Abstract
Recently, development and research of nutraceuticals based on marine collagen peptides (MCPs) have been growing due to their high homology with human collagens, safety, bioavailability through gut, and numerous bioactivities. The major concern regarding safety of MCPs intake relates to increased risk of oxidative stress connected with collagen synthesis (likewise in fibrosis) and to ROS production by MCPs-stimulated phagocytes. In this clinical-laboratory study, fish skin MCPs combined with plant-derived skin-targeting antioxidants (AO) (coenzyme Q10 + grape-skin extract + luteolin + selenium) were administered to volunteers (n = 41). Skin properties (moisture, elasticity, sebum production, and biological age) and ultrasonic markers (epidermal/dermal thickness and acoustic density) were measured thrice (2 months before treatment and before and after cessation of 2-month oral intake). The supplementation remarkably improved skin elasticity, sebum production, and dermal ultrasonic markers. Metabolic data showed significant increase of plasma hydroxyproline and ATP storage in erythrocytes. Redox parameters, GSH/coenzyme Q10 content, and GPx/GST activities were unchanged, while NO and MDA were moderately increased within, however, normal range of values. Conclusions. A combination of MCPs with skin-targeting AOs could be effective and safe supplement to improve skin properties without risk of oxidative damage.
1. Introduction
Dietary vitamins, plant-derived polyphenols, fatty acids, proteins, essential amino acids, and trace elements have demonstrated beneficial effects on skin health and appearance [1–3]; hence, the use of nutraceuticals targeting skin is steadily growing. For example, photoprotection by intake of dietary antioxidants has been a subject of numerous in vitro, animal, and human studies [4, 5]. Within this direction, the search for reliable and effective antiageing remedies for both topical and systemic administration has become a “hot spot” for cosmetic, food, and biomedical companies. One of the strongest limitations for skin-targeting plant-derived dietary substances with potential antiageing efficacy is their low bioavailability due to limited and selective penetration through the intestinal barrier, destruction by the intestinal microorganisms, high rate of metabolism, and preferential distribution between tissues and organs [6, 7].
Marine fish collagen and collagen peptides have been widely used as functional foods or dietary supplements due to their homology to human collagen structure [8], safety profile [9], stability, biocompatibility, high bioavailability through gastrointestinal barrier [10], and potent bioactivities [11]. Marine collagen peptides (MCPs) obtained by enzymatic digestion of fish skin have been shown to exert several health effects mainly in two directions: metabolic disorders and skin/bone repair. Thus, they positively affected glucose and lipid metabolism in patients with type II diabetes mellitus [12], improved lipid metabolism in obese people [13] and genetically modified mice [14], ameliorated early alcoholic liver injury [15], and possessed hypotensive and lipid normalising action in patients with primary hypertension [16]. A great majority of publications demonstrated significant wound healing efficacy of orally administered MCPs in animal models of excision and full-thickness skin wounds [10, 17, 18]. Recently, collagen peptides isolated by enzymatic digestion from fish, bovine, and porcine skin as well as from chicken and bovine cartilage have drawn particular interest for the treatment of patients with osteoarthritis. Several clinical trials showed that MCPs were safe and provided an improvement in terms of pain and functions in such patients [19]. From mechanistic point of view, the oral intake of MCPs stimulated the synthesis of extracellular matrix (ECM) macromolecules such as endogenous collagen, by upregulating gene expression of several collagen-modifying enzymes involved in posttranslational collagen modification and cross-linking [20]. Several in vitro studies have shown antioxidant properties of very-low-molecular-weight (1–20 Da) MCPs [21, 22] containing proline, which is a scavenger of hydroxyl radicals. Of importance for the present study, MCPs are considered antiageing compounds because they seem to increase life span in rats by inhibiting spontaneous tumour incidence [9], possess photoprotective and immunomodulating properties [23–25], and improve/eliminate signs of premature senescence of human skin [26, 27].
The major concern regarding safety and clinical feasibility of regular intake of MCPs has been raised from the well established fact that the induction of collagen synthesis, mainly assessed by the increased hydroxyproline levels, is often associated with oxidative stress [28–30]. Moreover, MCPs of different origin have been shown to activate innate immune response of macrophages and neutrophils through Toll-like receptor 4, which leads to NADPH-oxidase (NOX4) activation and reactive oxygen species overproduction [31, 32]. A newly developed composition of MCPs with a complex of essential skin-targeting antioxidants, that is, coenzyme Q10 + selenium + luteolin + grape-skin extract, demonstrated UVA-protective effects in the preliminary in vitro experiments on human skin biopsies [25]. However, the composition under commercial name of CELERGEN® has never been evaluated clinically when administered as a food supplement.
The goal of the present clinical-laboratory study was to elucidate the effects of the oral administration of CELERGEN on skin physiology and dermal collagen deposition in the group of healthy middle-aged subjects with clinical signs of skin ageing. The cutaneous clinical-instrumental data were compared with the systemic metabolic parameters of collagen synthesis, redox balance, and energy storage. For the first time, we demonstrated (i) remarkable improvement of ageing skin physiology and structure, which corresponded to enhanced systemic markers of collagen synthesis; (ii) systemic redox balance, sustained by the antioxidant complex; and (iii) increased systemic energy storage. We also hypothesised that moderately increased plasmatic levels of nitric oxide (NO) and malonyl dialdehyde (MDA) may play positive roles of mediators in the MCPs-induced collagen and ATP synthesis/storage, as well as in sebum production. On these grounds, we suggested that selected antioxidants targeting the distinct organs/tissues should be essential components of MCPs-containing nutraceuticals for more effective, individualised, and safe supplementation.
2. Materials and Methods
2.1. Patients
The study enrolled a group of 41 adult healthy Caucasian volunteers of both sexes recruited from the Beauty Institute on Arbat (Moscow, Russia) staff (age 37–72 years; mean age 50.6 ± 10.4 years; 5 males and 36 females) following the exclusion and inclusion criteria for an open single-blind clinical study. The inclusion criteria were as follows: (i) healthy white adult subjects of both sexes, 35–75 years of age, (ii) subjects with visible symptoms of aged facial skin, (iii) subjects who agreed to interrupt any intake of antioxidant nutraceuticals/drugs for at least 1 week before and during the entire duration of the trial, and (iv) subjects without any difficulty to understand and follow the clinical investigator instructions. Pregnant and breastfeeding women, subjects with allergic/intolerance reactions to any component of the tested product, subjects on any other nutraceutical interventions or/and therapies, and subjects simultaneously engaged in other clinical trials were excluded from the study. The participants were informed that they could interrupt clinical trial at any moment, without any explanation of causative reason for their action, or in case they noticed any adverse reaction to the tested product or had any sensation that the product intake affected their appearance negatively.
The protocol of the clinical trial was duly analysed and approved by the Ethical Committee of the Beauty Institute on Arbat, Moscow, Russia (number 11/EK-2014). All recruited subjects gave their informed consent to personal and anamnestic data collection and biological material sampling. The guidelines of Helsinki Declaration for human experimentation were strictly followed during the conduct of the clinical trial.
2.2. Food Supplement under Investigation
Food supplement containing marine collagen peptides derived from skin of deep sea fish (MCPs, 570 mg), grape-skin extract (10 mg), coenzyme Q10 of plant origin (10 mg), luteolin (10 mg), and selenium (0.05 mg) of plant origin was formulated in soft gelatine capsules. As inactive solvents, refined and partly hydrogenated soybean oil as well as small admixture of pure soybean lecithin were used. The product, under the commercial name of CELERGEN (manufacturer: Laboratories-Dom, Carouge, Switzerland), was kindly provided by Suisse Ueli Corporation. According to the manufacturer's information, the deep sea fish sources, that is, Pollachius virens, Hippoglossus hippoglossus, and Pleuronectes platessa, originated from the French coast of the North Sea.
