Abstract
Background
Preschool hyperactivity is an early risk factor for adult mental health problems and criminality. Little is known about; (a) the patterns of long‐term service costs associated with this behavioural marker in the general population and (b) the specific factors predicting hyperactivity‐related costs. We undertook a prospective study investigating associations between preschool hyperactivity and average individual annual service costs up to late adolescent and young adulthood.
Methods
One‐hundred and seventy individuals rated as hyperactive by their parents and 88 nonhyperactive controls were identified from a community sample of 4,215 three years olds. Baseline information about behaviour/emotional problems and background characteristics were collected. At follow‐up (when individuals were aged between 14 and 25 years) information was obtained on service use, and associated costs since the age of three. Based on this information we calculated the average cost per annum incurred by each individual.
Results
Compared to controls, preschoolers with hyperactivity had 17.6 times higher average costs per annum across domains (apart from nonmental health costs). These were £562 for each hyperactive individual compared with £30 for controls. Average annual costs decreased as a function of age, with higher costs incurred at younger ages. The effects of hyperactivity remained significant when other baseline factors were added to the model. Effects were fully mediated by later psychiatric morbidity. When the hyperactive group were examined separately, costs were consistently predicted by male gender and, for some cost codes, by conduct problems.
Conclusions
Preventative approaches targeting early hyperactivity may be of value. Services should be targeted towards high‐risk individuals with careful consideration given to the cost‐to‐benefit trade‐off of early intervention strategies.
Keywords: Hyperactivity, ADHD, conduct disorder, longitudinal, preschool children, health economics evaluation
Introduction
ADHD is a common and debilitating neurodevelopment disorder that affects individuals across the life span (Sonuga‐Barke & Taylor, in press). Although, internationally, administrative prevalence varies widely from region to region (Hinshaw et al., 2011), meta‐analysis of population‐based studies suggest little variation between countries in true prevalence once measurement factors are controlled (Polanczyk, de Lima, Horta, Biederman, & Rohde, 2007). The worldwide prevalence was estimated to be 3.2% in a recent meta‐analysis (e.g. Polanczyk, Salum, Sugaya, Caye, & Rohde, 2015). ADHD has a substantial negative impact on daily functioning and achievement in multiple domains (Polderman, Boomsma, Bartels, Verhulst, & Huizink, 2010). In the long term, ADHD is linked to reduced academic performance (Holmberg & Bolte, 2014), more limited employment prospects (Fletcher, 2014), increased risk of criminality (Dalsgaard, Mortensen, Frydenberg, & Thomsen, 2013), substance use (Dunne, Hearn, Rose, & Latimer, 2014), risky sexual behaviour (Sarver, McCart, Sheidow, & Letourneau, 2014) and relationship difficulties (Moya, Stringaris, Asherson, Sandberg, & Taylor, 2014). ADHD in childhood increases the risk of low socio‐economic status (SES) in adult life (Galera et al., 2012). It also negatively impacts on carers and families (Cussen, Sciberras, Ukoumunne, & Efron, 2012). Globally, ADHD is associated with substantial levels of disability and impairment (Erskine et al., 2014) and reduced quality of life (Danckaerts et al., 2010).
ADHD represents a significant economic burden to health, education, social care and criminal justice systems although costs vary substantially from county to country. For instance, in the United States Doshi et al. (2012) reported that ADHD‐related health care sector costs ranged from $21 to 44 billion and educational sector costs from $15 to 25 billion. In the United Kingdom, annual service costs have been estimated at £670 million (Telford et al., 2013). In Germany, Schlander, Trott, and Schwarz (2010), found that direct medical costs for patients with ADHD, exceeded matched controls by a factor of >2.5. In addition to direct health care costs, educational services carried a significant economic burden, on average constituting 45% of total costs. In the Netherlands, education was the largest cost category (Le et al., 2013). Untreated ADHD had a high fiscal burden relating to education in terms of tax revenue losses (Kotsopoulos, Connolly, Sobanski, & Postma, 2013). ADHD is also associated with indirect costs such as higher mental health care costs for the mothers of ADHD patients (Van Roijen, van Straten, Al, Rutten, & Donker, 2006) and loss of family income (Kessler, Lane, Stang, & van Brunt, 2000). Costs are not limited to any particular period of the life span (D'Amico et al., 2014) with evidence of substantial burden even in preschool (Marks et al., 2009).
These high levels of burden and cost reinforce the need for the development and implementation of cost‐effective ADHD treatments (Beecham, 2014). Although it has its developmental roots in the preschool years (Sonuga‐Barke & Halperin, 2010), ADHD is normally first diagnosed and treated in middle to late childhood. A combination of medication (Banaschewski et al., 2006) and psycho‐social treatments (Daley et al., 2014) is recommended. Medications are efficacious and cost effective (NICE, 2009). However, they are limited in a number of ways. For instance, some patients do not respond positively – showing either unmanageable side effects or poor symptom control. Medication may not improve important areas of functioning. Parent/clinicians’ concerns or the restrictive government policies seen in a number of countries may limit access to medications for some patients. For these reasons, the development of effective nonpharmacological treatments is a major health care priority. Recent meta‐analyses, focusing on studies with blinded outcomes, have highlighted the potentially limited value of psychological and dietary approaches (Sonuga‐Barke et al., 2013). Behavioural parent training was, however, of value in relation to co‐occurring conduct problems (Daley et al., 2014) and cognitive training helped ADHD‐related neuropsychological deficits (Cortese et al., 2015). Dietary exclusions and supplements may have a role in some cases (Stevenson et al., 2014).
Given these limitations and constraints there is a possible role for early intervention prevention strategies for ADHD management (Sonuga‐Barke, Koerting, Smith, McCann, & Thompson, 2011). Such approaches would target early signs of difficulty, to prevent the onset of the full disorder and its escalation to more complex presentations (Halperin, Bedard, & Curchack‐Lichtin, 2012). Longitudinal studies commencing in preschool suggest that there is a significant degree of developmental continuity associated with early hyperactivity (Kan et al., 2013). However, the correlations are moderate suggesting that many individuals displaying raised symptom levels during preschool do not go on to have ADHD or related problems later on in life (Campbell, Pierce, March, Ewing, & Szumowski, 1994). Given their likely costs, this suggests that early interventions will need to be carefully targeted to those at greatest long‐term risk, if they are to be cost‐effective. This means, from an economic perspective, that the development of cost‐effective early intervention programmes will depend on the ability to identify those individuals at particular risk of generating long‐term burden. Currently little is known about: (a) the patterns of long‐term service costs associated with early ADHD markers (i.e. preschool hyperactivity) in the general population or (b) the specific characteristics that differentiate those hyperactive individuals at risk of creating high care burden. We addressed these questions in a prospective study of the longitudinal associations between preschool hyperactivity and average individual per annum service costs up to late adolescent and young adulthood.
