN adults relative to other American adults. Finally, although we controlled for demographic variables in the logistic regression models, we lacked a broad range of cultural, historical, and contextual measures that might be considered in analyses, as this was a secondary data analysis. Future studies should examine these important factors.
Despite these limitations, we identified potentially important associations between problem-gambling severity and psychiatric disorders among a nationally representative sample of AI/AN adults. Furthermore, we used reliable and valid diagnostic instruments to examine associations between problem-gambling severity and psychiatric disorders among AI/AN and other American adult populations. The findings of stronger associations between problem-gambling severity and psychiatric disorders among AI/AN relative to other American adults suggest the importance of developing clinically innovative interventions that focus on historical trauma, which can alleviate psychological suffering and unresolved grief, to improve the mental health of AI/AN individuals.
Supplementary Material
Acknowledgments
This study was supported by CASAColumbia, the National Center for Responsible Gaming, National Institute of Mental Health 5T32MH014235, and CTSA grants UL1TR000142 and KL2TR000140 from the National Center for Advancing Translational Science (NCATS), components of the National Institutes of Health (NIH), and NIH roadmap for Medical Research.
Role of the Funding Source
The funding agencies had no involvement in the design; collection, analysis, and interpretation of data; the writing of the report; and the decision to submit the article for publication.
Footnotes
Contributors
Drs. Marc Potenza and Corey Pilver conceptualized the current study; Dr. Grace Kong wrote the first draft of the manuscript; Drs. Rani Hoff, Corey Pilver, and Philip Smith analyzed the data; Dr. Philip Smith wrote the results section, Drs. Grace Kong, Philip Smith, and Marc Potenza interpreted the study findings. All authors have read and approved the final article.
Conflicts of Interest
The authors report that they have no financial conflicts of interest with respect to the content of this manuscript. Dr. Potenza has received financial support or compensation for the following: Dr. Potenza has consulted for and advised Somaxon, Boehringer Ingelheim, Lundbeck, Ironwood, Shire, INSYS and RiverMend Health; has received research support from the National Institutes of Health, Veteran’s Administration, Mohegan Sun Casino, the National Center for Responsible Gaming, and Forest Laboratories, Ortho-McNeil, Oy-Control/Biotie, Glaxo-SmithKline, Pfizer, and Psyadon pharmaceuticals; has participated in surveys, mailings or telephone consultations related to drug addiction, impulse control disorders or other health topics; has consulted for gambling entities, law offices and the federal public defender’s office in issues related to impulse control disorders; provides clinical care in the Connecticut Department of Mental Health and Addiction Services Problem Gambling Services Program; has performed grant reviews for the National Institutes of Health and other agencies; has edited or guest-edited journal sections; has given academic lectures in grand rounds, CME events and other clinical or scientific venues; and has generated books or book chapters for publishers of mental health texts. The rest of the authors have no conflicts of interests to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. text revision. [Google Scholar]
- Atkins S, et al. Patterns and correlates of adult American Indian substance use. J Drug Issues. 2013:1–20. [Google Scholar]
- Barry DT, et al. Differences in the associations between gambling problem severity and psychiatric disorders among Black and White adults: Findings from the National Epidemiological Survey on Alcohol and Related Conditions. Am J Addict. 2011a;20:69–77. doi: 10.1111/j.1521-0391.2010.00098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry DT, et al. Gambling problem severity and psychiatric disorder among Hispanic and white adults: Findings from a nationally representative sample. J Psychiatr Res. 2011b;45:404–11. doi: 10.1016/j.jpsychires.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beals J, et al. Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: mental health disparities in a national context. Am J Psychiatry. 2005;162:1723–32. doi: 10.1176/appi.ajp.162.9.1723. [DOI] [PubMed] [Google Scholar]
- Brave Heart MYH, et al. Historical trauma among indigenous peoples of the Americas: concepts, research, and clinical considerations. J Psychoactive Drugs. 2011:43. doi: 10.1080/02791072.2011.628913. [DOI] [PubMed] [Google Scholar]
- Buchwald D, et al. Use of traditional health practices among Native Americans in a primary care setting. Med Care. 2000;38:1191–9. doi: 10.1097/00005650-200012000-00006. [DOI] [PubMed] [Google Scholar]
- Chou K, Afifi TO. Disordered (pathological or problem) gambling and Axis I psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Am J Epidemiol. 2011;173:1289–97. doi: 10.1093/aje/kwr017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie CL, et al. Racial discrimination, post traumatic stress, and gambling problems among urban aboriginal adults in Canada. J Gambl Stud. 2013;29:393–415. doi: 10.1007/s10899-012-9323-z. [DOI] [PubMed] [Google Scholar]
