Abstract
Background:
Since the data of primary hypertension (HT) in children is scanty in India, this study attempted to evaluate HT by a multidimensional investigation of the various risk factors in children and adolescents.
Materials and Methods:
A total of 3906 subjects were recruited, all of whom lived in Chennai, an urban area of Tamil Nadu. The children and adolescents aged from 10 to 17 years were selected by random sampling. The children/adolescents were randomized into one control and further divided into two groups. The National High Blood Pressure Education Program fourth report (2004) and anthropometric body mass index (BMI), food frequency questionnaire (PURE) were followed in the study.
Results:
Out of 3906 children, 2107 were girls and 1799 boys. On screening, we found 9.5% to be hypertensive with the prevalence rate of boys and girls 8% and 10.8%, respectively. Overall obesity was 2.7%, (boys 2%, girls 3.32%); hypertensives and normotensives were 8.4% and 2.1%, respectively. We found that overweight (odds ratio [OR]: 2.06 [1.40–3.01] 95% confidence interval [CI]), obese children (OR: 1.21 [2.72–6.48] 95% CI), and those with a family history of HT (OR: 1.66 [1.20–2.30] 95% CI) had increased risk of hypertension. Females were 1.39 times (OR: 1.39 [1.11–1.72] 95% CI) more at risk of getting HT. Multivariate analysis showed that obese children/adolescent were four times more likely to have HT than children with normal BMI (OR: 4.67 [3.00–7.26] 95% CI].
Conclusion:
Family history of HT, obesity, and female gender are associated with a high risk of HT. The prevalence of HT was higher among obese adolescents than among slender subjects. This may be related to their sedentary lifestyle, faulty eating habits, high fat content in the diet and little physical activity.
Keywords: Children, hypertension, Indian adolescents, obesity
INTRODUCTION
Hypertension (HT) is not an adult disease anymore; it is a silent disease that is generally asymptomatic in childhood and adolescent period.[1] Hypertension is the main risk factor for renal, cardiac, and cerebrovascular diseases.[1,2] It plays the important pathophysiological role in the development of the reduction in baroreflex sensitivity and retinal alteration.[3] Hypertension studies in children and adolescents are of great importance since control at this stage is likely to prevent adverse sequelae in later life.[4] Hypertension is a major cause of morbidity, which unless controlled in early life, may tend to introduce a high risk in adulthood. A previous worldwide report records the prevalence of hypertension in children as ranging from 3% to 16.2%.[4,5,6] The diversity of the results in hypertension studies stems from the different criteria used, selection of the age group and study population (ethnic), study area (urban and rural), culture, as well as dietary habits (socioeconomic).[1,4,7] This study was to detect the prevalence and risk factors of hypertension in children/adolescents aged 10 to 17 years.
MATERIALS AND METHODS
The objectives and the importance of the study were first explained to the teachers and parents. The children/adolescents aged 10–17 years in each selected school in Chennai were examined. Two field survey teams, each comprising a medical officer and a social scientist were formed. The physician elicited medical history and carried out clinical examination including measurement of blood pressure (BP). The social scientist recorded the background information such as the food frequency questionnaire (FFQ) and anthropometric measurements. After getting the child to sit for five minutes, with the back supported and both feet on the floor, systolic and diastolic blood pressures (SBP) were measured on the right arm extended over a table at the level of heart with a calibrated standard sphygmomanometer. A set of different sized cuffs was used to circle the arm completely up to two-thirds of the upper arm without overlapping. Systolic pressure was recorded when the initial sound was heard (Phase I of the Korotkoff sound); diastolic pressure was recorded at the disappearance of the sound (Phase V of the Korotkoff sound). The cuff was deflated at a rate not >2 mmHg/s. BP was taken three times at 2–3 min intervals. The arithmetic mean of these three sitting BP measurements was used as the mean sitting office BP (MSSBP). A cross check of 5–7% of the hypertension subjects at different times by different teams was done for both accuracy and consistency. All BP measurements were recorded in the source documents. Every effort was made to avoid staff-child interaction, such as talking, in order to maximize reproducibility. Every effort was made to have the same staff member take the BP measurements of the same child, at the same time of day, using the same equipment.
