Abstract
Objective:
To investigate the anatomic symmetry of maxillary and mandibular posteriors in Indian subpopulation using cone beam computed tomography (CBCT).
Materials and Methods:
CBCT images of 246 patients that had at least one noncarious, posterior tooth free of restorations in each quadrant were enrolled for retrospective analysis. A total of 3015 teeth (811 maxillary premolars, 845 mandibular premolars, 738 maxillary molars, and 621 mandibular molars) were analyzed for number of roots and root canals, canal morphology and anatomic symmetry, and concurrent types between the maxilla and mandible.
Results:
There was no difference in the percentage of symmetry for maxillary first (81.5%) and second (81.5%) premolars. Mandibular second premolars (98.3%) exhibited greater symmetry than mandibular first premolars (96.1%). First molars (77.5% and 82.1%) showed greater symmetry than second molars (70.8% and 78.6%), in both maxillary and mandibular arches, respectively. The most common anatomy observed were: maxillary first premolars – 2 roots with 2 canals, maxillary second premolars – 1 root with 2 canals, mandibular first and second premolars – 1 root with 1 canal, maxillary first and second molars – 3 roots with 4 canals, and mandibular first and second molars – 2 roots with 3 canals. When compared with any other teeth, maximum asymmetry was observed in maxillary second molar (29.2%).
Conclusion:
The percentage of symmetry observed in the present study varied from 70% to 98% with least percentage of symmetry in maxillary second molars. These data should alert the clinicians while treating homonymous teeth of the same patient.
Keywords: Anatomic symmetry, cone beam computed tomography, C-shaped canal, posterior teeth, radix entomolaris, radix paramolaris, root canal morphology
INTRODUCTION
A thorough knowledge of the root and the root canal morphology of all existing canals plays a significant role in determining the success of endodontic treatment.[1] Successful treatment of endodontic complications is associated with diagnostic imaging techniques that provide information about the teeth and their surrounding structures.[2]
Various in vitro methods used have been used for evaluating the root canal morphology.[3] However, in vivo methods such as conventional periapical radiographs[4] and cone beam computed tomography (CBCT) are valuable diagnostic tools for assessing anatomic symmetry of teeth between the right and left sides in the same patient. This can be of high clinical relevance when treating multiple teeth in the same patient.[3]
Recently, CBCT has been introduced to overcome the limitations of conventional radiographs such as distortion and superimposition of bony and dental structures.[5] In addition, CBCT has proven useful in evaluating root canal morphology in the maxillary region[6] and morphologic evaluation in endodontics.[7] The posterior teeth have a more complex morphological variations, such as abnormal number of roots and root canals,[8] existence of C-shaped root canals,[9] radix entomolaris (RE),[10] and radix paramolaris (RP).[11]
The aim of the present study was to analyze the CBCT images of maxillary and mandibular posterior teeth in Indian subpopulation and to determine the bilateral symmetry in root and root canal configuration using CBCT.
MATERIALS AND METHODS
CBCT images of 246 patients, who required CBCT investigation, as part of their dental diagnosis and treatment for reasons including preoperative assessment for multiple implants, endodontic management of teeth with unusual root canal morphology, facial trauma, maxillary sinusitis, and orthodontic treatment because of impacted teeth were obtained from imaging center for inclusion in this retrospective study. The patients were selected with the mean age of 43 years (range, 15–70 years) who had at least one noncarious, posterior tooth free of restorations in each quadrant, since the scattering and beam hardening effects produced by CBCT technology can affect the quality of the image.[12] This study was approved by Institutional Ethics Committee.
CBCT was performed by Kodak 9500 cone beam 3D (Carestream Health Inc., Rochester, NY) equipment with the following technical parameters: Field of view 18 cm × 20 cm, effective exposure time of 10.8 s (pulsated), tube voltage 60–90 kV, 2–15 mA (pulsated mode) with an estimated radiation dosage of 30–80 µSv and slice thickness of 0.2 mm.
CBCT images were analyzed using 3D module version 2.4 Kodak Dental Imaging software (Carestream Health Inc., Rochester, NY) on a 17-inch Samsung light emitting diode screen (Seoul, Korea) with a resolution of 1280 × 1024 pixels. The images obtained were viewed three-dimensionally as well as in the axial, sagittal, and coronal planes. CBCT images in all the three planes were observed for three times to get a detailed view of the root canal system of the examined teeth. CBCT images were evaluated at the same time by a professional endodontist and oral radiologist, to obtain similar findings. In cases of complex root canal anatomy, where consensus could not be obtained after mutual consultation, a third evaluator (endodontist) was asked to confirm the root canal morphology and internal anatomy.
