Abstract
Background
Childhood obesity is a systemic and complex multilevel public health problem. Research approaches are needed that effectively engage communities in reversing environmental determinants of child obesity.
Objectives
This article discusses the Communities and Schools Together Project (CAST) and lessons learned about the project’s community-based participatory research (CBPR) model.
Methods
A partnership of schools, community organizations, and researchers used multiple methods to examine environmental health risks for childhood obesity and conduct school–community health programs. Action work groups structured partner involvement for designing and implementing study phases.
Lessons Learned
CBPR in child obesity prevention involves engaging multiple communities with overlapping yet divergent goals. Schools are naturally situated to participate in child obesity projects, but engagement of key personnel is essential for functional partnerships. Complex societal problems require CBPR approaches that can align diverse communities and necessitate significant coordination by researchers. CBPR can provide simultaneous health promotion across multiple communities in childhood obesity prevention initiatives. Support for emergent partner activities is an essential practice for maintaining community interest and involvement in multi-year CBPR projects.
Conclusion
Investigator-initiated CBPR partnerships can effectively organize and facilitate large health-promoting partnerships involving multiple, diverse stakeholder communities. Lessons learned from CAST illustrate the synergy that can propel projects that are holistically linked to the agents of a community.
Keywords: child obesity prevention, communities and schools, community-based participatory research, GIS and health, community health
1. Introduction
Childhood obesity has become a major public health concern in the United States. Over the last 30 years, obesity rates have doubled for U.S. children and tripled for adolescents.1 The term obesiogenic has been used to describe the living environments that have developed over the last 50 years that have resulted in the current consumption of readily available, low cost, energy-dense foods and corresponding declines in population physical activity.2–5 Obesity is seen as a “complex system in which behavior is affected by multiple individual-level factors and socioenvironmental factors (ie, factors related to the food, physical, cultural, or economic environment that enable or constrain human behavior, or both).”6(p.1) These complex, systemic factors that have contributed to the current obesity epidemic require new forms of health promotion across multiple dimensions of our economy, public policy frameworks, and community environments.6–8 CBPR is an approach that can help organize and connect these organizations with schools and families for obesity prevention research and interventions because it empowers community solutions and adaptions to local needs.
The Communities and Schools Together (CAST) project created a large partnership between educators, researchers, and non-governmental organizations (NGO), to facilitate place-based health promotion for childhood obesity prevention. CAST used a hybrid approach to CBPR that involved a pre-established, investigator-initiated research design. This article first discusses the project processes used to adhere to CBPR ideals while initiating new working relationships between multiple communities of stakeholders. Additionally, we highlight the lessons learned in integrating this investigator-initiated approach to CBPR and discuss the importance of this type of approach for conducting obesity prevention projects.
2. CBPR Context for CAST
CBPR links the context of change (eg, community, neighborhood) with the diversity of actors needed to study and combat a public health problem like obesity.9 The approach emphasizes development and inclusion of local knowledge about the community, including feasible and acceptable intervention efforts, and does so by engaging communities in the full research process. Indeed, in many respects the community is often placed at the center of the research effort.10–11
Defining a single community within CBPR initiatives is often problematic. A review of CBPR by Viswanathan and colleagues12 found a noticeable degree of variability in CBPR study designs, public health focus, and scope of community involvement. Systemic problems such as obesity are likely to involve a network of communities with overlapping work, membership, or funding. Each community may frame its focus on childhood health through various lenses of nutrition, physical activity, poverty, and family.
Building a CBPR collaboration involving organizations of variable size and capacity presents unique challenges in a partnership. The way a community–researcher partnership develops in a CBPR study can vary and ultimately impact how, by, and for whom the research is conceptualized and conducted. In some cases a community may invite a researcher or research team to work with them. In other cases the researcher or research team may approach a community to undertake research on a topic the investigators perceive as a public health challenge for the community. By making the decision to approach a community, the investigators ultimately must decide which group or groups to contact and include. Such decisions can have implications for power dynamics since the researchers set agendas and take responsibility for the analysis, representation and dissemination of the results, leaving the participants with little power in these aspects of the project.13
The CAST project represented a combination of existing activity within the community and pre-mediated research design and aims on the part of health researchers. In many ways the project was the outgrowth of the personal involvement of several CAST members in local community groups such as the county food policy council and a county-wide school-based body mass index data collection effort. Through these connections and relationships, the lead authors of this paper initiated a plan to respond to a National Institutes of Health (NIH) program grant announcement that focused on community-based research. Their community network relationships enabled them to identify a school district and community grass roots organizations that had strong commitments to either healthy nutrition and/or food system innovations or to research and policy changes related to enhancing child physical activity. While some of these organizations had experience working with one another prior to CAST, the project ultimately brought together a partnership of 60 participants, a school district, and nine NGOs with a central focus on childhood obesity prevention.
