Abstract
Patient: Male, 83
Final Diagnosis: Remitting seronegative symmetrical synovitis with pitting edema
Symptoms: Morning stiffness • pitting edema of the hands • shoulder and hip pain
Medication: —
Clinical Procedure: 18FDG PET/CT
Specialty: Rheumatology
Objective:
Rare disease
Background:
Remitting seronegative symmetrical synovitis with pitting edema (RS3PE) is a rare condition that occurs in elderly individuals. It can present alone or in association with various rheumatic or malignant diseases.
Case Report:
An 83-year-old man presented with anemia, hyper-sedimentation, and pitting edema of the back of the hands. The patient complained of pain and stiffness of the shoulder and hip girdles, especially in the morning. He was previously diagnosed with adenocarcinoma of the prostate. After 3 years of watchful waiting, treatment with goserelin, a gonadotropin releasing hormone agonist, was started, when PSA had increased to 67.9 µg/l. About 1 year before the cancer treatment, the patient also presented with sore and swollen hands, compatible with RS3PE, which remitted after a few months of prostatic cancer treatment. Thorough laboratory evaluation was performed upon admission to the Rheumatology Department and he was referred for FDG PET/CT on suspicion of metastases of the previously diagnosed prostatic cancer. PET/CT imaging revealed increased FDG up-take in the soft tissues around the shoulders and hips, but no evidence of bone metastasis or other malignant findings. A diagnosis of polymyalgia rheumatica (PMR) together with RS3PE syndrome was made and treatment with prednisolone 15 mg/d was started, which resulted in rapid resolution of the symptoms.
Conclusions:
Presence of RS3PE in relation with PMR and prostatic cancer in our patient suggests a common trigger factor. To the best of our knowledge, this is the first report of a case of RS3PE that presented twice with 2 different diagnoses in the same patient.
MeSH Keywords: Paraneoplastic Syndromes, Polymyalgia Rheumatica, Prostatic Neoplasms, Rheumatology
Background
Remitting seronegative symmetrical synovitis with pitting edema (RS3PE) is a rare condition that has been reported as a paraneoplastic syndrome [1], frequently together with prostate, stomach, and colon cancers [2]. It occurs in elderly individuals and is characterized by symmetrical distal synovitis, pitting edema of the dorsum of the hands, and seronegativity of rheumatoid factor. It responds well to low-dose steroids and remains in remission for a long time unless associated with malignancy [2,3].
Polymyalgia rheumatica (PMR) is characterized by inflammatory pain and stiffness of the shoulder and pelvic girdles, with biochemical evidence of inflammation. It occurs most frequently in patients over 50 years of age [4]. However, clinical diagnosis of PMR is rather difficult due to the large differential diagnosis that can mimic PMR [5]. Although malignant diseases can present with PMR-like syndrome, physicians should be aware of co-occurrence of both conditions at the same time. Here, we report the case of an 83-year-old man who presented twice with RS3PE; first as a paraneoplastic syndrome with adenocarcinoma of prostate and then with concurrent PMR.
Case Report
An 83-year-old man was referred to the Rheumatology Department due to anemia, hyper-sedimentation, and pitting edema of the back of the hands. The patient complained of pain and stiffness of the shoulder and hip girdles, especially in the morning. On physical examination the patient had normal range of motion of the shoulder, but range of motion of the hip was limited. There were signs of arthritis in the left knee. He had no symptoms or signs of headache, visual problems, jaw claudication, scalp tenderness, or any other cranial symptoms. The patient had been diagnosed with adenocarcinoma of the prostate 4 years before the presentation of these symptoms. Prostate-specific antigen (PSA) and Gleason score were 16 µg/l and 5 (2+3), respectively, at that point of time. He was under watchful waiting for 3 years until the PSA increased to 67.9 µg/l. This triggered initiation of hormonal ablation. Therefore, treatment with injection of goserelin 10.8 mg every 3 months, together with bicalutamide 150 mg/day in the first 2 weeks, was started. After 9 months, treatment was changed to leuprorelin every 6 months and the PSA level decreased to less than 0.1 µg/l within 3 months after treatment. One year before the initiation of treatment with goserelin, the patient also had sore and swollen hands, compatible with RS3PE. This phenomenon disappeared when PSA level fell to 0.3 µg/l.