Fish skin was homogenised in distilled water, with addition of complex proteases. The enzymatic proteolytic process was carried out at 40°C and pH 8.0 for 3 h, after which the proteases were inactivated by short-term heating (56°C for 10 min). The liquid was sterilised by Millipore filtration (pore size 0.02 mm) and spray-dried to prepare MCP powder, as described in detail previously [17, 33]. Chemical analysis by Kjeldahl assay of the powder confirmed a >90% content of collagen peptides, with moisture and ash content <10%. According to previous publications [10, 33, 34], the molecular weight distribution of MCPs after the described enzymatic digestion process was within the range of 10–60 Da, and MCPs were enriched in glycine, glutamine, proline, hydroxyproline, asparagine, alanine, and arginine.
The aqueous extract of grape skin was obtained from Vitis vinifera Linn. fruit and contained at least 70% of polyphenols and 20% of procyanidins as per UV/Vis spectrophotometry data. The coenzyme Q10 component of plant origin was of highest purity (100 ± 3%), confirmed by both IR spectrophotometry and high performance liquid chromatography (HPLC) methods. Food-quality luteolin was extracted from Marigold plant petals, and the extract contained 20% of luteolin and 1% of zeaxanthin evaluated by HPLC analysis. Selenium in the form of selenite (according to gravimetric method) was extracted from plant bulbs and leaves. Acute and chronic toxicity data and documents of Certificates of Analyses, Security, and Registration in Switzerland were duly provided by the manufacturer.
2.3. Clinical Study Design
The entire trial duration was 4 months (May–December 2014), that is, 2 months of pretreatment period, followed by 2 months of treatment with the test nutraceutical administration. The facial skin parameters of recruited volunteers were analysed three times: at the first visit (enrollment), at the second visit 2 months after the pretreatment period, and at the third visit immediately after the treatment period. Each assessment session comprised instrumental methods for measuring skin physiology parameters and ultrasound properties of the skin layers. This design allowed us to use the same subject as a control and an experiment. During the treatment period, the volunteers were recommended to take 2 capsules of CELERGEN a day (at breakfast and dinner time) for 60 consecutive days. At the second and third visits, the participants donated 20 mL of venous blood after overnight fasting and test tubes were coded by the principal clinical investigator. Blood samples were routinely processed for general haematology (haemoglobin content, differential cell count, and the rate of erythrocyte sedimentation) and biochemistry (glucose levels, plasma protein and lipid profiles, transaminases activities, and C-reactive protein content). Laboratory operators carried out analytical determinations blindly, and statistician was not informed which set of analyses was done in the control or experimental periods, hence ranking this study of clinical efficacy of the nutraceutical as “a single-blind” clinical investigation.
2.4. Assessment of Skin Physiology Parameters
Several physiological parameters, mainly barrier properties, of the facial skin were assessed by appropriate SOFT PLUS TOP probes, with microcamera visual analysis and patented computerised programs (Callegari, Parma, Italy). Skin elasticity was determined by the elastometric approach used in the SOFT PLUS technique. The transepidermal water loss (TEWL), an index of skin moisture, was assessed with Tewameter, which measures the water evaporation through cutaneous levels. When the skin is aged or damaged, the barrier properties of the skin are affected, with increased water evaporation and reduced skin hydration. Sebum content was measured by the SOFT PLUS sebometric probe.
2.5. Assessment of Ultrasound Properties of the Skin
Assessment of ultrasound properties of the skin was performed by a digital ultrasound imaging system DUB CUTIS (Digital Ultraschall Bildsystem, Germany), which allowed determining four parameters simultaneously: epidermal and dermal thickness and epidermal and dermal ultrasonic density. The first two parameters are indirect markers of collagen (dermis) and lipid (epidermis) synthesis and retention while the second pair of parameters characterises the evenness and order in the epidermal and dermal structures, respectively. The elastic properties of the skin were additionally analysed by a TPM system containing elastometric sensor (22 MHz) which combines digital ultrasound examination with an imaging record (DUB CUTIS, Germany). A computerised multifunctional diagnostic tool integrating different morphometric parameters (epidermal thickness, tone, wrinkles, and elasticity) for face skin biological age determination was used (SOFT PLUS TOP, Callegari, Parma, Italy).
2.6. Reagents and Assay Kits
The majority of chemical reagents, HPLC standards, mediums, solvents, and luciferin-luciferase for ATP assay were from Sigma Chemical Co. (St. Louis, MO, USA); kits for enzyme activity assays and Griess reagent for nitrites/nitrates determination were from Cayman Chemical Company (Ann Arbor, MI, USA). Manufacturers of other reagents are mentioned within the respective methods.
2.7. Redox and Oxidation Markers' Studies
Complete differential blood cell counts and metabolic analyses were performed on fresh ethylenediaminetetraacetic acid- (EDTA-) anticoagulated venous blood of 12 hrs fasting subjects. Biochemical assays were performed on peripheral blood plasma or red blood cells (RBC), either immediately (ATP, glutathione, and coenzyme Q10) or within 72 hrs, on sample aliquots stored at −80°C under argon. Plasma levels of nitrites/nitrates (NO2 −/NO3 −, expressed as μmoles/L) were measured spectrophotometrically by Griess reagent [35]. Protein content was measured according to Bradford [36], using a microplate assay kit (Bio-Rad, Hercules, CA, USA). Total glutathione (reduced + oxidized glutathione, GSH + GSSG, mg/g Hb) levels in erythrocytes were measured by HPLC (Shimadzu Scientific Instruments, Columbia, MD, USA) according to Reed et al. [37]. Total coenzyme Q10 (CoQ10H2 + CoQ10, mg/L) levels in plasma were quantified by HPLC as described previously [38]. In brief, 1 mL plasma sample, with adequate amount of coenzyme Q9 (internal standard) and 500 μL acetic acid (50% solution), was extracted twice, first with 3.5 mL and then with 2.5 mL of ethanol/hexane mixture (2 : 5 vol/vol), with homogenisation and subsequent centrifugation. The upper phase containing hexane extract was evaporated under nitrogen flux and then resuspended in an adjusted amount of a methanol/isopropanol (3 : 2 vol/vol) mixture for HPLC analysis. Reduced and oxidized forms of coenzyme Q10 (CoQ10H2 and CoQ10) were quantified simultaneously with HPLC equipped with analytical Supelcosil LP-18 column (24 cm × 4.6 mm, 5 μm, Supelco, Bellefonte, PA, USA) plus its guard column, and in line photodiode array and electrochemical detector (ESA CoulArray, Bedford, MA, USA) in accord with previously published methods [39, 40]. The clinical normality range was extrapolated from the above publications.
Plasmatic Cu,Zn-superoxide dismutase 3 (Cu,Zn-SOD3, U/g protein) activity was measured spectrophotometrically at 505 nm using appropriate kit from Cayman Chemical Company (Ann Arbor, MI, USA) [41, 42]. RBC were lysed in hypotonic solution and the postspin cell lysates were analysed. Total RBC glutathione-S-transferase (GST, U/mg Hb) activity was measured spectrophotometrically by the methods described previously, using chloro-2,3-dinitrobenzene as substrate [43]. RBC glutathione peroxidase (GPx, U/g Hb) activity was determined using Cayman Chemical kit, according to the method [44].
Plasma levels of MDA were determined by slightly modified spectrophotometric analysis of thiobarbituric acid-reactive substances (TBARS) described elsewhere [45]. After a 15 min treatment of plasma (200 μL) with trichloroacetic (1.22 M) and hydrochloric (0.6 M) acids, alkaline solution of TBA was added and the mixture was boiled for 30 min. TBARS were extracted with butanol and analysed spectrophotometrically at 535 nm. The results were expressed in μM of MDA using the appropriate calibration curve.
