Abstract
Background
Bystander first aid and basic life support can likely improve victim survival in trauma. In contrast to bystander first aid and out‐of‐hospital cardiac arrest, little is known about the role of bystanders in trauma response. Our aim was to determine how frequently first aid is given to trauma victims by bystanders, the quality of this aid, the professional background of first‐aid providers, and whether previous first‐aid training affects aid quality.
Methods
We conducted a prospective 18‐month study in two mixed urban–rural Norwegian counties. The personnel on the first ambulance responding to trauma calls assessed and documented first aid performed by bystanders using a standard form.
Results
A total of 330 trauma calls were included, with bystanders present in 97% of cases. Securing an open airway was correctly performed for 76% of the 43 patients in need of this first‐aid measure. Bleeding control was provided correctly for 81% of 63 patients for whom this measure was indicated, and prevention of hypothermia for 62% of 204 patients. Among the first‐aid providers studied, 35% had some training in first aid. Bystanders with documented first‐aid training gave better first aid than those where first‐aid training status was unknown.
Conclusions
A majority of the trauma patients studied received correct pre‐hospital first aid, but still there is need for considerable improvement, particularly hypothermia prevention. Previous first‐aid training seems to improve the quality of first aid provided. The effect on patient survival needs to be investigated.
Editorial comment: what this article tells us.
In this prospective study of trauma patients, it was found that correct first aid was provided in a majority of cases, most often by health care workers. The quality of first aid was better if it was provided by persons with previous first‐aid training.
A majority of trauma deaths occur at the scene of injury, often before the arrival of emergency medical services (EMS), particularly in rural areas.1, 2 Bystanders to a traumatic injury are in a position to provide life‐saving and time‐critical measures, such as securing a free airway or control of bleeding, long before the arrival of the EMS.
The bystander's role has been thoroughly investigated in out‐of‐hospital cardiac arrest. Various approaches to improving bystander first aid, such as teaching compression‐only resuscitation, has led to increased bystander first‐aid response and, in some cases, to improved survival.3, 4
Bystander first aid in trauma has received little attention, even though it has potential for mortality reduction.
In a recent review, we found only 11 papers covering the topic. Reported results, though scarce, are interesting, suggesting that bystander first aid resulted in a possible improvement in survival of 1.8–5%, but how often and how well first aid was provided varied greatly.5 Two recent studies have reported that injuries were potentially survivable in 6–20% of trauma victims who died either at the scene of injury, during ambulance transportation, or within 4 h of hospital arrival.6, 7 Thus, optimization of first responder actions may improve survival.
The primary aim of this study was to determine the frequency of first aid given by bystanders to victims of trauma in a combined rural and urban Norwegian region. Secondary aims were to assess (1) whether these first‐aid measures were performed correctly, and (2) to determine the professional background of first aiders. We also assessed: (3a) the extent of the first‐aid providers' previous first‐aid training and (3b) impact of this training on the correctness of the first aid provided.
Methods
We conducted a prospective, observational study. The study area covered the Norwegian counties of Finnmark, Troms, and parts of Nordland County, which comprise the two northernmost administrative health trusts of Norway. The region is a mixed urban–rural area covering 80,012 km2 with approximately 265,000 inhabitants. The area has four local hospitals as well as the tertiary trauma centre for Northern Norway.
From 1 October 2012 to 1 April 2014, the personnel of the first EMS unit to arrive at the scene of each immediate‐response trauma call registered and evaluated the first aid rendered prior to their arrival in a standard form.
Inclusion criteria
Trauma calls were defined as calls in which EMS units were assigned to respond to complaints that fell into the ICD‐10 categories V01‐Y98, excluding intoxications.8 Only immediate‐response calls were included.
The form
The form was developed by the authors, two of whom work as EMS physicians. It was subsequently tested in the services during a 3‐month period from May to August 2011. The form was then adjusted, based on discussion with one representative from each ambulance base. Forms were placed in each EMS unit, and written instructions and information on the project was attached to the forms. The following information was collected:
Patient data and environment
On the form, it was recorded whether the patient was alive, dead, or CPR was in progress upon the ambulance's arrival on the scene, and at the time the EMS unit delivered the patient to another unit or care facility. From the EMS patient record, the following data were obtained: cause of injury, patient's age and gender, apparent injuries sustained based on EMS' examination, Glasgow Coma Scale (GCS), pulse rate, respiratory rate, and blood pressure.
In addition, outside temperature and weather conditions were documented by the EMS. Mode of trauma, response time, and assignment driving distance were recorded from the EMS' record.
