Abstract
Background:
Establishing rapport is an important step in physician–patient communication resulting in a positive effect on patient satisfaction and overall clinical outcomes. However, there is a dearth of studies on the condition of doctor–patient relations in Saudi Arabia. This study was performed to estimate the proportion of physicians who have a good rapport with patients in their practice and the proportion of satisfied attendees.
Materials and Methods:
A cross-sectional study was conducted at a Primary Health Care Center, Dammam, KSA. The data were collected through a structured self-administered questionnaire given to samples of attendees and physicians to estimate patient satisfaction and the practice of rapport by physicians.
Results:
A total of 374 attendees and 27 physicians participated in the study. The percentage of physicians who had good rapport was 51.9%. Factors that showed significant relationship with rapport practice were: Physician's age (p = 0.016), physician's experience (p = 0.043), and professional status (p = 0.031). The attendees satisfied with their physician's rapport with them were 50.5%. Factors that showed significant relationship with satisfaction were: Attendee's age (p < 0.0001), educational level (p < 0.0001), having a chronic illness (p < 0.0001), having appointment (p < 0.0001), physicians' professional status (p < 0.0001), and a nonsurgical specialty (p < 0.0001).
Conclusion and Recommendation:
Physicians' rapport with patients and patients' satisfaction with physicians' empathy is not high. Training is required to optimize physician–patient communication.
Keywords: Patient rapport, patient satisfaction, Saudi Arabia
INTRODUCTION
Good doctor communication skills are important in all aspects of patient care. They help to achieve an accurate diagnosis, build trust with patients, and improve compliance to treatment, overall patient satisfaction, therapeutic outcome, and avoid litigation.[1,2,3,4] The skills are considered an essential component of high-quality health care.[5]
The initial and most important step in communication with patients is the establishment of rapport. This may take time, but will definitely decrease the patient's tension and fear and improve doctor–patient relationship, which in turn creates a strong base for further management. Rapport is established through a series of verbal and nonverbal means of communication such as smiling, introducing oneself, calling the patient by the preferred name, making eye contact and assuming a welcoming posture, and showing empathy.[6] When communication improves, the risk of malpractice may decrease, but compliance, patient satisfaction, and outcomes improve. Moreover, physicians who use their rapport-building skills often experience less stress in their work and are more satisfied.[7]
Building rapport, as an essential part of physician–patient communication and relationship, needs training that emphasises on using the local language and being aware of the cultural attributes of patients.[8] These play a huge role in communication with patients. For example, in the KSA, many patients prefer to be called by a nickname that includes their oldest son's name, but shaking hands with the opposite sex is unacceptable.
Communication skills have not been part of some of the study curricula in pregraduate medical schools in Saudi Arabia. Furthermore, foreign doctors, even those who are trained in communication skills have difficulty in applying their skills due to language problem and cultural barriers.[9]
The objective of this study was to assess the establishment of rapport with patients by physicians working in the Primary Health Care Center (PHCC), Dammam City, KSA and assess patients' satisfaction with that relationship.
MATERIALS AND METHODS
A cross-sectional study was carried out at the PHCC in Dammam, KSA.
All physicians and patients at the PHCC, Dammam, who were more than 15 years of age and were mentally and physically able to communicate in simple Arabic about their medical care were included. Patients who were <15 years of age and unable to communicate verbally (e.g., speech disorder and hearing impairment) were excluded.
All attendees were cared for at one PHCC where 30 physicians provided health care. Using the automated sample size calculator, the sample size of attendees was estimated at 374 subjects from the PHCC with a total population of 9000 patients per month, with a confidence interval of 5%. The sample size of the physicians was a comprehensive sample of all 30 physicians, 27 (90.0%) of whom participated in the study.
The patient sample of attendees was selected using a systemic sampling procedure, whereby every seventh patient visiting the PHCC, Dammam, on two days per week, over a period of 3 weeks was selected. The two days were randomly selected from Sunday to Thursday. The days were divided into morning and afternoon clinics. On day 1, the females were taken in the morning, and the males in the afternoon and the converse was done on the 2nd day of that week.