All the posterior teeth were examined according to the Vertucci's classification for number of roots and their morphology, the number of root canals in each root, configuration of the root canal system, and bilateral symmetry.[13] Interarch and intra-arch comparison was performed for the bilateral symmetry of posterior teeth using Chi-square test using SPSS software version 16.0 (SPSS Inc. Chicago, IL) at a 0.05 significance level.
RESULTS
External anatomy of roots and number of root canals
In the 418 maxillary first premolars examined, 214 (51.2%) had 2 roots with individual canals and 204 (48.8%) had 1 root. 84.1% (n = 172) of the single rooted maxillary first premolar had 2 canals, and the remaining 15.9% (n = 32) had 1 canal. In the 393 maxillary second premolars examined, 37 (9.4%) had 2 roots with individual canals and 356 (90.6%) had 1 root. 44.9% (n = 160) of the single rooted maxillary second premolar had 2 canals, and the remaining 55.1% (n = 196) had 1 canal.
In the 447 mandibular first premolars examined, 9 (2.0%) had 2 roots with individual canals and 438 (98.0%) had 1 root. 5.4% (n = 24) of the single-rooted mandibular first premolar had 2 canals and the remaining 94.6% (n = 414) had 1 canal. In the 398 mandibular second premolars examined, 397 (99.7%) were found to have single root with single canal and remaining 1 (0.3%) had two canals.
In the 367 maxillary first molars [Figure 1] examined, 2 (0.5%) had 4 separate roots (mesiobuccal [MB], distobuccal [DB], mesiopalatal [MP], and distopalatal [DP]) with individual canals, 355 (96.8%) teeth had 3 separate roots; whereas 263 (74.1%) of the MB roots had second canal (MB2) and the other 92 (25.9%) MB roots had 1 canal. Of the 3 rooted teeth with MB2 (n = 263), 1 (0.4%) had 2 canals in palatal (P) root. The remaining 10 (2.7%) teeth had 2 roots; 1 (10%) had 5 canals (3 in buccal (B) and 2 in P), 2 (20%) had 4 canals, 6 (60%) had 3 canals, and 1 (10%) had 2 canals (C-shaped in the B root).
Figure 1.
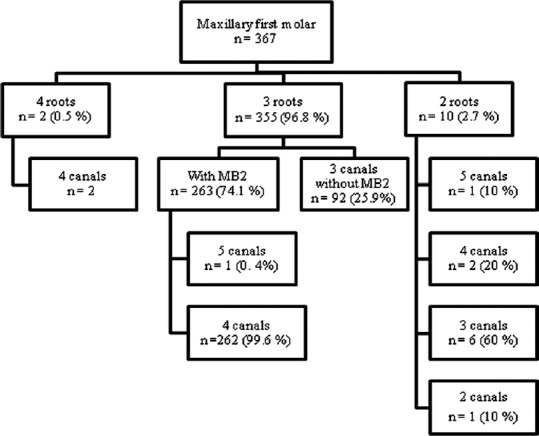
Distribution of roots and root canals observed in maxillary first molars
In the 371 maxillary second molars [Figure 2] examined, 4 (1.1%) had 4 separate roots (MB, DB, MP, and DP); 1 (25%) had MB2 and 3 (75%) had individual canals in the MB root. Two hundred and ninety-eight (80.3%) teeth had 3 separate roots; whereas 179 (60.1%) of the MB roots had 2 canals (MB1 and MB2) and other 119 (39.9%) MB roots had 1 canal. Of the 3 rooted teeth with MB2 (n = 179), 1 (0.6%) had 2 canals in P root. 33 (8.9%) teeth had 2 roots; 5 (15.2%) had 4 canals (1 had 3 in B and 1 in P, 4 had 2 in B and 2 in P), 19 (57.6%) had 3 canals (2 B and 1 in P), 9 (27.3%) had 2 canals. The remaining 36 (9.7%) teeth had 1 root; 1 (2.7%) had 4 canals, 6 (16.7%) had 3 canals, 18 (50%) had 2 canals, 9 (25%) had single canal, and 2 (5.6%) had C-shaped canal configuration. The overall frequency of C-shaped canal in maxillary second molar was 0.5%.
Figure 2.