First‐aid providers
The following data were collected: number of bystanders present, number of bystanders involved in first aid, whether the bystander had any prior first‐aid training (yes/no/unknown), the profession of the bystander and whether or not she/he was currently at work. Health care personnel present on the scene who were not part of EMS were included as first‐aid providers, regardless of whether they were bystanders to accidents at their work place or were random passers‐by.
First aid
The following first‐aid measures were selected for evaluation: securing the scene, provision of free airway, recovery position, CPR, control of bleeding, and hypothermia prevention. Each measure was marked as not required, done, done incorrectly/inadequately, or should have been done.
Analysis and statistics
The sum of the components of the Revised Trauma Score (RTS) was used as a measure for injury severity.9
To quantify overall first‐aid performance in each case, the individual first‐aid measures for every case was scored from −1 to 1. A correctly performed measure was scored as 1, any non‐indicated measure was scored as 0, and indicated measures not performed or measures performed incorrectly were scored as −1. The sum was then divided by the total number of indicated measures to provide a total score. The measure “securing the scene” was omitted from the score. When comparing first‐aid quality between groups, cases of non‐injury, cases with no measures necessary and cases with no bystanders present were excluded.
Statistical analysis was performed using SPSS Statistics for Mac version 21 (IBM Corp., Armonk, NY, USA). The specific analysis used for individual comparisons is specified in the Results section.
Ethics
The Regional Committee for Medical and Health Research Ethics, University of Tromsø, approved of the study 28.01.2011 (Ref. 2010/3328/REK nord).
Results
A total of 562 cases were collected, and 154 cases were excluded (due to the following reasons: evaluation of EMS' own first aid (n = 11), no assessment of first aid (n = 8), patient's record missing (n = 7), not an immediate‐response call (n = 20), intoxication (n = 33), non‐trauma problem (n = 73), no patient (n = 2)). Further, for 78 cases, no injury was found and they were excluded from further analyses.
Patients
The patients had a median age of 36 years (range 0–93 years, 41 missing), and 65% were male (28 missing). Forty‐eight per cent of the patients had complete information for RTS (Table 1). Overall, 22% of injured patients exhibited abnormalities in at least one of the physiological parameters GCS, respiratory rate or systolic blood pressure.
Table 1.
Patient injury severity by revised trauma score
| Revised trauma score | Per cent of patients | |
|---|---|---|
| 0 | 7.6% | n = 12 |
| 8 | 2.5% | n = 4 |
| 9 | 0.6% | n = 1 |
| 10 | 2.5% | n = 4 |
| 11 | 5.7% | n = 9 |
| 12 | 81.0% | n = 128 |
| Total | n = 158 |
Upon arrival of the EMS on scene, 2% (8/330) of the patients were already dead, and 1% (4/330) had ongoing CPR. At the end of the assignment (defined as either the EMS leaving the scene, delivering the patient to another EMS unit or delivering the patient to a care facility), 4% (12/330) were dead. The causes of injury are given in Fig. 1.
Figure 1.
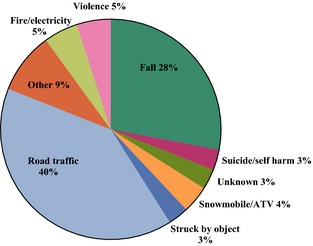
Cause of injury.
EMS response and scene
Median EMS response time, from the EMS notification by the dispatcher to the arrival at the scene, was 8.5 min (range 0–74 min). Average outside temperature was +1 °C (range −33 to 23). The scene of injury was indoors for 20% of the patients.
First aid
Figure 2 shows how often individual first‐aid measures were indicated, by per cent of cases with injured patients, and Fig. 3 shows how well each measure was performed. Whether hypothermia prevention measures were attempted was not correlated with the outside air temperature (P = 0.14, Binary Logistic Regression Analysis) or to whether the scene of injury was indoor or outdoor (P = 0.98, chi‐square test), while whether the EMTs assessed hypothermia prevention as indicated was correlated both with temperature and scene location (P < 0.01).
Figure 2.

Measure indicated and measure attempted, by per cent of cases. Absoulte numbers given for each column. Total cases = 330.
Figure 3.
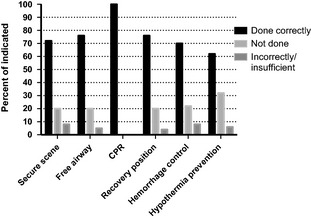
Quality of indicated first‐aid measures.
Bystanders
Bystanders were present in 97.2% of cases. There were a median of three people present at each call, with a median of one first‐aid provider per call. For 79% of calls, there was more than one bystander present.