CAST relied on the nine key principles for CBPR that were outlined by Israel and colleagues14 as the central organizing tenants for the project. The project was designed to (1) recognize community as a unit of individual and collective identity; (2) build on the strengths, resources, and relationships that already exist within a community; (3) facilitate collaborative partnerships in all phases of research to promote empowerment and power sharing among partners; (4) promote co-learning and reciprocal contributions in relationships between researchers and community partners; (5) integrate a balance between knowledge attainment and action based on the mutual benefit of partners and community; (6) emphasize locally identified problems and ecological perspectives in promoting relevant and socially accepted research and actions; (7) promote collaborative systems development through a cyclical, iterative, and multilevel process of research and practice initiatives; (8) disseminate information to all partners and have all partners participate in dissemination; and (9) recognize and respond to the need for a long-term commitment by a collaboration in ameliorating local public health risks.
3. The CAST Multilevel Partnership
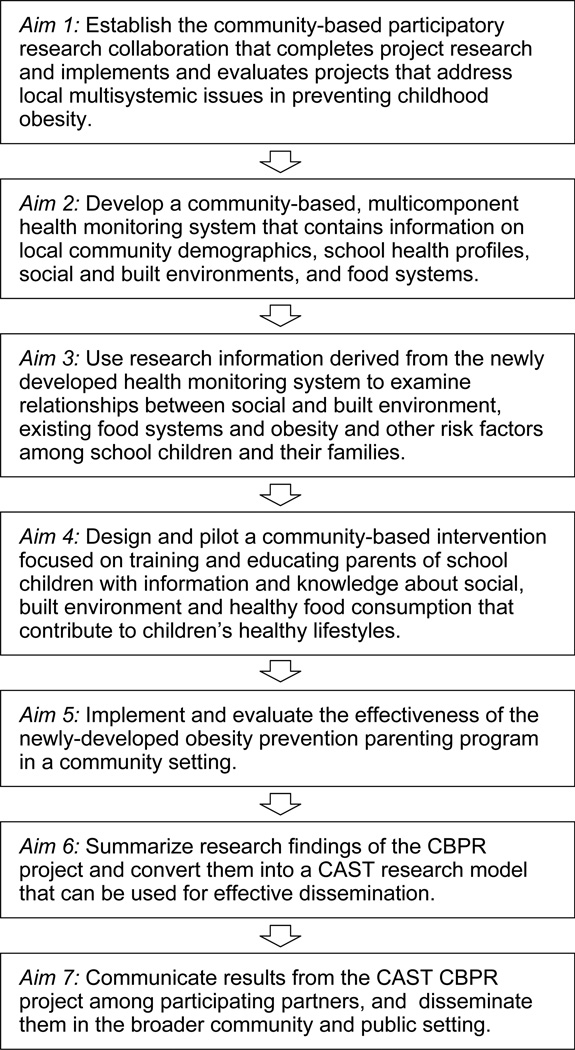
The overarching goal of CAST was to develop a collaborative research partnership to examine the environmental factors increasing childhood risks for obesity. The project’s 5 years of activity were organized around six sequential aims (see Figure 1). While the development of the collaboration (Aim 1) was the focal activity at the beginning of the project, attention to and engagement of the partnership pervaded all research and intervention development in the study.
Figure 1.
CAST Project Aims
The CAST CBPR partnership drew from multiple types of communities with local influence on child physical activity, food environments, and nutrition in the partner school district. In all, four main communities were defined within the project: (1) the school district, including school personnel (administrators, teachers, and staff), (2) the parents and families of the seven elementary schools, (3) the community of NGO groups, and (4) the research–academic community. A discussion of each follows.
The first type or level of community was the school district located in the southern Willamette Valley of Oregon, USA. Although this was a moderately sized district serving 3,000 elementary students, schools were heterogeneous in demographics, school facility quality, and school building culture. Each of the seven elementary schools maintained unique faculty cultures, leadership styles and priorities, relational approaches and histories with external communities, student–family composition, and neighborhood built environment features. School district personnel, including administrators and health and nutrition staff, assisted in connecting and interpreting the norms and needs of individual schools during the project.
The second community in CAST consisted of the elementary school parents. Parents from each elementary school were recruited to form a Parent Advisory Council. Membership represented the ethnic diversity of the school and district. The bilingual, bicultural parent group spent a year developing an organizational and communication structure and building trust. As they learned together as a group, parents began to participate in, various aspects of the project such as collecting information, and piloting project instruments and interventions.
The third community in the CAST partnership consisted of a diverse group of local organizations and non-profit agencies. Each invited partner organization was known to investigators for its local leadership in agriculture–food systems development, nutrition education, or pedestrian transportation. Each organization was contacted prior to proposal submission to NIH to discuss and review the proposal and provide letters of support indicating their specific interests and willingness to participate in the project.
