Abstract
Background
To treat moderate to severe acne vulgaris, we developed an optical fiber imported intra-tissue photodynamic therapy: the optical fiber irradiation 5-aminolevulinic acid photodynamic therapy (OFI-ALA-PDT). The aim of this study was to compare the treatment effect and tolerability of OFI-ALA-PDT versus traditional ALA-PDT in the treatment of moderate to severe acne vulgaris.
Material/Methods
60 patients with facial acne enrolled into this study were randomly divided into an OFI-ALA-PDT group and a traditional ALA-PDT group, with 30 patients in each group. The difference between these 2 groups was the red light irradiation methods used. In the OFI-ALA-PDT group we used intra-tissue irradiation (import the red light directly into the target lesion with optical fiber) for 5 min, while the traditional ALA-PDT group received whole-face irradiation for 20 min. All patients received 1 irradiation every 7 to 10 days for a total of 6 irradiations. Treatment effects and adverse reactions were recorded after the 4th and 6th irradiation, and at 4, 8, 16 weeks after the entire treatment.
Results
After the 4th irradiation, significantly different effective rates were observed in these groups (90.0% for the OFI-ALA-PDT group and 66.7% for the control group). However, no significant difference in effective rate was recorded in the later observations. There were 182 adverse reactions in the OFI-ALA-PDT group and 497 in the control group, which showed a significant difference (P<0.05).
Conclusions
OFI-ALA-PDT showed improved treatment effective rate in the early stage of irradiation, and it had fewer adverse reactions.
MeSH Keywords: Acne Vulgaris, Aminolevulinic Acid, Photochemotherapy
Background
Acne vulgaris is a common skin disease of great cosmetic concern to young people. Propionibacterium acnes and sebum secretion are the main contributors to acne pathogenesis.
The recommended treatments for acne include topical medications and systemic use of antibiotics, hormones, and retinoids, according to severity [1]. Tretinoin or isotretinoin is very effective for the treatment of intractable acne but its use has been limited due to the potential for teratogenicity [2].
Topical photodynamic therapy (PDT) with topical application of sensitizers in the treatment of different kinds of skin diseases is of increasing research interest. PDT is based on the activation of light-sensitive molecules (photosensitizers) to cause cell death by producing cytotoxic oxygen radicals. 5-aminolevulinic acid (ALA) is frequently used in topical PDT because it is converted into protoporphyrin (PpIX), an extremely active photosensitizer, upon irradiation with red light [3]. Recent studies have suggested that ALA-PDT is also effective in treatment of acne vulgaris [1,4].
With the increasing use of ALA-PDT for patients with acne vulgaris, adverse effects have increased, including pain, burning sensation, itching, prickling, erythema, edema, pustules, acneiform eruption, and excoriations [5–7], with causes related to the concentration of photosensitizer, the energy of light, and skin conditions of patients. The inaccuracy of whole-face irradiation is also an important reason. Therefore, we studied an optical fiber intra-tissue irradiation 5-aminolevulinic acid photodynamic therapy (OFI-ALA-PDT) in the treatment of moderate to severe acne in patients treated in our department from January 2014 to June 2015.
Material and Methods
Patients
Patient inclusion criteria were according to the diagnosis and classification in the Cunkuffe classification method [8]. These classifications areas are: light (mainly whiteheads and blackheads), medium (mainly inflammatory papules and pustules), and severe (inflammatory papules, nodules, and inflammatory cysts). Exclusion criteria were: (1) internal or external use of antibiotics within the last 4 weeks; (2) systemic use of a retinoid in the last 6 months; (3) photosensitive or keloid history; (4) pregnant or liver function unusual; (5) cannot complete the course; (6) staff directly participating in the study; and (7) participants currently in other clinical studies or who participated in another study within the last 3 months. The study was upon the approval of the hospital ethics committee and all the patients signed informed consent.
These 60 patients with moderate to severe acne were treated from January 2014 to June 2015 in our dermatology department. Rash was limited to the face, and the main symptoms were inflammatory papules, pustules, nodules, and cysts, with different degrees of pigmentation and scarring. Patients were randomly divided into 2 groups, with 30 patients in each. The treatment group (OFI-ALA-PDT) included 12 males and 18 females, aged 12–44 years, with an average of 26.8±5.2 years; the course of disease ranged from 3 to 120 months with an average of 30 months, with no drop-outs. In the control group, there were 16 males and 14 females, aged 15–42 years with an average of 27.3±4.8 years; the course of disease ranged from 4 to 108 months, with an average of 33 months, with no drop-outs. No significant differences were observed between the 2 groups in sex, age, or course of disease (P>0.05).