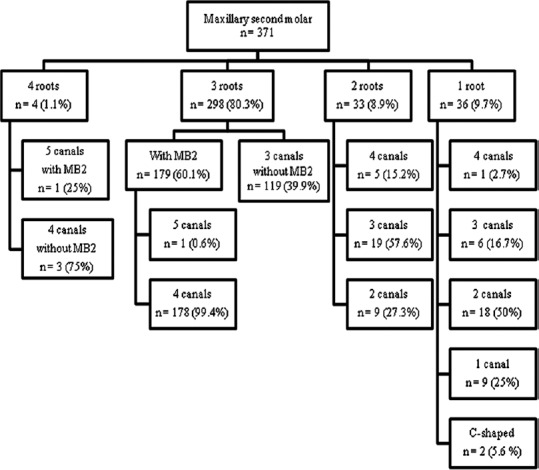
Distribution of roots and root canals observed in maxillary second molars
In the 299 mandibular first molars [Figure 3] examined, 17 (5.7%) had 3 separate roots, 280 (93.6%) had 2 roots, and 2 (0.7%) had 1 root. When 3 separate roots were present 15 (88.2%) teeth had RE; 1 (6.7%) had 5 canals (2 mesial [M], 1 DB and 2 distolingual [DL]) and 14 (93.3%) had 4 canals (2 M, 1 DB, and 1 DL). The remaining 2 (11.8%) out of 17 teeth had RP with 3 individual canals. When 2 roots were present, 6 (2.1%) had 5 canals (3 in M and 2 in distal [D]), 73 (26.1%) had 4 canals; 5 (6.8%) had 3 canals in the M root (MB, middle mesial [MM], and mesiolingual) and 1 canal in the D root, 68 (93.2%) had 2 canals in each root, 198 (70.7%) teeth had 3 canals (2 in the M root and 1 in the D root), and 3 (1.1%) teeth had 2 canals. The remaining 2 (0.7%) teeth had 1 root with C-shaped canal configuration. In the 297 teeth with more than 1 root, 11 (3.7%) had MM canal. The overall frequency of RE, RP, and C-shaped canal in mandibular first molar was 5%, 0.7%, and 0.7%, respectively.
Figure 3.
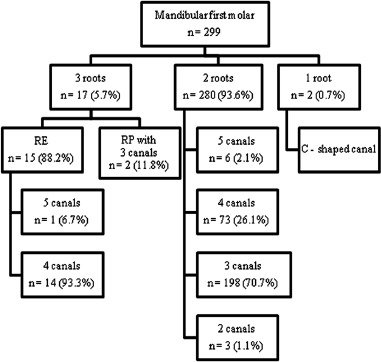
Distribution of roots and root canals observed in mandibular first molars
In the 322 mandibular second molars [Figure 4] examined, 8 (2.5%) had 3 separate roots, 286 (88.8%) had 2 roots, and the remaining 28 (8.7%) had 1 root. When 3 separate roots were present, 3 (37.5%) had RE, and the remaining 5 (62.5%) had RP with 3 individual canals. When 2 roots were present, 1 (0.3%) had 5 canals (3 in M and 2 in D), 14 (4.9%) had 4 canals; 5 (35.7%) had 3 canals in the M root and 1 canal in the D root, 9 (64.3%) had 2 canals in each root, 251 (87.8%) had 3 canals (2 in the M root and 1 in the D root), 20 (7%) had 2 canals. When 1 root were present, 1 (3.6%) had 3 canals, 1 (3.6%) had 2 canals, and the remaining 26 (92.8%) had C-shaped canal configuration. In the 294 teeth with more than 1 root, 3 (1%) had MM canal. The overall frequency of RE, RP, and C-shaped canal in mandibular second molar was 0.9%, 1.5%, and 8.1%, respectively.
Figure 4.
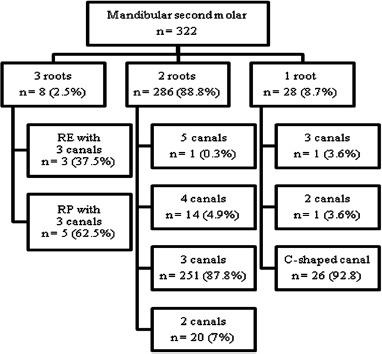
Distribution of roots and root canals observed in mandibular second molars
Internal anatomy of root canals
In the maxillary first premolars examined, when 1 root was present, the root canal configuration was type I (15.9%), type II (26.1%), and type IV (58%). In the maxillary second premolar, when 1 root was present, the root canal configuration was type I (55.1%), type II (25.2%), type III (1.9%), type IV (15%), type V (1.9%), and type VI (0.9%). In the mandibular first premolar, when 1 root was present, the root canal configuration was type I (94%), type II (1.3%), type IV (2.7%), type V (1.3%), and C-shaped (0.7%). In the mandibular second premolar, when 1 root was present, the root canal configuration was type I (98.4%), type V (0.8%), and C-shaped (0.8%).
