Abstract
In cardiovascular surgery ischemia-reperfusion injury is a challenging problem, which needs medical intervention. We investigated the effects of curcumin on cardiac, myocardial, and mitochondrial parameters in perfused isolated working Guinea pig hearts. After preliminary experiments to establish the model, normoxia was set at 30 minutes, hypoxia was set at 60, and subsequent reoxygenation was set at 30 minutes. Curcumin was applied in the perfusion buffer at 0.25 and 0.5 μM concentrations. Cardiac parameters measured were afterload, coronary and aortic flows, and systolic and diastolic pressure. In the myocardium histopathology and AST in the perfusate indicated cell damage after hypoxia and malondialdehyde (MDA) levels increased to 232.5% of controls during reoxygenation. Curcumin protected partially against reoxygenation injury without statistically significant differences between the two dosages. Mitochondrial MDA was also increased in reoxygenation (165% of controls), whereas glutathione was diminished (35.2%) as well as glutathione reductase (29.3%), which was significantly increased again to 62.0% by 0.05 μM curcumin. Glutathione peroxidase (GPx) was strongly increased in hypoxia and even more in reoxygenation (255% of controls). Curcumin partly counteracted this increase and attenuated GPx activity independently in hypoxia and in reoxygenation, 0.25 μM concentration to 150% and 0.5 μM concentration to 200% of normoxic activity.
1. Introduction
Ischemia-reperfusion injury causes challenging problems in cardiovascular surgery [1–3]. Hypoxia and reoxygenation as a model for ischemia and reperfusion [4] have mainly been studied in isolated perfused rat hearts. Neely et al. [5] modified the original Langendorff preparation [6] into the working rat heart model, which we used to investigate the phenomenon of ischemia-reperfusion injury [7]. Now, we changed the rat heart model into isolated perfused working Guinea pig hearts.
Many chemicals used for cardio protection exert severe unwanted side effects. For this reason, natural and more moderate compounds are screened for their protective efficacy against ischemia-reperfusion injury [8]. Curcumin may be a suitable candidate [9] because it has a wide range of clinical activities [10] and structural similarities to antioxidants, for example, tocopherols and cardio protective compounds like flavonoids.
We present a first set of data about cardio protective effects of curcumin using the perfused isolated working Guinea pig heart model. The aims of this study were to find the appropriate experimental conditions for our model and to investigate effects of curcumin under these experimental conditions. In the future, we intend to use this model for the screening of extracts from Indonesian medicinal plants and to study their effects on hypoxia/ischemia-reoxygenation/reperfusion injury.
2. Materials and Methods
The complete isolated working heart perfusion device was established and all experiments were conducted at the Department of Physiology, Faculty of Medicine, Universitas Indonesia. Young adult Guinea pigs, aged one year and weighing 300–400 g, were obtained from the Animal Breeding Department of the Agricultural University of Bogor, Indonesia. All substances used (if not indicated differently) were purchased from Merck, Darmstadt, Germany, via their Indonesian subsidiary in Jakarta or from Sigma-Aldrich at highest purity available.
2.1. The Model
The arrangement of the perfusion apparatus had been described and schematically depicted by Deisinger and Freisleben [11]. Each Guinea pig was neck-fractured by rapid cervical dislocation, the heart was excised, and the aorta immediately connected to the aortic cannula of the apparatus and was perfused retrogradely as known from the Langendorff preparation. Subsequently, the perfusion cannula was connected anterogradely to the left atrium for normoxic perfusion with Krebs-Henseleit buffer [12] gassed with carbogen (O2 95%/CO2 5%). During hypoxia, hearts were perfused with the same buffer gassed with N2 95%/CO2 5%. In reoxygenation, conditions were readjusted to “normoxia,” that is, anterograde perfusion with carbogen-gassed buffer [7]. Normoxia and reoxygenation lasted 30 min, each, whereas hypoxic perfusion varied from 15 to 60 min.
For perfusion of the myocardium, it is important that the cannulation of the aorta does not disturb the access to the coronary arteries. The perfusate flows back to the right atrium mainly via the sinus coronarius and drops from the heart via the open pulmonary artery and venae cavae into a glass vessel, from where it flows back into the buffer circulation. Coronary flow was measured by the volume of perfusate that dropped per minute from the heart into a graduated glass vessel.
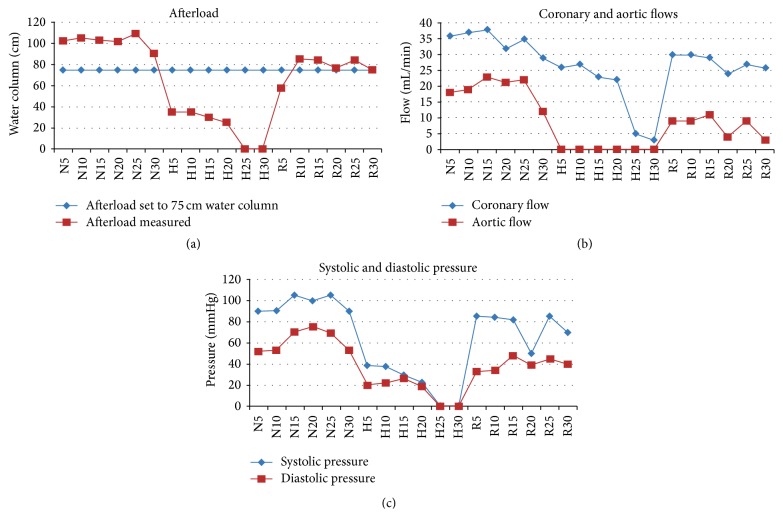
Afterload was measured as the height (cm) of the buffer column, which could be maintained by the aortic pressure. Aortic flow was determined as the volume (mL) per minute at a fixed afterload of 75 cm buffer column (Figure 1).
Figure 1.