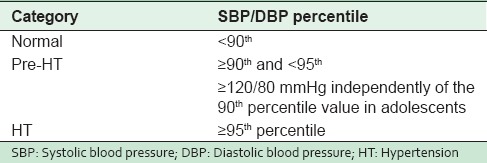
Hypertension was defined as MSSBP above the 95th percentile for age, gender, and height as per recommendation of the National High Blood Pressure Education Program Working Group on high BP in children/adolescents (NHBPEP Fourth Report 2004).[8] The height and weight were measured with the child standing without shoes; body mass index (BMI) was calculated for all children/adolescents. They were categorized according to their BMI as obese (or) overweight. Information on risk factors for hypertension like family history of hypertension and diabetes mellitus were asked for their socioeconomic status was also assessed. Their reduced physical activities (arbitrarily children who engaged in a physical activity <30 min for 4 days per week) posed a high risk. Hours of watching television and their monthly consumption of oil were also noted as high risk factors. The fourth report on the diagnosis, evaluation and treatment of high BP in children and adolescents is an authentic source of childhood and adolescent hypertension (2004). In this report, BP is classified into three categories based on percentile values [Table 1].
Table 1.
Definition and classification of hypertension in children/adolescents
We followed the same FFQ-PURE study from the South India described earlier[9] for the study monthly per capital income was assessed by the children with a score of 16–29, and above; modified Kuppusamy scale (2007) was assigned to the upper socioeconomic status and <15 lower socioeconomic status.[10] The factors found to be significant by univariate analysis, namely the family history of hypertension, diabetes mellitus, obesity, high socioeconomic status, and female gender were included for multivariate analysis. The data were collected and entered, after which we manually checked and rechecked for accuracy. Any inconsistencies found were resolved using the raw data. The association was studied in a univariate analysis by Pearson Chi-square test. Those variables found to be significantly associated were then studied by multivariate analysis logistic regression. Statistical software SPSS 11.5 for Windows was utilized to analyze data. A P-value ≤ 0. 0 5 was considered statistically significant.
RESULTS
The study sample comprised a total of 3906 children/adolescents from various schools. They were screened for hypertension and associated risk factors. There were 2107 girls and 1799 boys [Table 2].
Table 2.
Prevalence of hypertension among 10-17 year old children and adolescents by age and gender
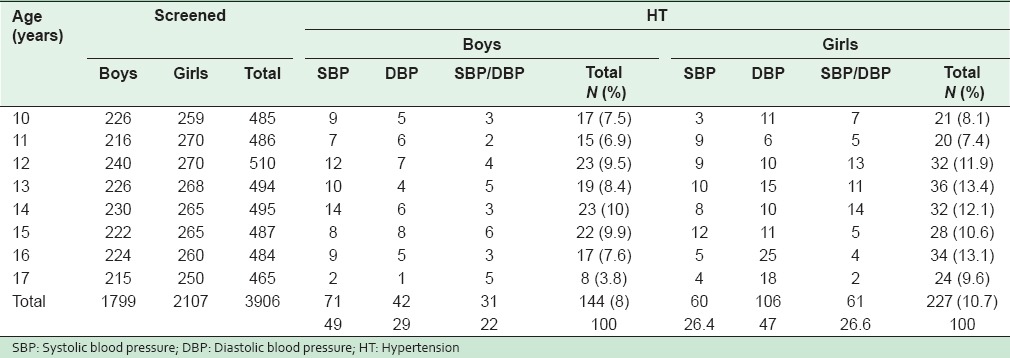
The overall prevalence of hypertension was 9.5% (371) of 3906 children/adolescents studied; the prevalence of hypertension in boys was 8% (144 of 1799) with peak prevalence around 12–15 years of age. Isolated systolic hypertension was found in 71 (29%) of the 144 children. Children/adolescents with both systolic and diastolic hypertension were 31 (21%) out of 144. Of the girls, the overall prevalence was 10.7% (227) of 2107 children, with peak prevalence around 12–16 years of age. Isolated systolic hypertension was present in 60 girls (26.4%); diastolic hypertension alone was seen in 106 children (47%) and 61 (26.6%) out of 227 children had both systolic and diastolic hypertension. Univariate analyses of risk factors for hypertension in these children/adolescents were done [Table 3].
Table 3.