The distribution of the first‐aid providers' professions is shown in Fig. 4A. In 25% of the cases, the bystanders were at work when the injury occurred, 45% were not at work and the situation was not documented in the remaining 30% of cases. The distribution of the first‐aid providers' professions, in cases in which they were at work but were not part of emergency services (i.e. firefighters and police officers) is shown in Fig. 4B. A total of 95% of the police officers who were acting as first aiders were at work, as were 65% of firefighters and 23% of health care personnel (not including EMS personnel in line of duty, who were excluded from the study).
Figure 4.
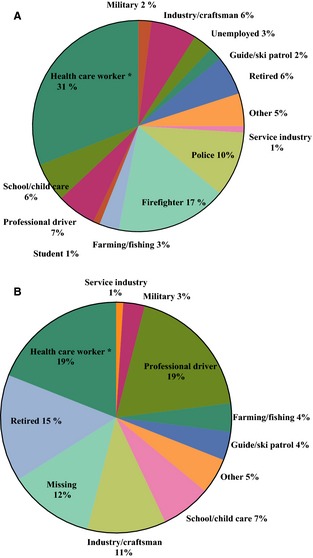
(A) Profession of 196 first‐aid providers, in cases in which the profession was recorded. (B) Distribution of professions among bystanders who were at work when acting as first‐aid providers (excluding police and firefighters). *Excluding personnel of Emergency Medical Services in line of duty.
First‐aid training and first‐aid quality
In 35% (110/330) of the cases, at least one person with first‐aid training was present; in 5% (15/330) of the cases, none of those present had first‐aid training; and in 60% of cases, the first‐aid training status was unknown. Those with documented training gave better first aid compared to those with no documented first‐aid training (P = 0.002 mean score 0.56 ± 0.75 vs. 0.15 ± 0.95, Mann–Whitney U‐test). This finding was consistent also when police, firefighters and health care personnel were excluded from analysis (P = 0.05). First‐aid quality did not vary by profession (P = 0.39, Kruskal–Wallis test).
Discussion
In this study, we found that the majority of trauma patients who needed first aid, received correct first aid from bystanders, though most first‐aid measures are relatively seldom needed. There is still room for improvement, particularly in hypothermia prevention. Health care workers, firefighters and police officers commonly act as first‐aid providers. Our findings indicate that persons with previous first‐aid training give better first aid.
There is little previous research published on bystander first aid in trauma for comparison. Pelinka et al. and Thierbach et al. published results from urban Germany and Austria.10, 11 In that material, securing of the scene was performed correctly in 87% of cases. That is better than in our study, in which this measure was performed correctly in 72% of cases. Haemorrhage control and hypothermia prevention were performed correctly more often in our study. Haemorrhage control was done correctly in 70% in our study vs. 60% in the German/Austrian study, and hypothermia prevention correctly in 62% vs. 42%. In other studies, first aid has been provided correctly in a range from 10.5% to 65% of cases.7 It is feasible that the difference is due to patients being more lightly injured in our study, or because our study area largely comprises rural areas where bystanders may have had more time to perform measures before the arrival of the EMS than in urban areas, where EMS response times may be shorter. However, in our analysis, EMS response time did not correlate with changes in first‐aid quality. First‐aid provision may be lower in other areas because helpers may fear legal repercussion, a phenomenon our area enjoys freedom from.12
In out‐of‐hospital cardiac arrest (OHCA), CPR rates internationally are reported to vary between 15% and 55%.4, 13, 14 First‐aid rates in our study were substantially higher, but in line with CPR rates for OHCA in Norway.15, 16 This suggests that bystanders in Norway are motivated to assist in medical emergencies, and are relatively well trained in first aid and CPR. Our results may thus be in the higher range of what can be expected from first‐aid coverage in trauma.
Our results are encouraging, but still with room for improvement. Particularly, prevention of hypothermia has a tendency to be forgotten, which agrees with findings from Austria and Germany.10, 11 In international guidelines and the more common Norwegian first‐aid courses, hypothermia prevention in trauma receives little attention. Hypothermia has been associated with worse outcomes in trauma, and its importance should perhaps be further stressed in guidelines and courses.17, 18, 19
Health care personnel (EMS not included) was the most common profession among the first‐aid providers. The majority were off duty, but almost a fourth were at work when acting as first‐aid providers, suggesting that they are prone to encounter situations where first aid is necessary as part of their work. The finding is in line with the findings of Mauritz et al. in a study from Vienna.20
Firefighters and police officers were also frequent as first‐aid providers. Other large groups represented were professional drivers, school and child care workers, and pensioners. Should these findings be replicated, these are professions that may be particularly singled out for first‐aid training.