Method
Participants
Between 1989 and 1997, 4,215 three‐year‐old children living in the New Forest and Southampton region of Hampshire (England) were assessed using, amongst other measures, the parent‐completed Werry Weiss Peters Activity Rating Scale (WWP: Routh, Schroeder, & O'Tuama, 1974). Of these, 543 children both had basic demographic information and a total score of ≥20 (top 17.2%) and were categorized as being in the hyperactive group (see Table 1). Between 2010 and 2014, when their ages ranged from 14 and 24 years, 499 (204 female) were traced and recontacted (the hyperactive group). Follow‐up data were collected from 170 (34.1%; 89 females). Of the remainder, 87 declined to take part, 240 were nonresponders and two were deceased. A random sample of 88 children from those who did not meet the symptom threshold (i.e. WWP < 20) was recruited as the control group. Hyperactive and control groups did not differ significantly in terms of the age at follow‐up (Table 2). To check the representativeness of the contributing sample we compared participants and nonparticipants on variables collected at age three (Table 1). Groups did not differ as a function of participation except that male control participants had significantly lower hyperactivity scores but lived in more deprived neighbourhoods than nonparticipants. The difference for hyperactivity was nonsignificant (t = −1.41, p = .16) when cases which could not be traced were excluded suggesting that these differences between groups in terms of hyperactivity were due to finding contact addresses.
Table 1.
Comparisons between participants and nonparticipants within the originally selected sample on preschool measures
| Participants | Nonparticipants | t score | p value | ||||
|---|---|---|---|---|---|---|---|
| n | Mean (SD) | N | Mean (SD) | ||||
| Hyperactive males | WWP Hyperactivity | 81 | 27.51 (6.74) | 236 | 28.23 (7.65) | −.76 | .45 |
| BCL Conduct problems | 77 | 2.95 (1.45) | 218 | 3.33 (1.70) | −1.88 | .06 | |
| BCL Emotional problems | 77 | 1.34 (1.13) | 219 | 1.51 (1.28) | −1.04 | .30 | |
| Carstairs deprivation | 80 | −1.06 (1.78) | 201 | −1.05 (1.96) | −.04 | .97 | |
| Hyperactive females | WWP Hyperactivity | 89 | 27.80 (7.95) | 137 | 28.21 (7.68) | −.39 | .70 |
| BCL Conduct problems | 82 | 2.71 (1.64) | 126 | 2.79 (1.64) | −.30 | .77 | |
| BCL Emotional problems | 82 | 1.32 (1.22) | 125 | 1.54 (1.44) | −1.13 | .26 | |
| Carstairs deprivation | 87 | −.92 (1.97) | 113 | −.95 (1.78) | −.12 | .91 | |
| Control males | WWP Hyperactivity | 40 | 7.90 (5.01) | 118 | 10.66 (5.07) | −2.99 | <.01 |
| BCL Conduct problems | 40 | 1.43 (.93) | 118 | 1.81 (1.25) | −1.74 | .08 | |
| BCL Emotional problems | 40 | .88 (1.07) | 118 | 1.04 (1.12) | −.83 | .41 | |
| Carstairs deprivation | 39 | −.85 (2.03) | 116 | .15 (2.51) | −2.25 | .03 | |
| Control females | WWP Hyperactivity | 48 | 8.43 (4.71) | 92 | 9.51 (5.09) | −1.23 | .22 |
| BCL Conduct problems | 47 | 1.21 (1.10) | 93 | 1.56 (1.09) | −1.77 | .08 | |
| BCL Emotional problems | 47 | .80 (.94) | 93 | .94 (.89) | −.85 | .40 | |
| Carstairs deprivation | 48 | −1.26 (2.38) | 89 | −.41 (2.53) | .63 | .53 | |
Table 2.
Demographic and clinical characteristics: Comparisons between the hyperactive and control groups
| Scale | Hyperactive | Control | t score | p value | ||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |||
| Baseline | ||||||
| WWP Hyperactivity | 170 | 27.66 (7.38) | 88 | 8.19 (4.83) | 25.46 | <.01 |
| BCL: Conduct problems | 159 | 2.83 (1.56) | 87 | 1.31 (1.03) | 9.16 | <.01 |
| BCL: Emotional Problems | 159 | 1.33 (1.18) | 87 | .83 (.99) | 3.49 | <.01 |
| Carstairs index of deprivation | 167 | −.99 (1.88) | 87 | −.45 (2.25) | −1.91 | .06 |
| Follow‐up | ||||||
| Conners Clinical Index | 166 | 53.63 (28.56) | 86 | 32.88 (22.56) | 6.31 | <.01 |
| Age at follow‐up | 170 | 18.22 (3.76) | 88 | 17.67 (.58) | 1.88 | .06 |
| Gender | ||||||
| Male | 170 | 47.6% | 88 | 45.5% | X² = .11 | .74 |
Procedure
The study received ethical approval from the University of Southampton and the National Health Service Research ethics committees. Participants and parents provided written consent. The majority of data were collected via face‐to‐face interviews in the individual's homes, with some control families (n = 38) completing the questionnaires online. Interviews lasted approximately 1 hour. A reimbursement of £20 was made to each participant for costs incurred during participation.
Measures
History of service use
A detailed history of service use was obtained from parents who were interviewed at follow‐up using the Client Service Receipt Inventory (CSRI). The CSRI is a well‐established measure that collects information about the use of a range of resources (CSRI‐R: Beecham & Knapp, 2001). It has good face validity and test–retest reliability (Beecham, 1992; Byford et al., 2007; Mirandola, Bisoffi, Bonizzato, & Amaddeo, 1999; Patel et al., 2005; Thorn et al., 2013). In the current study, we focused on the recall of significant episodes and events incurring service costs over the period from age three to follow‐up. While asking parents to remember events over such a long period is likely to work well for major events such as hospitalizations (Chisholm et al., 2000) the occurrence of small or insignificant service use events may be relatively under‐reported. A method using routine recall at regular intervals would be more effective for such events (Barrett & Byford, 2007; Jobe et al., 1990). However, given the comparative nature of the current analysis, any bias towards under‐reporting events introduced in the current analysis could be assumed to have similar effects on cost estimates for the hyperactive and controls groups. Resources measured included; NHS community and hospital based resources, (categorized as general or mental health care), primary/community‐based health care including GP/nurse visits, community paediatrics and psychological services, as well as therapies provided in community or primary care settings such as those for sleep difficulties, hyperactivity support and parenting group programmes. Accident and emergency, outpatient or inpatient visits and/or therapies such day hospital visits, sleep clinics and specialist consultant visits was considered as secondary care resource use. The personal social services domain included social worker, respite/foster care and supportive housing. Frontline and special education services domain included any special educational needs‐related services utilized for learning difficulties or behavioural and emotional problems. Extra costs for special or boarding school and costs from educational suspension/exclusion were included. Moreover, costs resulting from criminal activities and use of the criminal justice services were estimated in addition to costs related to time spent in prison, court appearances and fines paid. Family borne costs included out of pocket expenses and damages to family property due to the child's behaviour.