Univariate analysis for association between various risk factors and hypertension among 10-17 year old children and adolescents
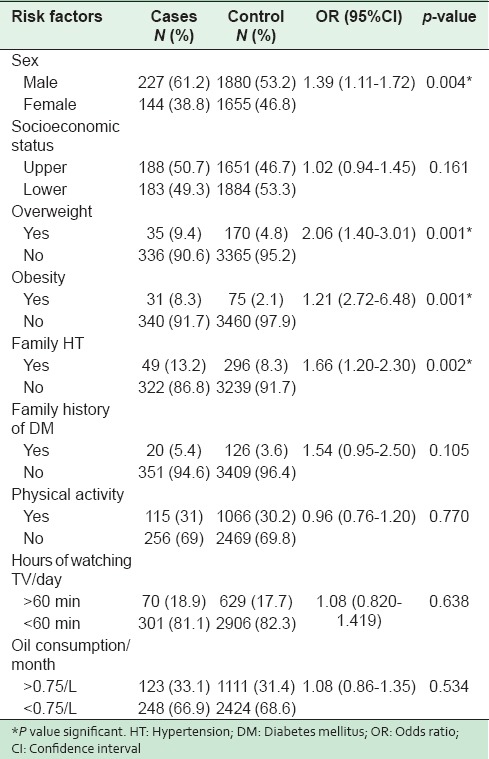
The overall prevalence of obesity was 2.7% among the hypertensives (106 out of 3906); 2.1% (75 out of 3535) in the normotensive obesity in boys was 2% (36 out of 1799) and 3.32% (70 out of 2107) in girls. The overall prevalence of overweight was 5.25% (205 out of 3906). In normotensives, the prevalence of overweight was 4.8% (170 out of 3535) and it was 9.43% (35 out of 371) in hypertensives. Overweight in boys was 2.17% (39 out of 1799) and 7.87% (166 out of 2107) in girls. A positive family history of hypertension among hypertensives was 13.2% compared to 8.3% of the normotensives. A positive family history of diabetes mellitus in the hypertensives was 5.3% as against 3.6% of the normotensives. The prevalence of hypertension in children/adolescents of low socioeconomic families was 8.85% as against 10.2% in children/adolescents of high socioeconomic families. Children/adolescents with hypertension were more likely to be obese than children/adolescents with normal BP (odds ratio [OR]: 1.21 [2.72–6.48] 95% confidence interval [CI]). Children/adolescents with hypertension were 1.6 times more associated with a family history of hypertension than children with normal BP (OR: 1.66 [1.20–2.30] 95% CI) Children who had hypertension were 1.3 times more likely to be girls than the normotensives (OR: 1.39 [1.11–1.72] 95% CI). Other risk factors were not found to be significant by univariate analysis.
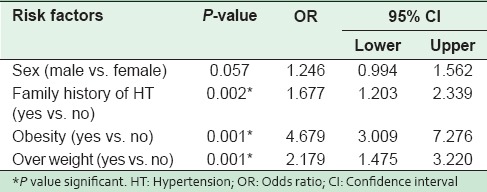
The factors found to be significant by univariate analysis were included in multivariate analysis [Table 4]. Family history of hypertension (OR: 1.67 [1.21–2.33] 95% CI) obesity (OR: 4.67 [3.00–7.27] 95% CI), and overweight (OR: 2.17 [1.47–3.22] 95% CI) were found to be independent risk factors associated with hypertension in the study population. Other risk factors were not found to be significant by univariate analysis. Multivariate logistic regression showed that cases had 1.67 times higher family history, were 4.67 times more obese and were 2.17 times more overweight compared to control children.
Table 4.
Multiple logistic regression analysis - factors for hypertension in children and adolescents aged 10-17 years
DISCUSSION
The mean systolic and diastolic BP levels of children were studied in relation to age in both males and females. In both sexes, blood pressure increased progressively with age. The gradual increase in mean systolic and diastolic BP of boys and girls with age noted agrees with the findings in the task force committee report and other studies.[1,8] The mean SBP for boys in various age groups were higher than girls. The difference in diastolic pressure between boys and girls was negligible. The varying results may be due to varying age groups in the study, the different criteria adopted to define hypertension, and the basic differences between racial groups as relates to geographic, dietary, and cultural factors.[1,4,5,11,12,13,14] In this study, there were more hypertensive girls (10.8%) than boys (8.0%), results which do not correlate with those of other studies,[14] in which hypertensive boys were 11.9%; girls were 11.4%; prevalence of overweight (7.87%) and obesity (3.32%) in girls was higher than overweight (2.17%) and obesity (2%) in boys.
In our study, the prevalence of obesity was 2.7%, which is higher than that reported by another another study.[5] The reason for the increased prevalence could be the changing lifestyles. Positive family history of diabetes mellitus among hypertensives was 5.3% as against 3.6% in normotensives, which is similar to the study by Chanda et al., in which it was 5.4% in hypertensives and 3.1% in normotensives.[15] Hypertension in obese children/adolescents was 8.35%, which was twice what was observed by other study groups.[5,15] In this study, there was a positive family history of hypertension in 8.3%, which is less than what was observed by another Indian study.[16] Significant risk factors for hypertension in adolescents in our study by univariate analysis were obesity, overweight, and a positive family history of hypertension, which agreed with a previous study.[16]
CONCLUSION
There is an increasing trend toward a high prevalence of hypertension in children of school age as a result of obesity and positive family history of hypertension and diabetes mellitus. High socioeconomic status, faulty lifestyle, dietary habits, and physical inactivity are key factors which must be dealt with immediately and aggressively. Based on our findings, hypertension is no more a disease that comes at a later stage in life. It has its roots in the young. It is crucial to advise obese children to modify their lifestyle with respect to diet, exercise, and salt intake to maintain a normal BP and avoid the childhood onset of adult hypertension.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We sincerely thank Director, (ICH and HC, Chennai) for support of this work. We thank the principals and teachers of the Middle and High School in each zone of Chennai. We thank the staff nurses, post graduate students, and social workers of ICH and HC, Chennai for valuable help throughout the study.