The fourth community involved a multidisciplinary team of academic researchers representing the project’s lead independent research organization, two universities, and a regional intergovernmental agency. Researcher backgrounds drew from education, psychology, nutritional anthropology, public planning and management, transportation planning, and landscape architecture. The researchers assembled during proposal development had experience in community-engaged research and expertise needed to lead the various strands of the study’s design.
4. Organizational Structure for Facilitating the CAST Partnership
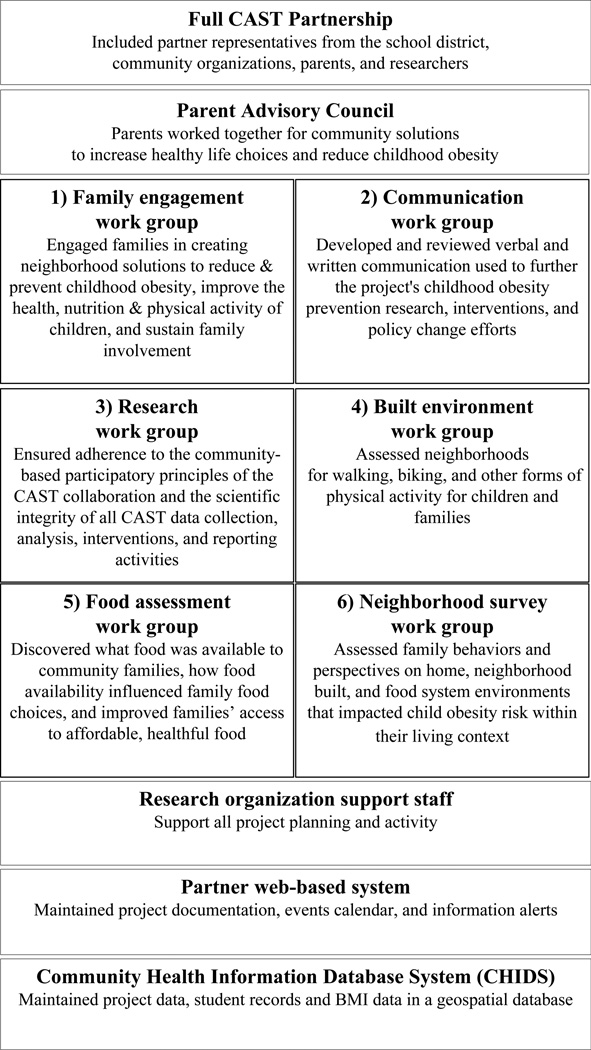
In order to manage multidimensional partner participation within the project, investigators drew from the literature on organizational learning15–18 to integrate a research work group structure that engaged the aforementioned communities in project processes (see Figure 2). The full CAST partnership convened once or twice annually to review CBPR processes, provide group decision-making opportunities, and examine updates on project accomplishments. The Parent Advisory Council met one evening monthly, was co-facilitated in English and Spanish, and provided a continuous forum for parent involvement in CAST. Six work groups (numbered in Figure 2) formed the core forum for project action. CAST partners participated in the various work groups and, thus, were involved in designing and conducting projects assessments, evaluating partner-led interventions, and designing the project’s family health program. The lead organization’s research staff team provided primary logistical support for the project, a project web-based information management system to support partner communication and information sharing, and the project’s Community Health Information Database System, which served as the repository for all project data.
Figure 2.
Operating Structure for Integrating Community-Based Participatory Research among the CAST Partnership
Facilitators of work groups were chosen consensually by group members and tended to be representatives from organizations involved in multiple work groups. Facilitators included a member of the partner school district, members of the study’s lead research organization, the GIS agency specialist who worked across all sectors of the project’s research, university graduate students with expertise in community-engaged pedestrian assessments, and the county Extension Service Director who had expertise in public communication and media campaigns. Each work group developed a mission statement, an annual set of project goals, and a summary of achievements from the previous year that were maintained as annual Work Group Descriptions. Work groups reported goals and accomplishments at full Partnership meetings. All project meetings were transcribed to maintain a written record of discussions, decisions, procedural developments, and accomplishments in the project (see Table 1). Partner agreements were negotiated annually to clarify member involvement in work groups, ancillary project work that partners wished to pursue (such as food preparation, intervention supports), and the fiscal reimbursements the project would make to partner organizations for time spent in meetings and activities.
Table 1.
