Abstract
Background
Tiotropium + olodaterol has demonstrated improvements beyond lung function benefits in a large Phase III clinical program as a once-daily maintenance treatment for COPD and may be a potential option for the initiation of maintenance treatment in COPD. Despite guideline recommendations that combined long-acting β2-agonists and inhaled corticosteroids should only be used in individuals at high risk of exacerbation, there is substantial use in individuals at lower risk. This raises the question of the comparative effectiveness of this combination as maintenance treatment in this group compared to other combination regimens.
Objective
The study aimed to assess the effect on lung function of once-daily tiotropium + olodaterol versus twice-daily salmeterol + fluticasone propionate in all participants with Global initiative for chronic Obstructive Lung Disease 2 or 3 (moderate to severe) COPD.
Methods
This was a randomized, double-blind, double-dummy, four-treatment, complete crossover study in which participants received once-daily tiotropium + olodaterol (5/5 µg and 2.5/5 µg) via Respimat® and twice-daily salmeterol + fluticasone propionate (50/500 µg and 50/250 µg) via Accuhaler® for 6 weeks. The primary end point was change in forced expiratory volume in 1 second (FEV1) area under the curve from 0 hour to 12 hours (AUC0–12) relative to the baseline after 6 weeks.
Results
Tiotropium + olodaterol 5/5 µg and 2.5/5 µg demonstrated statistically significant improvements in FEV1 AUC0–12 compared to salmeterol + fluticasone propionate (improvements from baseline were 317 mL and 295 mL with tiotropium + olodaterol 5/5 µg and 2.5/5 µg, and 188 mL and 192 mL with salmeterol + fluticasone propionate 50/500 µg and 50/250 µg, respectively). Tiotropium + olodaterol was superior to salmeterol + fluticasone propionate in lung function secondary end points, including FEV1 area under the curve from 0 hour to 24 hours (AUC0–24).
Conclusion
Once-daily tiotropium + olodaterol in participants with moderate-to-severe COPD provided superior lung function improvements to twice-daily salmeterol + fluticasone propionate. Dual bronchodilation can be considered to optimize lung function in individuals requiring maintenance treatment for COPD.
Keywords: COPD, maintenance treatment, lung function, tiotropium, FEV1, inhaled corticosteroid
Introduction
In addition to smoking cessation and nonpharmacologic interventions, including pulmonary rehabilitation, maintenance pharmacotherapy is well established for the management of COPD to optimize lung function and improve symptoms.1,2 Tiotropium is a once-daily COPD maintenance treatment for which there is a broad evidence base that has demonstrated long-term improvements in lung function, quality of life, exacerbation risk, and exercise capacity,3–7 with a similar safety profile when delivered via the HandiHaler® and Respimat® inhalers.8 The benefits of tiotropium + olodaterol as a once-daily maintenance treatment in COPD have been demonstrated in two large Phase III studies (TONADO® 1 and 2) in participants with a wide range of airway limitation (moderate to very severe).9 Tiotropium + olodaterol demonstrated improvements in lung function, health-related quality of life, and rescue medication use compared to tiotropium and olodaterol individually over 52 weeks.9 In a further Phase III study – VIVACITO® – pulmonary function testing (PFT) was performed over 24 hours and results demonstrated improvements in lung function over the full 24-hour dosing interval with tiotropium + olodaterol compared to the individual therapies.10 As well as demonstrating efficacy improvements, these Phase III studies showed that the tolerability profile of tiotropium + olodaterol is similar to that of tiotropium monotherapy.9,10
Inhaled corticosteroid (ICS) + long-acting β2-agonist (LABA) is an option for maintenance treatment that is recommended only for individuals who are at high risk of exacerbation, characterized as Global initiative for chronic Obstructive Lung Disease (GOLD) groups C and D, although prospective studies showing improved outcomes with this treatment regimen for these individuals are lacking.2 These individuals typically, though not exclusively, have severe or very severe airflow limitation (forced expiratory volume in 1 second [FEV1] <50% predicted, GOLD 3 and 4 spirometric classification).2 ICS + LABA is also an option for those with Asthma–COPD Overlap Syndrome.11
In clinical practice, however, ICS + LABA is also commonly used as maintenance treatment for individuals with low exacerbation risk who have less severe COPD, despite a lack of evidence to show that this is the optimal treatment approach for this group.12–14 For instance, the TONADO® studies investigated the efficacy and safety of tiotropium + olodaterol over a period of 1 year, including FEV1 area under the curve (AUC) from 0 hour to 3 hours (AUC0–3) response, trough FEV1, and St George’s Respiratory Questionnaire score. In these studies, 38.4% of participants who were categorized as GOLD A or B, based on spirometry and prior exacerbation history, were receiving an ICS-containing treatment at baseline.15 The safety profile of ICS also needs to be considered, due to the association with increased adverse events (AEs), such as pneumonia, and increased risk of fracture with long-term exposure.2,16
Given the increasing number of treatment options available, clinicians must decide the approach that is most appropriate for individuals who require initiation of maintenance treatment for COPD. Because several studies have shown the benefit of long-acting muscarinic antagonist (LAMA) or LABA monotherapy,3–7,17–19 we wished to test whether LAMA + LABA combination therapy would be more efficacious than a single agent. Therefore, in this study, we investigated the 24-hour lung function profile of once-daily tiotropium + olodaterol delivered via the Respimat® inhaler compared to two commonly used doses of twice-daily salmeterol + fluticasone propionate via Accuhaler® after 6 weeks, to assess the approach that was most effective at optimizing lung function. The results of this study have been reported previously at the European Respiratory Society International Conference 2015.20
Materials and methods
Study design
ENERGITO® was a Phase IIIb, multicenter, multinational, randomized, double-blind, double-dummy, active-controlled, four-treatment, complete crossover study to compare the effect, on the lung function profile, of orally inhaled once-daily tiotropium + olodaterol (5/5 µg and 2.5/5 µg) via Respimat® compared to twice-daily salmeterol + fluticasone propionate (50/500 µg and 50/250 µg) via Accuhaler® after 6 weeks of treatment in participants with COPD. The trial was registered with ClinicalTrials.gov under official identifier NCT01969721.
The primary end point was the response (change from baseline) in terms of FEV1 AUC from 0 hour to 12 hours (AUC0–12) after 6 weeks of treatment. The key secondary end point was response in terms of FEV1 AUC from 0 hour to 24 hours (AUC0–24).
Other secondary end points were response in terms of FEV1 AUC from 12 hours to 24 hours (AUC12–24), peak FEV1 from 0 hour to 3 hours (peak0–3 FEV1) response, and trough FEV1 response. The primary safety end point was the incidence of AEs.
Further end points were trough forced vital capacity (FVC) response; peak0–3 FVC response; FVC AUC0–24, FVC AUC0–12, and FVC AUC12–24 responses; and FEV1 and FVC measured at all time points after 6 weeks of treatment.