2.8. ATP Measurement in Erythrocytes
100 μL of erythrocyte pellet was stored on ice until analysis. Ice-cold water (990 μL) was added to 10 μL of the erythrocytes pellet and mixed and the lysed erythrocytes were kept on ice. The principle of ATP assay is based on the quantitative bioluminescent determination of adenosine 5′-12 triphosphate (ATP), assessed by the Bioluminescence Assay Kit. In the assay, ATP is consumed when firefly luciferase catalyses the oxidation of D-luciferin to adenyl-luciferin which, in the presence of oxygen, is converted to oxyluciferin with light emission. This second reaction is essentially irreversible. When ATP is the limiting reagent, the light emitted is proportional to the ATP present. The measurements of luciferin-luciferase chemiluminescence were performed on a Victor2 1420 multilabel counter, equipped with Wallac 1420 Software (Perkin Elmer, MA, USA). Results were expressed as mmoles/L.
2.9. Hydroxyproline Assay
The plasma levels of free hydroxyproline (Hyp) and hydroxyproline in the form of oligopeptides, mainly proline-hydroxyproline, were determined by a chemical colorimetric method using a commercial kit (Hydroxyproline Detection Kit) in accord with the manufacturer's instructions. Hyp concentrations were quantified in the linear range of its calibration curve using an array reader (Bio-Rad, Hercules, CA, USA) and expressed in μg/mL of plasma.
2.10. Statistical Analysis
Statistical analysis of clinical data was carried out using WINSTAT programs for personal computers (Statistics for Windows 2007, Microsoft, USA). All biochemical and molecular measurements were done in triplicate and data were statistically evaluated. Values were presented as mean, standard error of the mean, and 1.96 × standard error of triplicate analyses. When several datasets were compared, data were analysed by Student's t-test for unpaired data. Differences between initial/final data for a single participant were analysed by paired t-test and by Mann-Whitney test for changes from baseline. All reported p values are from two-tailed tests, and p values of less than 0.05 were considered to indicate statistical significance.
3. Results
3.1. Subjective Evaluation by Participants and Clinical Investigators
All healthy volunteers (n = 41) recruited in the trial duly completed it. There were no drop-offs due to low compliance or adverse effects of the supplementation. Routine haematological and biochemical analyses, which were carried out after blood donation in the beginning and after the cessation of the study, did not show statistically significant changes possibly reflecting adverse consequences of the test nutraceutical in the prescribed dosages (data not shown). The subjective evaluation of the product effects on selected general health parameters is shown in Table 1. The participants were predominantly satisfied with the effects obtained on general health conditions and skin properties and partly also by enhanced muscle strength and stamina. No effect whatsoever on digestion was registered.
Table 1.
Subjective evaluation of the 2-month food supplement administration effects, by participants (n = 41).
| Parameter | Number (%) of participants | ||
|---|---|---|---|
| Improvement | No effect | Aggravation | |
| General health conditions | 21 (51%) | 20 (49%) | 0 (0%) |
| Stamina/muscle strength/joint motility | 15 (36%) | 26 (64%) | 0 (0%) |
| Digestive system | 0 (0%) | 41 (100%) | 0 (0%) |
| Skin conditions | 25 (61%) | 16 (39%) | 0 (0%) |
3.2. Effects on Facial Skin Properties
Comparison of digital photos taken before and after clinical trial showed visible qualitative improvement of aesthetic aspect of face with pronounced lifting effect (data not shown).
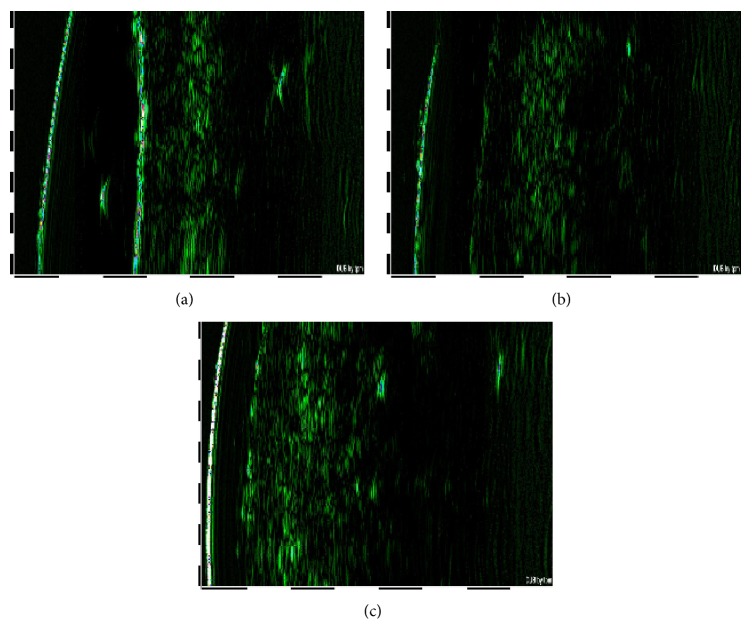
Characteristic digital images of ultrasound examinations made at trial beginning (2 months before the beginning of supplementation), at the first day of nutraceutical administration, and immediately after the trial cessation are shown, respectively, in Figures 1(a), 1(b), and 1(c). The individual ultrasonic characteristics were rather stable and were not subjected to statistically significant changes during the 2 months of pretreatment period (Tables 2 and 3; compare columns 1 and 2). The analysis of individual data showed that highly enhanced dermal thickness and homogenous distribution of collagen fibers in dermis were detectable in 23% (n = 11) of the participants after the trial cessation. Statistical evaluation of dermal thickness and acoustic density revealed significant changes exclusively at the third visit (Table 2), while the ultrasonic properties of epidermis remained unchanged (Table 3).
Figure 1.
Digital images of facial skin ultrasound examinations (patient number 23, e.g.), made 2 months before the beginning of the trial (a), at the day of the trial beginning (b), and immediately after the trial cessation (c).
Table 2.
Effects of the 2-month food supplement administration on the ultrasonic properties of the dermis (n = 41).
| Parameter | Dermis | ||
|---|---|---|---|
| Pretreatment period | Before treatment | After treatment | |
| Thickness, μm | 3884 ± 30 | 3900 ± 31 | 4133 ± 28∗ |
| Acoustic density | 5.2 ± 0.2 | 5.1 ± 0.2 | 6.3 ± 0.1∗ |
∗ p < 0.05 versus “before treatment.”
Table 3.
Effects of the 2-month food supplement administration on the ultrasonic properties of the epidermis (n = 41).
| Parameter | Epidermis | ||
|---|---|---|---|
| Pretreatment period | Before treatment | After treatment | |
| Thickness, μm | 76.9 ± 1.0 | 77.0 ± 0.8 | 77.6 ± 0.9 |
| Acoustic density | 35.6 ± 2.4 | 35.2 ± 2.2 | 35.4 ± 2.0 |
Analyses of the main physiological parameters of the skin relevant to ageing, such as elasticity, moisture, and sebum content, demonstrated their comparative stability in the pretreatment period, as there were no significant changes between the first and the second sets of measurements (Table 4, columns 1 and 2). Conversely, CELERGEN administration statistically significantly enhanced skin elasticity and sebum production (p < 0.0001), whilst not influencing cutaneous moisture (Table 4, columns 2 and 3). Biological age, calculated on the basis of ultrasound and cutaneous physiology measurements, tended to decrease after the trial; however, the difference did not reach statistical significance.
Table 4.
Effects of the 2-month food supplement administration on the parameters of skin physiology (n = 41).
| Parameter | Pretreatment period | Before treatment | After treatment |
|---|---|---|---|
| Elasticity | 34.06 ± 1.54 | 33.66 ± 1.21 | 40.26 ± 0.87∗∗∗ |
| Moisture | 48.83 ± 3.02 | 49.03 ± 3.52 | 46.54 ± 3.02 |
| Sebum | 29.89 ± 4.16 | 29.37 ± 4.76 | 56.86 ± 4.04∗∗∗ |
| Skin biological age | 50.11 ± 1.91 | 49.51 ± 1.68 | 48.09 ± 1.74 |
∗∗∗ p < 0.0001 versus “before treatment.”
It should be noticed that all tested parameters of skin physiology and structure were not subjected to temporal fluctuations during the 2-month pretreatment period, and therefore changes observed can be viewed as a result of CELERGEN administration.