Results of laboratory evaluations are summarized in Table 1. The patient was anemic and the levels of erythrocyte sedimentation rate and C-reactive protein had increased. Bone marrow aspiration was done to rule out hematological malignancy or bone metastasis; results were normal and demonstrated normal surface antigen with normal karyotype. The result of peripheral blood smear showed hypochromic erythrocytes with a slight increase in nucleated blood cells without immature or plasma cells. The patient was referred for FDG PET/CT scan due to suspicion of metastases. FDG PET/CT is a routine examination in cases of suspected occult cancer or suspected metastases from known cancer, as well as to identify causes of rheumatologic diseases [6]. The results of FDG PET/CT imaging visualized a strong FDG uptake in the soft tissues around the shoulders and hips, consistent with PMR (Figure 1). There was no evidence of bone metastases and no other findings suspicious for malignancies. Therefore, the patient was referred to the Rheumatology Department due to suspicion of an underlying rheumatologic condition. Ultrasound-guided puncture of the left knee was done to determine the cause of swelling in the affected joint, and the result showed a small increase in leucocytes (860×10E6/l, normal range <200×10E6/l)) with no evidence of crystal deposition, which was compatible with arthrosis. Temporal artery biopsy was performed to diagnose a possible inflammation and the result was negative. Treatment with prednisolone 15 mg/d was started with a tapering schedule of reducing 2.5 mg every 2 weeks. Ca-vitamin D supplementation and alendronate 70 mg every week were additionally prescribed to reduce the risk of osteoporosis. The patient became asymptomatic after a short period of time and all subsequent biochemistry test results were normal. Decreasing the prednisolone dosage to 5 mg/d resulted in recurrence of symptoms and slight increase in CRP value. As a result, prednisolone dosage was increased to 12.5 mg/d again, whereupon symptoms disappeared, and that was successfully tapered afterward. The prednisolone medication was ceased after 18 months, without any related adverse effects. After 4-year follow-up in the Rheumatology Department and 8 years after cancer diagnosis, the patients is still alive and has no symptoms or signs of PMR or RS3PE, without having any evidence of cancer recurrence, and PSA level has remained undetectable (PSA <0.1 µg/l). He also has no complaints of pain in the left knee and recently started to exercise at a gym.
Table 1.
Results of laboratory tests at admission to the department of rheumatology, approximately one year after initiation of prostatic cancer treatment.
| Laboratory test | Reference value | Patient’s value |
|---|---|---|
| Hemoglobin | 8–11 mmol/l | 5.7 mmol/l |
| Mean cell volume | 80–100 fl | 86 fl |
| Reticulocytes | 35–100×10E9/l | 51×10E9/l |
| Iron | 9–35 µmol/l | 3.7 µmol/l |
| Transferrin | 24.4–41.0 µmol/l | 25.7 µmol/l |
| Ferritin | 15–300 µg/l | 404 µg/l |
| Haptoglobin | 0.47–2.05 g/l | 3.39 g/l |
| Folate | 5–30 nmol/l | 8.6 nmol/l |
| Cobalamin | 140–650 pmol/l | 220 pmol/l |
| Urate | 0.20–0.45 mmol/l | 0.26 mmol/l |
| Erythrocyte sedimentation rate | <20 mm/hr | 106 mm/hr |
| C-reactive protein | <10 mg/l | 100 mg/l |
| PSA (prostate-specific antigen) | 0.1 µg/l | <5.00 µg/l |
| IgM rheumatoid factor | <15 IU/mL | Negative |
| Anti ccp (anti-cyclic citrullinated peptide antibody) | <20.0 U | Negative |
| ANA (antinuclear antibody) | £1.0 U | Negative |
| Jo-1 antibody | <1.0 U | Negative |
Figure 1.
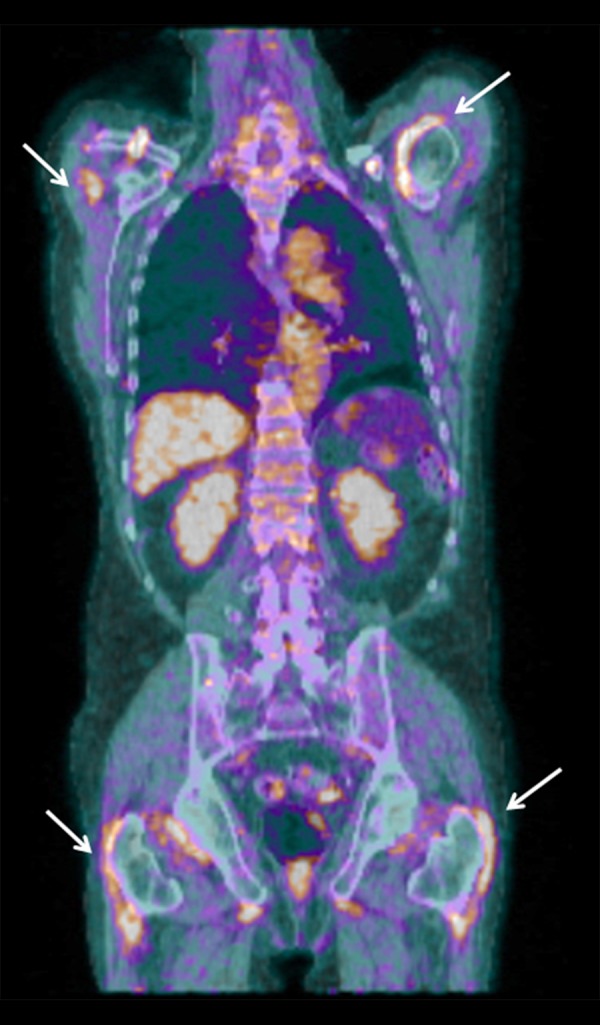
Fused coronal FDG-PET/CT scan of the patient suspected of having malignancy and RS3PE syndrome. Diffusely increased FDG uptake in soft tissue around the shoulder and hip girdles (white arrows) and FDG-positive axillary lymph nodes (not shown) were suggestive of polymyalgia rheumatica. Physiologic FDG uptake can be seen in the liver and the urinary tract, but there were no other pathologic findings (i.e., no evidence of bone metastases and no lesions suspicious of malignancy). The scan was performed according to the Department of Nuclear Medicine’s standard procedure, which follows guidelines from the European Association of Nuclear Medicine. CT was performed as a low-dose scan without contrast enhancement.