- Desai RA, Potenza MN. Gender differences in the assoications between past-year gambling problems and psychiatric disorders. Social Psychiatry Psychiatr Epidemiol. 2008;43:173–83. doi: 10.1007/s00127-007-0283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVoe JF, Darling-Churchill KE. Status and trends in the education of American Indians and Alaska Natives: 2008. Washington, DC: National Center for Education Statistics, Institute of Education, Sciences, U.S. Department of Education; 2008. [Google Scholar]
- Duran B, et al. Native Americans and the trauma of hisotry. In: Thornton R, editor. Studying Native America: Problems and Prospects in Native American Studies. Madison, WI: University of Wisconisn Press; 1998. [Google Scholar]
- Duran B, et al. Child maltreatment prevalence and mental disorders outcomes among American Indian women in primary care. Child Abuse Negl. 2004;28:131–45. doi: 10.1016/j.chiabu.2003.06.005. [DOI] [PubMed] [Google Scholar]
- Elia C, Jacobs D. The incidence of pathological gambling among Native Americans treated for alcohol dependence. Int J Addict. 1993;28:659–66. doi: 10.3109/10826089309039654. [DOI] [PubMed] [Google Scholar]
- Evans WN, Topoleski JH. The Social and Economic Impact of Native American Casinos. The National Bureau of Economic Research; 2002. Working Paper No. 9198. [Google Scholar]
- Evans-Campbell T. Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. J Interpers Violence. 2008;23:316–38. doi: 10.1177/0886260507312290. [DOI] [PubMed] [Google Scholar]
- Gerdes K, et al. The impact of Indian gaming on economic development. J Poverty. 1997;2:17–30. [Google Scholar]
- Giddens JL, et al. Shared genetic contributions to anxiety disorders and pathological gambling in a male population. J Affect Disord. 2011;132:406–12. doi: 10.1016/j.jad.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gone JP, Trimble JE. American Indian and Alask Native mental health: Diverse perpsectives on enduring disparities. Annu Rev Clin Psychol. 2012;8:131–60. doi: 10.1146/annurev-clinpsy-032511-143127. [DOI] [PubMed] [Google Scholar]
- Grant BF, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnosis modules in a general population sample. Drug Alcohol Depend. 2003a;20:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, et al. Nicotine dependence, subsyndromal and pathological gambling, and other psychiatric disorders: data from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:1107–15. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Grant BF, et al. Source and accuracy statement: wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003b. [Google Scholar]
- Hewitt D. Spirits of bingoland: A study of problem gambling among Alberta native people. Edmonton, Alberta: Nechi Training, Research and Health Promotion Institution; 1994. [Google Scholar]
- Lorains FK, et al. Prevalence of comorbid disorders in problem and pathological gambling: systematic review and meta-analysis of population surveys. Addict. 2011;106:490–8. doi: 10.1111/j.1360-0443.2010.03300.x. [DOI] [PubMed] [Google Scholar]
- National Indian Gaming Commission. Gaming tribe report. 2011. [Google Scholar]
- Norris T, et al. The American Indian and Alaska Native population: 2010. 2010 Census Briefs. 2012:1–21. [Google Scholar]
- Oetzel J, Duran B. Intimate partner violence in American Indian and/or Alaska Native communities: A social ecological framework of determinants and interventions. Am Indian Alsk Native Ment Health Res. 2004;11:49–68. doi: 10.5820/aian.1103.2004.49. [DOI] [PubMed] [Google Scholar]
- Patterson-Silver Wolf DA, et al. Sociocultural influences on gambling and alcohol use among Native Americans in the United States. J Gambl Stud. 2014:1–18. doi: 10.1007/s10899-014-9512-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, et al. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66:564–74. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- Potenza MN, et al. Shared genetic contributions to pathological gambling and major depression in men. Arch Gen Psychiatry. 2005;62:1015–21. doi: 10.1001/archpsyc.62.9.1015. [DOI] [PubMed] [Google Scholar]
- Slutske WS, et al. A twin study of the association between pathological gambling and antisocial personality disorder. J Abnorm Psychol. 2001;110:297–308. doi: 10.1037//0021-843x.110.2.297. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 13.0. College Station, Tx: StataCorp LP; 2013. [Google Scholar]
- Volberg RA, Bernhard BJ. The 2006 Study of Gambling and Problematic Gambling in New Mexico. Albuquerque: 2006. [Google Scholar]
- Wardman D, et al. Problem and pathological gambling in North American aboriginal popultaions: A review of the empirical literature. J Gambl Stud. 2001;17:81–100. doi: 10.1023/a:1016699628402. [DOI] [PubMed] [Google Scholar]
- Westermeyer J, et al. Lifetime prevalence of pathological gambling among American Indian and Hispanic American veterans. Am J Public Health. 2005;95:860–6. doi: 10.2105/AJPH.2003.023770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell NR, et al. Epidemiology and etiology of substance use among American Indians and Alaska Natives: Risk, protection, and implications for prevention. Am J Drug Alcohol Abuse. 2012;38:376–82. doi: 10.3109/00952990.2012.694527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xian H, et al. Environmental factors selectively impact co-occurrence of problem/pathological gambling with specific drug-use disorders in male twins. Addict. 2014;109:635–44. doi: 10.1111/add.12407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman MA, et al. The development of a measure of enculturation for Native American youth. Am J Commun Psychol. 1996;24:295–310. doi: 10.1007/BF02510403. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