Baseline measures (3 years)
Preschool hyperactivity
This was assessed using the Werry Weiss Peters Activity Rating Scale (WWP: Routh et al., 1974) – a 27‐item parent report scale measuring hyperactivity in young children, as rated by their parent. The scale has good levels of reliability and validity correlates with other measures of hyperactivity and predicts levels of hyperactivity 5 years after initial testing (Sonuga‐Barke, Stevenson, Thompson, & Viney, 1997).
Other preschool behavioural problems
The Behaviour Problems Checklist (BCL: Richman, Stevenson, & Graham, 1982) is a 19‐item parent report questionnaire with good psychometric properties. Subscales for conduct (i.e. poor social adjustment) and emotional problems (i.e. poor emotional adjustment) are reported here.
Socio‐economic deprivation
The Carstairs Index of Deprivation (Carstairs & Morris, 1991) is based on data from the UK census (1991 in this case) about the characteristics of families living in different postcode regions. Four factors are taken into account: unemployment, overcrowding, social class and car access. Scores for each component were standardized to UK norms and combined in a single continuous score. High scores reflect greater deprivation. Carstairs scores can also be classified into quintiles enabling comparisons to be made to the general UK population. Within our sample, 7.5% of participants scored within the fifth quintile (most deprived 20% of the UK population) and 14.2% scored within the first quintile (least deprived 20% of the UK population). The remaining 78.3% scored within in the middle 60% (quintiles 2, 3 or 4).
Outcomes measure (14–25 years)
General mental health problems
The Conners Comprehensive Behaviour Rating Scale – parent version (CBRS: Conners, 2008) was adapted where necessary for use with older adolescents and young adults. In particular, we used the Conners Clinical Index (CCI) which represents the probability that the participant's score falls within a clinical range for disruptive behaviour disorders, mood disorders, learning disorders, language disorders, anxiety disorders and ADHD (Conners, 2008).
Estimating service use costs
Resource use was categorized by cost domain. Direct medical care and personal social service (PSS) resource use was translated into monetary terms using unit costs derived from the PSSRU (Curtis, 2013) and UK NHS reference costs. Unit costs for frontline and special education services for children were obtained from the Department for Education (DfE), criminal justice services were taken from the literature (Dartington, 2013), costing of medication followed recommendations (dose/duration) from the British National Formulary (BNF, 2013), and cost for damaged property and items were obtained from local providers. For the purpose of the analysis, estimates of average individual costs per annum in each cost domain and in total were estimated. This was done by estimating cumulative costs across the whole period divided by the number of years between baseline (at age 3 years) and follow‐up for each individual.
Statistical analysis
First, using the full follow‐up sample, we compared costs for the hyperactive and control groups. Cost data analysis is complicated by the highly positively skewed nature of the data – most individuals incurred zero costs. Therefore, due to this violation of normality assumption in the data, confirmed using the Shapiro‐Wilds test, we used nonparametric bootstrapping and GLM (Generalized Linear models; Barber & Thompson, 2004). Considering the full sample in the first set of models, the predictor variable was the group allocation (hyperactive versus control) and outcome variables were average individual costs per annum in each separate domain. Model fit were evaluated using deviance plots of residuals against the Akaike information criterion (AIC). In all univariate analyses, gamma distribution was selected to describe the distribution of each cost outcome along with identity link functions which leaves interpretation of the coefficients unchanged from the conventional OLS model (additive effects). In the second set of models we added additional baseline predictors into the model to test whether any effects of group were driven by these. In this model we added age as a factor to examine whether greater costs were incurred at older ages. For each outcome we used a two‐step model, first by applying logistic regression to estimate the probability of incurring cost within the sample as a whole and second by exploring predictors of cost for those with nonzero costs – a conventional way of assessing costs in highly skewed cost data. Third, introducing the WWP score as a continuous variable, we explored the association of costs with the hyperactivity score and calculated the additional cost incurred for each one‐unit increase in hyperactivity. In this analysis we also tested a quadratic term to explore the potential nonlinearity of the cost‐hyperactivity relationship, after adjusting for other base line factors (as in the above models). Fourth, we replicated the two‐step multivariate analyses in the hyperactive sample only to identify which factors over and above group membership were important predictors of costs. Fifth, we then compared the characteristics of members of the hyperactive group incurring zero and nonzero costs. Finally, we used a nonparametric, resampling approach to test whether associations between preschool hyperactivity and costs were mediated by ongoing morbidity (i.e. CCI) as recommended by Preacher and Hayes (2008).
Results
Demographic and baseline clinical characteristics of participants are presented in Table 2. The groups differed on preschool conduct problems and emotional problems as well as CCI, but not SES. One individual with a long standing eating disorder and who accounted for 74% (£104,742.80) of the total mental health cost in the control group was excluded from the analysis as an outlier.
Do hyperactive preschoolers incur greater average annual service use costs than their peers? How are these distributed across different cost domains?
There were statistically significant differences between the hyperactive and control groups on costs across the various domains – with the exception of general health (Table 3). The main cost drivers were use of mental health services and education and criminal related services. The difference between the arithmetic means for the two groups was £531.3 (£333 to £730; p < .001) for the average annual individual cost – 17.6 times greater in the hyperactive compared to the control group (Table 3).
Table 3.
Cost comparison between hyperactive and control group by domain
| Hyperactive (n = 166) | Control (n = 83) | CI (95%) | p | |||
|---|---|---|---|---|---|---|
| Mean | (SD) | Mean | (SD) | |||
| Health Care | ||||||
| Mental Health | 179.99 | (467.7) | 15.93 | (65.9) | (91.6 to 236.5) | <.001 |
| General Health | 25.79 | (177.9) | 5.99 | (39.2) | (−8.5 to 48.1) | .170 |
| Public Sector | ||||||
| Education | 267.49 | (1080.8) | 6.15 | (22.6) | (97.0 to 425.7) | .002 |
| Criminal Justice | 71.46 | (330.9) | 1.40 | (10.7) | (19.7 to 120.4) | .006 |
| Family costs | 16.73 | (50.8) | 0.68 | (5.2) | (8.3 to 23.9) | <.001 |
| Total | 561.47 | (1302.7) | 30.14 | (78.5) | (332.6 to 730.0) | <.001 |
Is it hyperactivity per se that drives increased costs?