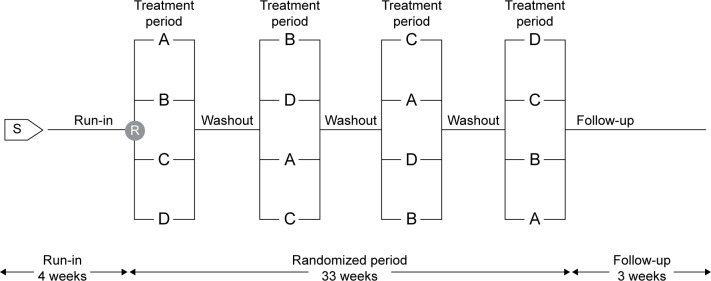
Eligible participants entered a 4-week screening period during which prescription corticosteroids (inhaled or oral), β-adrenergics (inhaled short- or long-acting, oral or patch, except for β-blockers), and long-acting anticholinergics were discontinued. Participants were then randomized into the crossover part of the study and received each of the four treatments – tiotropium + olodaterol 5/5 µg and 2.5/5 µg and salmeterol + fluticasone propionate 50/500 µg and 50/250 µg – for a period of 6 weeks in a randomized sequence, with each treatment separated by a 21-day washout (Figure 1).
Figure 1.
Study design.
Notes: Treatment periods are 6 weeks and washout periods are 3 weeks. A–D refer to treatment groups.
Abbreviations: R, randomization; S, screening.
Participants entered a 21-day follow-up period after study completion or discontinuation, during which they were permitted to resume medications prescribed prior to the study. Open-label salbutamol was provided for rescue medication use, which was recorded by the participant. A short-acting anticholinergic (ipratropium bromide) was provided for use during the screening and washout periods.
Patients
All participants provided signed, informed consent in compliance with the guidelines of the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use, Harmonised Tripartite Guideline E6: Good Clinical Practice. The trial was initiated after the protocol, informed consent, and patient information forms were approved by the local Institutional Review Boards or Independent Ethics Committees for the European Union by the Competent Authority and, for the other counties, approval by, or notification to, local health authorities. Inclusion criteria were as follows: a diagnosis of COPD; moderate-to-severe pulmonary impairment (postbronchodilator FEV1 ≥30% and <80% of predicted normal);21 postbronchodilator FEV1/FVC <70% at screening visit; age ≥40 years; current or ex-smoker with a smoking history of >10 pack-years; able to perform technically acceptable PFT and maintain paper diaries as required; and able to competently inhale medication from the Respimat® inhaler (a metered-dose inhaler) and the Accuhaler®. Participants were excluded if they met any of the following criteria: significant disease other than COPD; any COPD exacerbation requiring treatment with antibiotics, systemic steroids, or hospitalization in the past 3 months; abnormal laboratory tests according to the investigator; or a history of asthma. Additional exclusion criteria are summarized in Table S1. Participants were entered into the study based on moderate-to-severe pulmonary impairment (GOLD 2–3) graded according to the 2010 version of the GOLD strategy document.22 Information on symptoms and prior exacerbation history was not collected for screening purposes; therefore, participants were not screened based on the updated GOLD A–D patient group classification.2
Treatment schedule
Each morning, participants self-administered two puffs of the Respimat® (tiotropium + olodaterol 5/5 µg or 2.5/5 µg or placebo) followed by one puff of the Accuhaler® (salmeterol + fluticasone propionate 50/500 µg or 50/250 µg or placebo). Each evening (12 hours after the morning dose), participants inhaled one puff of the Accuhaler® only. Self-administration of medication was performed under supervision during clinic visits and the time of administration was recorded for accurate timing of postdose PFT. The timing of medication dosing was established at the start of each treatment period, and subsequent doses were administered within 30 minutes of the first dose time (ie, at 24 hours ±30 minutes).
Assessments
At the screening visit, in addition to physical examination and laboratory testing, participants underwent reversibility testing using 400 µg salbutamol and received training in use of the devices. At the start of the treatment periods, predose PFT was performed at 1 hour and at 10 minutes prior to inhalation of trial medication for the first treatment period, then at 30 minutes before dosing at the start of subsequent treatment periods. Postdose PFT at the start of all treatment periods was performed at 30 minutes, 1 hour, 2 hours, and 3 hours postdose. At the end of each 6-week dosing period, PFT was performed 30 minutes prior to inhalation of trial medication and up to 24 hours after dosing (30 minutes, 1 hour, 2 hours, 3 hours, 4 hours, 6 hours, 8 hours, 10 hours, 11 hours 50 minutes, 12 hours 30 minutes, 13 hours, 14 hours, 22 hours, 23 hours, and 23 hours 50 minutes postdose). PFT up to 14 hours postdose was included to capture the peak associated with the evening dose of salmeterol + fluticasone propionate. PFT was performed using MasterScope® CT spirometers (ERT, Hoechberg, Germany), which complied with, and were calibrated daily in accordance with, the criteria of the American Thoracic Society and European Respiratory Society.23 AEs and concomitant therapies were recorded from screening through to follow-up.
Statistical analysis
Efficacy analyses were performed for all participants who received at least one dose of trial medication and had both baseline and postbaseline measurements for the primary end point, defined as the full analysis set. The per-protocol analysis set was defined as all participants without any important protocol deviations related to efficacy in any treatment period. If the number of participants in the per-protocol analysis set was <90% of those in the full analysis set, the primary efficacy analyses were to be performed on the per-protocol analysis set, as supportive analyses. All treated participants were included in the safety analyses.
For the primary end point of FEV1 AUC0–12 response and key secondary end point of FEV1 AUC0–24 response, response is defined as change from patient baseline. Patient baseline values were obtained by calculating the mean of the period baseline values taken for each patient on the first day of each treatment period prior to administration of the morning dose. For the primary and secondary end points, hypotheses were tested in hierarchical order, each at the 5% level of significance (two-sided) to protect the overall probability of type I error at 0.05 (two-sided). For the primary and secondary end points, the changes from baseline (start of each treatment period) at 6 weeks were analyzed using a restricted maximum-likelihood-based mixed-effects repeated-measures model, including treatment and period as fixed effects, patient as random effect, and period baseline and patient baseline as covariates. Compound symmetry was used as a covariate structure for within-patient variation. The SAS procedure MIXED was used for the restricted maximum-likelihood estimation, and Kenward–Roger approximation was used for denominator degrees of freedom.24 Adjusted mean values as well as treatment comparisons are presented, together with 95% confidence intervals.
Results
Patient disposition and baseline disease characteristics
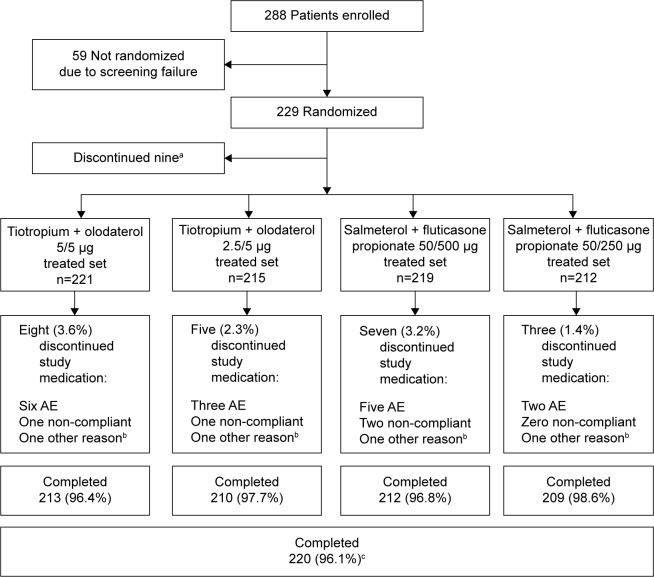
Overall, 288 participants were enrolled in the study and 229 were randomized to receive treatment (Figure 2); 59 participants were not randomized due to screening failure. Discontinuation from study medication was low (nine participants did not complete any treatment arm); primary reasons for discontinuation were AEs and noncompliance (Figure 2).