CAST Partner Participation in Work Groups
| Organization | Area of Experience & Interest | Work Groups | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Parent Advisory Council |
Family Engagement |
Communication | Research | Built Environment |
Food Assessment |
Family Survey |
CHIDS, School Data |
||
| Bethel School District | Education and student health | Fa | Fa | ||||||
| Environmental Center of Sustainability | Agriculture and community development | ||||||||
| Lane Council of Governments | Geographical Information Systems (GIS) and public record data research | Fa | |||||||
| Lane County Food Policy Council | Food systems research, policy and interventions | ||||||||
| Lane Transit District-Point2Point | Public transportation & interventions | ||||||||
| Oregon Research Institute | Research and community interventions | Fa | fb | Fa | Fa | ||||
| Oregon State University Extension Services-Lane Co. | Nutrition education interventions | Fa | |||||||
| University of Oregon-PPPM | Active transport and built environment research and interventions | Fa | |||||||
| Willamette Farm and Food Coalition | Local farming, food system research and interventions | ||||||||
Note.
 Indicates workgroup participation by partner organization.
Indicates workgroup participation by partner organization.
F indicates that an organization partner member facilitates the work group meetings, planning, and task completion.
f indicates that an organizational partner member cofacilitates work group meetings, planning, and task completion.
5. Community Health-Related Assessments and Activities
5.1. Assessments
The CBPR process was informed by assessments of environmental influences on nutrition, physical activity, and health. Work groups guided specific community assessments in order to inform their discussions and contribute to the greater CAST project. Information gathered from the assessments was assembled into a community health database.
Assessments occurred at four levels in the project: child, family, neighborhood built environment, and community food environment. Children were recruited to participate in annual BMI assessments over the 5 years of the project or until they passed into middle school using a passive consent/opt-out system. Longitudinal child BMI results provided the key dependent variable used in the project’s environmental examination of obesity risk in the community. The family physical and social environment was assessed through an annual Neighborhood Family Survey, which asked parents to report on family food shopping practices, family eating practices, child and parent physical activity attitudes and behaviors, parent perspectives on neighborhood safety, built environment, social cohesion, and parent–family demographics. The neighborhood built environment was assessed by parents using mobile GIS-based tools to evaluate local street and intersection attributes for walking safety. Various community food environment audits were conducted by project partners to evaluate the availability of resources for residents to access healthful, affordable food.
Results from assessments were reported at biannual partner meetings, shared in school newsletters and made available to the public through the project’s website (https://cast.ori.org/, Research Results tab). Some results were immediately applicable to CAST project aims while others assisted partners in parallel organizational activities. For instance, the BMI assessment results were reported back to schools, but were also used to identify higher risk children for recruitment into the Family Health Program. The community–school mobilizing process in the neighborhood walkability environment assessment led to a successful 2-year Safe Routes to School (SRTS) grant application, retrofitted sidewalk infrastructure along an established residential street leading to an elementary school, and ongoing involvement of the district in regional SRTS planning and programming. Parent training on child pedestrian safety skills was also ultimately incorporated into CAST’s family-based health program.
5.2. Emergent Partner-Driven Activities
The CBPR partnership in CAST involved practice-based NGOs interested in advancing a broad range of experiments in school settings and the community. While these activities (described below) were not originally identified in the project’s grant application, they were extremely important to partner organizations as tangible actions in the collaboration that integrated specific interests and capacities of members.
The CAST collaboration took action in several areas. CAST partners piloted four additional activities that were aligned with their interests and concerns: (1) a Farm to School program that promoted purchasing of local produce for the district’s lunch program, cafeteria tasting tables, a featured locally grown fruit or vegetable of the month served on salad bars in all elementary schools, and farm field visits by second and third graders in three of the district elementary schools; (2) a fall and spring school garden program conducted in two of the lowest income schools; (3) a community growers’ market held over two summers at a community center, supported under the auspices of the neighborhood association and the city; and (4) a Trainer-in-Residence physical education program that was piloted in fourth and fifth grade classrooms and involved volunteer professional trainers from the local community presenting activity lessons in teacher-led physical education classrooms for a 6-week period, two sessions per week. All of these health programs continued beyond CAST, using pilot experiences and evaluations for ongoing program improvement and funding successes. There was reciprocity between partner organizations and the project that brought mutual development, recognition and support within the broader school and public sector.
5.3 Planned Project Health Program
The specific aims of the CAST proposal called for the development of a parent training program for child obesity prevention. The CAST Family Health Program was designed, piloted, and evaluated for feasibility during the latter 2 years of the project. The program was a multicultural, bilingual family education program that provided behavioral, skill-based health training to parents and their children in efforts to reduce community risk for child obesity. The program involved parent and child curricula taught over 10 weeks in 2-hour group sessions. Parent sessions were organized around positive parenting principles (eg, behavior monitoring, active communication, encouragement, goal setting, and problem solving) that were applied to nutrition planning and physical activity for families and children. Children (grades 2–5) attended parallel group sessions aimed at increasing age appropriate knowledge of heart health and obesity risk, reading menu labels, learning physical activity games for home and school, beginning gardening principles, and whole-food cooking.