REFERENCES
- 1.Martin L, Oepen J, Reinehr T, Wabitsch M, Claussnitzer G, Waldeck E, et al. Ethnicity and cardiovascular risk factors: Evaluation of 40,921 normal-weight, overweight or obese children and adolescents living in Central Europe. Int J Obes (Lond) 2015;39:45–51. doi: 10.1038/ijo.2014.167. [DOI] [PubMed] [Google Scholar]
- 2.ESCAPE Trial Group. Wühl E, Trivelli A, Picca S, Litwin M, Peco-Antic A, et al. Strict blood-pressure control and progression of renal failure in children. N Engl J Med. 2009;361:1639–50. doi: 10.1056/NEJMoa0902066. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell P, Cheung N, de Haseth K, Taylor B, Rochtchina E, Islam FM, et al. Blood pressure and retinal arteriolar narrowing in children. Hypertension. 2007;49:1156–62. doi: 10.1161/HYPERTENSIONAHA.106.085910. [DOI] [PubMed] [Google Scholar]
- 4.Falkner B, Cossrow ND. Prevalence of metabolic syndrome and obesity-associated hypertension in the racial ethnic minorities of the United States. Curr Hypertens Rep. 2014;16:449. doi: 10.1007/s11906-014-0449-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaur S, Sachdev H, Dwivedi SN, Lakshmi R, Kapil U, Sareen N. Association of obesity with hypertension amongst school-age children belonging to lower income group and middle income group in national capital territory of Delhi. Indian J Community Med. 2013;38:175–9. doi: 10.4103/0970-0218.116355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li YP, Yang XG, Zhai FY, Piao JH, Zhao WH, Zhang J, et al. Disease risks of childhood obesity in China. Biomed Environ Sci. 2005;18:401–10. [PubMed] [Google Scholar]
- 7.Yan WL, Li XS, Wang Q, Huang YD, Zhang WG, Zhai XH, et al. Overweight, high blood pressure and impaired fasting glucose in Uyghur, Han, and Kazakh Chinese children and adolescents. Ethn Health. 2014;20:1–11. doi: 10.1080/13557858.2014.921894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555–76. [PubMed] [Google Scholar]
- 9.Bharathi AV, Kurpad AV, Thomas T, Yusuf S, Saraswathi G, Vaz M. Development of food frequency questionnaires and a nutrient database for the Prospective Urban and Rural Epidemiological (PURE) pilot study in South India: Methodological issues. Asia Pac J Clin Nutr. 2008;17:178–85. [PubMed] [Google Scholar]
- 10.Kumar N, Shekhar C, Kumar P, Kundu AS. Kuppuswamy's socioeconomic status scale-updating for 2007. Indian J Pediatr. 2007;74:1131–2. [PubMed] [Google Scholar]
- 11.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: A systematic review and meta-regression analysis. Circulation. 2008;117:3171–80. doi: 10.1161/CIRCULATIONAHA.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Constantine E, Merritt C. Hypertensive emergencies in children: Identification and management of dangerously high blood pressure. Minerva Pediatr. 2009;61:175–84. [PubMed] [Google Scholar]
- 13.Subramanian H, Soudarssanane MB, Jayalakshmy R, Thiruselvakumar D, Navasakthi D, Sahai A, et al. Non-pharmacological Interventions in Hypertension: A Community-based Cross-over Randomized Controlled Trial. Indian J Community Med. 2011;36:191–6. doi: 10.4103/0970-0218.86519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saptharishi L, Soudarssanane M, Thiruselvakumar D, Navasakthi D, Mathanraj S, Karthigeyan M, et al. Community-based Randomized Controlled Trial of Non-pharmacological Interventions in Prevention and Control of Hypertension among Young Adults. Indian J Community Med. 2009;34:329–34. doi: 10.4103/0970-0218.58393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chadha SL, Tandon R, Shekhawat S, Gopinath N. An epidemiological study of blood pressure in school children (5-14 years) in Delhi. Indian Heart J. 1999;51:178–82. [PubMed] [Google Scholar]
- 16.Mohan B, Kumar N, Aslam N, Rangbulla A, Kumbkarni S, Sood NK, et al. Prevalence of sustained hypertension and obesity in urban and rural school going children in Ludhiana. Indian Heart J. 2004;56:310–4. [PubMed] [Google Scholar]