Figure 2.
Patient disposition.
Notes: aNine patients did not complete any treatment; bincludes lack of efficacy; ccompleting ≥1 treatment arm.
Abbreviation: AE, adverse event.
In the treated population, the majority of participants were male (64.6%) and white (99.6%), and almost half of participants were smokers at the time of the study (44.5%) (Table 1). Most participants had GOLD 2 lung function impairment (72.1%) and the remainder had GOLD 3 (27.9%). Participants were highly treated prior to the study; the most frequently recorded baseline pulmonary medications were LAMA (53.7%), short-acting β-agonist (53.3%), and LABA + ICS (38.0%) (Table 1).
Table 1.
Demographic and baseline patient characteristics (treated population)
| Total (n=229) | |
|---|---|
| Sex, n (%) | |
| Male | 148 (64.6) |
| Female | 81 (35.4) |
| Race, n (%) | |
| White | 228 (99.6) |
| Asian | 1 (0.4) |
| Region, n (%) | |
| Western Europe | 169 (73.8) |
| Eastern Europe | 60 (26.2) |
| Mean (SD) age, years | 63.6 (7.6) |
| Alcohol history, n (%) | |
| Nondrinker | 58 (25.3) |
| Drinker | 171 (74.7) |
| Smoking status, n (%) | |
| Ex-smoker | 127 (55.5) |
| Current smoker | 102 (44.5) |
| Mean (SD) smoking history, pack-years | 39.1 (18.3) |
| Mean (SD) prebronchodilator screening | |
| FEV1, L | 1.425 (0.456) |
| % of predicted normal FEV1, L | 49.490 (12.228) |
| Mean (SD) postbronchodilator screening | |
| FEV1, L | 1.624 (0.468) |
| % of predicted normal FEV1, L | 56.436 (11.812) |
| GOLD, n (%) | |
| 1 (≥80%) | 0 |
| 2 (50–<80%) | 165 (72.1) |
| 3 (30–<50%) | 64 (27.9) |
| 4 (<30%) | 0 |
| Baseline pulmonary medication, n (%) | |
| LAMA | 123 (53.7) |
| SABA | 122 (53.3) |
| LABA/ICS | 87 (38.0) |
| LABA | 54 (23.6) |
| SAMA | 24 (10.5) |
| ICS | 22 (9.6) |
| Xanthines | 11 (4.8) |
| Mucolytics | 5 (2.2) |
| Oral β-adrenergics | 2 (0.9) |
| Oxygen | 1 (0.4) |
| Steroids, other | 1 (0.4) |
Abbreviations: FEV1, forced expiratory volume in 1 second; GOLD, Global initiative for chronic Obstructive Lung Disease; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; SABA, short-acting β-agonist; SAMA, short-acting muscarinic antagonist; SD, standard deviation.
Efficacy
FEV1 AUC0–12 (primary end point), FEV1 AUC0–24, and FEV1 AUC12–24 after 6 weeks of treatment were increased from baseline by >120 mL in all treatment arms, with greater increases at both dose levels of once-daily tiotropium + olodaterol compared to twice-daily salmeterol + fluticasone propionate. Responses appeared to be similar for the two dose levels of tiotropium + olodaterol and salmeterol + fluticasone propionate (Table 2). Treatment comparisons for the primary end point revealed statistically significant improvements in FEV1 AUC0–12 with either dose of tiotropium + olodaterol compared to either dose of salmeterol + fluticasone propionate, ranging from +103 mL to +129 mL (P<0.0001 for all comparisons).
Table 2.
Adjusted mean FEV1 AUC responses after 6 weeks of treatment (full analysis set)
| Tiotropium + olodaterol 5/5 µg | Tiotropium + olodaterol 2.5/5 µg | Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | |
|---|---|---|---|---|
| Patients, n | 216 | 214 | 217 | 211 |
| Adjusted mean (SE) FEV1 | 317 (14) | 295 (14) | 188 (14) | 192 (15) |
| AUC0–12 response, mL | ||||
| Adjusted mean (SE) FEV1 | 244 (14) | 228 (14) | 159 (14) | 162 (14) |
| AUC0–24 response, mL | ||||
| Adjusted mean (SE) FEV1 | 172 (14) | 160 (14) | 129 (14) | 132 (14) |
| AUC12–24 response, mL |
Notes: The adjusted mean (SE) was obtained from fitting a mixed-effects repeated-measures model including the following: fixed effects of treatment and period; period baseline and patient baseline as covariates; patient as a random effect; compound symmetry covariance structure for within-patient variation; and Kenward–Roger approximation of denominator degrees of freedom.
Abbreviations: AUC, area under the curve; AUC0–12, AUC from 0 hour to 12 hours; AUC0–24, AUC from 0 hour to 24 hours; AUC12–24, AUC from 12 hours to 24 hours; FEV1, forced expiratory volume in 1 second; SE, standard error.
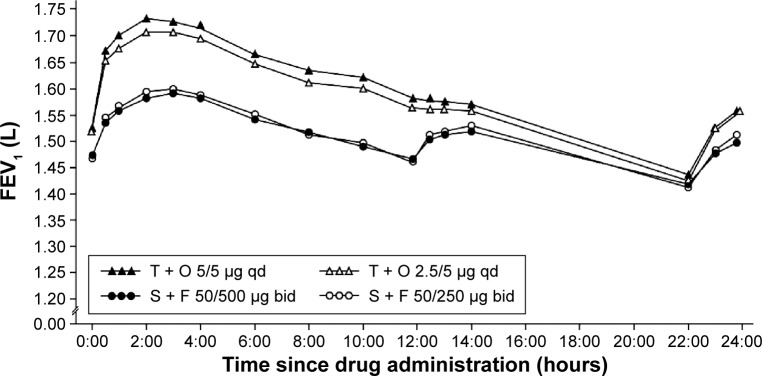
Tiotropium + olodaterol showed improved FEV1 values over the full 24-hour dosing interval compared to salmeterol + fluticasone propionate after 6 weeks of treatment (Figure 3). Accordingly, analysis of the key secondary end point of FEV1 AUC0–24 response showed significantly greater improvements with either dose of tiotropium + olodaterol versus either dose of salmeterol + fluticasone propionate, ranging from +65 mL to +86 mL (P<0.0001 for all comparisons) (Table 3). Improvements in FEV1 AUC12–24 response after 6 weeks of treatment were also significantly greater with tiotropium + olodaterol compared to salmeterol + fluticasone propionate (P<0.05 for all comparisons) (Table 3). There was a trend for greater improvement in FEV1 AUC parameters with tiotropium + olodaterol 5/5 µg compared to either dose of salmeterol + fluticasone than with tiotropium + olodaterol 2.5/5 µg compared to salmeterol + fluticasone (Table 3).
Figure 3.
Adjusted mean 24-hour FEV1 profile after 6 weeks of treatment (full analysis set).
Abbreviations: bid, twice daily; F, fluticasone propionate; FEV1, forced expiratory volume in 1 second; O, olodaterol; qd, once daily; S, salmeterol; T, tiotropium.
Table 3.