The CAST Family Health Program used community-based procedures to design, staff, and host the program’s implementation in district schools. First, parent, school, and community members worked with the lead researcher in designing the parent and child curriculum. Second, local school and community professionals were integrated into staffing the program. A Physical Education Specialist in the district co-led classroom instruction for students and facilitated weekly physical activity sessions. A community fitness trainer conducted adult physical activity sessions. A juvenile detention catering service was contracted to deliver curriculum-related meals that fed parents and children each week while also introducing foods and recipes for parent menu planning. School nurses were hired on an hourly basis to conduct parent bio-screening assessments used in the curriculum and program’s evaluation. Nurses were able to explain bio-screening results to both English and Spanish speaking parents. The third community-based feature of the Family Health Program was housing the program for free in district elementary schools. This space provided a unique environment that was able to provide cafeterias for meals, instructional rooms appropriate for adults and children, age-appropriate child care space for infants and preschoolers, and gyms with equipment needed for physical activity.
6. Lessons Learned in the CAST CBPR Partnership
The CBPR partnership that grew out of CAST was shaped by five interacting factors: (1) the multiple communities involved in the project (eg, schools, parents, community organizations, and researchers), (2) the challenges and opportunities in managing partner-driven interventions that emerged through partner involvement, (3) the central and changing role of the school district during the study, (4) the dynamic nature of the CBPR partnership (eg, changes in partner organizations and project membership during CAST’s development), and (5) the coordinating role of researchers in initiating the conceptual design and facilitating the study’s research and intervention activities.
6.1. Lesson One: Overlapping yet diverging goals of multiple communities in a CBPR partnership can lead to community capacity building
CAST involved a large partnership that used multilevel approaches in structuring collaboration processes. These approaches, as discussed by Crisp and colleagues,19 included (1) top-down organizing through the lead researcher in identifying partner members and the research–intervention focus in the proposal; (2) bottom-up organizational development through the use of work group priority setting, intervention experimentation, and resource sharing in the project; and (3) partnership development in terms of formalizing new organizational relationships and groups (eg, the Parent Advisory Council), which determined consensual decisions in the study.
At a community-capacity building level, the CAST CBPR framework operated simultaneously within the school, family, NGO, and researcher communities to both strengthen and create relational networks. This multifaceted, multilevel research and activity approach developed a capacity for responding to emerging requests and opportunities to address obesogenic factors in the community. The project’s locally maintained health database allowed the partnership to join and relate information from different sources and share project activities and findings across the partnership and, ultimately, with the broader community.
For example, civic transportation leaders requested that the community-based walkability research conducted in CAST be presented to transportation engineers to provide data on parent perspectives on street network safety indicators. This dialogue helped to develop a clearer insight into the objective framework used by transportation planners in designing streetscapes for child active transport and the opportunities to include community perspectives in an ongoing regional transportation process. Later, county engineers presented a sidewalk infrastructure project to retrofit 1.5 miles of county roads adjacent to one of the project’s elementary schools. Many of the affected landowners were older and without children at home; their concern was the impact of the sidewalk on their privacy and loss of landscaping. Others residents were concerned over reduced parking and flow of traffic, especially at the beginning and end of the school day. These tensions had led engineers to suggest a design that minimized change but also created a narrow sidewalk with no buffer from traffic. The parent walkability study supported larger sidewalks divided from the road by a grass strip, especially due to the importance of the sidewalk for providing access to the school. The CAST work helped frame the discussion from the perspective of vulnerable groups, which also supported the needs of elderly residents, who generally supported sidewalks because it created a common-space for interacting with their neighbors.
6.2. Lesson Two: Partners” emergent activities can both stretch and enhance the project
An area of research not clearly anticipated in the project involved many of the partner- driven activities that were piloted and evaluated in through CAST. These emergent activities (eg, Farm to School program, community growers’ market, school garden program, and physical education Trainer-in-Residence program) required project resources for piloting and evaluation activities. Yet, they provided an opportunity to respond flexibly to (1) partner interests; (2) changing awareness in the schools and community for needed programs; and (3) availability of intervention programs that previously had not been developed, implemented, or evaluated in the partner school district. Supporting these programs allowed CAST to not only test the feasibility of new interventions but also to invest in the program and organizational development of partners while expanding the scope and content of the project’s research. For instance, CAST conducted an extensive examination of fourth and fifth grade student physical fitness in pre–post measures with the physical education Trainer-in-Residence program. This study provided the first fitness data on students collected in the school district and was integrated with CAST height–weight information on students and school academic achievement scores to support new grant applications and partner organizational growth in physical activity intervention.
The funding announcement by NIH, Community Participation in Research [R01: PA-07-283], supported research on health promotion, disease prevention, and health disparities that was jointly conducted by communities and researchers. This funding mechanism provided CAST the flexibility needed to respond to unanticipated and partner-determined directions that emerge naturally in CBPR projects, yet adhere to the broad aims and research design specified in the proposal.