Parameters measured in preliminary experiments: (a) Afterload measured (red squares) during the course of 30 min of normoxia (about 100 cm water column) immediately dropped within 5 min of hypoxia to about 35 cm water column and then slowly decreased to zero between 10 and 25 min of hypoxia. In reoxygenation, afterload immediately improved again to 60 cm water column within 5 min and recovered to around 80 cm water column between 10 and 30 min of reoxygenation (red squares). To set up the “working” heart model, afterload was constantly set to 75 cm water column (blue diamond line). In subsequent experiments, the heart muscle had to pump against this pressure in its cardiac output (systolic phase). (b) Due to our model, aortic flow (red squares) was zero during hypoxia; it was around 20 mL/min in normoxia and recovered to about 10 mL/min (about 50% of normoxia) during the first 15 min of reoxygenation and then started to fluctuate and slowly decreased to almost zero by the end of experimental reoxygenation (R30). Coronary flow (blue diamonds) slowly decreased during normoxia and hypoxia from 35–40 mL/min to 3–5 mL/min by the end of hypoxia and then recovered rapidly to 30 mL/min in the beginning of reoxygenation and subsequently decreased slightly to 25 mL/min within 30 min of reoxygenation. (c) Systolic pressure (blue diamonds) was 90–100 mmHg in normoxia, dropped to 40 mmHg within 5 min of hypoxia, and further decreased to zero in 25 min of hypoxia. Within 5 min of reoxygenation, systolic pressure immediately recovered to 80–85 mmHg for 15 min and then started to fluctuate between 50 and 85 mmHg until the end of the experimental reoxygenation (R30). Diastolic pressure (red squares) showed similar course at a lower level with normoxic pressure of 55–75 mmHg, decreased to 20–25 mmHg in hypoxia, and dropped to zero after 20–25 min of hypoxia. Recovery during reoxygenation was stable between 35 and 45 mmHg until the end of experimental reoxygenation. These data in preliminary experiments served as the basis of setting up our model in subsequent main experiments with 60 min of hypoxia.
To measure systolic and diastolic pressure and heart rate a Nikon Kohden Polygraph was connected. This device also recorded the electrocardiogram, that is, initial arrhythmias; however, further electrocardiographic records were not in an interpretable quality (not shown). Hence, cardiograms were only used to decide about inclusion-exclusion criteria.
2.2. Experimental Procedures: Preliminary Experiments
We conducted preliminary experiments in order to
set up the model and the sequential course of normoxia, hypoxia, and reoxygenation with 15 or 30 min of normoxic perfusion, 15, 30, or 60 min of hypoxia, and subsequent reoxygenation up to 30 min. In these experiments the excised hearts were examined for suitability, that is, stability over the time course in this model,
determine inclusion-exclusion criteria and find out sensitive parameters for measurements in this model. Afterload was first determined in preliminary experiments and then adjusted to 75 cm water column in the main experiments (Figure 1),
find appropriate concentrations of curcumin in this model. We applied 0.25, 0.5, and 1 μM concentrations, given into the perfusate at 15 min of normoxia. After a first set of experiments, application of 1 μM concentration was discontinued because we did not see dose-dependent effects and lower concentrations (0.25 and 0.5 μM) were even more effective in our model (not shown).
In our preliminary experiments hematoxylin-eosin staining and histopathological examination were conducted using Olympus light microscope at 1000x magnification and compared to aspartate aminotransferase (AST) measurements. For the latter Merck kit (Cat. number 14829) with solution A containing Tris HCl pH 7.8, L-aspartate, malate dehydrogenase, and lactate dehydrogenase and solution B containing 2-oxoglutarate and NADH was used according to the manufacturer's manual with slight modification. One mL of solution A was mixed with 0.25 mL of solution B and incubated for 30 min. To 1 mL of this mixture 0.2 mL of perfusate was added and the absorption measured at 340 nm in Shimadzu spectrophotometer at 1, 2, and 3 min. In our preliminary experiments, we had tested the volumes needed for measurement of the low AST concentrations in the perfusate. The units per liter perfusate were then correlated to the weight of heart tissue and expressed as U × L−1 × g−1 heart tissue.
In the main experiments, histopathological examination was not continued, because histopathology correlated well with AST measurements and myocardial tissue was rather needed for the isolation of mitochondria and all other experimental procedures.
For statistical evaluation one-way ANOVA was used (normal parametric distribution); for nonparametric evaluation post hoc Tukey and Wilcoxon-Mann-Whitney U tests were applied. Results are presented as mean values ± standard deviation (SD); statistical significance is set to p < 0.05. Furthermore, the means of all normoxic values are set to 100% and the results of hypoxia, reoxygenation, curcumin 0.25 μM, and curcumin 0.5 μM concentrations expressed as percentage.
2.3. Inclusion-Exclusion Criteria
Our animal housing and experimental procedures strictly followed the Helsinki and Tokyo regulations on animal studies in their actual versions. Guinea pigs were kept in small groups of 3–5 animals with ad libitum access to food and water, in an acclimatized room with a window and thus natural day-and-night light fluctuations. Inclusion criteria for the main experiments were young adult Guinea pigs, aged one year; body weight 300–400 g; heart rate of the isolated perfused heart between 150 and 250 beats per minute; and coronary flow of the isolated perfused heart during normoxia between 20 and 50 mL.
Exclusion criteria for the main experiments were time between excision of the heart and retrograde perfusion more than 3 min; initial arrhythmias after cannulation longer than 3 min; and afterload = aortic pressure performance: less than 75 cm water column in normoxia.
2.4. Main Experiments
Conditions in the main experiments are indicated where necessary. Protein was measured according to Lowry et al. [13]; thiobarbituric acid-reactive substances (TBARS) were determined according to Chirico [14] using Waters HPLC device with a Spherisorb 5ODS2-C18 column. TBARS are expressed as malondialdehyde (MDA) throughout the text. Glutathione (GSH) was determined with the method of Ellman [15].
Mitochondria were prepared as described by Mela and Seitz [16] omitting nagarse. Relative specific activity of succinate dehydrogenase (SDH) was measured for control: 40 μL of the sample was added into a cuvette containing a mixture of 120 μL NaPi 800 mM, pH 7.6; 120 μL KCN 10 mM; 240 μL sodium succinate 100 mM; 48 μL 2,6-dichlorophenolindophenol 1 mM; and 632 μL distilled water. The absorption at λ = 600 nm was followed for 5 min at 37°C in a Shimadzu spectrophotometer equipped with a thermostat cuvette holder. We measured relative specific SDH activities between 7.89 and 12.72 to characterize our mitochondrial preparations [17].
Enzyme activity of glutathione peroxidase (GPx) and glutathione reductase (GR) were measured as described by Flohé and Günzler [18] with slight modifications: our reaction mixture contained 200 μL GSH 20 mM; 200 μL sodium azide 20 mM; 200 μL EDTA 20 mM; 200 μL NADPH 1 mM; and 100 μL NaPi 0.1 M, pH 7.0. For measurement of GPx activity, 20 μL glutathione reductase 1 U was added and incubated with 60 μL isolation buffer at 37°C for 10 min. Subsequently, 20 μL of mitochondrial preparation was added and absorption followed for 5 min at λ = 340 nm. For measurement of glutathione reductase, instead of 20 μL glutathione reductase 1 U, glutathione peroxidase was added, accordingly. All photometric measurements were accomplished in a Shimadzu spectrophotometer equipped with a thermostat cuvette holder.