Initial GLMs with gamma distributions adjusting for covariates did not converge. Refitted models using Gaussian distributions indicated acceptable fit to the data. Both the full model, and the model conditional on nonzero costs gave similar results (Table 4). Group remained a significant predictor in both models. In addition, male gender and age had statistically significant effects on average individual costs per annum (Table 4). In the full model, male gender was associated with an additional £446.28 (£171.5 to £721.1; p = .001) per annum independent of the effect of hyperactivity (i.e. £557.85; £256.1 to £859.6; p < .001). Age was also significant, indicating that getting older reduces average individual annual cost by £34.47 per year (£‐68.5 to £‐0.5; p = .047). In the nonzero model, the effect of hyperactivity and male gender were £910.34 (£394.0 to £1426.7; p = .001) and £583.87 (£189.8 to£ 977.9; p = .004), respectively; age was not a statistically significant predictor of costs.
Table 4.
GLM multivariable analyses on average individual average costs per annum costs (full sample N = 234)
| Predictor | β coefficient | Robust SE | p‐value | CI (95%) |
|---|---|---|---|---|
| Hyperactive/Control | 557.85 | 153.98 | <.001 | (256.1 to 859.6) |
| Gender (male) | 446.28 | 140.20 | .001 | (171.5 to 721.1) |
| Age | −34.47 | 17.34 | .047 | (−68.5 to −0.5) |
| Conduct problems | 2.90 | 57.29 | .960 | (−109.4 to 115.2) |
| Emotional problems | 66.36 | 81.58 | .416 | (−93.5 to 226.3) |
| Carstairs Deprivation | 16.52 | 25.29 | .514 | (−33.1 to 66.1) |
| Constant | 373.65 | 307.99 | .225 | (−230.0 to 977.3) |
| Conditional of cost>0 (N = 123) | ||||
| Hyperactive/Control | 910.34 | 263.43 | .001 | (394.0 to 1426.7) |
| Gender (male) | 583.87 | 201.04 | .004 | (189.8 to 977.9) |
| Age | −42.05 | 22.85 | .066 | (−86.8 to 2.7) |
| Conduct problems | −106.41 | 106.09 | .316 | (−314.3 to 101.5) |
| Emotional problems | 173.42 | 135.22 | .200 | (−91.6 to 438.5) |
| Carstairs’ Deprivation | 58.33 | 56.24 | .300 | (−51.9 to 168.6) |
| Constant | 616.56 | 440.72 | .162 | (−247.2 to 1480.4) |
Top panel outcome variable is the average individual costs per annum and input variables baseline predictors with hyperactivity as a categorical variable. Bottom panel outcome variable is the same model conditional on having costs greater than zero during the follow‐up period (i.e. nonzero cases).
What is the additional marginal cost per unit increase in preschool hyperactivity?
Each one‐unit increase in the hyperactivity score added a cost of £49.8 (16.0–83.6; p = .004) to average individual cost per annum after adjusting for other factors as in the model above (Table 5). There was an underlying significant linear trend (p = .004). The quadratic term was also statistically significant (p = 0.20). This is also evident in Figure 1, which graphs average individual cost per annum against WWP score, as an augmented component‐plus‐residuals plot following the model. The graph shows clear deviation from linearity with a number of individuals with WWP scores between 20 and 30 incurring substantial costs.
Table 5.
Polynomial regression analyses on average individual costs per annum against the hyperactivity score (full sample N = 234)
| Predictor | β coefficient | Robust SE | p | CI (95%) |
|---|---|---|---|---|
| WWP score linear | 49.80 | 17.25 | .004 | (16.0 to 83.6) |
| WWP scorepolynomial | −0.86 | 0.37 | .020 | (−1.6 to −0.1) |
| Gender (male) | 426.88 | 138.08 | .002 | (156.2 to 697.5) |
| Age | −35.28 | 17.61 | .045 | (−69.8 to −0.8) |
| Conduct problems | 33.37 | 57.95 | .565 | (−80.2 to 147.0) |
| Emotional problems | 77.10 | 82.94 | .353 | (−85.5 to 239.7) |
| Deprivation | 4.63 | 24.04 | .847 | (−42.5 to 51.8) |
| Constant | 117.92 | 283.80 | .678 | (−438.3 to 674.1) |
Fitting a polynomial regression model to data points. The outcome variable is average individual costs per annum and input variables include baseline predictors with hyperactivity as a continuous variable. This model is similar to the model at the top of Table 4 but differs in terms of including WWP score as both a linear and a polynomial term to depict nonlinearity of the association between cost and WWP score.
Figure 1.
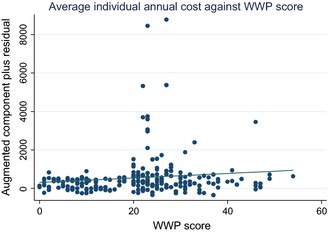
Average individual annual cost as a function of WWP score with a linear term fitted illustrating the peak between WWP scores between 20 and 30
Which hyperactive preschoolers are most likely to incur additional service use costs?
When the analysis was restricted to the hyperactive sample, male gender was the only other statistically significant predictor of costs, with similar results in both models. In these, male gender was associated with increased costs of £669.52 (260.8–1078.3; p = .001) and £682.86 (207.0–1158.7; p = .005) for the full hyperactive and nonzero hyperactive samples, respectively (Table 6). Considering the average individual cost per annum for each domain separately, mental health care costs were mainly driven by conduct problems (£90.4; 31.0 to £149.8; p = .003), while education (£485.1; £125.1 to £845.1; p = .008) and criminal justice (£135.8; 15.2–256.4; p = .027) costs were driven by male gender. Logistic regression comparing participants with nonzero and zero costs revealed that male gender and conduct and emotional problems were statistically significant predictors of nonzero costs (Table 7).
Table 6.
GLM multivariable analyses on average individual costs per annum (hyperactive group, N = 153)
| Predictor | β coefficient | Robust SE | p | CI (95%) |
|---|---|---|---|---|
| WWP Hyperactivity | −16.12 | 10.98 | .142 | (−37.6 to 5.4) |
| Gender (male) | 669.52 | 208.54 | .001 | (260.8 to 1078.3) |
| Age | −30.08 | 18.25 | .099 | (−65.9 to 5.7) |
| Conduct problems | 14.33 | 74.90 | .848 | (−132.5 to 161.1) |
| Emotional problems | 122.75 | 116.64 | .293 | (−105.9 to 351.4) |
| Deprivation (Carstairs) | 26.25 | 43.84 | .549 | (−59.7 to 112.2) |
| Constant | 1,094.39 | 555.90 | .049 | (4.8 to 2183.9) |
| Conditional of cost>0 (N = 100) | ||||
| WWP Hyperactivity | −20.08 | 15.53 | .196 | (−50.5 to 10.4) |
| Gender (male) | 682.86 | 242.80 | .005 | (207.0 to 1158.7) |
| Age | −44.77 | 25.61 | .080 | (−95.0 to 5.4) |
| Conduct problems | −98.95 | 122.09 | .418 | (−338.2 to 140.3) |
| Emotional problems | 214.84 | 158.70 | .176 | (−96.2 to 525.9) |
| Deprivation (Carstairs) | 62.83 | 76.47 | .411 | (−87.0 to 212.7) |
| Constant | 2011.575 | 884.3691 | .023 | (278.2 to 3744.9) |
As in Table 4 but within the hyperactive group.