3.3. Plasmatic Oxidation Markers and Antioxidants
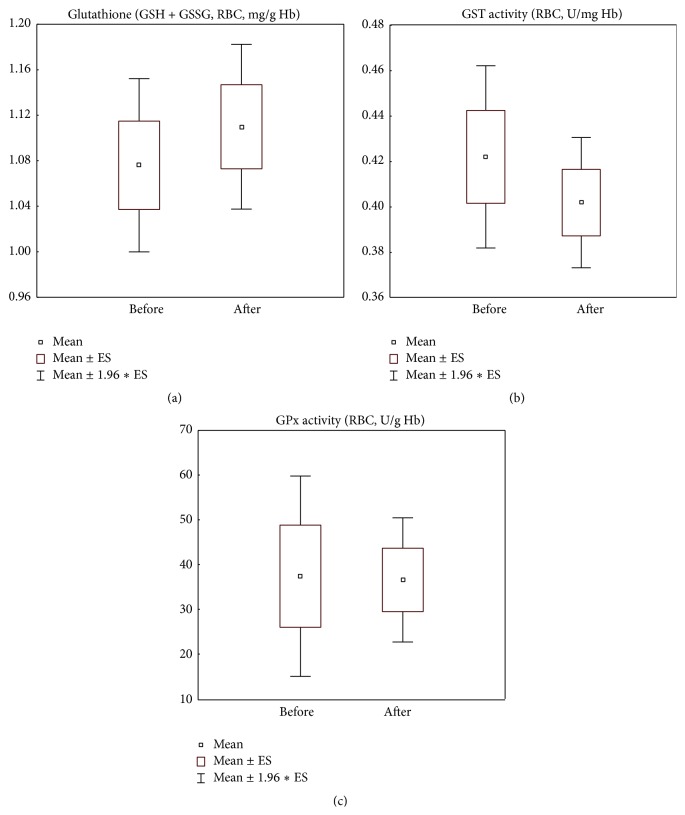
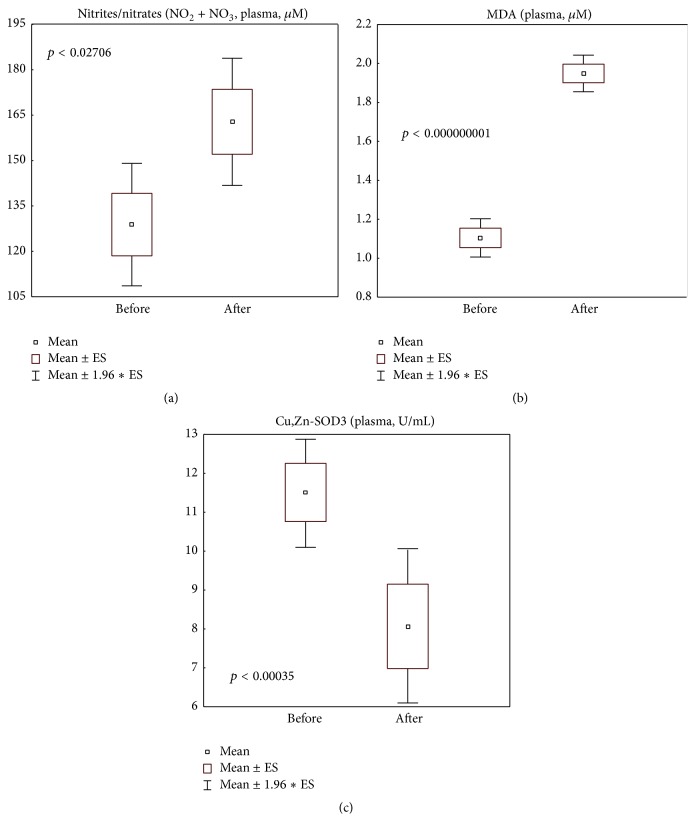
Surprisingly, CELERGEN administration did not affect several markers of glutathione metabolism such as total glutathione levels (normality range: 0.5–1.6 mg/g Hb) and glutathione-S-transferase and glutathione peroxidase activities (normality ranges: 0.2–0.7 U/mg Hb and 18.0–54.0 U/g Hb, resp.) (Figures 2(a), 2(b), and 2(c)). At the same time, nitrite/nitrate and MDA levels in plasma (normality ranges: 70.3–221.0 μM and 1.0–2.2 μM, resp.) were statistically significantly increased (p < 0.05 and p < 0.0001, resp.), although they remained within normal physiological range established in our laboratory (Figures 3(a) and 3(b)). Extracellular Cu,Zn-SOD3 activity was slightly suppressed (p < 0.001) but did not drop below the normality border (5.0–20.1 U/mL) (Figure 3(c)).
Figure 2.
Glutathione cycle parameters: erythrocyte levels of total glutathione (reduced and oxidized forms, GSH + GSSG) (a) and erythrocyte enzymatic activities of glutathione-S-transferase (b) and of glutathione peroxidase (c) in the study group of patients (n = 41), before and after food supplement administration period. Values are represented as mean (□), standard error of the mean (upper and lower limits of the box), and 1.96 × standard error (upper and lower whiskers). GSH: reduced glutathione; GSSG: oxidized glutathione; RBC: red blood cells; Hb: haemoglobin; GST: glutathione S-transferase; GPx: glutathione peroxidase. Reference normality range: RBC total glutathione (0.5–1.6 mg/g Hb); RBC GST activity (0.2–0.7 U/mg Hb); RBC GPx activity (18.0–54.0 U/g Hb).
Figure 3.
Systemic oxidative stress markers: plasma levels of nitrites/nitrates (NO2 + NO3) (a), of malonyl dialdehyde (MDA) (b), and of Cu,Zn-superoxide dismutase 3 (Cu,Zn-SOD3) (c) in the study group of patients (n = 41), before and after food supplement administration period. Values are represented as mean (□), standard error of the mean (upper and lower limits of the box), and 1.96 × standard error (upper and lower whiskers). Intergroup significant differences (p) are indicated in the relative panels. NO2 + NO3: nitrites + nitrates; MDA: malonyl dialdehyde. Reference normality range: plasma NO2 + NO3 (70.3–221.0 μM); plasma MDA (1.0–2.2 μM); plasma Cu,Zn-SOD3 (5.0–20.1 U/mL).
3.4. Parameters of Collagen and ATP Metabolism
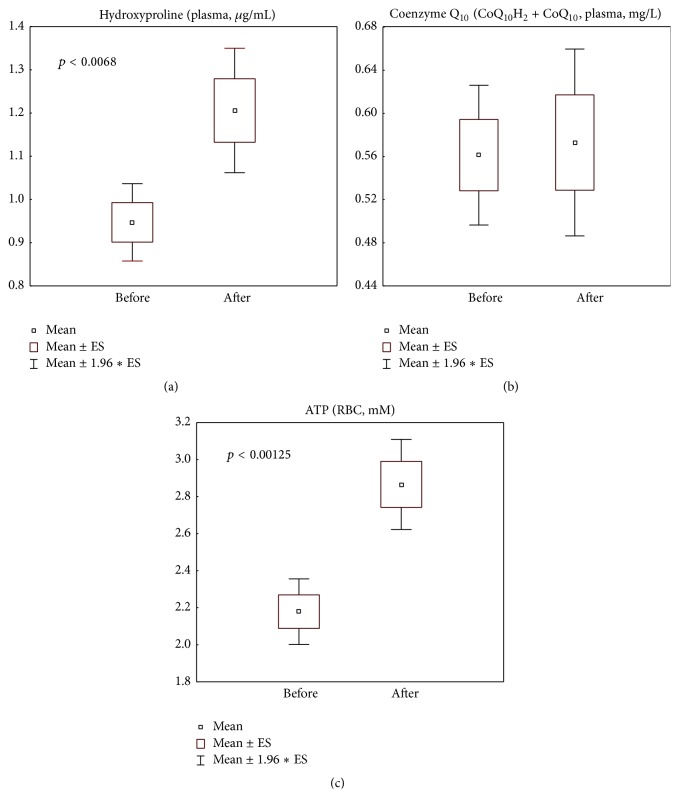
Plasma content of hydroxyproline was found highly elevated (p < 0.01) (Figure 4(a)), the same with ATP content in erythrocytes (p < 0.001) (Figure 4(c)), although total content of coenzyme Q10 was not changed after supplementation with the coenzyme Q10-containing nutraceutical (Figure 4(b)).