3. Results
3.1. Preliminary Experiments
The time course of our model with normoxia, hypoxia, and reoxygenation, 30 min each, is depicted in Figure 1. In our preliminary experiments, hypoxia varied, 15, 30, or 60 min; throughout the main experiments hypoxia was set to 60 min.
Heart rate was between 173 and 217 beats per minute and turned out to be a stable parameter in our experimental setting: it recovered after 15 and 30 min of hypoxia in reoxygenation to 100.5% and 98.9%, respectively, without curcumin, and to 97.1% and 101.7%, respectively, with 0.25 and 0.5 μM curcumin. Differences between all these values were statistically not significant indicating that the hearts were stable over the experimental course of our model.
For measurement of systolic pressure a water column in our device [7, 11] with normoxic values up to 100 cm was used corresponding to and exceeding the constant afterload water column of 75 cm, against which the isolated heart had to perform its work. In addition, systolic and diastolic pressure were measured using a mercury manometer (Figure 1(c)).
3.1.1. Histopathology and Aspartate Aminotransferase (AST)
Histopathological changes depended on the duration of hypoxia: in hypoxia up to 15 min we did not observe changes in tissue ultrastructure; however, changes became visible at 30 min and, particularly after 60 min, destruction of the myocardium was obvious (not shown). This result mirrored the measurement of AST activity in the perfusate: with only after 60 min of hypoxia, AST activity increased significantly during reoxygenation indicating tissue damage and release of AST from cardiomyocytes into the perfusate.
3.2. Main Experiments
For the main experiments, the following experimental settings were chosen: normoxia 30 min, hypoxia 60 min, and subsequent reoxygenation 30 min. Curcumin was injected into the perfusion buffer at 0.25 μM or 0.5 μM concentrations after 15 min of normoxic perfusion.
3.2.1. Cardiac Parameters
Cardiac parameters measured were systolic pressure, aortic flow, and coronary flow (Table 1).
Table 1.
Cardiac parameters.
| Normoxia | Hypoxia 60 min | Reoxygenation | |
|---|---|---|---|
| Systolic pressure: cm H2O (n = 9; mean ± SD) | |||
| 94.61 ± 9.38 | 0 | 52.31 ± 6.12 (55.3%) p < 0.05 | |
| Curc. 0.25 µM | 92.73 ± 10.06 | 0 | 83.37 ± 7.96 (89.9%) |
| Curc. 0.5 µM | 95.12 ± 11.0 | 0 | 77.78 ± 10.24 (83.2%) |
| Normoxia (mean = 94.15 = 100%) | 73.2% | ||
| Curc. 0.25 µM | 85.6% | ||
| Curc. 0.5 µM | 88.1% | ||
|
| |||
| Aortic flow: mL × min−1 (n = 9; mean ± SD) | |||
| 14.13 ± 4.70 | 0 | 4.37 ± 3.85 (30.9%) p = 0.05 | |
| Curc. 0.25 µM | 12.20 ± 3.75 | 0 | 6.10 ± 3.34 (50.0%) |
| Curc. 0.5 µM | 14.27 ± 4.73 | 0 | 6.73 ± 4.33 (47.2%) |
| Normoxia (mean = 13.5 = 100%) | 32.4% | ||
| Curc. 0.25 µM | 45.2% | ||
| Curc. 0.5 µM | 49.9% | ||
|
| |||
| Coronary flow: mL × min−1 (n = 9; mean ± SD) | |||
| 9.53 ± 3.04 | 0 | 15.97 ± 7.39 (167.6%) | |
| Curc. 0.25 µM | 10.53 ± 2.5 | 0 | 13.6 ± 3.56 (129.2%) |
| Curc. 0.5 µM | 8.9 ± 6.48 | 0 | 13.27 ± 7.19 (149.1%) |
| Normoxia (mean = 9.65 = 100%) | 165.5% | ||
| Curc. 0.25 µM | 140.9% | ||
| Curc. 0.5 µM | 137.5% | ||
3.2.2. Myocardial Tissue
Myocardial tissue parameters measured are shown in Table 2.
Table 2.
Myocardial tissue parameters.
| Normoxia | Hypoxia | Reoxygenation | |
|---|---|---|---|
| Aspartate aminotransferase (AST) | |||
| AST: U × L−1 × g−1 heart tissue (n = 5; mean ± SD) | |||
| 2.934 ± 1.451 (100%) | 3.249 ± 1.119 (110.7%) | 4.105 ± 1.917 (139.9%) | |
| N versus R p = 0.05 | |||
| Curc. 0.25 µM | 3.382 ± 2.149 (115.3%) | 2.397 ± 0.901 (81.7%) | |
| R versus R0.25 p < 0.05 | |||
| Curc. 0.5 µM | 3.671 ± 1.446 (125.1%) | 3.192 ± 1.516 (108.8%) | |
|
| |||
| TBARS, expressed as malondialdehyde (MDA) | |||
| MDA: nmol × g−1 heart tissue (n = 6; mean ± SD; N versus R and H versus H0.5 p < 0.05) | |||
| 8.33 ± 5.30 (100%) | 9.36 ± 6.24 (112.4%) | 19.37 ± 8.31 (232.5%; N versus R p < 0.05) | |
| Curc. 0.25 µM | 8.86 ± 0.48 (106.4%) | 12.46 ± 10.30 (149.6%) | |
| Curc. 0.5 µM | 5.88 ± 5.85 (70.6%) | 12.52 ± 6.85 (150.3%) | |
| H versus H0.5 (p < 0.05) | |||
The activity of AST was measured in the perfusate as U × L−1 and then correlated to the weight of the heart (= g heart tissue). TBARS, thiobarbituric acid reactive substances; N, normoxia; H, hypoxia; R, reoxygenation; R0.25, reoxygenation with curcumin (curc.) 0.25 µM; H0.5, hypoxia with 0.5 µM curc.