Table 7.
Logistic regression on zero versus nonzero cost individuals in the hyperactive group (N = 153)
| NonZero | β coefficient | Robust SE | p | CI(95%) |
|---|---|---|---|---|
| WWP Hyperactivity | 0.00 | 0.02 | .835 | (−0.05 to 0.04) |
| Age | 0.01 | 0.06 | .861 | (−0.10 to 0.12) |
| Gender | 0.78 | 0.39 | .042 | (0.03 to 1.54) |
| BCL conduct problems | 0.46 | 0.16 | .003 | (0.15 to 0.77) |
| BCL emotional problems | −0.35 | 0.16 | .028 | (−0.66 to −0.04) |
| Deprivation | −0.01 | 0.11 | .940 | (−0.22 to 0.20) |
| Constant | −0.57 | 1.46 | .699 | (−3.43 to 2.30) |
Binary outcome is zero versus nonzero costs during the follow‐up period and input variables include baseline predictors with hyperactivity as a continuous variable.
Are costs associated with preschool hyperactivity mediated by continuing psychiatric morbidity?
Using the full sample, when CCI was included as a mediator, the direct effects of preschool hyperactivity on costs were not significant [ß = .06, 95% CI (−.07, .19)]. The indirect path, however, was significant [ß = .09, 95% CI (.04, .18)] indicating that the relationship between preschool hyperactivity and average individual cost per annum is fully mediated by later mental health problems (Figure 2).
Figure 2.
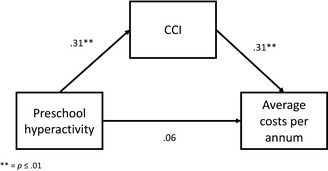
Model of preschool hyperactivity score (WWP) as a predictor of average individual annual service costs mediated by morbidity at follow‐up. CCI = Conners’ Clinical Index ** = p ≤ .01
Discussion
Although preschool hyperactivity is associated with long‐term psychiatric morbidity, not all hyperactive preschoolers go on to have problems later in life. The development of cost‐effective early interventions will therefore, depend on the ability to target treatment at young children whose behavioural difficulties will, over time, become associated with health economic burden. This article reports the first longitudinal health economic analysis of (a) average individual annual long‐term service use and related costs associated with preschool hyperactivity and (b) the factors that place affected individuals at particular risk for long‐term burden. There were a number of findings of note.
First, preschool hyperactivity was associated with considerable long‐term costs with a greater than 17‐fold difference between those scoring in the top 18% of the WWP distribution and controls. The fact that mental health, education, social service and criminal justice costs, but not general health costs, were all significantly higher in this group, provides evidence for the specificity of these effects. Further support for this specificity comes from the finding that adjusting for male gender, which was itself a powerful predictor of costs, social deprivation and other preschool behaviour problems did not significantly reduce the predictive power of hyperactivity. This finding is consistent with prior literature showing that hyperactive preschoolers are at increased risk of behavioural and mental health problems (McGee, Partridge, Williams, & Silva, 1991) and associated negative outcomes both in the medium and long‐term (Washbrook, Propper, & Sayal, 2013). However, the magnitude and persistence of the long‐term effects of preschool hyperactivity on service and other costs was unexpected given the long follow‐up period and the relatively lenient thresholds applied in defining preschool hyperactivity. In this sense it is worth noting that, given the broad definition of hyperactivity applied in this study (i.e. WWP scores ≥20 or top 18% of the population) most individuals included in the hyperactive group would not have met the criteria for preschool ADHD. Furthermore, according to Figure 1 the highest level of risk of economic burden was not necessarily associated with the highest WWP scores – the highest individual costs were incurred by participants with scores between 20 and 30 on the WWP. Our results provide health economic evidence for the potential utility of population‐based screening approaches with high risk defined using a relatively liberal cut‐off in terms of the severity of hyperactivity.
Second, when analyses were restricted to the hyperactive group, male gender was the most consistent predictor across analyses and outcomes. Conduct problems were also predictive of costs for some outcomes. In these cases, preschool hyperactivity and conduct problems were associated with particular risk for long‐term burden in boys. From a scientific perspective, these data are consistent with previous evidence that conduct problems exacerbate the risk associated with early hyperactivity (Fergusson, Horwood, & Ridder, 2005). From a practical perspective, our findings suggest that early screening approaches should include measures of conduct problems. It was also noticeable that from a peak cost at WWP scores of between 20 and 30 severity of hyperactivity appeared to reduce costs. However, the possibility that this is due to the small number of observations made beyond this point cannot be ruled out as an explanation for this.
Third, the effects of early hyperactivity seemed to be mediated by subsequent clinical problems as indexed by the CCI. As one might expect there was very little evidence for a direct pathway from preschool hyperactivity to costs. Although this suggests that long‐term costs linked to preschool hyperactivity are driven by ongoing clinical problems, it is clear (from the relatively small absolute β path weights) that not all clinically significant problems led to service use and costs suggesting an under treatment of problems in this high risk group. An analysis of the specific outcomes (i.e. ADHD, conduct problems, mood disorders) driving costs is warranted but is outside the scope of the current article.
Finally, social deprivation was surprisingly unimportant as a predictor of costs. Those preschoolers growing up in more socially deprived neighbourhoods did not appear to incur greater costs. This seems to go against recent evidence confirming the importance of social deprivation as a predictor of ADHD and related problems (Larsson, Sariaslan, Långström, D'Onofrio, & Lichtenstein, 2014). One possibility is that the use of a measure of social deprivation based on post‐code differences was insensitive to family specific circumstances that might drive service use. It is also possible that although social deprivation was associated with long‐term morbidity this was not translated into costs due to limited access to services by socially deprived families, although in the United Kingdom, key health and education services are freely available at the point of access.
Despite these findings providing initial support for the potential long‐term value of hyperactivity screening in preschool, the more general cost‐effectiveness of early identification will depend on (a) the costs and benefits of available interventions and (b) the uptake of these interventions by families of children at highest risk. With regard to the former, preschool behavioural parenting approaches have been shown to reduce parent‐rated hyperactivity scores by significant amounts (Daley et al., 2014). While a formal cost‐benefit analysis based on the long‐term costs of preschool‐hyperactivity has not been completed, the scale of the costs identified in this study suggest that the use of parent training for those screened positive for both hyperactivity and conduct problems could be cost effective.