Adjusted mean FEV1 AUC0–12, AUC0–24, and AUC12–24 responses after 6 weeks of treatment, showing the treatment differences (full analysis set)
| Treatment comparison
|
||||
|---|---|---|---|---|
| Tiotropium + olodaterol 5/5 µg versus
|
Tiotropium + olodaterol 2.5/5 µg versus
|
|||
| Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | |
| FEV1 AUC0–12, mL | ||||
| Adjusted mean (SE) | 129 (11) | 125 (11) | 106 (11) | 103 (11) |
| 95% CI | 107, 150 | 103, 147 | 85, 128 | 81, 124 |
| P-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| FEV1 AUC0–24, mL | ||||
| Adjusted mean (SE) | 86 (11) | 82 (11) | 69 (11) | 65 (11) |
| 95% CI | 65, 107 | 61, 103 | 48, 90 | 45, 86 |
| P-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| FEV1 AUC12–24, mL | ||||
| Adjusted mean (SE) | 43 (11) | 39 (12) | 32 (11) | 28 (11) |
| 95% CI | 21, 65 | 17, 62 | 9, 54 | 6, 51 |
| P-value | 0.0002 | 0.0007 | 0.0055 | 0.0146 |
Notes: The adjusted mean (SE) was obtained from fitting a mixed-effects repeated-measures model including the following: fixed effects of treatment and period; period baseline and patient baseline as covariates; patient as a random effect; compound symmetry covariance structure for within-patient variation; and Kenward–Roger approximation of denominator degrees of freedom.
Abbreviations: AUC, area under the curve; AUC0–12, AUC from 0 hour to 12 hours; AUC0–24, AUC from 0 hour to 24 hours; AUC12–24, AUC from 12 hours to 24 hours; CI, confidence interval; FEV1, forced expiratory volume in 1 second; SE, standard error.
The peak0–3 FEV1 responses at Day 1 and Day 43 and trough FEV1 responses after 6 weeks of treatment for tiotropium + olodaterol and salmeterol + fluticasone propionate are shown in Table 4. At the end of the 6-week treatment period (Day 43), tiotropium + olodaterol improved peak0–3 FEV1 response by +111 mL to +147 mL compared to salmeterol + fluticasone propionate (P<0.0001 for all comparisons) (Table 5). Notably, tiotropium + olodaterol also gave greater improvements in trough FEV1 after 6 weeks of treatment compared to both doses of salmeterol + fluticasone propionate, with improvements of +58 mL and +54 mL with tiotropium + olodaterol 5/5 µg and 2.5/5 µg, respectively, versus salmeterol + fluticasone propionate 50/500 µg (P<0.001 for all comparisons) (Table 5).
Table 4.
Peak0–3 FEV1 response at study Day 1 and Day 43 and trough FEV1 responses after 6 weeks of treatment (full analysis set)
| Tiotropium + olodaterol 5/5 µg | Tiotropium + olodaterol 2.5/5 µg | Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | |
|---|---|---|---|---|
| Patients, n | 218 | 215 | 218 | 211 |
| Adjusted mean (SE) peak0–3 | ||||
| FEV1 response, mL | ||||
| Day 1 | 345 (12) | 326 (12) | 265 (12) | 250 (12) |
| Day 43 | 432 (16) | 401 (16) | 285 (15) | 291 (16) |
| Patients, n | 216 | 214 | 217 | 211 |
| Adjusted mean (SE) trough | 197 (14) | 192 (14) | 139 (14) | 150 (14) |
| FEV1 response, mL |
Notes: The adjusted mean (SE) was obtained from fitting a mixed-effects repeated-measures model including the following: fixed effects of treatment and period; period baseline and patient baseline as covariates; patient as a random effect; compound symmetry covariance structure for within-patient variation; and Kenward–Roger approximation of denominator degrees of freedom.
Abbreviations: FEV1, forced expiratory volume in 1 second; peak0–3 FEV1, peak forced expiratory volume in 1 second from 0 hour to 3 hours; SE, standard error.
Table 5.
Peak0–3 FEV1 response at study Day 1 and Day 43 and trough FEV1 responses after 6 weeks of treatment, showing the differences between treatments (full analysis set)
| Treatment comparison
|
||||
|---|---|---|---|---|
| Tiotropium + olodaterol 5/5 µg versus
|
Tiotropium + olodaterol 2.5/5 µg versus
|
|||
| Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | |
| Peak0–3 FEV1, mL, Day 1 | ||||
| Adjusted mean (SE) | 80 (9) | 95 (9) | 61 (9) | 76 (9) |
| 95% CI | 62, 97 | 77, 112 | 44, 79 | 59, 94 |
| P-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| Peak0–3 FEV1, mL, Day 43 | ||||
| Adjusted mean (SE) | 147 (12) | 142 (12) | 116 (12) | 111 (12) |
| 95% CI | 123, 171 | 118, 166 | 92, 140 | 87, 135 |
| P-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| Trough FEV1, mL | ||||
| Adjusted mean (SE) | 58 (12) | 47 (12) | 54 (12) | 42 (12) |
| 95% CI | 34, 82 | 22, 71 | 29, 78 | 18, 67 |
| P-value | <0.0001 | 0.0002 | <0.0001 | 0.0007 |
Notes: The adjusted mean (SE) was obtained from fitting a mixed-effects repeated-measures model including the following: fixed effects of treatment and period; period baseline and patient baseline as covariates; patient as a random effect; compound symmetry covariance structure for within-patient variation; and Kenward–Roger approximation of denominator degrees of freedom.
Abbreviations: CI, confidence interval; FEV1, forced expiratory volume in 1 second; peak0–3 FEV1, peak forced expiratory volume in 1 second from 0 hour to 3 hours; SE, standard error.
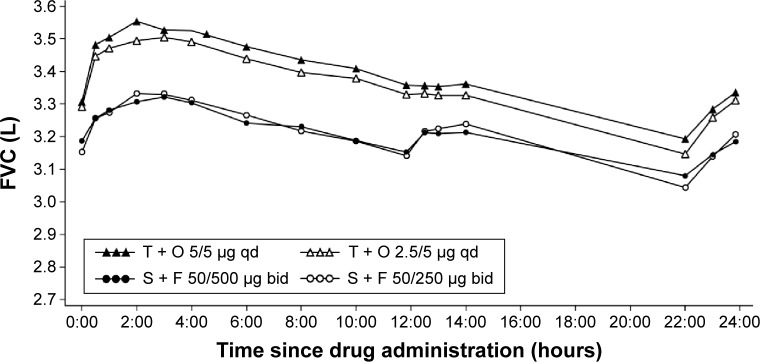
Changes in FVC after 6 weeks of treatment were significantly greater with tiotropium + olodaterol compared to salmeterol + fluticasone propionate, measured as FVC AUC0–12, FVC AUC0–24, FVC AUC12–24, and FVC AUC0–3, trough FVC, and peak0–3 FVC responses (P<0.0001 for all comparisons of tiotropium + olodaterol versus salmeterol + fluticasone propionate). The improvement in FVC with tiotropium + olodaterol compared to salmeterol + fluticasone propionate was maintained over the full 24-hour dosing interval (Figure 4 and Tables S2 and S3).
Figure 4.
Adjusted mean 24-hour FVC profile after 6 weeks of treatment (full analysis set).
Abbreviations: bid, twice daily; F, fluticasone propionate; FVC, forced vital capacity; O, olodaterol; qd, once daily; S, salmeterol; T, tiotropium.