(1) Aspartate Aminotransferase (AST). After 60 min of hypoxia, AST activity increased significantly during reoxygenation indicating tissue damage and release of AST from cardiomyocytes into the perfusate (Table 2). Curcumin, at 0.25 μM concentration, protected the myocardium from AST release significantly from 139.9% in reoxygenation to normoxic values. This protective effect was significant with 0.25 μM (p < 0.05) but not with 0.5 μM concentration (Table 2).
(2) Thiobarbituric Acid-Reactive Substances (TBARS)/Malondialdehyde (MDA). Lipid peroxidation (LPO) is considered a major reason of membrane destruction; LPO is often determined via thiobarbiturate reaction and expressed through its byproduct malondialdehyde (MDA). As can be seen in Table 2, MDA increased to 232.5% of normoxia (8.33 ± 5.30 nmol × g−1 tissue, 100%) during reoxygenation (19.37 ± 8.31 nmol × g−1 tissue) after 60 min of hypoxia. Although during hypoxia 0.5 μM concentration of curcumin had a stronger effect than 0.25 μM, both concentrations equally reduced MDA levels to 150% in reoxygenation.
3.2.3. Mitochondrial Parameters
The mitochondrial parameters measured are presented in Table 3.
Table 3.
Mitochondrial parameters.
| Normoxia | Hypoxia | Reoxygenation | |
|---|---|---|---|
| MDA: nmol × mg−1 mitochondrial protein (n = 6; mean ± SD; N versus R and R versus R0.25 p < 0.05) | |||
| 17.85 ± 2.79 (100%) | 21.24 ± 3.53 (119.0%) | 29.52 ± 9.47 (165.4%; N versus R; p < 0.05) | |
| Curc. 0.25 µM | 17.68 ± 4.40 (99.1%) | 16.47 ± 1.99 (92.3%; R versus R0.25; p < 0.05) | |
| Curc. 0.5 µM | 19.93 ± 3.62 (111.7%) | 24.45 ± 3.24 (137.0%) | |
|
| |||
| GSH: nmol × mg−1 protein (n = 6 in each group; mean ± SD) | |||
| 40.6 ± 10.9 (100%) | 22.9 ± 10.7 (56.4%) | 14.3 ± 4.3 (35.2%) | |
| N versus H (p = 0.011) | N versus R (p < 0.001) | ||
| Curc. 0.25 µM | 19.5 ± 7.1 (48.0%) | 27.0 ± 11.2 (66.5%) | |
| R versus R0.25 (p < 0.05) | |||
| Curc. 0.5 µM | 23.2 ± 7.0 (57.1%) | 28.3 ± 8.0 (69.7%) | |
| R versus R0.5 (p < 0.05) | |||
|
| |||
| GPx: nmol × min−1 × mg−1 protein (n = 6 in each group; mean ± SD) | |||
| 324.1 ± 115.0 (100%) | 392.2 ± 150.1 (121.1%) | 826.1 ± 268.0 (255.2%) | |
| H versus R (p < 0.05) | N versus R (p < 0.05) | ||
| Curc. 0.25 µM | 513.3 ± 59.4 (158.6%) | 498.6 ± 44.5 (153.8%) | |
| R versus R0.25 (p < 0.05) | |||
| Curc. 0.5 µM | 664.4 ± 206.3 (205.3%) | 665.0 ± 219.1 (205.7%) | |
|
| |||
| GR: nmol × min−1 × mg−1 protein (n = 6 in each group; mean ± SD) | |||
| 77.2 ± 15.7 (100%) | 45.3 ± 17.1 (58.8%) | 22.2 ± 9.6 (29.3%; N versus R p < 0.05) | |
| Curc. 0.25 µM | 36.9 ± 16.9 (48.8%) | 35.4 ± 16.0 (46.8%) | |
| Curc. 0.5 µM | 47.3 ± 18.6 (62.5%) | 46.9 ± 18.5 (62.0%; R versus R0.5 p = 0.006) | |
MDA, malondialdehyde; GSH, reduced glutathione; GPx, glutathione peroxidase; GR, glutathione reductase; N, normoxia; H, hypoxia; R, reoxygenation; R0.25, reoxygenation with 0.25 µM curcumin (curc.); R0.5, reoxygenation with 0.5 µM curc.
(1) Thiobarbituric Acid-Reactive Substances (TBARS). Mitochondrial TBARS levels are expressed as nmol MDA per g mitochondrial protein (n = 6). We found higher levels in normoxic mitochondria than in myocardial tissue if correlated to mitochondrial protein, 17.85 ± 2.79 (100%). During hypoxia the increase to 119% was only moderate but significant in reoxygenation, 165.4% (p < 0.05 versus N). Curcumin diminished mitochondrial MDA levels to normoxia at 0.25 μM concentration (R versus R0.25; p < 0.05), whereas 0.5 μM concentration of curcumin was less effective (Table 3).
(2) Reduced Glutathione (GSH). Mitochondrial GSH decreased from 40.6 ± 10.9 nmol × mg−1 protein in normoxia (100%) to 56.4% in hypoxia (p = 0.011 versus N) and 35.2% in reoxygenation (p < 0.001 versus N). During hypoxia, curcumin did not have much effect, but in reoxygenation it significantly increased GSH at both concentrations (Table 3).
(3) Glutathione Peroxidase (GPx). Glutathione peroxidase activity was 324.1 ± 115.0 nmol × min−1 × mg−1 protein in normoxia (100%). During hypoxia GPx activity increased slightly to 121.1% and in reoxygenation significantly to 255.2%. Curcumin, at 0.25 μM concentration, attenuated GPx activity to about 150% and at 0.5 μM concentration to about 200%, both during hypoxia and reoxygenation (Table 3).
(4) Glutathione Reductase (GR). Glutathione reductase activity was 77.2 ± 15.7 nmol × min−1 × mg−1 protein in normoxia (100%). During hypoxia GR activity decreased moderately to 58.8% and in reoxygenation significantly to 29.3% (p < 0.05). During hypoxia, curcumin did not have a significant effect on GR activity, but, in reoxygenation, 0.25 μM concentration increased GR activity to 46.8% and 0.5 μM concentration significantly increased GR activity to 62.0% (R versus R0.5 p = 0.006). Interestingly, values with curcumin were almost the same during hypoxia and reoxygenation, 48.8% and 46.8% at 0.25 μM concentration, 62.5% and 62.0% at 0.5 μM concentration (Table 3).
