Summary
Background
Penile involvement is a rare, self-limiting, benign genital condition. In Mondor’s disease the underlying pathology is thrombophlebitis of a superficial vein.
Case Report
In this case report, we want to present a rare Penile Mondor’s disease with literature review.
Conclusions
While the diagnosis can be based on history, physical examination and Doppler ultrasound, the necessity of both MRI, MR angiography and intracavernosal vasoactive agent administration can be questioned. Both MRI and intravenous vasoactive agent administration may be helpful in suspicious cases for differential diagnosis and to eliminate other etiologies like pelvic mass or thrombosis.
MeSH Keywords: Magnetic Resonance Imaging; Penile Diseases; Penis; Ultrasonography, Doppler
Background
Penile involvement is a rare, self-limiting, benign genital condition. In Mondor’s disease the underlying pathology is thrombophlebitis of a superficial vein. Diagnosis is usually made by physical examination but Doppler ultrasound and Magnetic Resonance Imaging (MRI) may be helpful [1,2]. In this case report, we want to present a rare Penile Mondor’s disease with literature review.
Case Report
A 35-year-old male presented with swelling and tenderness on the dorsal side of the penis. He had experienced this lesion for two weeks. There was no evidence of penile discharge, erectile dysfunction or dysuria. There was no history of trauma, vigorous sexual activity or predisposition to thrombosis. On examination a cord-like lesion was palpated around the coronal sulcus extending to the dorsal aspect of the proximal penis. Tenderness and mild skin erythema were found as well. There was no lymphadenopathy in the inguinal region. His blood cell count and biochemical test results were normal.
On Doppler ultrasound a cord-like 0.6-cm in diameter and 1.7-cm in length non-compressible lesion containing internal echogenicity with no color filling and flow spectrum around the coronal sulcus was detected. Doppler ultrasound of cavernosal arteries and veins were normal and the administration of vasoactive agent was thought to be unnecessary.
On MRI a cord-like lesion, isointense on T1-weighted images and hyperintense on T2-weighted images without contrast enhancement around the coronal sulcus extending to the dorsal aspect of the penis was detected (Figure 1). There was perilesional heterogenicity suggesting edema. There was no lymphadenopathy in the inguinal region. No pelvic mass or thrombosis was detected.
Figure 1.
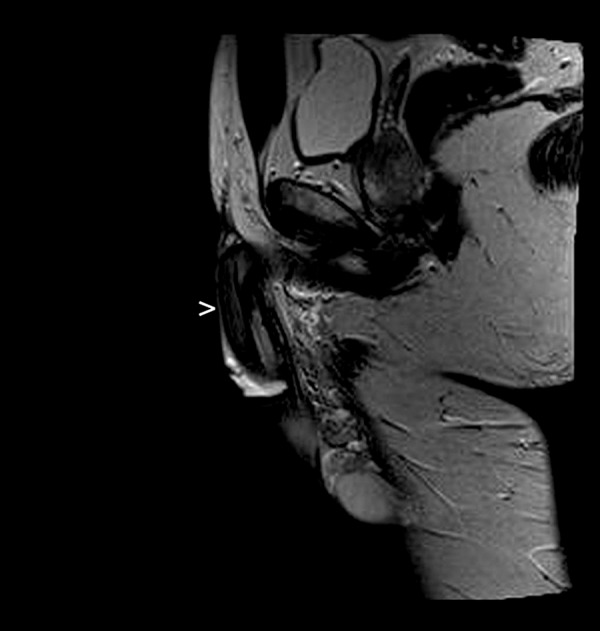
A sagittal T1-weighted magnetic resonance image of the penis (white arrowhead indicates isointense thrombophlebitis).
The diagnosis indicated superficial dorsal vein thrombophlebitis, Mondor’s disease. After administration of an oral corticosteroid his complaints improved and the lesion disappeared on physical examination. Also, venous flow returned on Doppler ultrasound.
Discussion
Mondor’s disease is a form of superficial thrombophlebitis that involves the lateral thoracic, thoracoepigastric or superior epigastric veins especially in women [3]. It was first defined by Henri Mondor in 1939. In 1955 Braun-Falco described dorsal phlebitis of the penis in the context of generalized phlebitis and in 1958 Helm and Hodge defined isolated penile involvement as Penile Mondor’s disease [4]. Penile involvement is an unusual, self-limiting, benign and under-recognized form of the disease which affects sexually active men with no specific etiology [4]. A total of 55 articles were found in the literature about penile Mondor’s disease and 51 of them were devoted to it.