Figure 4.
Metabolic parameters related to collagen and ATP synthesis: levels of plasma hydroxyproline (a) and of the lipophilic antioxidant total coenzyme Q10 (reduced and oxidized forms, CoQ10H2 + CoQ10) (b) and erythrocyte ATP (c) in the study group of patients (n = 41), before and after food supplement administration period. Values are represented as mean (□), standard error of the mean (upper and lower limits of the box), and 1.96 × standard error (upper and lower whiskers). Intergroup significant differences (p) are indicated in the relative panels. CoQ10H2: reduced coenzyme Q10; CoQ10: oxidized coenzyme Q10; ATP: adenosine triphosphate; RBC: red blood cells. Reference normality range: total coenzyme Q10 (0.4–1.6 mg/L); ATP (1.0–4.0 mM).
4. Discussion
In a preliminary ex vivo study of CELERGEN components against UVA-induced damage in human skin biopsies and fibroblasts [25], marine collagen peptides but not the complex of plant-derived antioxidants inhibited transcriptional and posttranscriptional matrix metalloproteinase-1 and elastase upregulation, leading the authors to hypothesise clinical feasibility for the prevention of skin photoaging. In contrast, another publication demonstrated that the bioflavonoid luteolin, a component of the CELERGEN antioxidant complex, effectively attenuated UVB-induced DNA damage, inflammation, and ROS overproduction in skin cells in vitro and in vivo [46].
In the present study, we obtained convincing clinical data on the efficacy of the marine collagen peptide and plant antioxidant formulation CELERGEN in improving dermal collagen deposition and structure (Table 2), as well as skin elasticity (Table 4). These effects were consistent with enhanced plasma levels of hydroxyproline, a systemic metabolic marker of collagen synthesis (Figure 4(a)). Nearly 100% of human Hyp is in fact found in collagen [47]. Hyp being an oxidative derivative of proline, both amino acids are essential for collagen biosynthesis, maturation, mode of deposition, and collagen fiber structure. Dietary proline intake promotes tissue repair in humans and animals [48]. Recently, Wang et al. [17] reported the experimental evidence that MCPs might improve collagen synthesis and maturation by inducing the expression of transforming growth factor beta-1 (TGF-β1) and basic fibroblast growth factor (bFGF). Our data (Figure 4(a)) are consistent with previously published ones on rats fed with MCPs from salmon or trout skin [49], showing that plasma levels of free and dipeptide (Pro-Hyp) forms of hydroxyproline were highly increased after single intake of MCPs in soybean oil. Similar data on the blood levels of Hyp and Hyp-containing peptides were obtained on healthy human volunteers [50].
Numerous animal studies on the effects of oral administration of natural or synthetic antioxidants towards collagen deposition, reactive species levels, and antioxidant defences generated highly conflicting data, depending on the experimental system. Thus, with various wound healing models, it was repeatedly demonstrated that either complex plant extracts containing active secondary metabolites (triterpenes, polyphenols, alkaloids, etc.) [18, 51] or a composition of collagen inducing polysaccharides like chitosan and antioxidants such as curcumin [52] or resveratrol [53] ameliorated wound healing increasing skin collagen deposition, while suppressing proinflammatory iNOS and myeloperoxidase, decreasing pathologically elevated levels of MDA and hydrogen peroxide, and improving enzymatic antioxidant defence. Recent studies showed that collagen peptides from fish skin remarkably promoted both wound healing and angiogenesis in different experimental settings [10, 17]. Of importance, excessive NO produced during the inflammatory phase of wound healing process impaired collagen accumulation [54], while moderate NO levels accelerated the granulation phase of wound closure [18, 55]. Moreover, wound healing acceleration by moderate levels of H2O2 through induction of vascular endothelial growth factor in keratinocytes and macrophages was proved in a number of experimental and clinical studies [56, 57]. Here, we found that, along with Hyp accumulation, plasma levels of nitrites and nitrates, related to NO production in the bloodstream, were moderately increased after CELERGEN treatment, though remaining within the range of normal values (Figure 3(a)). Similar results were obtained with plasmatic MDA (Figure 3(b)). This allowed us to suggest that redox regulation of cutaneous collagen synthesis process or/and fibroblast proliferation activation could have occurred due to physiologically relevant NO and/or MDA amounts generated following supplement intake. However, the suggestion deserves further mechanistic in vitro and clinical research.
On the other hand, in the models of cardiac fibrosis [58, 59], the significant decrease of the model-related oxidative stress obtained by the use of Momordica charantia fruit extract [58] or Fructose Chorpondiatis total flavonoids was indeed associated with simultaneous attenuation of collagen deposition, as assessed by Hyp levels. Similar results were obtained in other tissue models of fibrosis [28, 60–62], including skin fibrosis [29]. It seems that complex mixtures of fruit extracts contained both collagen synthesis affecting agents and antioxidants.
UV irradiation could cause skin photodamage causing the symptoms of premature photoageing. Evaluating the photoprotective effects of dietary MCPs isolated from jellyfish umbrella [24] or from fish scale [63] in the model of chronic UVA + UVB irradiation of mice, the authors concluded that MCPs enhanced skin immunity, reduced water loss, restored cutaneous collagen and elastin levels and structure, and maintained type III to I collagen ratio. Under similar experimental design, Zhuang et al. [64] showed the protective action of MCPs on antioxidant enzymes activities and glutathione, lipid, and Hyp contents of murine skin. In this connection, we found a significant reduction (within the range of normality) of plasmatic SOD3 activity following CELERGEN supplementation (Figure 3(c)). Extracellular plasmatic Cu,Zn-SOD3, a glycoprotein with a heparin-binding domain, is predominantly expressed in tissue ECM, where it is bound to heparin sulfate proteoglycan [65]. Physiologically, SOD3 maintains redox balance and tissue homeostasis and modulates innate and adaptive immune responses. Cutaneous homeostasis strongly depends on the ECM microenvironment; therefore, an elevated SOD3 activity may be a marker of adaptive response against intrinsic age-associated and external hazardous factors inducing immune suppression in the skin [66].
Since the supplementation of compounds with a direct antioxidant effect has failed so far to show clinical efficacy and sometimes even aggravated clinical picture [67], the search for drugs/therapeutic strategies to modulate oxidative stress has been drastically redirected nowadays towards (1) indirect AOs inducing endogenous enzymatic system of antioxidative defence, mainly, through Nrf2-connected pathway; (2) selective inhibitors of ROS/RNS-producing enzymes, for example, different isoforms of NADPH-oxidase, having shown definite clinical effects; (3) recognising essential and multiple physiological roles of redox balancing agents rather than mere inhibitors of free radical processes. Plant-derived polyphenols, quercetin, resveratrol, luteolin, and many others appear to possess all these multipotent capabilities [6]. The presence of quercetin and resveratrol from grape-skin extract and of luteolin in the antioxidant combination of CELERGEN may then well account for the observed redox balancing effects during the upregulation of MCPs-induced collagen synthesis (Figures 2(a), 2(b), and 2(c)). The majority of publications have in fact demonstrated a drop of GSH content and an increase of protective GPx activity when Hyp content was raised [28, 64, 68]. Of great importance, the presence of antioxidants in the tested formulation, whilst possibly protecting the redox balance from harmful side effects of collagen metabolism, did not negatively affect the desired process of dermal collagen synthesis/deposition. In fact, the observed elevation of plasmatic Hyp was comparable with that found previously [27], with pure fish MCPs in much higher dosages.