4. Discussion
In our experiments Guinea pig hearts were more stable than rat hearts over the experimental time course of one hour and thus more suitable to our experimental conditions in Jakarta. The discussion about the stability of the performance of isolated perfused hearts goes back almost four decades; isolated perfused Guinea pig hearts had been considered more stable than rat hearts by some working groups, whereas others could not confirm any differences, which may strongly depend on the experimental conditions [19–26]. We do not want to go into the discussion about differences in metabolic pathways (e.g., endogenous synthesis of ascorbic acid) and whether environmental (e.g., tropical) conditions may play a role. However, we state from our own experience that the slightly bigger Guinea pig hearts make it easier to fix them to the cannulas of the apparatus and thus reduce initial complications such as arrhythmias.
4.1. Main Experiments: Cardiac Parameters
In the main experiments hypoxia was set to 60 min and systolic pressure, aortic flow, and coronary flow were measured as cardiac parameters. Two concentrations of curcumin in the reoxygenation buffer were applied, 0.25 μM and 0.5 μM, but, generally, 0.5 μM curcumin did not exert higher effects than 0.25 μM concentration (after we had already ruled out 1 mM concentration of curcumin in our preliminary experiments).
Systolic pressure recovered during reoxygenation by 55-56%, under 0.25 μM curcumin between 85% and 90% and under 0.5 μM curcumin between 83% and 88%. Aortic flow recovered to 31-32% during reoxygenation, under 0.25 μM curcumin between 45% and 50% and under 0.5 μM curcumin between 47% and 50%.
Coronary flow exerted an overshooting reaction of almost 170% during reoxygenation. This overshoot might depend on the experimental setting of the isolated heart. Coronary flow was measured as the amount of buffer dropping down from the heart's perfused coronary arteries and sinus coronarius. Hence, the “coronary flow” especially during reoxygenation might be a mixture of coronary perfusion and leakiness of coronary vessels. The increase of about 70% over the normoxic value was certainly due to the leakiness of the coronary blood vessels after 60 minutes of hypoxia.
Leakiness of blood vessels is a well-known and dreadful reoxygenation/reperfusion phenomenon often causing considerable edema in tissues as part of ischemia-reperfusion injury [1–3]. Hence, the influence of curcumin in lowering this overshoot can be considered a positive therapeutic effect. Curcumin, at 0.25 μM concentration, reduced the overshoot to roughly 140% and at 0.5 μM concentration to about 138%. Thus, coronary flow under the aspect of ischemia-reperfusion injury did not improve much better with 0.5 μM than with 0.25 μM concentration of curcumin.
4.2. Myocardial Tissue
After 60 min of hypoxia lipid peroxidation destroyed cell membranes and cardiomyocytes became leaky and released AST into the perfusate, where its enzymatic activity increased during reoxygenation; in parallel, also MDA increased to about 233%. During reoxygenation curcumin reduced AST activity significantly at 0.25 μM (p < 0.05), but not at 0.5 μM concentration (p > 0.05). Curcumin reduced MDA significantly during hypoxia only at 0.5 μM, but not at 0.25 μM concentration, whereas both concentrations reduced equally MDA tissue levels from 233% in reoxygenation to about 150%.
Thiobarbiturate is the mostly used reagent to measure lipid peroxidation (LPO) and the result is expressed as TBARS (thiobarbituric acid-reactive substances) or as one of the major byproducts of LPO, MDA. These parameters are widely used as markers of oxidative stress and tissue damage. Recently, discussions have been extended about the concept of oxidative damage and the value of LPO and MDA as generalized markers of oxidative stress in cells, tissues, and body fluids. We do not go into this discussion here; however, one point of criticism often raised is that the markers are not determined at the place of origin. Hence, we tried to overcome this point by differentiating MDA as a parameter of tissue damage, measured from myocardium, and MDA measured from mitochondria as a parameter of LPO in mitochondrial membranes.
In general, 0.5 μM curcumin did not exert higher effects on myocardial tissue parameters (AST, MDA) than 0.25 μM concentration.
4.3. Mitochondrial Parameters
Mitochondrial MDA level was only decreased significantly during reoxygenation by 0.25 μM curcumin, but not by 0.5 μM concentration. At both concentrations, curcumin increased significantly mitochondrial GSH content during reoxygenation, whereas, during hypoxia, no significant effects on MDA and glutathione were observed. We were interested in the activities of glutathione reductase and glutathione peroxidase under the same conditions: The activity of glutathione reductase mirrored well the content of reduced glutathione. During reoxygenation curcumin exerted a significantly stimulating effect on GR at 0.5 μM, but not at 0.25 μM concentration. At either concentration, GR activity was almost the same during hypoxia and reoxygenation.
Glutathione peroxidase was slightly increased in hypoxia, but during reoxygenation its activity was tremendously high, 255% of normoxic control values. Curcumin, at 0.25 μM concentration, attenuated GPx to about 154% (p < 0.05) and at 0.5 μM to 206% (p > 0.05). Interestingly, at both concentrations, GPx had the same activity in hypoxia and reoxygenation of about 150% (0.25 μM curcumin) and 200% (0.5 μM curcumin) of normoxic values. Hence, curcumin, in two concentrations used in our experiments, appeared to be an independent attenuator of both GR and GPx during hypoxia and reoxygenation. Interestingly, on GR 0.5 μM curcumin had a stronger effect than 0.25 μM concentration, whereas the overshoot of GPx activity in reoxygenation was downregulated more strongly by 0.25 than by 0.5 μM of curcumin.
Protective effects through enhanced GPx during hypoxia and reoxygenation in other organs have been reported [27–29]; in human plasma GPx-3 isoenzyme was threefold increased over normal expression during hypoxia [30]. On the contrary, Manikandan et al. [31] reported decreased GPx activity during isoprenaline induced myocardial ischemia in rats. Curcumin at 15 mg × kg−1 body weight (pre- and postischemic application) managed to normalize GPx activity, whereas curcumin administered either pre- or postischemically had much lower effects.
Animal and organ distribution of cGPx was reported to be low in Guinea pig hearts [32] and less than one-third of the activity found in isolated mouse heart atria was detected in Guinea pigs [33]. On the other hand, overexpression of PHGPx protected a guinea pig cell line from LPO-mediated injury [34]. In mitochondria, two isoforms out of various GPx isoenzymes [35, 36] appear to exist, for example, cGPx (GPx-1) and PHGPx (GPx-4) [37, 38], and GPx-1 was reported to protect mouse heart mitochondria against hypoxia/reoxygenation injury [28]. Transgenic mice overexpressing cGPx were protected against cerebral ischemia/reperfusion injury and apoptosis induced by it, whereas cGPx-mutant mice and nontransgenic control animals were more susceptible [39]. In this context, selenium dependence of GPx isoenzymes should be considered, which differs “hierarchically” between isoforms [32] and we suggest that it should be the scope of future studies with our isolated perfused working guinea pig heart model [40].