First‐aid training was relatively common, with a third of first‐aid providers having undergone prior first‐aid training. Compared to those with no documented first‐aid training, persons with first‐aid training provided better first aid. There may be persons with unregistered training in the group without documented training, but this would rather reduce the observed difference. Our results supports that first‐aid training affects the quality of first aid. This study does not, however, assess whether first‐aid training makes bystanders more likely to step up and provide first aid in an emergency. Studies that have examined the effect of first‐aid training on helping behaviour are inconsistent.21
This study has several limitations. Primarily, the material does not allow for assessment of the effect of layperson first aid on survival. The effect of bystander first aid on survival needs to be established in order to determine whether the first link in the trauma chain of survival is in fact essential to the chain. A study from mine‐infested northern Iraq found a 5.8% improved survival in trauma patients receiving first aid.22 In an area with substantially lower occurrence of penetrating trauma, the effect may, however, be smaller. Autopsy studies have suggested a potential 1.8–4.5% reduction in mortality, but more clinical studies are needed.23, 24
The results in this study are based on the EMS' observations made upon arrival at the scene. Consequently, we do not know how soon after the injury the patient received first aid, or the length of time between the arrival of a layperson first‐aid provider and the EMS. Due to the study design, with the first responding EMS unit recording study data, several interesting variables were not assessed or unavailable. The most important of these is probably discerning between different levels of haemorrhage severity. The study was only granted insight into prehospital journals. These are hand‐written and not always complete leading to missing data on age, gender and cause of injury.
Conclusions
A majority of trauma victims in our region received correct first aid. Health care personnel, police officers, firefighters, professional drivers, school and child care workers, and pensioners were often first‐aid providers in trauma situations. Prior first‐aid training in first‐aid providers is likely associated with provision of better first aid. Focused efforts are needed to improve the practical hypothermia prevention training for trauma victims targeting the general population.
Acknowledgements
We are indebted to the employees of the Emergency Medical Services of Finnmark Hospital and the University Hospital of Northern Norway for supporting the study and gathering data.
Bakke HK, Steinvik T, Eidissen S‐I, Gilbert M, Wisborg T. Bystander first aid in trauma – prevalence and quality: a prospective observational study. Acta Anaesthesiologica Scandinavica 2015.
Conflicts of interest
Bakke is a previous volunteer for the Norwegian Red Cross Tromsø who receives income from first‐aid courses. He has worked as first‐aid instructor for Red Cross Tromsø. None of the other authors have any conflicts of interest to report.
Funding
Laerdal Medical Foundation, Gidske and Peter Jacob Sørensen Research Trust, the Odd Berg Groups' Medical Research Trust, and the Norwegian National Centre of Rural Medicine.
References
- 1. Pang J‐M, Civil I, Ng A, Adams D, Koelmeyer T. Is the trimodal pattern of death after trauma a dated concept in the 21st century? Trauma deaths in Auckland 2004. Injury 2008; 39: 102–6. [DOI] [PubMed] [Google Scholar]
- 2. Bakke HK, Hansen IS, Bendixen AB, Morild I, Lilleng PK, Wisborg T. Fatal injury as a function of rurality‐a tale of two Norwegian counties. Scand J Trauma Resusc Emerg Med 2013; 21: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nielsen AM, Lou Isbye D, Lippert FK, Rasmussen LS. Engaging a whole community in resuscitation. Resuscitation 2012;83:1067–71. [DOI] [PubMed] [Google Scholar]
- 4. Bray JE, Deasy C, Walsh J, Bacon A, Currell A, Smith K. Changing EMS dispatcher CPR instructions to 400 compressions before mouth‐to‐mouth improved bystander CPR rates. Resuscitation 2011; 82: 1393–8. [DOI] [PubMed] [Google Scholar]