Safety
Overall, the frequency of AEs was similar between all treatment groups, with 29.7%–37.0% of participants reporting at least one AE while on treatment. The most common AEs were COPD worsening, nasopharyngitis, and cough (Table 6). Severe AEs were recorded in ≤5% of participants and AEs leading to discontinuation occurred in <3% of participants in each treatment group. Serious AEs occurred in ≤4.1% of participants. There were two serious AEs leading to death in the tiotropium + olodaterol 5/5 µg group, one of which was a cerebral hemorrhage in a predisposed patient and the other occurred 19 days after the last dose of study treatment, with unknown cause (Table 6).
Table 6.
Summary of AEs (treated population)
| Tiotropium + olodaterol 5/5 µg, n (%) | Tiotropium + olodaterol 2.5/5 µg, n (%) | Salmeterol + fluticasone propionate 50/500 µg, n (%) | Salmeterol + fluticasone propionate 50/250 µg, n (%) | Total, n (%) | |
|---|---|---|---|---|---|
| Patients | 221 (100) | 215 (100) | 219 (100) | 212 (100) | 229 (100) |
| Any AE | 75 (33.9) | 74 (34.4) | 81 (37.0) | 63 (29.7) | 158 (69.0) |
| Severe AEs | 6 (2.7) | 7 (3.3) | 11 (5.0) | 5 (2.4) | 24 (10.5) |
| Drug-related AEsa | 6 (2.7) | 12 (5.6) | 9 (4.1) | 9 (4.2) | 23 (10.0) |
| Other significant AEsb | 4 (1.8) | 3 (1.4) | 2 (0.9) | 0 (0.0) | 9 (3.9) |
| AEs leading to discontinuation of trial drug | 6 (2.7) | 4 (1.9) | 3 (1.4) | 2 (0.9) | 15 (6.6) |
| Serious AEs | 7 (3.2) | 6 (2.8) | 9 (4.1) | 4 (1.9) | 22 (9.6) |
| Fatal AEs | 2 (0.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (0.9) |
| Immediately life-threatening | 0 (0.0) | 1 (0.5) | 0 (0.0) | 0 (0.0) | 1 (0.4) |
| AEs | |||||
| Requiring hospitalization | 5 (2.3) | 6 (2.8) | 9 (4.1) | 4 (1.9) | 20 (8.7) |
| Prolonged hospitalization | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.5) | 1 (0.4) |
| AEs occurring in >2% of patients overallc | |||||
| COPD worsening | 20 (9.0) | 12 (5.6) | 19 (8.7) | 9 (4.2) | 45 (19.7) |
| Nasopharyngitis | 12 (5.4) | 12 (5.6) | 11 (5.0) | 13 (6.1) | 40 (17.5) |
| Cough | 7 (3.2) | 5 (2.3) | 5 (2.3) | 4 (1.9) | 17 (7.4) |
| Dyspnea | 3 (1.4) | 3 (1.4) | 6 (2.7) | 4 (1.9) | 14 (6.1) |
| Headache | 8 (3.6) | 5 (2.3) | 2 (0.9) | 4 (1.9) | 14 (6.1) |
| Back pain | 4 (1.8) | 2 (0.9) | 2 (0.9) | 4 (1.9) | 11 (4.8) |
| Dysphonia | 0 (0.0) | 3 (1.4) | 3 (1.4) | 2 (0.9) | 7 (3.1) |
| Arthralgia | 1 (0.5) | 2 (0.9) | 2 (0.9) | 2 (0.9) | 6 (2.6) |
| Diarrhea | 1 (0.5) | 2 (0.9) | 1 (0.5) | 2 (0.9) | 5 (2.2) |
| Nausea | 1 (0.5) | 0 (0.0) | 2 (0.9) | 2 (0.9) | 5 (2.2) |
| Oropharyngeal pain | 1 (0.5) | 2 (0.9) | 2 (0.9) | 0 (0.0) | 5 (2.2) |
| Pneumonia | 1 (0.5) | 2 (0.9) | 1 (0.5) | 1 (0.5) | 5 (2.2) |
Notes:
Drug-related AEs were defined by the investigator;
according to ICH E3; cpercentages were calculated using the total number of patients per treatment group as the denominator.
Abbreviations: AE, adverse event; COPD, chronic obstructive pulmonary disease; ICH E3, International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use, Harmonised Tripartite Guideline E3.
Discussion
In this study, once-daily tiotropium + olodaterol improved lung function to a greater extent than twice-daily salmeterol + fluticasone propionate, demonstrating significant improvements in the primary end point of FEV1 AUC0–12 and all other measures of lung function. Importantly, superiority in lung function improvement with once-daily tiotropium + olodaterol compared to twice-daily salmeterol + fluticasone propionate was demonstrated over the full 24-hour dosing period. These results add to the 24-hour lung function profile of tiotropium + olodaterol from the VIVACITO® study. In addition, ENERGITO® included PFT measurements between 12 hours and 14 hours to account for the evening dose of salmeterol + fluticasone propionate; this testing schedule provided more rigorous testing over the full dosing interval compared to previous tiotropium + olodaterol studies.
Of particular note, the improvement in FEV1 AUC0–12 with tiotropium + olodaterol versus salmeterol + fluticasone propionate in our study was similar to the increases seen with indacaterol + glycopyrrolate, another once-daily maintenance treatment, which was compared to twice-daily salmeterol-fluticasone in the recent ILLUMINATE study of participants with moderate-to-severe COPD.1
Also of note were the significant improvements in all FVC parameters with tiotropium + olodaterol compared to salmeterol + fluticasone propionate. These improvements indicate a greater reduction in air trapping, and, therefore, lung hyperinflation, with tiotropium + olodaterol compared to salmeterol + fluticasone propionate. Furthermore, FVC parameters are associated with small-airways dysfunction, common in COPD; FVC responsiveness with tiotropium + olodaterol may indicate a specific improvement in the small airways following treatment.25
Optimization of lung function is an important treatment goal through the course of COPD, and there is a strong rationale to provide these benefits from the point at which individuals are identified as needing initiation of maintenance treatment. Although measures of symptomology and health-related quality of life are required, improvements in lung function measures have been shown to predict improvements in patient-reported outcomes, as well as risk of exacerbation.26 While this study did not include health status or symptomatic end points, four large studies have demonstrated that improvements in lung function with tiotropium + olodaterol are accompanied by clinically meaningful improvements in St George’s Respiratory Questionnaire score.9,27 In addition, an exploratory analysis from the TONADO® studies suggested a trend toward improvement in exacerbations;9 a large ongoing 52-week study will define the impact of tiotropium + olodaterol on exacerbation risk (DYNAGITO®; NCT02296138; 1237.19). The lung function results from the current study are also broadly in line with another study suggesting that LABA + ICS may not be the most effective treatment for improving lung function in individuals with moderate-to-severe COPD.1 In that study, a greater lung function response with indacaterol + glycopyrronium versus salmeterol + fluticasone was accompanied by a significant treatment-corrected difference in Transition Dyspnea Index focal score, but no difference in St George’s Respiratory Questionnaire score.
One potential limitation of the study is that it cannot be interpreted directly in the context of the current GOLD recommendations for treatment options, wherein individuals are grouped according to airflow limitation, exacerbation risk, symptoms, and breathlessness (GOLD patient groups A–D).2 Inclusion in the ENERGITO® study was based on the spirometric assessment of severity of airflow limitation used in an earlier version of the GOLD strategy report;22 participants with GOLD 2 and 3 (moderate and severe) COPD were screened and patient symptoms or exacerbation risk were not assessed as enrollment criteria. Regardless of this, the findings suggest that tiotropium + olodaterol provides lung function benefits in a representative population with moderate-to-severe COPD and that response to treatment is not affected by the prior use or type of maintenance treatment.