In the last decade, endogenously produced systemic and cutaneous redox-active substances (superoxide, hydrogen peroxide, NO, lipid peroxides, stable end products of lipid peroxidation, oxidative metabolites of cholesterol and squalene, etc.), previously recognised exclusively as undesirable metabolic by-products and markers of oxidative damage, have shown essential functions in cellular signalling and regulation of cell proliferation, differentiation, migration, innate immunity, energy production, ECM dynamics, vascular tone, stress responses and adaptation, and inflammation [55, 69–71]. In this frame, the moderate plasmatic elevation of MDA (Figure 3(b)) and NO (Figure 3(a)) observed in this study may reflect the regulatory functions of these mediators both in MCPs-induced collagen synthesis (Figure 4(a)) [69] and in the process of mitochondrial ATP production (Figure 4(c)). Only excessive amounts are damaging as they initiate cell senescence and death. It seems that, notwithstanding coenzyme Q10 supplementation during CELERGEN course, its plasmatic levels were not increased (Figure 4(b)), due to elevated consumption of the coenzyme in the mitochondrial cycle of energy production enhancing ATP storage in erythrocytes (Figure 4(c)) and in cell redox balance control (Figures 2(a)–2(c)).
The antiageing effects of CELERGEN supplementation were evidenced also by the highly increased sebum production (Table 4). It is established that the production of sebaceous lipids is strongly age dependent, being low in the prepubertal period, rising with sexual maturation, and gradually declining in the aging populations (starting from 46–55 years) [72] or in UV-induced premature skin ageing [70, 73]. Cutaneous lipid-soluble antioxidants such as vitamin E and squalene decay accordingly [74]. Since skin surface lipids (SSL) play multiple essential roles in skin barrier properties, skin smoothness, elasticity, and moisture, they are regarded as natural guards of normal cutaneous ecology. Moreover, moderate concentrations of specific SSL unsaturated components (squalene, cholesterol, and free fatty acids) are able to generate oxidised lipid by-products (MDA, 4-hydroxynonenal, oxidised cholesterol, and others), since being long recognised as key signalling molecules for skin immune and metabolic responses to environmental insults and microbial invaders [70, 75, 76]. On the other hand, excessive levels of microbially or photooxidised derivatives of unsaturated fatty acids and other sebum lipids could induce a vicious cycle of sebum overproduction followed by oxidation, thus maintaining inflammation characteristic for acne disease [76]. As shown by our clinical data (Table 1), no complaints about skin conditions were registered during the trial. Conversely, the marked improvement of skin elasticity could be attributed not only to collagen deposition in derma, but also to a moderate physiological increase of SSL content.
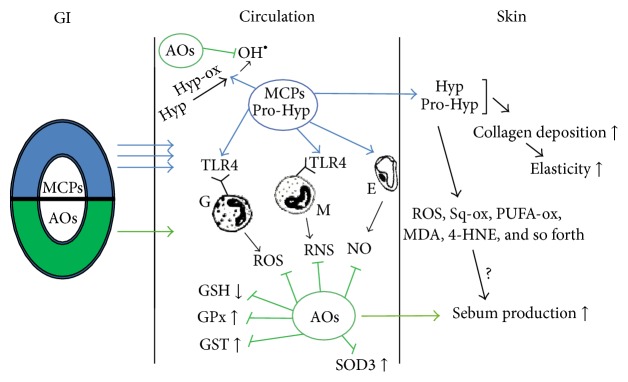
On the grounds of the results obtained and existing literature data, we hypothesised redox-dependent pathways (Figure 5) which may lead to clinical and generalised health effects of CELERGEN supplementation. Obviously, more profound basic research and further clinical studies are needed to prove this hypothesis and to evaluate the underlying mechanisms.
Figure 5.
Scheme of the hypothesised redox-dependent mechanisms of CELERGEN physiological effects. Marine collagen peptides (MCPs) easily penetrate gastrointestinal wall (GI, three arrows) and through blood circulation are mainly deposited in the skin. Antioxidant component of the nutraceutical is partly metabolised in GI thus possessing low bioavailability (one arrow); however, skin-targeting antioxidants and their metabolites reach different skin layers. While in the circulation, MCPs stimulate blood phagocytes (granulocytes and monocytes) and endotheliocytes (E) to produce reactive oxygen species (ROS) and reactive nitrogen species (RNS) by activating Toll-like receptors 4 (TLR4). Hydroxyproline (HYP) and prolyl-hydroxyproline (Pro-HYP) dipeptides as major components of MCPs are metabolised by corresponding oxidases and hydroxyl radicals are formed as by-products. Antioxidants prevent systemic oxidative stress blocking GSH oxidation, GPx, GST, and SOD3 activation. In the skin, collagen synthesis and deposition as well as elasticity are increased while (hypothetically) low levels of oxidised forms of skin lipids such as unsaturated fatty acids (PUFA-ox), squalene (Sq-ox), malonyl dialdehyde (MDA), and 4-hydroxy-2-nonenal (4-HNE) may facilitate cell signalling for ATP synthesis and sebum production.
5. Conclusions
The addition of dietary plant-derived antioxidants with known skin tropism and health effects towards human skin did not impair definite induction of collagen synthesis and its deposition as compact organised fibres in the dermal layer by marine fish skin-derived collagen peptides. Additional beneficial effects of antioxidants were observed systemically, as normal balance of systemic endogenous antioxidant defence was maintained, and protection of energy storage occurred.
Acknowledgments
The authors gratefully acknowledge Suisse Ueli Corporation for providing the product for the clinical study free of charge and for covering the costs of reagents and analyses. They are also grateful to Elena Schukina for excellent technical assistance and to Valeriy Chertushkin for organisation of the trial logistics.
Abbreviations
- MCPs:
Marine collagen peptides
- ECM:
Extracellular matrix
- NOX4:
NADPH-oxidase
- NO:
Nitric oxide
- MDA:
Malonyl dialdehyde
- HPLC:
High performance liquid chromatography
- TEWL:
Transepidermal water loss
- EDTA:
Ethylenediaminetetraacetic acid
- RBC:
Red blood cells
- Cu,Zn-SOD3:
Cu,Zn-superoxide dismutase 3
- GST:
Glutathione-S-transferase
- GPx:
Glutathione peroxidase
- TBARS:
Thiobarbituric acid-reactive substances
- Hyp:
Hydroxyproline
- TGF-β1:
Transforming growth factor beta-1
- bFGF:
Basic fibroblast growth factor
- ROS:
Reactive oxygen species
- RNS:
Reactive nitrogen species.
Conflict of Interests
The authors declare that they have no conflict of interests.