6.3. Lesson Three: Schools and districts are naturally situated to participate in child obesity projects, but engagement and commitment of key personnel is essential
School district nurses were instrumental in initiating collaborative relationships between researchers and the school district for the CAST study. With their advocacy, the district superintendent agreed to explore collaborative grant applications. He connected researchers with an elementary school principal who served as a guide in developing preliminary data used as background for the project’s needs and development of the project’s work plan. These relationships not only honed insights into feasible processes for researcher–school collaboration but also demonstrated a readiness by the district for embarking on a project of this complexity.
Other school district administrators also became important agents in the researcher–community–school partnership as the project developed. Even though school nurses continued to assist in scheduling BMI annual assessments, administrators worked closely with researchers to (1) hire the project’s Community School Coordinator (a dually employed liaison between the school district and the lead research organization), (2) conduct annual passive consents with kindergarten and newly enrolled families in the district, (3) coordinate data sharing between the district’s electronic database and the project, (4) provide meeting and intervention space free of charge to the project, and (5) integrate project information in school newsletters and websites. District personnel also participated in CAST work groups and attended public forums where project data was discussed in the context of policy changes, such as the previously mentioned retrofitting of sidewalks in a school region. Additionally, the school district’s Food Service Director worked collaboratively with researchers and community partners to integrate Farm to School programming and locally grown produce in school meals.
6.4. Lesson Four: Participation of organizations grow and recede over time causing changes to core partnerships and influencing the direction of CBPR projects
The CAST CBPR process was dynamic and involved changing environments, organizations, and community priorities. The partnerships in the project changed in membership during the project, leading to both challenges and opportunities for the study.
During the tenure of CAST, school nurses developed a new community-supported school-based health center. While this effort limited their participation in project work group activity, a CAST researcher maintained relationships with nurses and volunteered planning support for the health center. By the time the CAST Family Health Program was ready to be implemented, the district’s new school health center became a resource for providing bio-screening measures to parents in the program. This project connection supported the mission of the newly formed health center, developed functioning practitioner relationships between nurses, parents, and the district on family and child health, and provided the project a dependable resource for sensitive physical assessments in its health program.
Researchers and school nurses were also able to collaborate on a grant application to support ongoing BMI assessment in the schools as an independently operated program through the school-based health center. These scenarios illustrated the flexibility of CBPR to accommodate evolution and change in the dynamics of the research–school partnership. The development process fostered a unique opportunity for synergy and alignment between the project and newly formed health organization. A more fixed research design in CAST would not have been able to support emergent activities and capacities for more complex collaboration in program initiation between the district and project.
Other organizational changes also impacted the project’s membership. One NGO was in its initial phases of development when CAST began and determined that it was in its best interest to leave the collaboration and focus on its own start-up priorities. Another large organization, a university-based extension program, lost its county funding during the project and had to significantly curtail its participation in the study. This particularly impacted the development and implementation of the Family Health Program, which had been planned to rely heavily on this community organization for design and operations. However, other community members were identified to help design and implement the program. The result was a family-based program that was more strongly integrated with school and community resources than was originally envisioned by researchers. This experience showed how CBPR projects could be vulnerable to changes in partnerships; however, the collaborative structure enabled resilience and flexibility to adjust to such changes.
6.5. Lesson Five: Complex societal problems require CBPR approaches that necessitate significant coordination by researchers
The research design of CAST represented a hybrid approach to CBPR that involved a pre-established, investigator-initiated research design. CAST relied on work group members to develop the content of surveys, provide interpretation of preliminary findings, and assist in developing piloted interventions. In perhaps a purer CBPR project model12 the research design would have been more exploratory and iterative in its development. However, developing a comprehensive understanding of the multiple levels of influence in local child obesity was felt by researchers to require an a priori organization of a work plan that could be collaboratively refined and developed—itself an experiment in a project of this study’s complexity.
Extensive researcher leadership was necessary to develop and implement the iterative phases of the project, and the CBPR collaboration could not have achieved benchmark accomplishments without this guidance, expertise, and logistical support. The core leadership of the academic researchers in CAST was responsible for locating partner members and organizations and integrating this diverse membership into an ongoing yet evolving work group structure. This leadership also provided the project glue that held together a coalition of shifting members, where a lack of leadership might have caused parts of the partnership to drift off course from project objectives or scatter with a lack of direction and organizing processes over the duration of the project.