In this study, there was no apparent difference in lung function response between the two doses of salmeterol + fluticasone propionate tested (50/250 µg and 50/500 µg). This observation was similar to that seen in the recent WISDOM study, which assessed the effect of stepwise withdrawal of ICS from a regimen containing tiotropium, salmeterol, and fluticasone propionate. In the WISDOM study, there was no change in lung function when the twice-daily dose of fluticasone propionate was reduced from 500 µg to 250 µg, although participants were only observed on the 250 µg dose for a period of 6 weeks. Complete cessation of fluticasone propionate resulted in a modest decrease in lung function.28 These observations raise the question of whether only a low dose of ICS is required to achieve potential lung function improvement with these agents.
Conclusion
For individuals with moderate-to-severe COPD who require maintenance treatment with the goal of improving lung function, with associated symptomatic and health-status benefits, tiotropium + olodaterol should be considered as another treatment option that offers better lung function optimization than LABA + ICS. While tiotropium + olodaterol has demonstrated clinically significant improvements in symptoms and quality of life versus placebo,27 further studies are warranted to confirm whether the additional improvements of tiotropium + olodaterol relative to LABA + ICS demonstrated in this study translate into additional clinically relevant benefits for individuals.
Supplementary materials
Table S1.
Additional exclusion criteria
| Patients with any of the following conditions were to be excluded: |
| A diagnosis of thyrotoxicosis (due to the known class side-effect profile of β2-agonists) |
| A diagnosis of paroxysmal tachycardia (>100 beats/min) (due to the known class side-effect profile of β2-agonists) |
| A history of myocardial infarction within 1 year of the screening visit |
| Unstable or life-threatening cardiac arrhythmia |
| Hospitalization for heart failure within the past year |
| Known active tuberculosis |
| A malignancy for which the patient has undergone resection, radiation therapy, or chemotherapy within the past 5 years (except for treated basal cell carcinoma) |
| A history of life-threatening pulmonary obstruction |
| A history of cystic fibrosis |
| Clinically evident bronchiectasis |
| A history of significant alcohol or drug abuse |
| Patients who have undergone thoracotomy with pulmonary resection |
| Patients being treated with oral or patch β-adrenergics |
| Patients being treated with oral corticosteroid medication within 6 weeks prior to Visit 1 |
| Patients who regularly use daytime oxygen therapy for >1 hour per day and, in the investigator’s opinion, will be unable to abstain from the use of oxygen therapy during clinic visits |
| Patients who have completed a pulmonary rehabilitation program in the 6 weeks prior to the screening visit or patients who are currently in a pulmonary rehabilitation program |
| Patients who have taken an investigational drug within 1 month, 6 half-lives, or within the washout period (whichever is greater) prior to screening visit (Visit 1) |
| Patients with known hypersensitivity to β-adrenergic drugs, BAC, EDTA, or any other component of the Respimat® inhalation solution, or lactose monohydrate |
| Pregnant or nursing women |
| Women of childbearing potential not using a highly effective method of birth control.a Female patients will be considered to be of childbearing potential unless surgically sterilized by hysterectomy or bilateral tubal ligation or if in postmenopausal stage for ≥2 years |
| Patients who have previously been randomized in this study or are currently participating in another study |
| Patients who are unable to comply with pulmonary medication restrictions prior to randomization |
Notes:
Defined as those methods that result in a low failure rate (ie, <1% per year) when used consistently and correctly as defined by the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use – Guidance on Nonclinical Safety Studies for the Conduct of Human Clinical Trials and Marketing Authorization for Pharmaceuticals M3(R2) guidelines.
Abbreviations: BAC, benzalkonium chloride; EDTA, ethylenediaminetetraacetic acid.
Table S2.
Adjusted mean FVC AUC0–12, AUC0–24, and AUC12–24 responses after 6 weeks of treatment: treatment differences (full analysis set)
| Treatment comparison
|
||||
|---|---|---|---|---|
| Tiotropium + olodaterol 5/5 µg versus
|
Tiotropium + olodaterol 2.5/5 µg versus
|
|||
| Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | |
| FVC AUC0–12, mL | ||||
| Adjusted mean (SE) | 218 (18)* | 215 (18)* | 183 (18)* | 180 (18)* |
| 95% CI | 184, 253 | 180, 250 | 149, 218 | 146, 215 |
| FVC AUC0–24, mL | ||||
| Adjusted mean (SE) | 176 (17)* | 177 (17)* | 140 (17)* | 141 (17)* |
| 95% CI | 144, 209 | 144, 209 | 108, 173 | 108, 173 |
| FVC AUC12–24, mL | ||||
| Adjusted mean (SE) | 135 (18)* | 138 (18)* | 98 (18)* | 101 (18)* |
| 95% CI | 100, 170 | 103, 174 | 63, 133 | 66, 136 |
Notes:
P<0.0001. The adjusted mean (SE) was obtained from fitting a mixed-effects repeated-measures model including the following: fixed effects of treatment and period; period baseline and patient baseline as covariates; patient as a random effect; compound symmetry covariance structure for within-patient variation; and Kenward–Roger approximation of denominator degrees of freedom.
Abbreviations: AUC0–12, area under the curve from 0 hour to 12 hours; AUC0–24, area under the curve from 0 hour to 24 hours; AUC12–24, area under the curve from 12 hours to 24 hours; CI, confidence interval; FVC, forced vital capacity; SE, standard error.
Table S3.
Adjusted mean FVC AUC0–3, trough FVC, and peak0–3 FVC responses after 6 weeks of treatment: treatment differences (full analysis set)
| Treatment comparison
|
||||
|---|---|---|---|---|
| Tiotropium + olodaterol 5/5 µg versus
|
Tiotropium + olodaterol 2.5/5 µg versus
|
|||
| Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | |
| FVC AUC0–3, mL | ||||
| Adjusted mean (SE) | 104 (13)* | 110 (13)* | 82 (13)* | 88 (13)* |
| 95% CI | 78, 130 | 84, 136 | 56, 108 | 62, 114 |
| Trough FVC, mL | ||||
| Adjusted mean (SE) | 145 (20)* | 137 (20)* | 120 (20)* | 112 (20)* |
| 95% CI | 106, 183 | 98, 176 | 81, 158 | 74, 151 |
| Peak0–3 FVC response, mL | ||||
| Adjusted mean (SE) | 215 (20)* | 213 (20)* | 172 (20)* | 169 (20)* |
| 95% CI | 176, 255 | 173, 253 | 133, 211 | 130, 209 |
Notes:
P<0.0001. The adjusted mean (SE) was obtained from fitting a mixed-effects repeated-measures model including the following: fixed effects of treatment and period; period baseline and patient baseline as covariates; patient as a random effect; compound symmetry covariance structure for within-patient variation; and Kenward–Roger approximation of denominator degrees of freedom.
Abbreviations: AUC0–3, area under the curve from 0 hour to 3 hours; CI, confidence interval; FVC, forced vital capacity; peak0–3 FVC, peak forced vital capacity from 0 hour to 3 hours; SE, standard error.
Acknowledgments
This work was supported by Boehringer Ingelheim Pharma GmbH & Co. KG. The authors received no compensation related to the development of the manuscript. This work was supported by Boehringer Ingelheim Pharma GmbH & Co. KG. Medical writing assistance was provided by Tanja Torbica and Claire Scofield, on behalf of Complete Health-Vizion, and was contracted and compensated by Boehringer Ingelheim Pharma GmbH & Co. KG.