While the current study is the first to provide estimates of the long‐term costs of preschool hyperactivity using a longitudinal design in a large high‐risk sample, the findings need to be interpreted in the light of a number of limitations. First, attrition was high. This is due partly to the very long‐term follow‐up with no contact in the intervening years. However, the attrition analyses make us fairly confident that selection bias did not influence the comparison findings. Nevertheless, as control male participants were less hyperactive than nonparticipants this may have led to an under‐estimation of costs in this group and therefore an overestimation of difference between controls and hyperactive individuals in terms of costs. Second, we relied on parental retrospective accounts of resource use over a relatively long period‐of‐time. However, this is a widely used approach using a well‐validated instrument (Thorn et al., 2013) and it seems unlikely that differences of the magnitude reported in the current paper are the results of reporting biases. Third, a limited range of baseline variables were available. For instance, there was no information about mothers’ mental health, a factor which is linked to both child hyperactivity (Chronis et al., 2007) and service use (Sayal, Mills, White, Merrell, & Tymms, 2015).
In summary, preschool hyperactivity was associated with a significant and substantial elevation in mental health, educational, social service and criminal justice system costs independent of other preschool characteristics. Male hyperactive preschoolers with co‐occurring conduct problems were at particular risk. Future research should explore the potential utility of early screening for hyperactivity in the light of the long‐term costs identified in this study and benefits of early intervention strategies such as parent training.
Key points.
Preschool hyperactivity is known to represent a risk for long‐term mental health problems.
A prospective study to estimate the costs to mental health, social, educational and criminal justice services across childhood, adolescence and early adulthood associated with preschool hyperactivity was undertaken.
Preschoolers with high levels of hyperactivity had a 17‐fold increase in overall costs compared to nonhyperactive peers after taking into account other available preschool characteristics and factors.
Of those with hyperactivity, costs were especially great for male preschoolers and those with conduct problem.
Preventative approaches, targeting early hyperactivity may be of value, but need to be considered in the light of the costs and benefits of specific early intervention strategies.
Acknowledgements
This original article was invited by the journal as part of a special issue; it has undergone full, external peer review.
This was an independent study funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research scheme (RP‐PG‐0108‐10061). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, NIHR or the UK Department of Health. We would like to acknowledge the contribution of Donna McCann who was Principle Research Fellow and was involved in the design and implementation of the study.
The authors would like to acknowledge the contribution of all the families that took part in the study. We thank Jeremy Jones for his valuable comments on an earlier version of the article.
Competing interests (preceding 3 years): E.S‐B.: Speaker fees, consultancy, research funding and conference support from Shire Pharma. Speaker fees from Janssen Cilag, Medice. Book royalties from OUP and Jessica Kingsley. Consultancy from Neurotech solutions. Thompson: Conference support and research funding from Shire Pharma; Book royalties from Jessica Kingsley; training fees from the New Forest Development Fund. The remaining authors declare that they have no competing or potential conflicts of interest.
Conflict of interest statement: See Acknowledgements for disclosures.
References
- Banaschewski, T. , Coghill, D. , Santosh, P. , Zuddas, A. , Asherson, P. , Buitelaar, J. , … & Taylor, E. (2006). Long‐acting medications for the hyperkinetic disorders – A systematic review and European treatment guideline. European Child and Adolescent Psychiatry, 15, 476–495. [DOI] [PubMed] [Google Scholar]
- Barber, J. , & Thompson, S. (2004). Multiple regression of cost data: Use of generalised linear models. Journal Health Service Research Policy, 9, 197–204. [DOI] [PubMed] [Google Scholar]
- Barrett, B. , & Byford, S. (2007). Collecting service use data for economic evaluation in DSPD populations: Development of the Secure Facilities Service Use Schedule. British Journal of Psychiatry Supplement, 49, s75–s78. [DOI] [PubMed] [Google Scholar]
- Beecham, J. (1992). Measuring mental health needs. London: Gaskell. [Google Scholar]
- Beecham, J. (2014). Annual Research Review: Child and adolescent mental health interventions: A review of progress in economic studies across different disorders. Journal of Child Psychology and Psychiatry, 55, 714–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beecham, J. , & Knapp, M. (2001). Costing psychiatric interventions In Thornicroft G. (Ed.), Measuring mental health needs (2nd edn). London: Gaskell. [Google Scholar]
- British National Formulary (2013). BNF for Children. UK: Paediatric Formulary Committee; Available from: www.pharmpress.com/product/9780857111364/bnfc. [Google Scholar]
- Byford, S. , Leese, M. , Knapp, M. , Seivewright, H. , Cameron, S. , Jones, V. , … & Tyrer, P. (2007). Comparison of alternative methods of collection of service use data for the economic evaluation of health care interventions. Health Economics, 16, 531–536. [DOI] [PubMed] [Google Scholar]
- Campbell, S.B. , Pierce, E.W. , March, C.L. , Ewing, L.J. , & Szumowski, E.K. (1994). Hard‐to‐manage preschool boys: Symptomatic behavior across contexts and time. Child Development, 65, 836–851. [PubMed] [Google Scholar]
- Carstairs, V. , & Morris, R. (1991). Deprivation and health in Scotland. Aberdeen: Aberdeen University Press. [Google Scholar]
- Chisholm, D. , Knapp, M.R. , Knudsen, H.C. , Amaddeo, F. , Gaite, L. , & van Wijngaarden, B. (2000). Client Socio‐Demographic and Service Receipt Inventory‐European Version: Development of an instrument for international research. EPSILON Study 5. European Psychiatric Services: Inputs Linked to Outcome Domains and Needs. British Journal of Psychiatry Supplement, 39, s28–s33. [DOI] [PubMed] [Google Scholar]