In the maxillary first molar, when MB2 was present the canal configuration of the M root was type II (60%), type III (1%), and type IV (39%). One of these teeth exhibiting MB2 had type IV configuration in the Proot. When 2 roots with 5 canals were present, the canal configuration of B root was type VIII and P root was type IV, whereas when 2 roots with 4 canals were present, the canal configuration was 50% type VIII in the B root and 50% type IV in both B and P roots. When 2 roots with 3 canals were present, all the teeth had type IV canal configuration in the P root. When 2 roots with 2 canals were present, the canal configuration of the B root was C-shaped.
In the maxillary second molar, when MB2 was present the canal configuration of the M root was type II (67.3%), type IV (31.1%), and type V (1.6%). Two of these teeth showing MB2 had type IV canal configuration (3 roots with 5 canals) in the P root. When 2 roots with 4 canals were present, the canal configuration was 20% type VIII in the B root and 80% type IV in both the B and the P roots. When 2 roots with 3 canals were present the canal configuration of the B root was type IV. In single rooted teeth 16.7% had type VIII, 50% had type IV, 25% had type I, 5.6% had C-shaped canal configuration, and the remaining 2.7% had 4 separate canals that extend from the pulp chamber to the apex with distinct apical foramen (1 root with 4 canals).
In the mandibular first molar, when 3 roots with 5 canals were present, type IV canal configuration was seen in the M and DL roots. When 3 roots with 4 canals were present, the canal configuration of the M root was type IV. When 2 roots with 5 canals were present, the canal configuration of the M root was type VIII, and the D root was type II. When 2 roots with 4 canals were present 6.8% of the teeth had type VIII in M root and type I in the D root, whereas 93.2% had type IV canal configuration in both M and D roots. When 2 roots with 3 canals were present, the canal configuration in the M root was 28.6% type II, and 71.4% type IV. When 1 root was present, the canal configuration was C-shaped.
In the mandibular second molar, when 2 roots with 5 canals were present, the canal configuration of the M root was type VIII, and the D root was type II. When 2 roots with 4 canals were present, 35.7% of the teeth had type VIII in the M root and type I in the D root, whereas 64.3% of the teeth had type IV in the M root and type II in the D root. When 2 roots with 3 canals were present, the canal configuration was 43.6% type II in the M root, and 56.4% type IV in the D root. When 1 root was present 3.6% had type VIII, 3.6% had type II, and 92.8% had C-shaped canal configuration.
Bilateral symmetry of posteriors
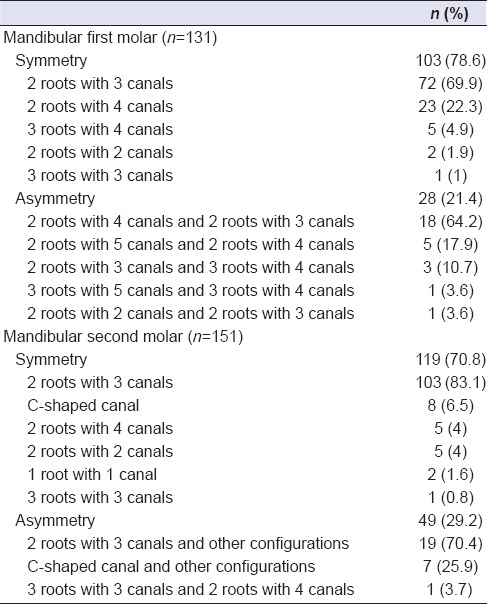
The analysis of bilateral symmetry for eligible patients with respect to number of roots and root canals was performed in the axial section of CBCT images. Of the 195 and 184 patients who had both of the maxillary first and second premolars, 81.5% (n = 159) and 81.5% (n = 150) showed anatomic symmetry, respectively [Table 1]. With respect to mandibular first and second premolars, 96.1% (n = 197) of 205 patients and 98.3% (n = 173) of 176 patients showed anatomic symmetry, respectively [Table 2]. Of the 160 and 168 patients who had both of the maxillary first and the second molars, 77.5% (n = 124) and 70.8% (n = 119) showed anatomic symmetry, respectively [Table 3]. With regards to mandibular first and second molars, the symmetry was observed in 78.6% (n = 103) of 131 patients and 82.1% (n = 124) of 151 patients, respectively [Table 4]. The difference in bilateral symmetry between maxillary and mandibular posterior teeth was statistically significant (P < 0.001; Chi-square test). However, the difference was not significant within the arch between the first and second of premolars and molars (P > 0.05; Chi-square test).