Footnotes
Disclosure
The institution where KMB is employed has received compensation for organizing or participating in advisory boards for Almirall Hermal, Cytos, Chiesi, Boehringer Ingelheim, AstraZeneca, Mundipharma, Novartis, and Revotar Biopharmaceuticals, and for participation in scientific meetings or courses supported by various pharmaceutical companies (Almirall Hermal, AstraZeneca, Boehringer Ingelheim, Novartis, Pfizer, and Takeda) in the past 3 years. KMB’s institution has also received consulting fees from Ablynx, Apellis Pharmaceuticals, Chiesi, and Cytos. The institution has received compensation for the design, performance or participation in single or multi-center clinical trials in the past 3 years from several companies including Almirall, Boehringer Ingelheim, Cytos, GSK, Mundipharma, Novartis, Pfizer, Revotar Biopharmaceuticals, Sterna AG, and TEVA. ED reports consultancy fees from Actelion, Boehringer, AstraZeneca, and Cipla, advisory board fees for Chiesi, AstraZeneca, and CSL Behring, and speaker fees for Glaxo-SmithKline and Boehringer. LG and AH are employees of Boehringer Ingelheim. JES, DZ, and LB report no conflicts of interest in this work.
Author Contributions
The authors meet criteria for authorship as recommended by the International Committee of Medical Journal Editors. They take full responsibility for the scope, direction, content of, and editorial decisions relating to, the manuscript, and were involved at all stages of development. All authors contributed toward data analysis, drafting and critically revising the paper, and they have approved the submitted manuscript and agree to be accountable for all aspects of the work.
References
- 1.Vogelmeier CF, Bateman ED, Pallante J, et al. Efficacy and safety of once-daily QVA149 compared with twice-daily salmeterol-fluticasone in patients with chronic obstructive pulmonary disease (ILLUMINATE): a randomised, double-blind, parallel group study. Lancet Respir Med. 2013;1(1):51–60. doi: 10.1016/S2213-2600(12)70052-8. [DOI] [PubMed] [Google Scholar]
- 2.Global Initiative for Chronic Obstructive Lung Disease Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. [Accessed September 30, 2015]. [updated February 18, 2015]. Available from: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2015_Feb18.pdf.
- 3.Tashkin DP, Celli B, Senn S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359(15):1543–1554. doi: 10.1056/NEJMoa0805800. [DOI] [PubMed] [Google Scholar]
- 4.Bateman ED, Tashkin D, Siafakas N, et al. A one-year trial of tiotropium Respimat® plus usual therapy in COPD patients. Respir Med. 2010;104(10):1460–1472. doi: 10.1016/j.rmed.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Yohannes AM, Willgoss TG, Vestbo J. Tiotropium for treatment of stable COPD: a meta-analysis of clinically relevant outcomes. Respir Care. 2011;56(4):477–487. doi: 10.4187/respcare.00852. [DOI] [PubMed] [Google Scholar]
- 6.Vogelmeier C, Hederer B, Glaab T, et al. Tiotropium versus salmeterol for the prevention of exacerbations of COPD. N Engl J Med. 2011;364(12):1093–1103. doi: 10.1056/NEJMoa1008378. [DOI] [PubMed] [Google Scholar]
- 7.O’Donnell DE, Flüge T, Gerken F, et al. Effects of tiotropium on lung hyperinflation, dyspnoea and exercise tolerance in COPD. Eur Respir J. 2004;23(6):832–840. doi: 10.1183/09031936.04.00116004. [DOI] [PubMed] [Google Scholar]
- 8.Wise RA, Anzueto A, Cotton D, et al. Tiotropium Respimat inhaler and the risk of death in COPD. N Engl J Med. 2013;369(16):1491–1501. doi: 10.1056/NEJMoa1303342. [DOI] [PubMed] [Google Scholar]
- 9.Buhl R, Maltais F, Abrahams R, et al. Tiotropium and olodaterol fixed-dose combination versus mono-components in COPD (GOLD 2–4) Eur Respir J. 2015;45(4):969–979. doi: 10.1183/09031936.00136014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beeh K-M, Westerman J, Kirsten A-M, et al. The 24-h lung-function profile of once-daily tiotropium and olodaterol fixed-dose combination in chronic obstructive pulmonary disease. Pulm Pharmacol Ther. 2015;32:53–59. doi: 10.1016/j.pupt.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Global Initiative for Asthma Diagnosis of Diseases of Chronic Airflow Limitation: Asthma COPD and Asthma – COPD Overlap Syndrome (ACOS) [Accessed July 30, 2015]. [updated 2014]. Available from: http://www.goldcopd.org/uploads/users/files/AsthmaCOPDOverlap.pdf.
- 12.Roche N, Pribil C, Van Ganse E, et al. Real-life use of fluticasone propionate/salmeterol in patients with chronic obstructive pulmonary disease: a French observational study. BMC Pulm Med. 2014;14:56. doi: 10.1186/1471-2466-14-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drivenes E, Østrem A, Melbye H. Predictors of ICS/LABA prescribing in COPD patients: a study from general practice. BMC Fam Pract. 2014;15:42. doi: 10.1186/1471-2296-15-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Price D, West D, Brusselle G, et al. Management of COPD in the UK primary-care setting: an analysis of real-life prescribing patterns. Int J Chron Obstruct Pulmon Dis. 2014;9:889–905. doi: 10.2147/COPD.S62750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watz H, Ferguson GT, Grönke L, Vob F, Abrahams R, Buhl R. Inhaled corticosteroid plus long-acting β2-agonist therapy is overused in the treatment of patients with chronic obstructive pulmonary disease: post hoc analyses of two 1-year studies [abstract] Am J Respir Crit Care Med. 2015;191(Meeting Abstracts):A5784. [Google Scholar]
- 16.Tricco AC, Strifler L, Veroniki AA, et al. Comparative safety and effectiveness of long-acting inhaled agents for treating chronic obstructive pulmonary disease: a systematic review and network meta-analysis. BMJ Open. 2015;5(10):e009183. doi: 10.1136/bmjopen-2015-009183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bouyssou T, Casarosa P, Naline E, et al. Pharmacological characterization of olodaterol, a novel inhaled β2-adrenoceptor agonist exerting a 24-hour-long duration of action in preclinical models. J Pharmacol Exp Ther. 2010;334(1):53–62. doi: 10.1124/jpet.110.167007. [DOI] [PubMed] [Google Scholar]
- 18.Lange P, Aumann J-L, Derom E, et al. The 24-h FEV1 time profile of olodaterol QD delivered via Respimat® in COPD: results from two 6-week studies [abstract 4635] Eur Respir J. 2013;42(suppl 57):982s. [Google Scholar]
- 19.Ferguson G, Feldman G, Hofbauer P, et al. Lung function efficacy of olodaterol QD delivered via Respimat® in COPD patients: results from two 48-week studies [abstract 187] Eur Respir J. 2013;42(suppl 57):5s. [Google Scholar]
- 20.Beeh K-M, Derom E, Echave-Sustaeta J, et al. ENERGITO: efficacy and safety of once-daily combined tiotropium + olodaterol versus twice-daily combined fluticasone propionate + salmeterol; Abstract presented at: The European Respiratory Society International Conference; September 26–30, 2015; Amsterdam. [Google Scholar]
- 21.Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. Eur Respir J. 1993;6(suppl 16):5–40. doi: 10.1183/09041950.005s1693. [DOI] [PubMed] [Google Scholar]
- 22.Global Initiative for Chronic Obstructive Lung Disease Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2010. [Accessed August 12, 2015]. [updated 2010]. Available from: http://www.goldcopd.org/uploads/users/files/GOLDReport_April112011.pdf.