Data were collected using a self-administered structured questionnaire completed by the selected physicians and attendees visiting the PHCC, Dammam, under direct supervision.
The rapport questionnaire included 19 questions. Each positive and negative response was assigned a mark of “1” or “0”, respectively. A rapport score was computed as the sum of all positive answers of the rapport questions. Score values equal or greater than the median were considered as “good”, and those below as “poor.” The rapport score was treated as the dependent variable and the independent variables included age (categorized as young, middle or elderly), gender, years of experience (categorized as short, average, and long), job title (general practitioner, resident, specialist, and consultant), whether speaks Arabic or not, and whether the primary language is Arabic or not Arabic. In addition, physicians were categorized into those whose specialty was of a surgical nature, i.e., whether the management of their patients involved surgical procedures or not.
Attendee's satisfaction was measured by 21 questions. Each positive and negative response was assigned a mark of “1” or “zero,” respectively. The score for satisfaction with rapport was computed as the sum of all positive answers on the rapport questions. Score values equal or greater than the median were considered as “good”, and those bellow it as “poor.” Satisfaction with the rapport score was similarly treated as the dependent variable for which the independent variables included age, gender, level of education, residence, with or without a chronic disease, with or without an appointment, visit type, physicians' specialty, and language.
Age was recorded to the nearest year and subjects were categorized as young (<30 years), middle-aged (30–54 years), or elderly (55 years and over); level of education was defined as low (illiterate and primary school), intermediate (intermediate and high school), or high(university graduates or postgraduate); has or does not has chronic disease, e.g. diabetes mellitus, hypertension, bronchial asthma, and sickle cell anemia; with or without an appointment; visit type defined as new or follow-up; physicians' specialty categorized as surgical or nonsurgical involving surgical means of patient management; physicians' professional status recorded as consultant, specialist or other; and physicians' language defined as Arabic or non-Arabic. Physicians' experience was categorized as short (<5 years), intermediate (5–9 years), and long (10 years and over).
Data were entered into the computer and analyzed using the Statistical Package for Social Sciences (SPSS), version 20.0. Frequency distribution tables were generated. Rapport scores for physicians and satisfaction scores for attendees were computed.
These proportions were tested against the independent variables using the Chi-squared test. A p-value < 0.05 was considered as indicative of statistical significance. Significant relations were further subjected to logistic regression analysis.
The questionnaires' reliability, as tested by SPSS, using the Split half Guttman method, was 67.1% and 79.3% for patients' and physicians' questionnaires, respectively.
All information regarding subjects and physicians were treated with the strictest confidentiality.
The study proposal was approved by the Research Committee of the National Guard Health Authority, Eastern Region, as well as by the Local Supervisory Training Committee for Family Medicine, in the Eastern Province, KSA.
A pilot study involving 20 subjects was carried out to test the logistics of the study, but the data were not included in the main study.
RESULTS
A total of 374 attendees participated in the study with a response rate of approximately 92% and 27 physicians participated with a response rate of 90.0%.
The attendees' mean age was 37.12 ± 11.2 years (mean ± standard deviation [SD]), with a range of 16–75 years. Attendees in the young, middle-aged, and elderly groups were 46.8%, 44.4%, and 8.8%, respectively. Females and males in the sample were 55.9% and 44.1%, respectively [Table 1]. Attendees residing in Dammam made up 75.7% of the total, 19.8% resided in Al-Khobar and 4.5% in other areas. About one-fourth of the attendees had low education. The majority (59.1%) had average education, and very few were highly educated [Table 2].
Table 1.