It became the continuous responsibility of the primary investigator to ensure that the research agenda of the project remained embedded within the purview of the project’s multiple community membership and reflected these diverse values, inputs, and priorities for action. For instance, the Parent Advisory Council expressed consistent concern over discrepancies between schools regarding child recess opportunities and lunch room policies. Researchers responded to this feedback by helping the council design an observation protocol of the school environment that operationalized their expressed concerns and aligned with observational research standards and the literature on school wellness environments. Harmonizing the broad demands of the study with the constituent communities was a consistent focus and tension in the project. The sensitivities of researchers to these demands on the science required consistent self-examination and discussion.
At the same time, the partnership also served as a critical learning resource for academic researchers. Partners (a) provided an iterative and in-depth level of discussion through work groups that helped refine investigator understanding and responses to local health problems; (b) helped guide the design of information gathering and activities with input from multiple, often typically unheard, perspectives (eg, low-income or Spanish speaking parents, or members of small community-based NGOs); (c) connected community members at a systemic level to better influence power structures that determined health change efforts within the community; and (d) helped the provide immediate benefits from research results in developing locally generated information to support the health goals of the organizations, schools, and communities participating in the study.
7. Conclusions
This CAST study extends prior research on the use of CBPR in child obesity projects by examining the experiences encountered while developing a multilevel CBPR model integrating researchers, a school district, and community stakeholders. The CAST project’s experiences with the shifting stakeholder involvement, emerging opportunities for unplanned partner-driven activities, and advocacy in the community are applicable for projects focusing on school-based health programs as well as other multilevel programs and projects.
CAST was a hybrid approach to CBPR that involved a pre-established, investigator-initiated research design. This is a form of CBPR that is often ignored in the CBPR literature—perhaps because it is seen as somewhat controversial, and/or inherently contradictory to the rationale for and tradition of CBPR. Yet such an approach provides an alternative model for organizing and integrating communities into the processes of locally based research science and health promotion. The CAST project, including all its challenges, illustrates that an investigator-initiated project is able to adhere to the important tenants of CBPR while also creating momentum, structure, and leadership in organizing multiple communities in working toward a community-based health promoting partnership.
Additionally, this work highlights the issue that the success of a CBPR initiative is not always captured with standard research methodologies.20,21 The reality for CBPR is that project change is inevitable. Not all community-based organizations or researchers will flourish within a research context that requires consistent adjustment to changing circumstances and initiatives within a community. Ultimately, however, the CAST experience illustrates the synergy that can develop and propel project activities that are holistically linked to the assets and needs of a community.
This CAST study extends prior research on the use of CBPR in child obesity projects examining the experiences encountered while developing a multilevel CBPR model integrating researchers, a school district, and community stakeholders. The CAST project’s experiences with the shifting stakeholder involvement, emerging opportunities for unplanned partner-driven activities, and advocacy in the community are applicable for projects focusing on school-based health programs as well as other multilevel programs and projects.
Acknowledgments
We are very grateful to the National Institute of Child Health and Human Development at the National Institutes of Health, grant R01 HD05783, that has financially supported and enabled us to complete the study. We also would like to thank Mr. Colt Gill, Superintendent, Dr. Drew Braun, Director of Instruction, Ms. Nichole Zwink, Adaptive Physical Education Specialist, Ms. Nola Colvin, Adaptive Physical Education Specialist, Ms. Annemarie Hirsch, District Nurse, Sherine Forrest, District Nurse, and Ms. Jennie Kolpak, Food Service Director, with Bethel School District 52; Dr. Marc Schlossberg, Associate Professor and Co-Director of the Sustainable Cities Initiative at the University of Oregon; Mr. David Richey, GIS Specialist at Lane Council of Governments; Ms. Lisa Van Winkle, Smart Ways to School Project Lead at Lane Transit District; Beatriz Robles Kieser, Director of CrossCulturalNow; Kate Hammarback, Coordinator of the 4-H Program, Lane County Extension Services; Lynne Fessenden, Executive Director, and Megan Kemple, Director, of the Farm to School Program of the Willamette, Farm and Food Coalition; and Aleta Miller, Executive Director of the Environmental Center of Sustainability and Co-Chair of the Active Bethel Citizen’s Neighborhood Association. Finally, we owe a great deal of gratitude to CAST Parent Advisory Council parents, other community partners, and Oregon Research Institute staff for guiding and supporting all the phases of research and activity completed in the study.
Contributor Information
Deb Johnson-Shelton, Oregon Research Institute.
Geraldine Moreno-Black, Email: geraldin@ori.org, Oregon Research Institute.
Cody Evers, Email: codye@ori.org, Oregon Research Institute.
Nicole Zwink, Email: nicole.zwink@bethel.k12.or.us, Bethel School District 52, Eugene, Oregon.
References
- 1.Ogden C, Carroll M. NCHS Health E-Stat: Prevalence of obesity among children and adolescents: United States, trends 1963–1965 through 2007–2008. 2010 Available from: http://www.cdc.gov/nchs/data/hestat/obesity_child_07_08/obesity_child_07_08.htm.