Treatment
In the treatment group (OFI-ALA-PDT) (Figure 1), 3.6% aminolevulinic acid was evenly applied to the rashes and the surrounding 0.5 to 1.0 cm of normal skin. After 1.5 h of incubation shielded from light, we wiped off the remaining photosensitizer, disinfected, inserted disposable optical fiber needles into the skin lesions with inflammatory papules and nodules, and imported the red light irradiation to the tissues located 3 mm below the follicular orifice (including the sebaceous glands) for 5 min. We used 633±3 nm wave length. For irradiation, a dose of 4.5 J/cm2 (dose at skin, detected by a VLP-200 laser power meter, Changchun Feimiao Tech., Ltd) was given for the first time (this dose was based on our previous data in an animal model, data not shown), and was adjusted to 3–24 J/cm2 in the following irradiations according to adverse reactions. Dark glasses were used to protect patients’ eyes during irradiation. The skin was sterilized again after irradiation and avoided strong light for 3 days. Irradiations were carried out every 7–10 days, and each patient received 6 irradiations in total. In the control group, the traditional skin surface irradiation was used. For irradiation, a dose of 54 J/cm2 at skin was used with a fixed-power density of 45 mW/cm2 for 20 min, and the distance between the light panel and patient’s apex nasi was set at 10 cm. The treatment was repeated every 7 to 10 days for 6 consecutive sessions.
Figure 1.
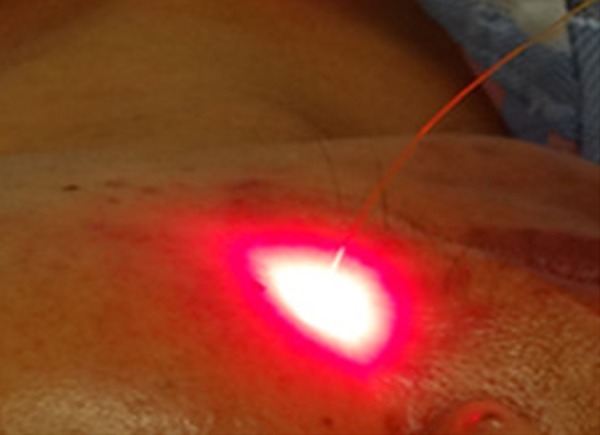
Illustration of intra-tissue OFI-ALA-PDT. The red light was imported directly into the target lesion with optical fiber.
Evaluation
Effective criteria [9] were the number of skin lesions and curative effect as recorded and judged by the same dermatologist.
“Cure” was 90% or more of the skin lesions disappeared; “remarkably effective” was 60% to 89% of the skin lesions disappeared; “effective” was 20% to 59% of skin lesions disappeared; and “invalid” was less than 20% of skin lesions disappeared. Effective rate was the percentage of cured cases plus remarkable cases divided by the total cases.
Treatment effects and adverse reactions were recorded during each treatment, before the next treatment and in the subsequent follow-up period. These adverse reactions include itching, pain, pustules, blisters, edematous erythema, pigmentation, reactive acne, and desquamation. We recorded the appearing and fading away time, severity, and actions used to combat these adverse reactions. Follow-up was performed at 4, 8, and 16 weeks after the last irradiation.
Statistics
SPSS17.0 software was used for statistical analyses. The chi-square test was used to compare different groups and the rank-sum test was used to compare adverse reactions between groups, age, and disease courses. P<0.05 was considered as statistically significant.