Sociodemographic characteristics of study sample in relation to rapport score at primary health care center, Dammam, Kingdom of Saudi Arabia, 2013
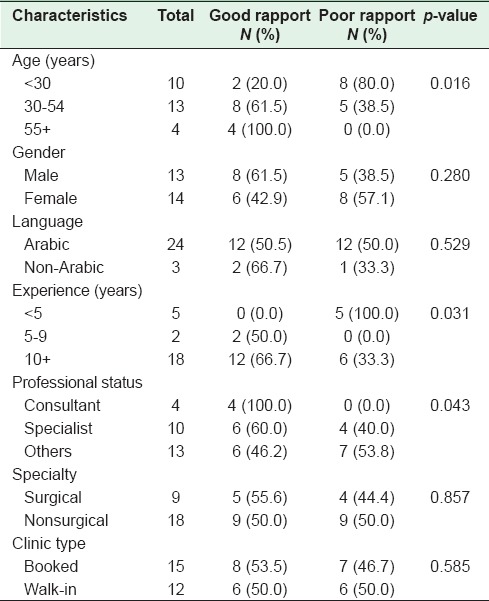
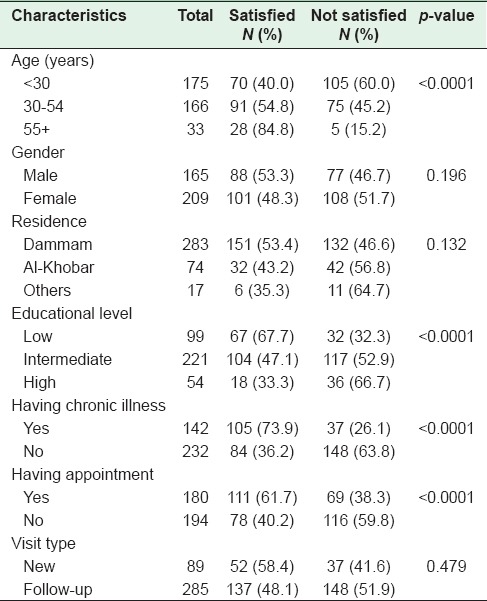
Table 2.
Relation of the study sample attendees satisfaction with sociodemographic and disease-related variables at the primary health care center, Dammam, Kingdom of Saudi Arabia, 2013
Almost 40.0% of the attendees had chronic illnesses. Those who had appointments were 48.1%, while those attending as walk-in were 51.9%. About 75% were seen by physicians with a nonsurgical specialty, and 25.4% were seen by physicians whose specialty was surgical in nature. Fourteen percent physicians were consultants, 31.0% were specialists, and 54.5% were of junior status [Table 3].
Table 3.
Physicians’ characteristics in relation to attendees’ satisfaction score with the physicians at primary health care center, Dammam, Kingdom of Saudi Arabia, 2013

The attendees seen by male and female physicians were 44.9% and 55.1%, respectively. Ninety four percent were seen by Arabic-speaking physicians and 6.0% were seen by non-Arabic speaking physicians. For 23.0%, it was the first visit to the physician, while for 77%, it was a follow-up visit.
The physicians' mean age was 41 ± 9.9 years (mean ± SD) with a range of 25–58 years. Young physicians constituted 37.0%, middle-aged physicians 48.1%, and older physicians were 14.8% of the sample. Male physicians amounted to 48.1% while female physicians were 51.9%. The mother tongue of 88.9% of the physicians was Arabic and for 11.1% it was not Arabic. The mean years of experience was 14.9 ± 8.4 years (mean ± SD). Physicians with short experience (working years for 1–6 years) came to 40.7%, 22.2% of the physicians had average experience (7–12 years), while 37.0% had long experience (more than 12). Consultants constituted 14.8%, specialists 37%, and others 48.2%. For 66.6% of the physicians, the specialty was nonsurgical and 33.3%had surgical specialties. Physicians with booked clinics were 55.6% while those with walk-in clinics were 44.4%. The percentage of physicians with good Rapport Practice Score was 51.9% with a mean rapport score of 71.8% ± 11 (mean ± SD), and a range of 47.4–91.2%.
Regarding the relation of sociodemographic and clinical characteristics of the study sample physicians with Rapport Practice Score, there were significantly more older physicians than younger ones who had a good rapport score (p < 0.016). Significantly more physicians with long experience than those with shorter experience had a good rapport score (p < 0.031, and p < 0.031, respectively). Furthermore, significantly more consultant physicians than the rest had a good rapport score (p < 0.043) [Table 1].
Attendees who were satisfied with their physician's rapport with them amounted to 50.5% while 49.5% were dissatisfied. The mean satisfaction score was 77.7% ± 16.9 (mean ± SD) with a range of 20.6–100%.