- 23.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 24.Kenward MG, Roger JH. The use of baseline covariates in crossover studies. Biostatistics. 2010;11(1):1–17. doi: 10.1093/biostatistics/kxp046. [DOI] [PubMed] [Google Scholar]
- 25.Pisi R, Aiello M, Zanini A, et al. Small airway dysfunction and flow and volume bronchodilator responsiveness in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:1191–1197. doi: 10.2147/COPD.S82509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones PW, Donohue JF, Nedelman J, Pascoe S, Pinault G, Lassen C. Correlating changes in lung function with patient outcomes in chronic obstructive pulmonary disease: a pooled analysis. Respir Res. 2011;12:161. doi: 10.1186/1465-9921-12-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singh D, Ferguson GT, Bolitschek J, et al. Tiotropium + olodaterol shows clinically meaningful improvements in quality of life. Respir Med. 2015;109(10):1312–1319. doi: 10.1016/j.rmed.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 28.Magnussen H, Disse B, Rodriguez-Roisin R, et al. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014;371(14):1285–1294. doi: 10.1056/NEJMoa1407154. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Additional exclusion criteria
| Patients with any of the following conditions were to be excluded: |
| A diagnosis of thyrotoxicosis (due to the known class side-effect profile of β2-agonists) |
| A diagnosis of paroxysmal tachycardia (>100 beats/min) (due to the known class side-effect profile of β2-agonists) |
| A history of myocardial infarction within 1 year of the screening visit |
| Unstable or life-threatening cardiac arrhythmia |
| Hospitalization for heart failure within the past year |
| Known active tuberculosis |
| A malignancy for which the patient has undergone resection, radiation therapy, or chemotherapy within the past 5 years (except for treated basal cell carcinoma) |
| A history of life-threatening pulmonary obstruction |
| A history of cystic fibrosis |
| Clinically evident bronchiectasis |
| A history of significant alcohol or drug abuse |
| Patients who have undergone thoracotomy with pulmonary resection |
| Patients being treated with oral or patch β-adrenergics |
| Patients being treated with oral corticosteroid medication within 6 weeks prior to Visit 1 |
| Patients who regularly use daytime oxygen therapy for >1 hour per day and, in the investigator’s opinion, will be unable to abstain from the use of oxygen therapy during clinic visits |
| Patients who have completed a pulmonary rehabilitation program in the 6 weeks prior to the screening visit or patients who are currently in a pulmonary rehabilitation program |
| Patients who have taken an investigational drug within 1 month, 6 half-lives, or within the washout period (whichever is greater) prior to screening visit (Visit 1) |
| Patients with known hypersensitivity to β-adrenergic drugs, BAC, EDTA, or any other component of the Respimat® inhalation solution, or lactose monohydrate |
| Pregnant or nursing women |
| Women of childbearing potential not using a highly effective method of birth control.a Female patients will be considered to be of childbearing potential unless surgically sterilized by hysterectomy or bilateral tubal ligation or if in postmenopausal stage for ≥2 years |
| Patients who have previously been randomized in this study or are currently participating in another study |
| Patients who are unable to comply with pulmonary medication restrictions prior to randomization |
Notes:
Defined as those methods that result in a low failure rate (ie, <1% per year) when used consistently and correctly as defined by the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use – Guidance on Nonclinical Safety Studies for the Conduct of Human Clinical Trials and Marketing Authorization for Pharmaceuticals M3(R2) guidelines.
Abbreviations: BAC, benzalkonium chloride; EDTA, ethylenediaminetetraacetic acid.
Table S2.
Adjusted mean FVC AUC0–12, AUC0–24, and AUC12–24 responses after 6 weeks of treatment: treatment differences (full analysis set)
| Treatment comparison
|
||||
|---|---|---|---|---|
| Tiotropium + olodaterol 5/5 µg versus
|
Tiotropium + olodaterol 2.5/5 µg versus
|
|||
| Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | |
| FVC AUC0–12, mL | ||||
| Adjusted mean (SE) | 218 (18)* | 215 (18)* | 183 (18)* | 180 (18)* |
| 95% CI | 184, 253 | 180, 250 | 149, 218 | 146, 215 |
| FVC AUC0–24, mL | ||||
| Adjusted mean (SE) | 176 (17)* | 177 (17)* | 140 (17)* | 141 (17)* |
| 95% CI | 144, 209 | 144, 209 | 108, 173 | 108, 173 |
| FVC AUC12–24, mL | ||||
| Adjusted mean (SE) | 135 (18)* | 138 (18)* | 98 (18)* | 101 (18)* |
| 95% CI | 100, 170 | 103, 174 | 63, 133 | 66, 136 |
Notes:
P<0.0001. The adjusted mean (SE) was obtained from fitting a mixed-effects repeated-measures model including the following: fixed effects of treatment and period; period baseline and patient baseline as covariates; patient as a random effect; compound symmetry covariance structure for within-patient variation; and Kenward–Roger approximation of denominator degrees of freedom.
Abbreviations: AUC0–12, area under the curve from 0 hour to 12 hours; AUC0–24, area under the curve from 0 hour to 24 hours; AUC12–24, area under the curve from 12 hours to 24 hours; CI, confidence interval; FVC, forced vital capacity; SE, standard error.
Table S3.
Adjusted mean FVC AUC0–3, trough FVC, and peak0–3 FVC responses after 6 weeks of treatment: treatment differences (full analysis set)
| Treatment comparison
|
||||
|---|---|---|---|---|
| Tiotropium + olodaterol 5/5 µg versus
|
Tiotropium + olodaterol 2.5/5 µg versus
|
|||
| Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | Salmeterol + fluticasone propionate 50/500 µg | Salmeterol + fluticasone propionate 50/250 µg | |
| FVC AUC0–3, mL | ||||
| Adjusted mean (SE) | 104 (13)* | 110 (13)* | 82 (13)* | 88 (13)* |
| 95% CI | 78, 130 | 84, 136 | 56, 108 | 62, 114 |
| Trough FVC, mL | ||||
| Adjusted mean (SE) | 145 (20)* | 137 (20)* | 120 (20)* | 112 (20)* |
| 95% CI | 106, 183 | 98, 176 | 81, 158 | 74, 151 |
| Peak0–3 FVC response, mL | ||||
| Adjusted mean (SE) | 215 (20)* | 213 (20)* | 172 (20)* | 169 (20)* |
| 95% CI | 176, 255 | 173, 253 | 133, 211 | 130, 209 |
Notes:
P<0.0001. The adjusted mean (SE) was obtained from fitting a mixed-effects repeated-measures model including the following: fixed effects of treatment and period; period baseline and patient baseline as covariates; patient as a random effect; compound symmetry covariance structure for within-patient variation; and Kenward–Roger approximation of denominator degrees of freedom.
Abbreviations: AUC0–3, area under the curve from 0 hour to 3 hours; CI, confidence interval; FVC, forced vital capacity; peak0–3 FVC, peak forced vital capacity from 0 hour to 3 hours; SE, standard error.