During reoxygenation GPx was considerably increased to 255% of control values. Increased GPx activity consumes more GSH and produces GSSG; GR activity is needed to replenish reduced GSH, but diminished GR activity will lead to GSH depletion in hypoxia and reoxygenation. Attenuation of GPx activity by curcumin and concomitant slight stimulation of GR activity, as observed in our model, would help to prevent rapid GSH depletion.
At higher concentration up to 2.5 μM curcumin was reported to protect rat liver mitochondria against tert-butylhydroxyperoxide- (t-BHP-) induced mitochondrial dysfunction, such as breakdown of transmembrane potential and swelling [17, 41]. On the other hand, at these concentrations curcumin was suspected to consume reduced glutathione [41]. It was assumed that curcumin participates in phenoxyl-radical recycling mechanisms as demonstrated for tocopherol and other phenolic compounds [42–44]. Such reductive “recycling” mechanisms involve reduced GSH [43, 44] and may consume glutathione at higher concentrations of curcumin (and other phenolic antioxidants) and thus contribute to GSH depletion during oxidative stress [17, 45]. Although these mechanisms still need further clarification, they may be the reason for prooxidant effects at higher concentrations; we had to rule out 1 μM curcumin in our preliminary experimentation and did not see a clear advantage of 0.5 μM over 0.25 μM concentration in some results of our main experiments.
In literature, curcumin concentrations differ considerably between experimental settings. Hence, it is difficult to compare results, especially since pharmacokinetic data are often missing. Pan et al. [46] investigated pharmacokinetic parameters of curcumin in mice: one mg × kg−1 body weight peaked in 0.5 μM plasma concentration, 50% of which was metabolized within 8 h. The concentrations in our perfusion buffer correlated to these data. In a Langendorff rat heart model [8] GPx was not much influenced by curcumin, whereas GR was stimulated. The differences with our results on GPx activity may be due to different animals and the experimental model. In the Langedorff preparation the isolated heart is perfused retrogradely, whereas in our model the isolated working heart is perfused anterogradely and its mechanical work is closer to physiological conditions. Their study, which only presented one value for ischemia-reperfusion (I/R) observed a decrease in GR activity during I/R to almost 47% [8]. Their value is very close to the average (about 44%) of our values in hypoxia (58.8%) and reoxygenation (29.3%). This decrease of GR during I/R can only be considered as an enzymatic or metabolic dysregulation, because the low GR activity cannot replenish higher GSH consumption by the oxidative stress during hypoxia/ischemia-reoxygenation/reperfusion, including the overshoot of GPx. Metabolic dysregulations (e.g., calcium paradox) have been observed in the scenario of ischemia-reperfusion injury [1–3].
Curcumin appeared to be an independent regulator of GR and GPx activities under our experimental conditions. In hypoxia and in reoxygenation, 0.25 μM concentration of curcumin attenuated GPx activity to 150% and 0.5 μM concentration of curcumin attenuated GPx to 200% of normoxic activity and, thus, moderately reduced the overshoot of GPx activity during reoxygenation. Concomitantly, curcumin attenuated GR during reoxygenation through moderate upregulation with 0.25 μM curcumin and significant upregulation with 0.5 μM concentration; in other words, towards GR 0.5 μM curcumin was more effective than the lower concentration. This attenuating effect on GR activity by curcumin was also observed in the Langendorff preparation by the before-mentioned study [8].
These considerations demonstrate that the concentration of curcumin is crucial to its metabolic effects; that is, the dosage of curcumin determines whether it exerts therapeutic activity. Moreover, the therapeutic efficacy of curcumin appears to go beyond its antioxidant effects [47, 48]: curcumin exerts regulatory effects on expression and activity of the enzymes involved in mitochondrial glutathione turnover.
5. Conclusion
In our experimental setting of the isolated perfused working Guinea pig heart curcumin exerts protection against hypoxia-reoxygenation injury at 0.25 μM and 0.5 μM concentrations on cardiac parameters and myocardial tissue damage and on mitochondrial GSH turnover. The higher concentration did not exert advantages over the lower one on cardiac parameters and myocardial tissue. On parameters of mitochondrial GSH turnover measured in our study, 0.5 μM concentration was only advantageous towards GR. In clinical cardio protective dose determination it should be considered that curcumin appears to have an upper dose limitation towards cardiac ischemia-reperfusion injury.