Discussion
RS3PE is a rare condition in the elderly and can appear as a first presentation of various types of rheumatic and malignant diseases. It is first described by McCarthy et al. [7] in 1985. The etiology of the RS3PE syndrome is unknown, but environmental factors and infection may affect the course of the disease. It can present alone or in association with rheumatic diseases (e.g., PMR and late-onset rheumatoid arthritis) and malignancies [8,9]. Diagnosis is based on clinical features. Absence of erosive or degenerative changes plus dramatic response to low-dose corticosteroid treatment is characteristic of the disease [10].
PMR is the most common rheumatic disease in older individuals. It is difficult to diagnose PMR due to the wide variation in clinical picture. In addition, there are no specific tests available for PMR. Presenting symptoms, including proximal pain and stiffness, a commonly accepted characteristic of PMR, are not indicative of PMR and can occur in other rheumatologic diseases. However, distal manifestations, such as peripheral arthritis and carpal tunnel syndrome, present in half of PMR cases [11].
Treatment with glucocorticoids is a mainstay and it results in rapid resolution of symptoms [11,12]. The British Society for Rheumatology and British Health Professionals in Rheumatology recommend use of prednisolone 15 mg/d when the diagnosis is established. Subsequently, the dosage should be gradually tapered over time. All patients diagnosed with PMR should commence calcium and vitamin D supplementation to reduce risk of osteoporosis [12].
Several previous studies reported a PMR-like syndrome as a presenting manifestation of various malignant diseases (e.g., prostate cancer [5,13,14], renal cell carcinoma [15], and lymphoma [16]). Other malignancies mimicking PMR include cancers of the gastrointestinal system, lungs, pancreas, uterus, and ovaries [5]. However, PMR patients have an increased risk of malignancies. A recent cohort study by Muller et al. [4] showed a 69% increased risk of malignancies in PMR patients within the first 6 months after a PMR diagnosis. When our patient was referred with suspected PMR, it was obvious to suspect a condition like metastatic prostate cancer mimicking PMR, but this was not shown by the FDG PET/CT scan. The subsequent diagnosis of PMR concurrent with RS3PE was seen as an independent phenomenon. Since PMR and RS3PE presented and disappeared almost at the same time, it can be assumed that there is an association between them.
RS3PE may present before, concurrent with, or after the diagnosis of malignant disease. In our case the RS3PE syndrome presented approximately 1 year before prostate cancer was estimated to need treatment, and the syndrome disappeared again after about 6 months of cancer treatment, which suggests a correlation between these 2 conditions. Considering the long disease history of prostate cancer, it might reasonably be assumed that the patient had been suffering from prostatic cancer for a very long time before the diagnosis. If the prostatic cancer was the triggering factor for RS3PE (in this case, when tumor burden was large enough), one could speculate that there are potential immunological mechanisms triggering RS3PE.
Conclusions
This report illustrates a rare case of RS3PE that occurred together with PMR and prostate cancer. Presence of RS3PE first, simultaneously with prostatic cancer, as a paraneoplastic syndrome, and thereafter concurrent with clinical presentation of PMR, suggests a common trigger factor for RS3PE from a prostatic cancer and PMR. It has previously been reported that there is an association between prostatic cancer and PMR as well as RS3PE. On the other hand, RS3PE was found to be correlated with prostatic cancer and PMR [10,13,17]. However, in the presented case prostatic cancer and PMR were seen together with RS3PE, although not at the same time. In line with earlier studies, our case report suggests that PMR and RS3PE belong to the same clinical entity. To the best of our knowledge, this is the first case report of RS3PE presenting twice in 2 different diagnoses in the same patient.