Table 1.
Bilateral comparison of the number of roots and root canals in maxillary first and second premolars
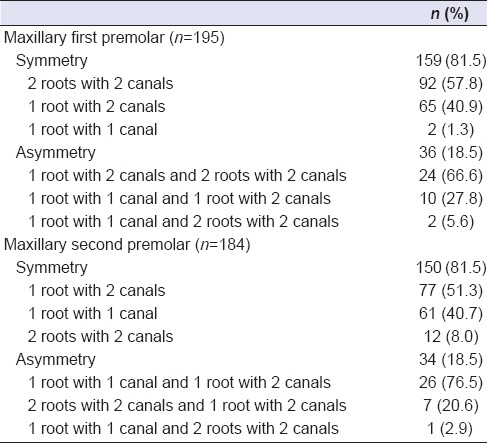
Table 2.
Bilateral comparison of the number of roots and root canals in mandibular first and second premolars
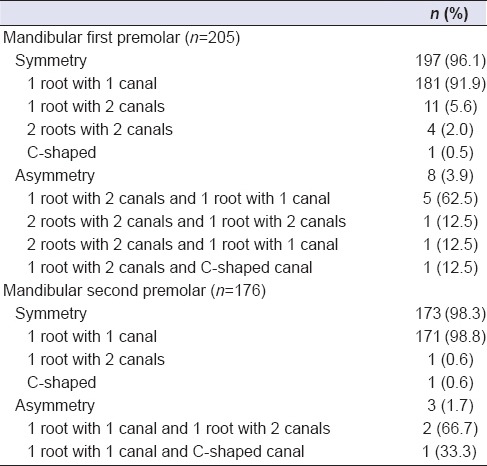
Table 3.
Bilateral comparison of the number of roots and root canals in maxillary first and second molars
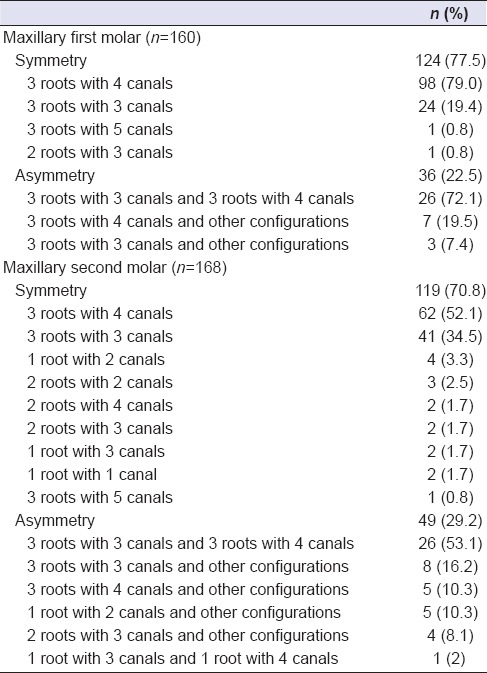
Table 4.
Bilateral comparison of the number of roots and root canals in mandibular first and second molars
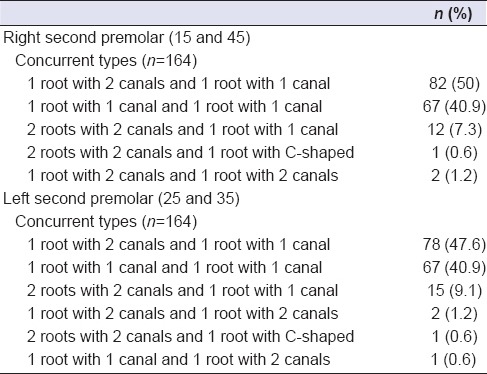
Concurrent configuration of premolars
The number of roots and root canals in first premolars [Table 5] and second premolars [Table 6] between the maxillary and mandibular arch were analyzed for the presence of concurrent combinations on both right and left side. Of the 181 and 196 patients, who had both of the right and left first premolars, respectively, 43% (n = 77) and 41.3% (n = 81) showed 2 roots with 2 canals and 1 root with 1 canal. Of the 164 patients who had both of the right and left second premolars, 50% (n = 82) and 47.6% (n = 78) showed 1 root with 2 canal and 1 root with 1 canal, respectively.