- Chronis, A.M. , Lahey, B.B. , Pelham, W.E., Jr , Williams, S.H. , Baumann, B.L. , Kipp, H. , … & Rathouz, P.J. (2007). Maternal depression and early positive parenting predict future conduct problems in young children with attention‐deficit/hyperactivity disorder. Developmental Psychology, 43, 70. [DOI] [PubMed] [Google Scholar]
- Conners, K. (2008). Conners comprehensive behavior rating scales™. New York: Pearson. [Google Scholar]
- Cortese, S. , Ferrin, M. , Brandeis, D. , Buitelaar, J. , Daley, D. , Dittmann, R.W. , … & Sonuga‐Barke, E.J.S. (2015). Cognitive training for attention‐deficit/hyperactivity disorder: Meta‐analysis of clinical and neuropsychological outcomes from randomized controlled trials. Journal of American Academy of Child and Adolescent Psychiatry, 54, 164–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis, L. (2013). Unit costs of health and social care 2013 PSSRU. Canterbury/Kent: PSSRU/University of Kent. [Google Scholar]
- Cussen, A. , Sciberras, E. , Ukoumunne, O.C. , & Efron, D. (2012). Relationship between symptoms of attention‐deficit/hyperactivity disorder and family functioning: A community‐based study. European Journal of Pediatrics, 171, 271–280. [DOI] [PubMed] [Google Scholar]
- Daley, D. , Oord, S.V. , Ferrin, M. , Danckaerts, M. , Doepfner, M. , Cortese, S. , … & Sonuga‐Barke, E.J.S. (2014). Behavioral interventions in attention‐deficit/hyperactivity disorder: A Meta‐analysis of randomized controlled trials across multiple outcome domains. Journal of the American Academy of Child & Adolescent Psychiatry, 53, 835–847. [DOI] [PubMed] [Google Scholar]
- Dalsgaard, S. , Mortensen, P.B. , Frydenberg, M. , & Thomsen, P.H. (2013). Long‐term criminal outcome of children with attention deficit hyperactivity disorder. Criminal Behaviour and Mental Health, 23, 86–98. [DOI] [PubMed] [Google Scholar]
- D'Amico, F. , Knapp, M. , Beecham, J. , Sandberg, S. , Taylor, E. , & Sayal, K. (2014). Use of services and associated costs for young adults with childhood hyperactivity/conduct problems: 20‐year follow‐up. British Journal of Psychiatry, 204, 441–447. [DOI] [PubMed] [Google Scholar]
- Danckaerts, M. , Sonuga‐Barke, E. , Banaschewski, T. , Buitelaar, J. , Dopfner, M. , Hollis, C. , … & Coghill, D. (2010). The quality of life of children with attention deficit/hyperactivity disorder: A systematic review. European Child & Adolescent Psychiatry, 19, 83–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dartington, T.S.R.U.A. (2013). Investing in children: Technical report. In T. E. A. G. Bjornstad (Ed.). Dartington: Dartington Press. [Google Scholar]
- Doshi, J.A. , Hodgkins, P. , Kahle, J. , Sikirica, V. , Cangelosi, M.J. , Setyawan, J. , … & Neumann, P.J. (2012). Economic impact of childhood and adult attention‐deficit/hyperactivity disorder in the United States. Journal of the American Academy of Child Adolescent Psychiatry, 51, 990–1002. [DOI] [PubMed] [Google Scholar]
- Dunne, E.M. , Hearn, L.E. , Rose, J.J. , & Latimer, W.W. (2014). ADHD as a risk factor for early onset and heightened adult problem severity of illicit substance use: An accelerated gateway model. Addictive Behaviors, 39, 1755–1758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erskine, H.E. , Ferrari, A.J. , Polanczyk, G.V. , Moffitt, T.E. , Murray, C.J.L. , Vos, T. , … & Scott, J.G. (2014). The global burden of conduct disorder and attention‐deficit/hyperactivity disorder in 2010. Journal of Child Psychology and Psychiatry, 55, 328–336. [DOI] [PubMed] [Google Scholar]
- Fergusson, D.M. , Horwood, L.J. , & Ridder, E.M. (2005). Show me the child at seven: The consequences of conduct problems in childhood for psychosocial functioning in adulthood. Journal of Child Psychology & Psychiatry, 46, 837–849. [DOI] [PubMed] [Google Scholar]
- Fletcher, J.M. (2014). The effects of childhood ADHD on adult labor market outcomes. Health Economics, 23, 159–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galera, C. , Bouvard, M.P. , Lagarde, E. , Michel, G. , Touchette, E. , Fombonne, E. , & Melchior, M. (2012). Childhood attention problems and socioeconomic status in adulthood: 18‐year follow‐up. British Journal of Psychiatry, 201, 20–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halperin, J.M. , Bedard, A.C.V. , & Curchack‐Lichtin, J.T. (2012). Preventive interventions for ADHD: A neurodevelopmental perspective. Neurotherapeutics: The Journal of the American Society for Experimental NeuroTherapeutics, 9, 531–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw, S.P. , Scheffler, R.M. , Fulton, B.D. , Aase, H. , Banaschewski, T. , Cheng, W. , … & Weiss, M. (2011). International variation in treatment procedures for ADHD: Social context and recent trends. Psychiatric Services, 62, 459–464. [DOI] [PubMed] [Google Scholar]
- Holmberg, K. , & Bolte, S. (2014). Do symptoms of ADHD at Ages 7 and 10 predict academic outcome at Age 16 in the general population? Journal of Attention Disorders, 18, 635–645. [DOI] [PubMed] [Google Scholar]
- Jobe, J.B. , White, A.A. , Kelley, C.L. , Mingay, D.J. , Sanchez, M.J. , & Loftus, E.F. (1990). Recall strategies and memory for health‐care visits. Milbank Quarterly, 68, 171–189. [PubMed] [Google Scholar]
- Kan, K.J. , Dolan, C.V. , Nivard, M.G. , Middeldorp, C.M. , van Beijsterveldt, C.E.M. , Willemsen, G. , & Boomsma, D.I. (2013). Genetic and environmental stability in attention problems across the lifespan: Evidence from the Netherlands twin register. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 12–25. [DOI] [PubMed] [Google Scholar]
- Kessler, R.C. , Lane, M. , Stang, P.E. , & van Brunt, D.L. (2000). The prevalence and workplace costs of adult attention deficit hyperactivity disorder in a large manufacturing firm. Psychological Medicine, 39, 137–147. [DOI] [PubMed] [Google Scholar]
- Kotsopoulos, N. , Connolly, M.P. , Sobanski, E. , & Postma, M.J. (2013). The fiscal consequences of ADHD in Germany: A quantitative analysis based on differences in educational attainment and lifetime earnings. Journal of Mental Health and Policy Economic, 16, 27–33. [PubMed] [Google Scholar]