- 2.Contaldo F, Pasanisi F. Obesity epidemics: secular trend or globalization consequence? Beyond the interaction between genetic and environmental factors. Clin Nutr. 2004;23:289–291. doi: 10.1016/j.clnu.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 3.Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nutr Rev. 1997;55:31–43. doi: 10.1111/j.1753-4887.1997.tb01593.x. [DOI] [PubMed] [Google Scholar]
- 4.Swinburn BA, Walter L, Ricketts H, Whitlock G, Law B, Norton R. The determinants of fat intake in a multi-ethnic New Zealand population. Fletcher Challenge—University of Auckland Heart and Health Study Management Committee. Int J Epidemiol. 1998;27:416–421. doi: 10.1093/ije/27.3.416. http://ije.oxfordjournals.org/ [DOI] [PubMed] [Google Scholar]
- 5.Ulijaszek S, Lofink H. Obesity in biocultural perspective. Annu Review Anthropol. 2006;35:337–360. [Google Scholar]
- 6.Huang TT, Drewnowski A, Kumanyika SK, Glass TA. A systems-oriented multilevel framework for addressing obesity in the 21st century. Prev Chronic Dis. 2009;6(3):A82. Available from: http://www.cdc.gov/pcd/issues/2009/jul/09_0013.htm. [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine of the National Academies. Does the built environment influence physical activity? Examining the evidence–Special Report 282. 2005 Available from: http://www.iom.edu/CMS/3793/15724/24476.aspx. [Google Scholar]
- 8.Institute of Medicine of the National Academies. Progress in preventing childhood obesity: focus on industry–brief summary: Institute of Medicine regional symposium. 2006 Available from: http://www.iom.edu/CMS/3788/25044/34007.aspx. [Google Scholar]
- 9.Glasgow RE, Green LW, Taylor MV, Stange KC. An evidence integration triangle for aligning science with policy and practice. Am J Prev Med. 2012;42:646–654. doi: 10.1016/j.amepre.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Northway R. Participatory research. Part 1: key features and underlying philosophy. Int J Ther Rehabil. 2010;17:174–179. [Google Scholar]
- 11.Plumb M, Price W, Kavanaugh-Lynch M. Funding community-based participatory research: lessons learned. J Interprof Care. 2004;18:428–439. doi: 10.1080/13561820400011792. [DOI] [PubMed] [Google Scholar]
- 12.Viswanathan M, Ammerman A, Eng E, Gartlehner G, Lohr KN, Griffith D, Rhodes S, Samuel-Hodge C, Maty S, Lux L, Webb L, Sutton SF, Swinson T, Jackman A, Whitener L. Evidence Report/Technology Assessment No. 99. Rockville, MD: Agency for Healthcare Research and Quality; 2004. Jul, Community-based participatory research: assessing the evidence. (Prepared by RTI–University of North Carolina Evidence-based Practice Center under Contract No. 290-02-0016). AHRQ Publication 04-E022-2. Available from: http://archive.ahrq.gov/downloads/pub/evidence/pdf/cbpr/cbpr.pdf. [PMC free article] [PubMed] [Google Scholar]
- 13.Cornwall A, Jewkes R. What is participatory research? Soc Sci Med. 1995;41:1667–1676. doi: 10.1016/0277-9536(95)00127-s. [DOI] [PubMed] [Google Scholar]
- 14.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Publ Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 15.Senge PM, Kleiner A, Roberts C, Ross RB, Smith BJ. The fifth discipline fieldbook: strategies and tools for building a learning organization. New York: Doubleday/Currency; 1994. [Google Scholar]
- 16.Senge PM. The fifth discipline: the art and practice of the learning organization. New York: Doubleday/Currency; 2006. Revised. [Google Scholar]
- 17.Argyris C, Schön DA. Organizational learning: a theory of action perspective. Reading, MA: Addison-Wesley; 1978. [Google Scholar]
- 18.Argyris C. On organizational learning. 2nd. Malden, MA: Blackwell Business; 1999. [Google Scholar]
- 19.Crisp BR, Swerissen H, Duckett SJ. Four approaches to capacity building in health: consequences for measurement and accountability. Health Promot Int. 2000;15:99–107. [Google Scholar]
- 20.Economos CD, Irish-Hauser S. Community interventions: a brief overview and their application to the obesity epidemic. J Law Med Ethics. 2007;35:131–137. doi: 10.1111/j.1748-720X.2007.00117.x. [DOI] [PubMed] [Google Scholar]
- 21.Uyeda K, Bogart LM, Hawes-Dawson J, Schuster MA. Development and implementation of a school-based obesity prevention intervention: lessons learned from community-based participatory research. Prog Community Health Partnersh. 2009;3:249–255. doi: 10.1353/cpr.0.0085. [DOI] [PMC free article] [PubMed] [Google Scholar]