Table 5.
Concurrent types of roots and root canals in first premolars between maxillary and mandibular arches
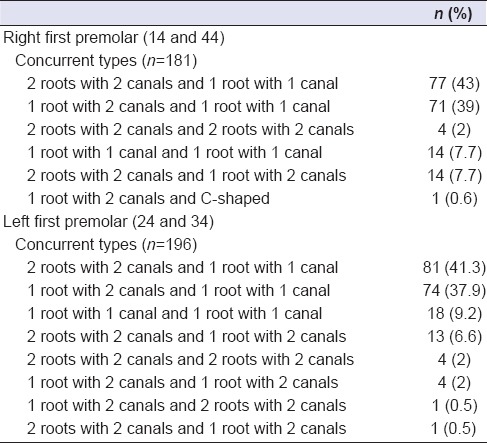
Table 6.
Concurrent types of roots and root canals in second premolars between maxillary and mandibular arches
DISCUSSION
CBCT has a good diagnostic accuracy in level with the digital operating microscope.[14] Moreover, for the patients who require three dimensional investigations, CBCT with low radiation dose is preferred over traditional CT examination.[15]
According to Pecora et al.,[16] an incidence of 2.5% has been reported for maxillary first premolar with more than two canals in a Brazilian population. However, no such canal configuration was observed in our study. Although, aberration in root canal configuration of mandibular premolars like C-shaped canal[17] and 4 roots with 4 canals[18] have been previously reported in the literature, the most commonly observed root canal morphology was type I.[19] A systematic review on permanent mandibular premolars for different ethnicities revealed poor corelation between the Indian population and the C-shaped canals.[20] Accordingly, the results of our study showed type I canal configuration with the highest incidence rate of 94% in the mandibular I premolar, 98.4% in the mandibular II premolar, and the least incidence rate for C-shaped canal configuration (0.7–0.8%).
Various studies on maxillary molars revealed the incidence of MB2 ranging from 52% to 78% in the first molar and 15.1–58% in the second molar.[3,21,22] In our present study, the frequency rate of MB2 was 74.1% in the first molar and 60.1% in the second molar. Moreover, one of the single rooted maxillary second molar had 4 canals. These unusual findings clearly demonstrate the effectiveness of CBCT.
Various literatures have highlighted the presence of MM canals[23,24] and middle distal canals[25] in the mandibular molars in different population. The MM canal was present in both mandibular first molars (3.7%) and second molars (0.9%) whereas none of the examined teeth had a middle distal canal.
The frequency of RE in mandibular first molars ranges from 3% to 40% in different populations (Indian 0.2%).[10] However, it is least common in the mandibular second molars.[11] In contradiction, the frequency of RP was relatively more in mandibular second molars than that of mandibular first molars.[11] Similarly, the frequency of RE was more in the mandibular first molars (5%) than that of mandibular second molars (0.9%), whereas the frequency of RP is more in the mandibular second molars (1.5%) than that of the mandibular first molars (0.7%) in our study. In mandibular first molars, one of the teeth with RE had 2 canals in the DL root which has not been reported in the literature.
Significant ethnic variations have been seen in the frequency of C-shaped root canal system in mandibular molars among the Japanese,[26] Chinese,[6] and Burmese population.[9] As far as Indian population is concerned, C-shaped canals are most commonly associated with mandibular second molars.[24,27] Accordingly, the results of our study showed a maximum incidence for C-shaped (8.1%) canals in mandibular second molars and an unusual incidence of C-shaped canal configuration in the maxillary second molars (0.5%). In addition, one tooth had similar configuration in the buccal root, which is a rare presentation.