- Larsson, H. , Sariaslan, A. , Långström, N. , D'Onofrio, B. , & Lichtenstein, P. (2014). Family income in early childhood and subsequent attention deficit/hyperactivity disorder: A quasi‐experimental study. Journal of Child Psychology and Psychiatry, 55, 428–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le, H.H. , Hodgkins, P. , Postma, M.J. , Kahle, J. , Sikirica, V. , Setyawan, J. , … & Doshi, J.A. (2013). Economic impact of childhood/adolescent ADHD in a European setting: The Netherlands as a reference case. European Child & Adolescent Psychiatry, 23, 587–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks, D.J. , Mlodnicka, A. , Bernstein, M. , Chacko, A. , Rose, S. , & Halperin, J.M. (2009). Profiles of service utilization and the resultant economic impact in preschoolers with attention deficit/hyperactivity disorder. Journal of Pediatric Psychology, 34, 681–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGee, R. , Partridge, F. , Williams, S. , & Silva, P. (1991). Twelve‐year follow‐up of preschool hyperactive children. Journal of the American Academy of Child & Adolescent Psychiatry, 30, 224–232. [DOI] [PubMed] [Google Scholar]
- Mirandola, M. , Bisoffi, G. , Bonizzato, P. , & Amaddeo, F. (1999). Collecting psychiatric resources utilisation data to calculate costs of care: A comparison between a service receipt interview and a case register. Social Psychiatry and Psychiatric Epidemiology, 34, 541–547. [DOI] [PubMed] [Google Scholar]
- Moya, J. , Stringaris, A.K. , Asherson, P. , Sandberg, S. , & Taylor, E. (2014). The impact of persisting hyperactivity on social relationships: A community‐based, controlled 20‐year follow‐up study. Journal of Attention Disorders, 18, 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (2009). Attention deficit hyperactivity disorder: Diagnosis and management of ADHD in children, young people and adults. London: NICE. [PubMed] [Google Scholar]
- Patel, A. , Rendu, A. , Moran, P. , Leese, M. , Mann, A. , & Knapp, M. (2005). A comparison of two methods of collecting economic data in primary care. Family Practice, 22, 323–327. [DOI] [PubMed] [Google Scholar]
- Polanczyk, G. , de Lima, M.S. , Horta, B.L. , Biederman, J. , & Rohde, L.A. (2007). The worldwide prevalence of ADHD: A systematic review and metaregression analysis. American Journal of Psychiatry, 164, 942–948. [DOI] [PubMed] [Google Scholar]
- Polanczyk, G. , Salum, G. , Sugaya, L.S. , Caye, A. , & Rohde, L. (2015). Annual research review: A metaanalysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Child Psychology & Psychiatry, 56, 345–365. [DOI] [PubMed] [Google Scholar]
- Polderman, T.J. , Boomsma, D.I. , Bartels, M. , Verhulst, F.C. , & Huizink, A.C. (2010). A systematic review of prospective studies on attention problems and academic achievement. Acta Psychiatrica Scandanavia, 122, 271–284. [DOI] [PubMed] [Google Scholar]
- Preacher, K.J. , & Hayes, A.F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Richman, N. , Stevenson, J. , & Graham, P. (1982). Preschool to school: A behavioural study. London: Academic Press. [Google Scholar]
- Routh, D.K. , Schroeder, C.S. , & O'Tuama, L. (1974). Development of activity level in children. Developmental Psychology, 10, 163–168. [Google Scholar]
- Sarver, D.E. , McCart, M.R. , Sheidow, A.J. , & Letourneau, E.J. (2014). ADHD and risky sexual behavior in adolescents: Conduct problems and substance use as mediators of risk. Journal of Child Psychology and Psychiatry, 55, 1345–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayal, K. , Mills, J. , White, K. , Merrell, C. , & Tymms, P. (2015). Predictors of and barriers to service use for children at risk of ADHD: Longitudinal study. European Child & Adolescent Psychiatry, 24, 545–552. [DOI] [PubMed] [Google Scholar]
- Schlander, M. , Trott, G.E. , & Schwarz, O. (2010). The health economics of attention deficit hyperactivity disorder in Germany. Part 1: Health care utilization and cost of illness. Nervenarzt, 81, 289–300. [DOI] [PubMed] [Google Scholar]
- Sonuga‐Barke, E. , Brandeis, D. , Cortese, S. , Daley, D. , Ferrin, M. , Holtmann, M. , … & on behalf of European ADHD Guidelines Group (2013). Non‐pharmacological interventions for attention‐deficit/hyperactivity disorder: Systematic review and meta‐analyses of randomised controlled trials of dietary and psychological treatments. American Journal of Psychiatry, 170, 275–289. [DOI] [PubMed] [Google Scholar]
- Sonuga‐Barke, E.J.S. , & Halperin, J.M. (2010). Developmental phenotypes and causal pathways in attention deficit/hyperactivity disorder: Potential targets for early intervention? Journal of Child Psychology and Psychiatry, 51, 368–389. [DOI] [PubMed] [Google Scholar]
- Sonuga‐Barke, E. , Koerting, J. , Smith, E. , McCann, D. , & Thompson, M. (2011). Early detection and intervention for attention‐deficit/hyperactivity disorder. Expert Reviews in Neurotherapeutics, 11, 557–563. [DOI] [PubMed] [Google Scholar]
- Sonuga‐Barke, E.J.S. , Stevenson, J. , Thompson, M. , & Viney, D. (1997). The structure of British pre‐school children's behaviour problems. Psychological Medicine, 7, 909–918. [DOI] [PubMed] [Google Scholar]
- Sonuga‐Barke, E.J.S. , & Taylor, E. (in press). Attention deficit/hyperactivity disorder and hyperkinetic disorder. (Chapter 55) In Thapar A., Pine D.S., Leckman J.F., Scott S., Snowling M.J. & Taylor E.A. (Eds.), Rutter's child & adolescent psychiatry. New York: Wiley Blackwell. [Google Scholar]
- Stevenson, J. , Buitelaar, J. , Cortese, C. , Ferrin, M. , Konofal, E. , & Lecendreux, M. (2014). Research Review: The role of diet in the treatment of attention‐deficit/hyperactivity disorder–an appraisal of the evidence on efficacy and recommendations on the design of future studies. Journal of Child Psychology and Psychiatry, 55, 416–427. [DOI] [PubMed] [Google Scholar]
- Telford, C. , Green, C. , Logan, S. , Langley, K. , Thapar, A. , & Ford, T. (2013). Estimating the costs of ongoing care for adolescents with attention‐deficit hyperactivity disorder. Social Psychiatry and Psychiatric Epidemiology, 48, 337–344. [DOI] [PubMed] [Google Scholar]
- Thorn, J.C. , Coast, J. , Cohen, D. , Hollingworth, W. , Knapp, M. , Noble, S.M. , … & Hughes, D. (2013). Resource‐use measurement based on patient recall: Issues and challenges for economic evaluation. Applied Health Economics and Health Policy, 11, 155–161. [DOI] [PubMed] [Google Scholar]
- van Roijen, L.H. , van Straten, A. , Al, M. , Rutten, F. , & Donker, M. (2006). Cost‐utility of brief psychological treatment for depression and anxiety. British Journal of Psychiatry, 188, 323–329. [DOI] [PubMed] [Google Scholar]
- Washbrook, E. , Propper, C. , & Sayal, K. (2013). Pre‐school hyperactivity and attention problems and educational outcomes in adolescence: Prospective longitudinal study. British Journal of Psychiatry, 203, 265–271. [DOI] [PubMed] [Google Scholar]