Significantly more elderly attendees, those with a lower level of education, those with chronic illnesses, and those with fixed appointments were satisfied with physicians' rapport than other groups (p < 0.0001) [Table 2].
Regarding physicians' characteristics, significantly more consultant physicians and those with nonsurgical specialties affected attendees' satisfaction (p < 0.0001) [Table 3].
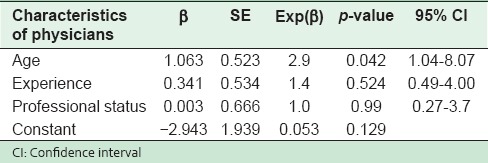
Logistic regression analysis of the relation of significant factors predicting Rapport Practice Score among study sample physicians showed that the age of the physician was a significant predictor of a good rapport score (p < 0.042) [Table 4].
Table 4.
Logistic regression analysis of variables predicting Rapport Practice Score among study sample physicians at primary health care center, Dammam, Kingdom of Saudi Arabia, 2013
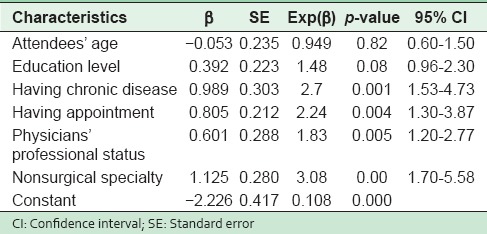
Moreover, logistic regression analysis of the relation of significant factors predicting satisfaction score among study sample attendees showed that attendees with chronic diseases, those with a prefixed appointments and those seen by consultant physicians, as well as those seen by nonsurgical physicians were significantly satisfied with the attention received (p < 0.001, p < 0.004, p < 0.005, and p < 0.000, respectively)[Table 5].
Table 5.
Logistic regression analysis of variables predicting satisfaction score among study sample attendees at primary health care center, Dammam, Kingdom of Saudi Arabia, 2013
DISCUSSION
In this study, the sample of attendees comprised mainly the young and middle-aged, providing a wide spectrum of ages. The percentages of females and males were almost the same, is roughly representative of the population of Saudi Arabia. The education of the majority of the study sample attendees average which is similar to the population of Saudi Arabia as published by the Central Department of Statistics and Information, Saudi Arabia, 2013.[10]
The percentage of satisfied attendees was 50.5%, and in a PHCC setting, which is considered the main venue for health care provision, and continuous care, this percentage is mediocre, especially since the range of ages sampled is very wide, covering almost all age groups. Research has shown good communication skill to be the key to better patient outcomes, and better patient satisfaction.[11] Also, patients' satisfaction appears to be a strong motivation for compliance to treatment and its success. Good rapport is essential for achieving proper doctor–patient relations, improving patient satisfaction and treatment compliance, and improving patient outcomes.[12] The physician's communication skills have a significant impact on physician-patient relationship. For instance, physicians who are warm, friendly, and understanding demonstrate better rapport with their patients than those who are not. These factors can increase patient compliance and improve treatment outcomes.[12,13,14]
The study revealed that most attendees were seen by physicians who were not consultants, and who displayed little rapport with their patients thus failing to stimulate much attendee satisfaction. The lack of skills for building rapport in Saudi Arabian hospitals may be explained by the fact that though physicians are of diverse nationalities, religions and cultures, and speak different languages, they all have to deal with the cultural norms, religion, and language of the Saudi population. Moreover, since these factors influence rapport building the lack of training on communication skills is made all the more obvious. It appears that the ideal circumstances for optimal communication in health care are for both physicians, especially primary care physicians, and patients to speak the same language.[15] Besides, the physician is required to identify with and respect different values, beliefs, cultural norms, especially those related to gender and social circumstance.[16,17] Unfortunately, there does not seem to be many programs that train physicians on communication skills, nor are there studies to address this problem in Saudi Arabia in general and in PHCCs in particular.
Elderly attendees and those with little education indicated greater satisfaction than younger and more educated attendees. In addition, those with chronic illnesses and those who had appointments were also better satisfied than others.