When bilateral comparison was performed between the arches and mandibular posteriors (97.1% in premolars and 80.5% in molars) exhibited greater symmetry (P < 0.001) than the maxillary posteriors (81.5% in premolars and 74.1% in molars). However, no remarkable variation was observed in the first and the second premolars for both arches. When molars were compared within the arches, the maxillary first molars (77.5%) exhibited greater symmetry than that of the second molars (70.8%), whereas the mandibular second molars (82.1%) showed greater symmetry (P > 0.05) than that of the first molars (78.6%). The percentage of symmetry for maxillary molars in White and Chinese population was found to be 75.8% and 84%, respectively.[3,6] However, a lesser percentage of symmetry (74.1%) was observed in our population. In contrast, this ethnic variation was reversed for maxillary first premolars with a greater percentage of symmetry (81.5%) in our population than that of the Chinese population (64%).[27]
Bilateral symmetry was frequently encountered in maxillary first and second premolars when 2 roots with 2 canals (57.8%) and 1 root with 2 canals (51.3%) were present, respectively. The most common type of symmetry in mandibular first and second premolars was 1 root with 1 canal (91.9% and 98.8%, respectively). High frequency of symmetry was observed in 3 roots with 4 canals in both first (79%) and second (52.1%) maxillary molars. Similarly, 2 roots with 3 canals showed the maximum percentage (83.1% and 69.9%) of symmetry in mandibular first and second molars, respectively which is very commonly seen in Indian population.[24]
In comparison with any other teeth, maximum percentage of asymmetry was observed in maxillary second molar (29.2%). When 3 roots with 3 canals were present on one side and 3 roots with 4 canals were present on the other side, higher frequency of asymmetry was observed in maxillary first molars (72.1%) and second molars (53.2%). This type of asymmetry could be attributed to the variation in the complex anatomy of the MB root.[3] In mandibular first molars, maximum asymmetry (64.2%) was seen in 2 roots with 3 canals and 2 roots with 4 canals. Maximum concurrent anatomy was found to be 2 roots with 2 canals, and 1 root with 2 canals in first and second maxillary premolars, respectively when the patients had 1 root with 1 canal in the mandibular premolars. These data are of great clinical importance in locating, negotiating, and managing the entire root canal system while treating multiple teeth in the same patient.
CONCLUSION
The overall average percentage of symmetry observed in our study was 83.9% ranging from 70% to 98% depending upon the tooth considered. In almost 30% of the CBCT images analyzed, the root canal configurations of the homonymous teeth are not alike especially for the maxillary second molar which is a technical challenge for the clinician.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cleghorn BM, Christie WH, Dong CC. The root and root canal morphology of the human mandibular first premolar: A literature review. J Endod. 2007;33:509–16. doi: 10.1016/j.joen.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Liang YH, Yuan M, Li G, Shemesh H, Wesselink PR, Wu MK. The ability of cone-beam computed tomography to detect simulated buccal and lingual recesses in root canals. Int Endod J. 2012;45:724–9. doi: 10.1111/j.1365-2591.2012.02025.x. [DOI] [PubMed] [Google Scholar]
- 3.Plotino G, Tocci L, Grande NM, Testarelli L, Messineo D, Ciotti M, et al. Symmetry of root and root canal morphology of maxillary and mandibular molars in a white population: A cone-beam computed tomography study in vivo. J Endod. 2013;39:1545–8. doi: 10.1016/j.joen.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 4.Yew SC, Chan K. A retrospective study of endodontically treated mandibular first molars in a Chinese population. J Endod. 1993;19:471–3. doi: 10.1016/S0099-2399(06)80536-4. [DOI] [PubMed] [Google Scholar]
- 5.Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG. Endodontic applications of cone-beam volumetric tomography. J Endod. 2007;33:1121–32. doi: 10.1016/j.joen.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 6.Zhang R, Yang H, Yu X, Wang H, Hu T, Dummer PM. Use of CBCT to identify the morphology of maxillary permanent molar teeth in a Chinese subpopulation. Int Endod J. 2011;44:162–9. doi: 10.1111/j.1365-2591.2010.01826.x. [DOI] [PubMed] [Google Scholar]