Results
Effective rate
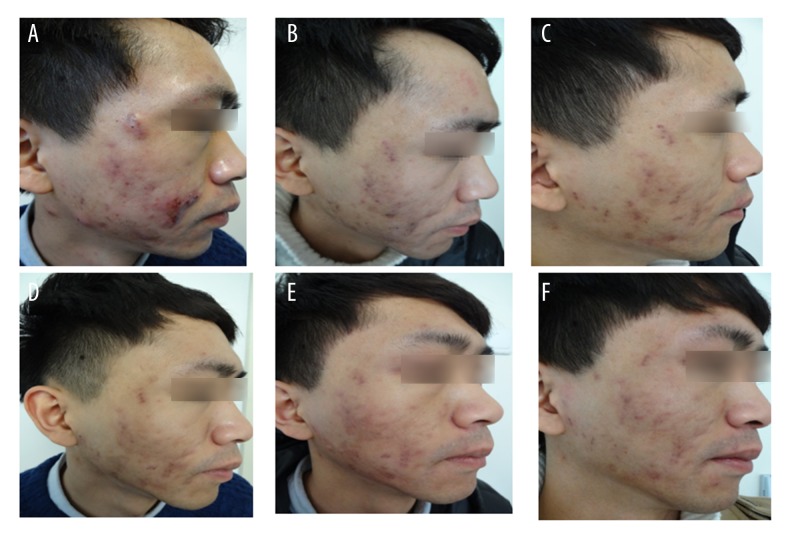
The treatment results are shown in Figure 2. By the end of the 4th irradiation, the effective rate of the OFI-ALA-PDT group was 90%, which is significantly higher than the control group’s 66.7% (χ2=4.812, P<0.05). However, there was no significant difference between these groups when all the 6 irradiations were finished (93.3% in the treatment versus 90% in the controls) (Table 1). Furthermore, follow-up at 4, 8, and 16 weeks after all the treatment showed no improvement in the OFI-ALA-PDT group (Table 1).
Figure 2.
Clinical photographs from a patient treated with OFI-ALA-PDT. (A) Before treatment. (B, C) After the fourth and sixth treatment. (D–F) Follow up at week 4, 8, 16.
Table 1.
Comparation of the therapeutic effect between the OFI-ALA-PDT and the control group during the treatment and follow-up.
| Detection time | Groups | Therapeutic effect | Effective rate (%) | χ2 | |||
|---|---|---|---|---|---|---|---|
| Cure | Remarkable effective | Effective | Invalid | ||||
| The 4th treatment | OFI-ALA-PDT | 18 | 9 | 3 | 0 | 90.0 | 4.812 |
| Control | 12 | 8 | 8 | 2 | 66.7 | ||
| The 6th treatment | OFI-ALA-PDT | 22 | 6 | 2 | 0 | 93.3 | 0.218 |
| Control | 19 | 8 | 3 | 0 | 90.0 | ||
| 4th week follow-up | OFI-ALA-PDT | 21 | 7 | 2 | 0 | 93.3 | 0.741 |
| Control | 19 | 7 | 4 | 0 | 86.7 | ||
| 8th week follow-up | OFI-ALA-PDT | 19 | 8 | 2 | 1 | 90.0 | 0.162 |
| Control | 16 | 10 | 4 | 0 | 86.7 | ||
| 16th week follow-up | OFI-ALA-PDT | 18 | 8 | 2 | 2 | 86.7 | 0.131 |
| Control | 15 | 10 | 4 | 1 | 83.3 | ||
Adverse reactions
There were 84 adverse reactions recorded in the OFI-ALA-PDT group during treatment, which is significantly less than the 242 recorded in the control group (Table 2). After the treatment, there are 98 adverse reactions in the treatment group and 255 in the control group (Table 2). Overall, 182 adverse reactions in the OFI-ALA-PDT group and 497 in the control group were recorded, indicating that OFI-ALA-PDT treatment performed better in decreasing the number of adverse reactions (P<0.01).
Table 2.
Comparation of the adverse effect between the OFI-ALA-PDT and the control group.
| During treatment | Follow-up | |
|---|---|---|
| Control | 242* | 255 |
| OFI-ALA-PDT | 84 | 98 |
| Comparation | Z=−11.399, P<0.01 | Z=−11.629, P<0.01 |
The adverse effect was measured as times.