References
- 1.Heinrich U., Tronnier H., Stahl W., Béjot M., Maurette J.-M. Antioxidant supplements improve parameters related to skin structure in humans. Skin Pharmacology and Physiology. 2006;19(4):224–231. doi: 10.1159/000093118. [DOI] [PubMed] [Google Scholar]
- 2.Maggini S., Wintergerst E. S., Beveridge S., Hornig D. H. Selected vitamins and trace elements support immune function by strengthening epithelial barriers and cellular and humoral immune responses. The British Journal of Nutrition. 2007;98(supplement 1):S29–S35. doi: 10.1017/s0007114507832971. [DOI] [PubMed] [Google Scholar]
- 3.Korkina L. G., Mikhal'chik E. V., Suprun M. V., Pastore S., Dal Toso R. Molecular mechanisms underlying wound healing and anti-inflammatory properties of naturally occurring bio-technologically produced phenylpropanoid glycosides. Cellular and Molecular Biology. 2007;53(5):78–83. doi: 10.1170/t822. [DOI] [PubMed] [Google Scholar]
- 4.Stahl W., Sies H. Photoprotection by dietary carotenoids: concept, mechanisms, evidence and future development. Molecular Nutrition and Food Research. 2012;56(2):287–295. doi: 10.1002/mnfr.201100232. [DOI] [PubMed] [Google Scholar]
- 5.Nichols J. A., Katiyar S. K. Skin photoprotection by natural polyphenols: anti-inflammatory, antioxidant and DNA repair mechanisms. Archives of Dermatological Research. 2010;302(2):71–83. doi: 10.1007/s00403-009-1001-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Korkina L. G., Pastore S., De Luca C., Kostyuk V. A. Metabolism of plant polyphenols in the skin: beneficial versus deleterious effects. Current Drug Metabolism. 2008;9(8):710–729. doi: 10.2174/138920008786049267. [DOI] [PubMed] [Google Scholar]
- 7.Richelle M., Sabatier M., Steiling H., Williamson G. Skin bioavailability of dietary vitamin E, carotenoids, polyphenols, vitamin C, zinc and selenium. The British Journal of Nutrition. 2006;96(2):227–238. doi: 10.1079/bjn20061817. [DOI] [PubMed] [Google Scholar]
- 8.Exposito J.-Y., Valcourt U., Cluzel C., Lethias C. The fibrillar collagen family. International Journal of Molecular Sciences. 2010;11(2):407–426. doi: 10.3390/ijms11020407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang J., Pei X.-R., Wang N., Zhang Z.-F., Wang J.-B., Li Y. Marine collagen peptides prepared from chum salmon (Oncorhynchus keta) skin extend the life span and inhibit spontaneous tumor incidence in sprague-dawley rats. Journal of Medicinal Food. 2010;13(4):757–770. doi: 10.1089/jmf.2009.1279. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Z., Wang J., Ding Y., Dai X., Li Y. Oral administration of marine collagen peptides from Chum Salmon skin enhances cutaneous wound healing and angiogenesis in rats. Journal of the Science of Food and Agriculture. 2011;91(12):2173–2179. doi: 10.1002/jsfa.4435. [DOI] [PubMed] [Google Scholar]
- 11.Senevirathne M., Kim S.-K. Development of bioactive peptides from fish proteins and their health promoting ability. Advances in Food and Nutrition Research. 2012;65:235–248. doi: 10.1016/b978-0-12-416003-3.00015-9. [DOI] [PubMed] [Google Scholar]
- 12.Zhu C.-F., Li G.-Z., Peng H.-B., Zhang F., Chen Y., Li Y. Therapeutic effects of marine collagen peptides on Chinese patients with type 2 diabetes mellitus and primary hypertension. The American Journal of the Medical Sciences. 2010;340(5):360–366. doi: 10.1097/maj.0b013e3181edfcf2. [DOI] [PubMed] [Google Scholar]
- 13.Zhu C.-F., Li G.-Z., Peng H.-B., Zhang F., Chen Y., Li Y. Treatment with marine collagen peptides modulates glucose and lipid metabolism in chinese patients with type 2 diabetes mellitus. Applied Physiology, Nutrition and Metabolism. 2010;35(6):797–804. doi: 10.1139/H10-075. [DOI] [PubMed] [Google Scholar]
- 14.Chevrier G., Mitchell P. L., Rioux L., et al. Low-molecular-weight peptides from salmon protein prevent obesity-linked glucose intolerance, inflammation, and dyslipidemia in LDLR−/−/ApoB100/100 mice. The Journal of Nutrition. 2015;145(7):1415–1422. doi: 10.3945/jn.114.208215. [DOI] [PubMed] [Google Scholar]
- 15.Lin B., Zhang F., Yu Y., et al. Marine collagen peptides protect against early alcoholic liver injury in rats. British Journal of Nutrition. 2012;107(8):1160–1166. doi: 10.1017/s0007114511004211. [DOI] [PubMed] [Google Scholar]
- 16.Kim S.-K., Ngo D.-H., Vo T.-S. Marine fish-derived bioactive peptides as potential antihypertensive agents. Advances in Food and Nutrition Research. 2012;65:249–260. doi: 10.1016/b978-0-12-416003-3.00016-0. [DOI] [PubMed] [Google Scholar]
- 17.Wang J., Xu M., Liang R., Zhao M., Zhang Z., Li Y. Oral administration of marine collagen peptides prepared from chum salmon (Oncorhynchus keta) improves wound healing following cesarean section in rats. Food & Nutrition Research. 2015;59 doi: 10.3402/fnr.v59.26411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gangwar M., Gautam M. K., Ghildiyal S., Nath G., Goel R. K. Mallotus philippinensis Muell. Arg fruit glandular hairs extract promotes wound healing on different wound model in rats. BMC Complementary and Alternative Medicine. 2015;15, article 123 doi: 10.1186/s12906-015-0647-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bello A. E., Oesser S. Collagen hydrolysate for the treatment of osteoarthritis and other joint disorders: a review of the literature. Current Medical Research and Opinion. 2006;22(11):2221–2232. doi: 10.1185/030079906x148373. [DOI] [PubMed] [Google Scholar]
- 20.Yamada S., Nagaoka H., Terajima M., Tsuda N., Hayashi Y., Yamauchi M. Effects of fish collagen peptides on collagen post-translational modifications and mineralization in an osteoblastic cell culture system. Dental Materials Journal. 2013;32(1):88–95. doi: 10.4012/dmj.2012-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Girgih A. T., Udenigwe C. C., Hasan F. M., Gill T. A., Aluko R. E. Antioxidant properties of Salmon (Salmo salar) protein hydrolysate and peptide fractions isolated by reverse-phase HPLC. Food Research International. 2013;52(1):315–322. doi: 10.1016/j.foodres.2013.03.034. [DOI] [Google Scholar]
- 22.Chalamaiah M., Dinesh Kumar B., Hemalatha R., Jyothirmayi T. Fish protein hydrolysates: proximate composition, amino acid composition, antioxidant activities and applications—a review. Food Chemistry. 2012;135(4):3020–3038. doi: 10.1016/j.foodchem.2012.06.100. [DOI] [PubMed] [Google Scholar]
- 23.Ren S.-W., Li J., Wang W., Guan H.-S. Protective effects of kappa-ca3000+CP against ultraviolet-induced damage in HaCaT and MEF cells. Journal of Photochemistry and Photobiology B: Biology. 2010;101(1):22–30. doi: 10.1016/j.jphotobiol.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Fan J., Zhuang Y., Li B. Effects of collagen and collagen hydrolysate from jellyfish umbrella on histological and immunity changes of mice photoaging. Nutrients. 2013;5(1):223–233. doi: 10.3390/nu5010223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marotta F., Kumari A., Yadav H., et al. Biomarine extracts significantly protect from ultraviolet A-induced skin photoaging: an ex vivo study. Rejuvenation Research. 2012;15(2):157–160. doi: 10.1089/rej.2011.1267. [DOI] [PubMed] [Google Scholar]
- 26.Proksch E., Schunck M., Zague V., Segger D., Degwert J., Oesser S. Oral intake of specific bioactive collagen peptides reduces skin wrinkles and increases dermal matrix synthesis. Skin Pharmacology and Physiology. 2014;27(3):113–119. doi: 10.1159/000355523. [DOI] [PubMed] [Google Scholar]
- 27.Proksch E., Segger D., Degwert J., Schunck M., Zague V., Oesser S. Oral supplementation of specific collagen peptides has beneficial effects on human skin physiology: a double-blind, placebo-controlled study. Skin Pharmacology and Physiology. 2013;27(1):47–55. doi: 10.1159/000351376. [DOI] [PubMed] [Google Scholar]