- 7.Matherne RP, Angelopoulos C, Kulild JC, Tira D. Use of cone-beam computed tomography to identify root canal systems in vitro. J Endod. 2008;34:87–9. doi: 10.1016/j.joen.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 8.Alaçam T, Tinaz AC, Genç O, Kayaoglu G. Second mesiobuccal canal detection in maxillary first molars using microscopy and ultrasonics. Aust Endod J. 2008;34:106–9. doi: 10.1111/j.1747-4477.2007.00090.x. [DOI] [PubMed] [Google Scholar]
- 9.Gulabivala K, Aung TH, Alavi A, Ng YL. Root and canal morphology of Burmese mandibular molars. Int Endod J. 2001;34:359–70. doi: 10.1046/j.1365-2591.2001.00399.x. [DOI] [PubMed] [Google Scholar]
- 10.De Moor RJ, Deroose CA, Calberson FL. The radix entomolaris in mandibular first molars: An endodontic challenge. Int Endod J. 2004;37:789–99. doi: 10.1111/j.1365-2591.2004.00870.x. [DOI] [PubMed] [Google Scholar]
- 11.Calberson FL, De Moor RJ, Deroose CA. The radix entomolaris and paramolaris: Clinical approach in endodontics. J Endod. 2007;33:58–63. doi: 10.1016/j.joen.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 12.Patel S. New dimensions in endodontic imaging: Part 2. Cone beam computed tomography. Int Endod J. 2009;42:463–75. doi: 10.1111/j.1365-2591.2008.01531.x. [DOI] [PubMed] [Google Scholar]
- 13.Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58:589–99. doi: 10.1016/0030-4220(84)90085-9. [DOI] [PubMed] [Google Scholar]
- 14.de Toubes KM, Côrtes MI, Valadares MA, Fonseca LC, Nunes E, Silveira FF. Comparative analysis of accessory mesial canal identification in mandibular first molars by using four different diagnostic methods. J Endod. 2012;38:436–41. doi: 10.1016/j.joen.2011.12.035. [DOI] [PubMed] [Google Scholar]
- 15.Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006;72:75–80. [PubMed] [Google Scholar]
- 16.Pécora JD, Saquy PC, Sousa Neto MD, Woelfel JB. Root form and canal anatomy of maxillary first premolars. Braz Dent J. 1992;2:87–94. [PubMed] [Google Scholar]
- 17.Velmurugan N, Sandhya R. Root canal morphology of mandibular first premolars in an Indian population: A laboratory study. Int Endod J. 2009;42:54–8. doi: 10.1111/j.1365-2591.2008.01494.x. [DOI] [PubMed] [Google Scholar]
- 18.Sachdeva GS, Ballal S, Gopikrishna V, Kandaswamy D. Endodontic management of a mandibular second premolar with four roots and four root canals with the aid of spiral computed tomography: A case report. J Endod. 2008;34:104–7. doi: 10.1016/j.joen.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Awawdeh LA, Al-Qudah AA. Root form and canal morphology of mandibular premolars in a Jordanian population. Int Endod J. 2008;41:240–8. doi: 10.1111/j.1365-2591.2007.01348.x. [DOI] [PubMed] [Google Scholar]
- 20.Kottoor J, Albuquerque D, Velmurugan N, Kuruvilla J. Root anatomy and root canal configuration of human permanent mandibular premolars: A systematic review. Anat Res Int 2013. 2013:254250. doi: 10.1155/2013/254250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.al Shalabi RM, Omer OE, Glennon J, Jennings M, Claffey NM. Root canal anatomy of maxillary first and second permanent molars. Int Endod J. 2000;33:405–14. doi: 10.1046/j.1365-2591.2000.00221.x. [DOI] [PubMed] [Google Scholar]
- 22.Yoshioka T, Kikuchi I, Fukumoto Y, Kobayashi C, Suda H. Detection of the second mesiobuccal canal in mesiobuccal roots of maxillary molar teeth ex vivo. Int Endod J. 2005;38:124–8. doi: 10.1111/j.1365-2591.2004.00918.x. [DOI] [PubMed] [Google Scholar]
- 23.Holtzmann L. Root canal treatment of a mandibular first molar with three mesial root canals. Int Endod J. 1997;30:422–3. doi: 10.1046/j.1365-2591.1997.00106.x. [DOI] [PubMed] [Google Scholar]
- 24.Neelakantan P, Subbarao C, Subbarao CV, Ravindranath M. Root and canal morphology of mandibular second molars in an Indian population. J Endod. 2010;36:1319–22. doi: 10.1016/j.joen.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Cantatore G, Berutti E, Castelluci A. Missed anatomy: Frequency and clinical impact. Endod Topics. 2006;15:3–31. [Google Scholar]
- 26.Cleghorn BM, Goodacre CJ, Christie WH. Morphology of teeth and their root canal system. In: Ingle JI, Backland LK, Baumgartner JC, editors. Endodontics. 6th ed. Hamilton, ON: BC Decker Inc; 2008. pp. 151–210. [Google Scholar]
- 27.Tian YY, Guo B, Zhang R, Yu X, Wang H, Hu T, et al. Root and canal morphology of maxillary first premolars in a Chinese subpopulation evaluated using cone-beam computed tomography. Int Endod J. 2012;45:996–1003. doi: 10.1111/j.1365-2591.2012.02059.x. [DOI] [PubMed] [Google Scholar]