Discussion
Acne is a common disease of dermatology. The clinical treatment for moderate to severe acne has mainly focussed on the systematic usage of antibiotics and retinoids. However, this kind of treatment is limited due its obvious adverse effects. In recent years, a large number of studies have confirmed that ALA-PDT by red light is a highly effective treatment for acne [10–14]. Unfortunately, with the extensive use of ALA-PDT, more and more adverse effects had been reported. Almost all photodynamic therapy patients experience various ranges of adverse reactions, including moderate to severe pain, erythema, pustules, and peeling [15]. The presently known factors affecting photodynamic therapy efficiency and safety include the concentration of photosensitizer, photosensitizer packet time, photosensitizer type, light type, and light parameters. The conventional method used to reduce adverse reactions is to avoid light and sunshine, and cold spray or cold repair facial mask after photodynamic therapy, but the effect is limited. Some new strategies were reported to reduce the adverse effects. One study used different concentrations of ALA for the treatment and found that the higher concentration was related to improved curative effect but caused severe adverse reactions [16]. Some studies reduced the ALA packet time from a few hours to 1 hour and observed low incidence of adverse reactions, especially in the case of pigmentation, but its curative effect is reduced to a certain degree [14,17,18]. At the same time, the use of new photosensitizers is also a popular research topic. Jang introduced new photosensitizers (indocyanine green and indole-3-acetic acid) in photodynamic therapy for acne. The study achieved a good effect, and only produced slight erythema (6/34) and pruritus (8/34) after each irradiation, which resolved within a few hours [19].
However, to date there have been no reports about methods of light irradiation. The photodynamic approach currently used in the ALA-PDT uses the external exposure mode. In this mode, to get to the hair follicle sebaceous glands, the red light has to penetrate the skin epidermis layer. However, this is bound to increase the light attenuation, and the epidermis layer may absorb more light, leading to local adverse effects. On the other hand, the hair follicle sebaceous glands would absorb less energy and the effect would be limited. Therefore, to address this problem, we used disposable optical fiber needles to penetrate the skin 3 mm to import the red light into subcutaneous layers of the target site. This method was expected to achieve accurate, minimally invasive, targeted therapy in the tissues and reduce damage to the normal skin surrounding the lesions, so it can alleviate the related adverse effects. To determine whether this irradiation method could improve the therapeutic effects, the traditional red light external exposure photodynamic therapy was included as a control. As expected, by the end of the 4th irradiation, the effective rate of the OFI-ALA-PDT group reached 90%, which is significantly higher than the 66.7% achieved in the control group (χ2=4.812, P<0.05). However, no improvement was observed in the later irradiations. These results indicate the OFI-ALA-PDT contributed to the effective rate in the early stage of irradiation but did not help the long-time therapy. Moreover, 182 adverse reactions in the OFI-ALA-PDT group and 497 in the control group were recorded, indicating that OFI-ALA-PDT treatment performed better in decreasing the adverse reactions (P<0.01).
Conclusions
Overall, the OFI-ALA-PDT treatment developed in this study showed improved treatment effective rate in the early stage of irradiation and fewer adverse reactions.
Footnotes
Source of support: This work was supported by the Fund for Scientific and Technological Transformation of Sichuan Province (14010134)
References
- 1.van de Kerkhof PC, Kleinpenning MM, de Jong EM, et al. Current and future treatment options for acne. J Dermatolog Treat. 2006;17(4):198–204. doi: 10.1080/09546630600830596. [DOI] [PubMed] [Google Scholar]
- 2.Holmes SC, Bankowska U, Mackie RM. The prescription of isotretinoin to women: is every precaution taken? Br J Dermatol. 1998;138(3):450–55. doi: 10.1046/j.1365-2133.1998.02123.x. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy JC, Pottier RH. Endogenous protoporphyrin IX, a clinically useful photosensitizer for photodynamic therapy. J Photochem Photobiol B. 1992;14(4):275–92. doi: 10.1016/1011-1344(92)85108-7. [DOI] [PubMed] [Google Scholar]