Acknowledgments
We thank senior physicians Erik Øster-Jørgensen and Lars Kjær Nielsen for their idea report this medical history.
Footnotes
Conflicts of interest
The authors declare that they have no conflicts of interest.
References:
- 1.Tunc SE, Arslan C, Ayvacioglu NB, et al. Paraneoplastic remitting seronegative symmetrical synovitis with pitting edema (RS3PE syndrome): a report of two cases and review of the literature. Rheumatol Int. 2004;24:234–37. doi: 10.1007/s00296-003-0395-z. [DOI] [PubMed] [Google Scholar]
- 2.Marto G, Klitna Z, Biléu MC, Barcelos A. Remitting seronegative symmetrical synovitis with pitting edema syndrome, associated with prostate adenocarcinoma: a case report. Acta Reumatol Port. 2010;35:358–60. [PubMed] [Google Scholar]
- 3.Salam A, Henry R, Sheeran T. Acute onset polyarthritis in older people: Is it RS3PE syndrome? Cases J. 2008;1:132. doi: 10.1186/1757-1626-1-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muller S, Hider SL, Belcher J, et al. Is cancer associated with polymyalgia rheumatica? A cohort study in the General Practice Research Database. Ann Rheum Dis. 2014;73:1769–73. doi: 10.1136/annrheumdis-2013-203465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Randazzo CT, Bernard AW, Rund DA. Metastatic prostate cancer mimicking polymyalgia rheumatica. Case Rep Emerg Med. 2011;2011:695320. doi: 10.1155/2011/695320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yamashita H, Kubota K, Mimori A. Clinical value of whole-body PET/CT in patients with active rheumatic diseases. Arthritis Res Ther. 2014;16:423. doi: 10.1186/s13075-014-0423-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCarty DJ, O’Duffy JD, Pearson L, Hunter JB. Remitting seronegative symmetrical synovitis with pitting edema. RS3PE syndrome. JAMA. 1985;254:2763–67. [PubMed] [Google Scholar]
- 8.Nygaard U, Vestergaard C, Koppelhus U. Remitting seronegative symmetrical synovitis with pitting oedema (RS3PE) of hands and feet in an 83-year-old man. Acta Derm Venereol. 2013;93:491–92. doi: 10.2340/00015555-1521. [DOI] [PubMed] [Google Scholar]
- 9.Bhakta BB, Pease CT. Late-onset rheumatoid arthritis: is pitting edema of the hands at onset a good prognostic indicator? Br J Rheumatol. 1997;36:214–19. doi: 10.1093/rheumatology/36.2.214. [DOI] [PubMed] [Google Scholar]
- 10.Cantini F, Salvarani C, Olivieri I, et al. Remitting seronegative symmetrical synovitis with pitting edema (RS3PE) syndrome: a prospective follow up and magnetic resonance imaging study. Ann Rheum Dis. 1999;58:230–36. doi: 10.1136/ard.58.4.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dasgupta B, Cimmino MA, Kremers HM, et al. 2012 Provisional classification criteria for polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology collaborative initiative. Arthritis Rheum. 2012;64:943–54. doi: 10.1002/art.34356. [DOI] [PubMed] [Google Scholar]
- 12.Dasgupta B, Borg FA, Hassan N, et al. BSR and BHPR guidelines for the management of polymyalgia rheumatica. Rheumatology (Oxford) 2010;49:186–90. doi: 10.1093/rheumatology/kep303a. [DOI] [PubMed] [Google Scholar]
- 13.Kane I, Menon S. Carcinoma of the prostate presenting as polymyalgia rheumatica. Rheumatology. 2003;42:385–87. doi: 10.1093/rheumatology/keg058. [DOI] [PubMed] [Google Scholar]
- 14.Hakkou J, Rostom S, Bahiri R, Hajjaj-Hassouni N. Paraneoplastic rheumatic syndromes: report of eight cases and review of literature. Rheumatol Int. 2012;32:1485–89. doi: 10.1007/s00296-011-2252-9. [DOI] [PubMed] [Google Scholar]
- 15.Sidhom OA, Basalaev M, Sigal LH. Renal cell carcinoma presenting as polymyalgia rheumatica. Resolution after nephrectomy. Arch Intern Med. 1993;153:2043–45. [PubMed] [Google Scholar]
- 16.Kampitak T. Polymyalgia rheumatica as the first presentation of metastatic lymphoma. Intern Med. 2010;49:1641–43. doi: 10.2169/internalmedicine.49.3400. [DOI] [PubMed] [Google Scholar]
- 17.Sibilia J, Friess S, Schaeverbeke T, et al. Remitting seronegative symmetrical synovitis with pitting edema (RS3PE): a form of paraneoplastic polyarthritis? J Rheumatol. 1999;26:115–20. [PubMed] [Google Scholar]