Research has shown that satisfaction was related to patients' age, psychological morbidity, and most significantly satisfaction with the length of waiting time at the clinic, which was less for patients who had appointments.[18] In addition, patients' confidence and trust in their physicians increased with the patient's age.[19] Another possible explanation is that patients with chronic illness usually had constant health care at booked clinics, where a good relationship with their caregiver had already been built. This shows the importance of continuity of health care and the fact that sustained continuity of care is associated with improved patient satisfaction, especially in patients with chronic conditions.[20] Furthermore, it was found that continuity of care was associated with a lower rate of visits to the Emergency Department and hospitalization. In addition, continuity of care improves the quality of the patient–physician communication and relationship, management of patients with chronic conditions, and patients' quality of life.[21,22] This may also explain the dissatisfaction of walk-in attendees or low rapport scores because walk-in patients tend to impose an unusual burden on the physician. A system should, therefore, be developed to deal effectively with the attendance of walk-in patients.
Visiting a physician with a high professional status was also observed to be positively related to satisfaction with physicians' empathy, while the gender of the physician and the language had no such effect. It was found that surgeons' expression of empathy with patients was infrequent, and any social conversation was brief.[23] It has been documented that the specialty physician had an effect on patterns of communication and on patient satisfaction, for the satisfaction of the patients of family physicians was more closely linked to rapport building, psychosocial exchange, and patient-centeredness than they were for other specialties.[24]
Similar to the satisfaction score, Physicians' Practice Score for Rapport was moderate, only 51.9%. Some factors affecting rapport score were found significant in this study. It was found that the older the physician, the better he/she was in establishing rapport. Also, more consultants and highly experienced physicians had better rapport scores than others. The reason for this is that the development of a good relationship with patients comes with time and certain skills.[25] This improved communication can only be developed through mutual trust, and respect which promotes the development of a therapeutic relationship.[26,27] However, rapport and good communication with patients are not skills that are easily acquired. These have to be developed through training and practice. Nonetheless, practitioners who are clinically competent, consistent, honest, and committed to their patients are able to further the building of patient trust and improve communication, rapport, and outcomes.[28]
CONCLUSION AND RECOMMENDATION
Though the establishment of rapport is important when dealing with patients, it is not given much attention. It is the responsibility of the health care providers to give more training to improve their skills and practice to create better physician–patient relationship, enhance patient satisfaction, and improve patient outcomes. Moreover, the study showed that attendees' satisfaction with physicians' empathy was not high. Measures need to be taken to train physicians on the skills of doctor–patient communication and relations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bertakis KD, Roter D, Putnam SM. The relationship of physician medical interview style to patient satisfaction. J Fam Pract. 1991;32:175–81. [PubMed] [Google Scholar]
- 2.Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: A systematic review. J Am Board Fam Pract. 2002;15:25–38. [PubMed] [Google Scholar]
- 3.Pinto RZ, Ferreira ML, Oliveira VC, Franco MR, Adams R, Maher CG, et al. Patient-centred communication is associated with positive therapeutic alliance: A systematic review. J Physiother. 2012;58:77–87. doi: 10.1016/S1836-9553(12)70087-5. [DOI] [PubMed] [Google Scholar]