Acknowledgments
The authors are especially thankful to Professor Zimmer, posthumously, who had donated the entire perfusion device to the Medical Faculty at Universitas Indonesia. His Guest Professorship in Jakarta, in 1998, was supported by the German Academic Exchange Service (DAAD). Financial support to this research project by the URGE Program of the Indonesian Government and assistance by the Deutsch-Indonesische Gesellschaft für Medizin (DIGM e.V.) as well as the Indonesian Society For Free Radical Research (INA-SFRR) are also gratefully acknowledged. Furthermore, the authors want to express their gratitude to Dr. Gordon McDonald for proofreading the paper.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Freisieben H.-J. Lipoate ameliorates ischemia-reperfusion in animal models. Clinical Hemorheology and Microcirculation. 2000;23(2–4):219–224. [PubMed] [Google Scholar]
- 2.Hanselmann A., Beyersdorf F., Matheis G., et al. Verminderung des Postischämie-Syndroms nach akutem peripherem Gefäßverschluß durch Modifikation der initialen Reperfusion unter Berücksichtigung des Kalziumgehaltes des Reperfusates. Zeitschrift für Herz-, Thorax- und Gefäßchirurgie. 1990;4:13–20. (Ger). [Google Scholar]
- 3.Mitrev Z., Beyersdorf F., Hallmann R., et al. Reperfusion in skeletal muscle: controlled limb reperfusion reduces local and systemic complications after prolonged ischemia. Cardiovascular Surgery. 1994;2(6):737–748. [PubMed] [Google Scholar]
- 4.Ytrehus K. The ischemic heart—experimental models. Pharmacological Research. 2000;42(3):193–203. doi: 10.1006/phrs.2000.0669. [DOI] [PubMed] [Google Scholar]
- 5.Neely J. R., Liebermeister H., Battersby E. J., Morgan H. E. Effect of pressure development on oxygen consumption by isolated rat heart. American Journal of Physiology. 1967;212(4):804–814. doi: 10.1152/ajplegacy.1967.212.4.804. [DOI] [PubMed] [Google Scholar]
- 6.Langendorff O. Untersuchungen am überlebenden Säugetierherzen. Pflüger, Archiv für die Gesammte Physiologie des Menschen und der Thiere. 1895;61(6):291–332. doi: 10.1007/bf01812150. [DOI] [Google Scholar]
- 7.Freisleben H.-J., Kriege H., Clarke C., Beyersdorf F., Zimmer G. Hemodynamic and mitochondrial parameters during hypoxia and reoxygenation in working rat hearts. Arzneimittel-Forschung/Drug Research. 1991;41(1):81–88. [PubMed] [Google Scholar]
- 8.González-Salazar A., Molina-Jijón E., Correa F., et al. Curcumin protects from cardiac reperfusion damage by attenuation of oxidant stress and mitochondrial dysfunction. Cardiovascular Toxicology. 2011;11(4):357–364. doi: 10.1007/s12012-011-9128-9. [DOI] [PubMed] [Google Scholar]
- 9.Wongcharoen W., Phrommintikul A. The protective role of curcumin in cardiovascular diseases. International Journal of Cardiology. 2009;133(2):145–151. doi: 10.1016/j.ijcard.2009.01.073. [DOI] [PubMed] [Google Scholar]
- 10.Goel A., Kunnumakkara A. B., Aggarwal B. B. Curcumin as ‘Curecumin’: from kitchen to clinic. Biochemical Pharmacology. 2008;75(4):787–809. doi: 10.1016/j.bcp.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 11.Deisinger B., Freisleben H.-J. Animal models in hypoxia/reoxygenation and ischemia/reperfusion: II. Perfusion procedures. The Indonesian Journal of Vascular Surgery. 1998;2(1):1–12. [Google Scholar]
- 12.Krebs H. A., Henseleit K. Untersuchungen über die Harnstoffbildung im Tierkörper. Biological Chemistry Hoppe-Seyler. 1932;210:33–66. (Ger). [Google Scholar]
- 13.Lowry O. H., Rosenbrough N. J., Farr A. L., Randall R. J. Protein measurement with the Folin phenol reagent. The Journal of Biological Chemistry. 1951;193(1):265–275. [PubMed] [Google Scholar]
- 14.Chirico S. High-performance liquid chromatography-based thiobarbituric acid tests. Methods in Enzymology. 1994;234:314–318. doi: 10.1016/s0076-6879(94)33035-2. [DOI] [PubMed] [Google Scholar]
- 15.Ellman G. L. Tissue sulfhydryl groups. Archives of Biochemistry and Biophysics. 1959;82(1):70–77. doi: 10.1016/0003-9861(59)90090-6. [DOI] [PubMed] [Google Scholar]
- 16.Mela L., Seitz S. Isolation of mitochondria with emphasis on heart mitochondria from small amount of tissue. Methods in Enzymology. 1979;55:39–46. doi: 10.1016/0076-6879(79)55006-x. [DOI] [PubMed] [Google Scholar]
- 17.Susilowati S., Suyatna F. D., Setiawati A. The prevention of curcumin against rat liver mitochondrial swelling induced by tert-butylhydroperoxide. Medical Journal of Indonesia. 2006;15(3):131–136. doi: 10.13181/mji.v15i3.230. [DOI] [Google Scholar]
- 18.Flohé L., Günzler W. A. Assays of glutathione peroxidase. Methods in Enzymology. 1984;105:114–121. doi: 10.1016/s0076-6879(84)05015-1. [DOI] [PubMed] [Google Scholar]
- 19.Bünger R., Haddy F. J., Querengässer A., Gerlach E. An isolated guinea pig heart preparation with in vivo like features. Pflügers Archiv—European Journal of Physiology. 1975;353(4):317–326. doi: 10.1007/bf00587028. [DOI] [PubMed] [Google Scholar]
- 20.Bünger R., Sommer O., Walter G., Stiegler H., Gerlach E. Functional and metabolic features of an isolated perfused guinea pig heart performing pressure-volume work. Pflügers Archiv. 1979;380(3):259–266. doi: 10.1007/bf00582904. [DOI] [PubMed] [Google Scholar]
- 21.Bünger R., Swindall B., Brodie D., Zdunek D., Stiegler H., Walter G. Pyruvate attenuation of hypoxia damage in isolated working guinea-pig heart. Journal of Molecular and Cellular Cardiology. 1986;18(4):423–438. doi: 10.1016/S0022-2828(86)80905-1. [DOI] [PubMed] [Google Scholar]
- 22.Flynn S. B., Gristwood R. W., Owen D. A. A. Characterization of an isolated, working guinea-pig heart including effects of histamine and noradrenaline. Journal of Pharmacological Methods. 1978;1(3):183–195. doi: 10.1016/0160-5402(78)90048-7. [DOI] [Google Scholar]
- 23.Gessner B., Müller-Ruchholtz E. R., Reinauer H. Regulation der pyruvatdehydrogenaseaktivität und dynamik des isoliert perfundierten meerschweinchenherzens im thiaminmangel. Pflügers Archiv. 1972;334(4):327–344. doi: 10.1007/BF00592167. [DOI] [PubMed] [Google Scholar]
- 24.Maddock H. L., Broadley K. J., Bril A., Khandoudi N. Effects of adenosine receptor agonists on guinea-pig isolated working hearts and the role of endothelium and NO. Journal of Pharmacy and Pharmacology. 2002;54(6):859–867. doi: 10.1211/0022357021779041. [DOI] [PubMed] [Google Scholar]