- 5. Tannvik TD, Bakke HK, Wisborg T. A systematic literature review on first aid provided by laypeople to trauma victims. Acta Anaesthesiol Scand 2012; 56: 1222–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Davis JS, Satahoo SS, Butler FK, Dermer H, Naranjo D, Julien K, Van Haren RM, Namias N, Blackbourne LH, Schulman CI. An analysis of prehospital deaths. J Trauma Acute Care Surg 2014; 77: 213–8. [DOI] [PubMed] [Google Scholar]
- 7. Berbiglia L, Lopez PP, Bair L, Ammon A, Navas G, Keller M, Diebel LN. Patterns of early mortality after trauma in a neighborhood urban trauma center: can we improve outcomes? Am Surg 2013;79:764–7. [PubMed] [Google Scholar]
- 8. World Health Organization . ICD‐10: International Statistical Classification of Diseases and Health Related Problems, 2nd edn Geneva: WHO Press, 2004. [Google Scholar]
- 9. Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the Trauma Score. J Trauma Acute Care Surg 1989; 29: 623–9. [DOI] [PubMed] [Google Scholar]
- 10. Pelinka LE, Thierbach AR, Reuter S, Mauritz W. Bystander trauma care–effect of the level of training. Resuscitation 2004; 61: 289–96. [DOI] [PubMed] [Google Scholar]
- 11. Thierbach AR, Pelinka LE, Reuter S, Mauritz W. Comparison of bystander trauma care for moderate versus severe injury. Resuscitation 2004; 60: 271–7. [DOI] [PubMed] [Google Scholar]
- 12. Pallavisarji U, Gururaj G, Nagaraja Girish R. Practice and perception of first aid among lay first responders in a southern district of India. Arch Trauma Res 2013;1:155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I, Resuscitation Outcomes Consortium Investigators . Regional variation in out‐of‐hospital cardiac arrest incidence and outcome. JAMA 2008; 300: 1423–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stiell IG, Wells GA, Field B, Spaite DW, Nesbitt LP, De Maio VJ, Nichol G, Cousineau D, Blackburn J, Munkley D, Luinstra‐Toohey L, Campeau T, Dagnone E, Lyver M, Ontario Prehospital Advanced Life Support Study Group . Advanced cardiac life support in out‐of‐hospital cardiac arrest. N Engl J Med 2004; 351: 647–56. [DOI] [PubMed] [Google Scholar]
- 15. Lindner TW, Søreide E, Nilsen OB, Torunn MW, Lossius HM. Good outcome in every fourth resuscitation attempt is achievable ‐ an Utstein template report from the Stavanger region. Resuscitation 2011; 82: 1508–13. [DOI] [PubMed] [Google Scholar]
- 16. Lien Nilsen JM, Bo I, Rasmussen JR, Haanaes EK, Gilbert M. Doubled survival from out‐of‐hospital cardiac arrest in a rural community in north‐norway following implementation of an aggressive chest pain protocol with early prehospital thrombolysis for STEMI. Circulation 2011;124:A17087 (abstract 17087). [Google Scholar]
- 17. Markenson D, Ferguson JD, Chameides L, Cassan P, Chung KL, Epstein J, Gonzales L, Herrington RA, Pellegrino JL, Ratcliff N, Singer A. Part 17: first aid: 2010 American Heart Association and American Red Cross Guidelines for First Aid. Circulation 2010; 122(18 Suppl. 3): 934–46. [DOI] [PubMed] [Google Scholar]
- 18. Norsk Førstehjelpsråd (Norwegian First Aid Council) . Norsk Grunnkurs i Førstehjelp. Stavanger, Norway: Lærdal Medical A/S, 2011. [Google Scholar]
- 19. Søreide K. Clinical and translational aspects of hypothermia in major trauma patients: from pathophysiology to prevention, prognosis and potential preservation. Injury 2014; 45: 647–54. [DOI] [PubMed] [Google Scholar]
- 20. Mauritz W, Pelinka LE, Kaff A, Segall B, Fridrich P. Maßnahmen durch Ersthelfer am Unfallort Eine prospektive, epidemiologische Studie im Raum Wien. Wien Klin Wochenschr 2003; 15: 698–704. [DOI] [PubMed] [Google Scholar]
- 21. He Z, Wynn P, Kendrick D. Non‐resuscitative first‐aid training for children and laypeople: a systematic review. Emerg Med J 2014; 31: 763–8. [DOI] [PubMed] [Google Scholar]
- 22. Murad MK, Husum H. Trained lay first responders reduce trauma mortality: a controlled study of rural trauma in Iraq. Prehosp Disaster Med 2010; 25: 533–9. [DOI] [PubMed] [Google Scholar]
- 23. Ashour A, Cameron P, Bernard S, Fitzgerald M, Smith K, Walker T. Could bystander first‐aid prevent trauma deaths at the scene of injury? Emerg Med Australas 2007; 19: 163–8. [DOI] [PubMed] [Google Scholar]
- 24. Henriksson E, Oström M, Eriksson A. Preventability of vehicle‐related fatalities. Accid Anal Prev 2001; 33: 467–75. [DOI] [PubMed] [Google Scholar]