- 4.Marei HF. Medical litigation in oral surgery practice: Lessons learned from 20 lawsuits. J Forensic Leg Med. 2013;20:223–5. doi: 10.1016/j.jflm.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine (IOM) Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 6.Brown T, Williams B, Boyle M, Molloy A, McKenna L, Molloy L, et al. Levels of empathy in undergraduate occupational therapy students. Occup Ther Int. 2010;17:135–41. doi: 10.1002/oti.297. [DOI] [PubMed] [Google Scholar]
- 7.Barnett PB. Rapport and the hospitalist. Am J Med. 2001;111:31S–5S. doi: 10.1016/s0002-9343(01)00967-6. [DOI] [PubMed] [Google Scholar]
- 8.Dorgan KA, Lang F, Floyd M, Kemp E. International medical graduate-patient communication: A qualitative analysis of perceived barriers. Acad Med. 2009;84:1567–75. doi: 10.1097/ACM.0b013e3181baf5b1. [DOI] [PubMed] [Google Scholar]
- 9.Ramaswamy R, Williams A, Clark EM, Kelley AS. Communication skills curriculum for foreign medical graduates in an internal medicine residency program. J Am Geriatr Soc. 2014;62:2153–8. doi: 10.1111/jgs.13094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Forty-Nine Issues. Saudi Arabia: The Central Department of Statistics and Information; 2013. Statistical Year Book. [Google Scholar]
- 11.Lang EV. A better patient experience through better communication. J Radiol Nurs. 2012;31:114–9. doi: 10.1016/j.jradnu.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Najavits LM, Strupp HH. Differences in the effectiveness of psychodynamic therapists: A process-outcome study. Psychotherapy. 1994;31:114–23. [Google Scholar]
- 13.Barnett PB. Rapport and the hospitalist. Am J Med. 2001;111:31S–5S. doi: 10.1016/s0002-9343(01)00967-6. [DOI] [PubMed] [Google Scholar]
- 14.Williams DD, Garner J. The case against “the evidence”: A different perspective on evidence-based medicine. Br J Psychiatry. 2002;180:8–12. doi: 10.1192/bjp.180.1.8. [DOI] [PubMed] [Google Scholar]
- 15.Sears J, Khan K, Ardern CI, Tamim H. Potential for patient-physician language discordance in Ontario. BMC Health Serv Res. 2013;13:535. doi: 10.1186/1472-6963-13-535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cole MB, McLean V. Therapeutic relationships re-defined. Occup Ther Ment Health. 2003;19:33–56. [Google Scholar]
- 17.Harkreader H. Fundamentals of Nursing: Caring and Clinical Judgment. Philadelphia: WB Saunders; 2000. [Google Scholar]
- 18.Shilling V, Jenkins V, Fallowfield L. Factors affecting patient and clinician satisfaction with the clinical consultation: Can communication skills training for clinicians improve satisfaction? Psychooncology. 2003;12:599–611. doi: 10.1002/pon.731. [DOI] [PubMed] [Google Scholar]
- 19.Croker JE, Swancutt DR, Roberts MJ, Abel GA, Roland M, Campbell JL. Factors affecting patients' trust and confidence in GPs: Evidence from the English national GP patient survey. BMJ Open. 2013;3:pii: E002762. doi: 10.1136/bmjopen-2013-002762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Health Quality Ontario. Continuity of care to optimize chronic disease management in the community setting: An evidence-based analysis. Ont Health Technol Assess Ser. 2013;13:1–41. [PMC free article] [PubMed] [Google Scholar]
- 21.Nyweide DJ, Anthony DL, Bynum JP, Strawderman RL, Weeks WB, Casalino LP, et al. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Intern Med. 2013;173:1879–85. doi: 10.1001/jamainternmed.2013.10059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dreiher J, Comaneshter DS, Rosenbluth Y, Battat E, Bitterman H, Cohen AD. The association between continuity of care in the community and health outcomes: A population-based study. Isr J Health Policy Res. 2012;1:21. doi: 10.1186/2045-4015-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levinson W, Chaumeton N. Communication between surgeons and patients in routine office visits. Surgery. 1999;125:127–34. [PubMed] [Google Scholar]
- 24.Paasche-Orlow M, Roter D. The communication patterns of internal medicine and family practice physicians. J Am Board Fam Pract. 2003;16:485–93. doi: 10.3122/jabfm.16.6.485. [DOI] [PubMed] [Google Scholar]
- 25.Kennedy M. In doc we trust. Building rapport with young patients takes time and skill. WMJ. 2000;99:33–6. [PubMed] [Google Scholar]
- 26.Fox V. Therapeutic alliance. Psychiatr Rehabil J. 2002;26:203–4. doi: 10.2975/26.2002.203.204. [DOI] [PubMed] [Google Scholar]
- 27.Myers DG. Psychology. 4th ed. New York: Worth Publishers; 1995. [Google Scholar]
- 28.Usherwood T. Understanding the Consultation: Evidence, Theory and Practice. Buckingham: Open University Press; 1999. [Google Scholar]