- 4.Hongcharu W, Taylor CR, Chang Y, et al. Topical ALA-photodynamic therapy for the treatment of acne vulgaris. J Invest Dermatol. 2000;115(2):183–92. doi: 10.1046/j.1523-1747.2000.00046.x. [DOI] [PubMed] [Google Scholar]
- 5.Ko DY, Kim KH, Song KH. Comparative study of photodynamic therapy with topical methyl aminolevulinate versus 5-aminolevulinic acid for facial actinic keratosis with long-term follow-up. Ann Dermatol. 2014;26(3):321–31. doi: 10.5021/ad.2014.26.3.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yin R, Lin L, Xiao Y, et al. Combination ALA-PDT and ablative fractional Er: YAG laser (2,940 nm) on the treatment of severe acne. Lasers Surg Med. 2014;46(3):165–72. doi: 10.1002/lsm.22219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaves YN, Torezan LA, Niwa AB, et al. Pain in photodynamic therapy: mechanism of action and management strategies. An Bras Dermatol. 2012;87(4):521–26. doi: 10.1590/s0365-05962012000400001. quiz 527–29. [DOI] [PubMed] [Google Scholar]
- 8.Cunliffe WJ, Goulden V. Phototherapy and acne vulgaris. Br J Dermatol. 2000;142(5):855–56. doi: 10.1046/j.1365-2133.2000.03528.x. [DOI] [PubMed] [Google Scholar]
- 9.Shalita AR, Berson DS, Thiboutot DM, et al. Effects of tazarotene 0.1% cream in the treatment of facial acne vulgaris: pooled results from two multicenter, double-blind, randomized, vehicle-controlled, parallel-group trials. Clin Ther. 2004;26(11):1865–73. doi: 10.1016/j.clinthera.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 10.Yang GL, Zhao M, Wang JM, et al. Short-term clinical effects of photodynamic therapy with topical 5-aminolevulinic acid for facial acne conglobata: an open, prospective, parallel-arm trial. Photodermatol Photoimmunol Photomed. 2013;29(5):233–38. doi: 10.1111/phpp.12059. [DOI] [PubMed] [Google Scholar]
- 11.Wang HW, Lv T, Zhang LL, et al. Prospective study of topical 5-aminolevulinic acid photodynamic therapy for the treatment of moderate to severe acne vulgaris in Chinese patients. J Cutan Med Surg. 2012;16(5):324–33. doi: 10.1177/120347541201600509. [DOI] [PubMed] [Google Scholar]
- 12.Jeong E, Hong JW, Min JA, et al. Topical ALA-photodynamic therapy for acne can induce apoptosis of sebocytes and Down-regulate their TLR-2 and TLR-4 expression. Ann Dermatol. 2011;23(1):23–32. doi: 10.5021/ad.2011.23.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fabbrocini G, Cacciapuoti S, De Vita V, et al. The effect of aminolevulinic acid photodynamic therapy on microcomedones and macrocomedones. Dermatology. 2009;219(4):322–28. doi: 10.1159/000252854. [DOI] [PubMed] [Google Scholar]
- 14.Oh SH, Ryu DJ, Han EC, et al. A comparative study of topical 5-aminolevulinic acid incubation times in photodynamic therapy with intense pulsed light for the treatment of inflammatory acne. Dermatol Surg. 2009;35(12):1918–26. doi: 10.1111/j.1524-4725.2009.01315.x. [DOI] [PubMed] [Google Scholar]
- 15.Wiegell SR, Wulf HC. Photodynamic therapy of acne vulgaris using 5-aminolevulinic acid versus methyl aminolevulinate. J Am Acad Dermatol. 2006;54(4):647–51. doi: 10.1016/j.jaad.2005.12.033. [DOI] [PubMed] [Google Scholar]
- 16.Yin R, Hao F, Deng J, et al. Investigation of optimal aminolaevulinic acid concentration applied in topical aminolaevulinic acid-photodynamic therapy for treatment of moderate to severe acne: a pilot study in Chinese subjects. Br J Dermatol. 2010;163(5):1064–71. doi: 10.1111/j.1365-2133.2010.09860.x. [DOI] [PubMed] [Google Scholar]
- 17.Gold MH, Goldman MP. 5-aminolevulinic acid photodynamic therapy: where we have been and where we are going. Dermatol Surg. 2004;30(8):1077–83. doi: 10.1111/j.1524-4725.2004.30331.x. discussion 1083–84. [DOI] [PubMed] [Google Scholar]
- 18.Taylor MN, Gonzalez ML. The practicalities of photodynamic therapy in acne vulgaris. Br J Dermatol. 2009;160(6):1140–48. doi: 10.1111/j.1365-2133.2009.09054.x. [DOI] [PubMed] [Google Scholar]
- 19.Jang MS, Doh KS, Kang JS, et al. A comparative split-face study of photodynamic therapy with indocyanine green and indole-3-acetic acid for the treatment of acne vulgaris. Br J Dermatol. 2011;165(5):1095–100. doi: 10.1111/j.1365-2133.2011.10472.x. [DOI] [PubMed] [Google Scholar]