- 25.Soboll S., Buenger R., Müller M., Sommer O. Compartmentation of adenine nucleotides in the isolated working guinea pig heart stimulated by noradrenaline. Biological Chemistry Hoppe-Seyler. 1981;362(2):125–132. doi: 10.1515/bchm2.1981.362.1.125. [DOI] [PubMed] [Google Scholar]
- 26.Suwito R. R. Die langzeitstabilität isolierter, unterschiedlich belasteter, arbeitender rattenherzen bei zusatz von pyruvat zum perfusionsmedium [Dissertation] Berlin, Germany: Freie Universität Berlin; 1983 (German) [Google Scholar]
- 27.Lepore D. A., Shinkel T. A., Fisicaro N., et al. Enhanced expression of glutathione peroxidase protects islet β cells from hypoxia-reoxygenation. Xenotransplantation. 2004;11(1):53–59. doi: 10.1111/j.1399-3089.2004.00082.x. [DOI] [PubMed] [Google Scholar]
- 28.Thu V. T., Kim H. K., Ha S. H., et al. Glutathione peroxidase 1 protects mitochondria against hypoxia/reoxygenation damage in mouse hearts. Pflügers Archiv. 2010;460(1):55–68. doi: 10.1007/s00424-010-0811-7. [DOI] [PubMed] [Google Scholar]
- 29.White C. W., Jackson J. H., McMurtry I. F., Repine J. E. Hypoxia increases glutathione redox cycle and protects rat lungs against oxidants. Journal of Applied Physiology. 1988;65(6):2607–2616. doi: 10.1152/jappl.1988.65.6.2607. [DOI] [PubMed] [Google Scholar]
- 30.Bierl C., Voetsch B., Jin R. C., Handy D. E., Loscalzo J. Determinants of human plasma glutathione peroxidase (GPx-3) expression. The Journal of Biological Chemistry. 2004;279(26):26839–26845. doi: 10.1074/jbc.m401907200. [DOI] [PubMed] [Google Scholar]
- 31.Manikandan P., Sumitra M., Aishwarya S., Manohar B. M., Lokanadam B., Puvanakrishnan R. Curcumin modulates free radical quenching in myocardial ischaemia in rats. The International Journal of Biochemistry & Cell Biology. 2004;36(10):1967–1980. doi: 10.1016/j.biocel.2004.01.030. [DOI] [PubMed] [Google Scholar]
- 32.Brigelius-Flohé R. Tissue-specific functions of individual glutathione peroxidases. Free Radical Biology and Medicine. 1999;27(9-10):951–965. doi: 10.1016/s0891-5849(99)00173-2. [DOI] [PubMed] [Google Scholar]
- 33.Floreani M., Napoli E., Palatini P. Role of antioxidant defences in the species-specific response of isolated atria to menadione. Comparative Biochemistry and Physiology Part C: Toxicology & Pharmacology. 2002;132(2):143–151. doi: 10.1016/s1532-0456(02)00060-1. [DOI] [PubMed] [Google Scholar]
- 34.Yagi K., Komura S., Kojima H., et al. Expression of human phospholipid hydroperoxide glutathione peroxidase gene for protection of host cells from lipid hydroperoxide-mediated injury. Biochemical and Biophysical Research Communications. 1996;219(2):486–491. doi: 10.1006/bbrc.1996.0260. [DOI] [PubMed] [Google Scholar]
- 35.Mannervik B. The enzymes of glutathione metabolism: an overview. Biochemical Society Transactions. 1987;15(4):717–718. doi: 10.1042/bst0150717. [DOI] [PubMed] [Google Scholar]
- 36.Meister A. Glutathione metabolism and its selective modification. The Journal of Biological Chemistry. 1988;263(33):17205–17208. [PubMed] [Google Scholar]
- 37.Imai H., Nakagawa Y. Regulatory and cytoprotective aspects of lipid hydroperoxide metabolism. Free Radical Biology and Medicine. 2003;34(2):145–169. doi: 10.1016/s0891-5849(02)01197-8. [DOI] [PubMed] [Google Scholar]
- 38.Handy D. E., Loscalzo J. Redox regulation of mitochondrial function. Antioxidants & Redox Signaling. 2012;16(11):1323–1367. doi: 10.1089/ars.2011.4123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Furling D., Ghribi O., Lahsaini A., Mirault M.-E., Massicotte G. Impairment of synaptic transmission by transient hypoxia in hippocampal slices: improved recovery in glutathione peroxidase transgenic mice. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(8):4351–4356. doi: 10.1073/pnas.060574597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Venardos K., Harrison G., Headrick J., Perkins A. Effects of dietary selenium on glutathione peroxidase and thioredoxin reductase activity and recovery from cardiac ischemia-reperfusion. Journal of Trace Elements in Medicine and Biology. 2004;18(1):81–88. doi: 10.1016/j.jtemb.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 41.Suyatna F. D., Djohan R., Nafrialdi A., Suherman S. K. The antioxidant effects of curcumin on rat liver mitochondrial dysfunction induced by tert-butylhydroperoxide. Journal of Ecophysiology and Occupational Health. 2004;4:145–151. [Google Scholar]
- 42.Freisleben H.-J. Free radicals and the antioxidant network. In: Freisleben H.-J., Deisinger B., editors. Free Radical-Related Diseases and Antioxidants in Indonesia. Sankt Augustin, Germany: Gardez; 1999. pp. 1–12. [Google Scholar]
- 43.Kagan V. E., Serbinova E. A., Forte T., Scita G., Packer L. Recycling of vitamin E in human low density lipoproteins. Journal of Lipid Research. 1992;33(3):385–397. [PubMed] [Google Scholar]
- 44.Kagan V. E., Freisleben H.-J., Tsuchiya M., Forte T., Packer L. Generation of probucol radicals and their reduction by ascorbate and dihydrolipoic acid in human low density lipoproteins. Free Radical Research Communications. 1991;15(5):265–276. doi: 10.3109/10715769109105222. [DOI] [PubMed] [Google Scholar]
- 45.Freisleben H.-J., Packer L. Free-radical scavenging activities, interactions and recycling of antioxidants. Biochemical Society Transactions. 1993;21(2):325–330. doi: 10.1042/bst0210325. [DOI] [PubMed] [Google Scholar]
- 46.Pan M.-H., Huang T.-M., Lin J.-K. Biotransformation of curcumin through reduction and glucuronidation in mice. Drug Metabolism and Disposition. 1999;27(4):486–494. [PubMed] [Google Scholar]
- 47.Fiorillo C., Becatti M., Pensalfini A., et al. Curcumin protects cardiac cells against ischemia-reperfusion injury: effects on oxidative stress, NF-κB, and JNK pathways. Free Radical Biology and Medicine. 2008;45(6):839–846. doi: 10.1016/j.freeradbiomed.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 48.Hong D., Zeng X., Xu W., Ma J., Tong Y., Chen Y. Altered profiles of gene expression in curcumin-treated rats with experimentally induced myocardial infarction. Pharmacological Research. 2010;61(2):142–148. doi: 10.1016/j.phrs.2009.08.009. [DOI] [PubMed] [Google Scholar]