Patients presented with a palpable thick cord-like structure extending to the dorsum of the penis, accompanied by tenderness and skin erythema. The etiology of the disease is usually unknown but various factors like trauma, excessive and prolonged sexual activity, prolonged sexual abstinence, local or distant infection, history of sexually transmitted disease, use of intracavernouse drugs, use of vacuum, thrombophilia, inguinal hernia operation, orchiopexy, varicoselectomy, Behçet’s disease, body building exercises, pelvic tumors, paraneoplastic syndromes, filled bladder causing venous occlusion, intravenous drug abuse and tendency for thrombosis were mentioned [5,6].
Diagnosis is usually made based on history and physical examination. The role of imagining in Mondor’s disease is to identify the intravascular thrombus [2]. Gigli et al. reported that grey scale and Doppler ultrasound can be useful in case of diagnostic uncertainty, to detect the extent of thrombosis and to follow up [7]. Moreover, Ozturk reported that Doppler ultrasound may have an important role in differential diagnosis especially to distinguish between non-venerial sclerosing lymphangitis of the penis and Mondor’s disease [4]. Cases diagnosed with MR angiography were reported on [2] but its necessity is still controversial [4].
On Doppler ultrasound, tube-like lesions with no color filling and no venous flow are expected, like in our case. But these findings were evaluated insufficient by Hye Yeon Han et al. who described cavernosal artery flow signal pattern of low peak systolic velocity and high resistance in their case report, suggesting further analyses in larger populations [1]. Also, return of blood flow after treatment on follow-up Doppler ultrasound supports the diagnosis like in our cases.
Berto et al. reported that MRI T1-weighted spin echo and T2-weighted spin echo sequence combination shows thrombosed vessels optimally, like in our case. Additionally, MR angiography elaborates detecting and showing the extension of a thrombosed vessel [2]. MRI may also provide more information about the cause of the disease, like pelvic mass or thrombosis. Signal intensity of the thrombus depends on the time delay between the onset of thrombosis and imaging. In acute stage (0–5 days) the signal intensity of the vessel is isointense on T1- and hyperintense on T2-weighted images, in subacute stage (5–15 days) the signal is hyperintense in both T1- and T2-weighted images. In chronic stage (after 15 days) the signal becomes isointense on T1- and iso-hyperintense on T2-weighted images like in our case.
Conclusions
While the diagnosis can be made based on history, physical examination and Doppler ultrasound appropriately, the necessity of both MRI, MR angiography and intracavernosal vasoactive agent administration can be questioned [1,4]. Both MRI and intravenous vasoactive agent administration may be helpful in suspicious cases for differential diagnosis and to eliminate other etiologies like pelvic mass or thrombosis.
Footnotes
Conflict of interest
There is no conflict of interest concerning this manuscript.
References
- 1.Han HY, Chung DJ, Kim KW, Hwang CM. Pulsed and color Doppler sonographic findings of penile Mondor’s disease. Korean J Radiol. 2008;9:179–81. doi: 10.3348/kjr.2008.9.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boscolo-Berto R, Iafrate M, Casarrubea G, Ficarra V. Magnetic resonance angiography findings of penile Mondor’s disease. J Magn Reson Imaging. 2009;30:407–10. doi: 10.1002/jmri.21857. [DOI] [PubMed] [Google Scholar]
- 3.Kondo T. Traumatic funicular phlebitis of the thoracic wall resembling Mondor’s disease: a case report. J Med Case Rep. 2011;5:127. doi: 10.1186/1752-1947-5-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Öztürk H. Penile Mondor’s disease. Basic Clin Androl. 2014;24:5. doi: 10.1186/2051-4190-24-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Griger DT, Angelo TE, Grisier DB. Penile Mondor’s disease in a 22-year-old man. J Am Osteopath Assoc. 2001;101:235–37. [PubMed] [Google Scholar]
- 6.Zor M, Tahmaz L, Başal Ş, et al. Otuz iki yaşında olguda penil mondor hastalığı. Turkiye Klinikleri Journal of Medical Sciences. 2009;29:1751–53. [in Turkish] [Google Scholar]
- 7.Gigli F, Beltrami P, Arancio M, Zattoni F. Mondor’s penile disease: personal experience. J Androl Sciences [Internet] 2008:15. [Google Scholar]