- 28.Zhu Z., Yang G., Wang Y., et al. Suppression of thioredoxin system contributes to silica-induced oxidative stress and pulmonary fibrogenesis in rats. Toxicology Letters. 2013;222(3):289–294. doi: 10.1016/j.toxlet.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Zhou C.-F., Yu J.-F., Zhang J.-X., et al. N-acetylcysteine attenuates subcutaneous administration of bleomycin-induced skin fibrosis and oxidative stress in a mouse model of scleroderma. Clinical and Experimental Dermatology. 2013;38(4):403–409. doi: 10.1111/ced.12033. [DOI] [PubMed] [Google Scholar]
- 30.Cooper S. K., Pandhare J., Donald S. P., Phang J. M. A novel function for hydroxyproline oxidase in apoptosis through generation of reactive oxygen species. Journal of Biological Chemistry. 2008;283(16):10485–10492. doi: 10.1074/jbc.m702181200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Altenhöfer S., Radermacher K. A., Kleikers P. W., Wingler K., Schmidt H. H. Evolution of NADPH oxidase inhibitors: selectivity and mechanisms for target engagement. Antioxidants & Redox Signaling. 2015;23(5):406–427. doi: 10.1089/ars.2013.5814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ott C., Jacobs K., Haucke E., Navarrete Santos A., Grune T., Simm A. Role of advanced glycation end products in cellular signaling. Redox Biology. 2014;2(1):411–429. doi: 10.1016/j.redox.2013.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pei X., Yang R., Zhang Z., et al. Marine collagen peptide isolated from chum salmon (Oncorhynchus keta) skin facilitates learning and memory in aged C57BL/6J mice. Food Chemistry. 2010;118(2):333–340. doi: 10.1016/j.foodchem.2009.04.120. [DOI] [Google Scholar]
- 34.Zague V., De Freitas V., Rosa M. D. C., De Castro G. Á., Jaeger R. G., MacHado-Santelli G. M. Collagen hydrolysate intake increases skin collagen expression and suppresses matrix metalloproteinase 2 activity. Journal of Medicinal Food. 2011;14(6):618–624. doi: 10.1089/jmf.2010.0085. [DOI] [PubMed] [Google Scholar]
- 35.Giovannoni G., Land J. M., Keir G., Thompson E. J., Heales S. J. R. Adaptation of the nitrate reductase and Griess reaction methods for the measurement of serum nitrate plus nitrite levels. Annals of Clinical Biochemistry. 1997;34(2):193–198. doi: 10.1177/000456329703400212. [DOI] [PubMed] [Google Scholar]
- 36.Bradford M. M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Analytical Biochemistry. 1976;72(1-2):248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 37.Reed D. J., Babson J. R., Beatty P. W., Brodie A. E., Ellis W. W., Potter D. W. High-performance liquid chromatography analysis of nanomole levels of glutathione, glutathione disulfide, and related thiols and disulfides. Analytical Biochemistry. 1980;106(1):55–62. doi: 10.1016/0003-2697(80)90118-9. [DOI] [PubMed] [Google Scholar]
- 38.De Luca C., Deeva I., Mariani S., Maiani G., Stancato A., Korkina L. Monitoring antioxidant defenses and free radical production in space-flight, aviation and railway engine operators, for the prevention and treatment of oxidative stress, immunological impairment, and pre-mature cell aging. Toxicology and Industrial Health. 2009;25(4-5):259–267. doi: 10.1177/0748233709103032. [DOI] [PubMed] [Google Scholar]
- 39.Lang J. K., Gohil K., Packer L. Simultaneous determination of tocopherols, ubiquinols, and ubiquinones in blood, plasma, tissue homogenates, and subcellular fractions. Analytical Biochemistry. 1986;157(1):106–116. doi: 10.1016/0003-2697(86)90203-4. [DOI] [PubMed] [Google Scholar]
- 40.De Luca C., Filosa A., Grandinetti M., Maggio F., Lamba M., Passi S. Blood antioxidant status and urinary levels of catecholamine metabolites in β-thalassemia. Free Radical Research. 1999;30(6):453–462. doi: 10.1080/10715769900300491. [DOI] [PubMed] [Google Scholar]
- 41.Sun Y., Oberley L. W., Li Y. A simple method for clinical assay of superoxide dismutase. Clinical Chemistry. 1988;34(3):497–500. [PubMed] [Google Scholar]
- 42.Sandström J., Nilsson P., Karlsson K., Marklund S. L. 10-Fold increase in human plasma extracellular superoxide dismutase content caused by a mutation in heparin-binding domain. The Journal of Biological Chemistry. 1994;269(29):19163–19166. [PubMed] [Google Scholar]
- 43.Habig W. H., Pabst M. J., Jakoby W. B. Glutathione S transferases. The first enzymatic step in mercapturic acid formation. The Journal of Biological Chemistry. 1974;249(22):7130–7139. [PubMed] [Google Scholar]
- 44.Paglia D. E., Valentine W. N. Studies of quantitative and qualitative characterization of erythrocyte glutathione peroxidase. The Journal of Laboratory and Clinical Medicine. 1967;70(1):158–169. [PubMed] [Google Scholar]
- 45.Yagi K. A. A simple fluorometric assay for lipoperoxide in blood plasma. Biochemical Medicine. 1976;15(2):212–216. doi: 10.1016/0006-2944(76)90049-1. [DOI] [PubMed] [Google Scholar]
- 46.Wölfle U., Esser P. R., Simon-Haarhaus B., Martin S. F., Lademann J., Schempp C. M. UVB-induced DNA damage, generation of reactive oxygen species, and inflammation are effectively attenuated by the flavonoid luteolin in vitro and in vivo. Free Radical Biology and Medicine. 2011;50(9):1081–1093. doi: 10.1016/j.freeradbiomed.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 47.Perez G R. M., Vargas S R., Ortiz H Y. D. Wound healing properties of Hylocereus undatus on diabetic rats. Phytotherapy Research. 2005;19(8):665–668. doi: 10.1002/ptr.1724. [DOI] [PubMed] [Google Scholar]
- 48.Barbul A. Proline precursors to sustain mammalian collagen synthesis. The Journal of Nutrition. 2008;138(10):2021S–2024S. doi: 10.1093/jn/138.10.2021S. [DOI] [PubMed] [Google Scholar]
- 49.Saito M., Kiyose C., Higuchi T., Uchida N., Suzuki H. Effect of collagen hydrolysates from salmon and trout skins on the lipid profile in rats. Journal of Agricultural and Food Chemistry. 2009;57(21):10477–10482. doi: 10.1021/jf902355m. [DOI] [PubMed] [Google Scholar]
- 50.Ohara H., Matsumoto H., Ito K., Iwai K., Sato K. Comparison of quantity and structures of hydroxyproline-containing peptides in human blood after oral ingestion of gelatin hydrolysates from different sources. Journal of Agricultural and Food Chemistry. 2007;55(4):1532–1535. doi: 10.1021/jf062834s. [DOI] [PubMed] [Google Scholar]
- 51.Murthy S., Gautam M. K., Goel S., Purohit V., Sharma H., Goel R. K. Evaluation of in vivo wound healing activity of Bacopa monniera on different wound model in rats. BioMed Research International. 2013;2013:9. doi: 10.1155/2013/972028.972028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jebahi S., Saoudi M., Farhat L., et al. Effect of novel curcumin-encapsulated chitosan-bioglass drug on bone and skin repair after gamma radiation: experimental study on a Wistar rat model. Cell Biochemistry and Function. 2015;33(3):150–159. doi: 10.1002/cbf.3098. [DOI] [PubMed] [Google Scholar]
- 53.Yaman I., Derici H., Kara C., et al. Effects of resveratrol on incisional wound healing in rats. Surgery Today. 2013;43(12):1433–1438. doi: 10.1007/s00595-012-0455-7. [DOI] [PubMed] [Google Scholar]
- 54.Park J. E., Abrams M. J., Efron P. A., Barbul A. Excessive nitric oxide impairs wound collagen accumulation. The Journal of Surgical Research. 2013;183(1):487–492. doi: 10.1016/j.jss.2012.11.056. [DOI] [PubMed] [Google Scholar]
- 55.Sen C. K., Khanna S., Babior B. M., Hunt T. K., Christopher Ellison E., Roy S. Oxidant-induced vascular endothelial growth factor expression in human keratinocytes and cutaneous wound healing. The Journal of Biological Chemistry. 2002;277(36):33284–33290. doi: 10.1074/jbc.m203391200. [DOI] [PubMed] [Google Scholar]
- 56.Khanna S., Roy S., Bagchi D., Bagchi M., Sen C. K. Upregulation of oxidant-induced VEGF expression in cultured keratinocytes by a grape seed proanthocyanidin extract. Free Radical Biology and Medicine. 2001;31(1):38–42. doi: 10.1016/s0891-5849(01)00544-5. [DOI] [PubMed] [Google Scholar]
- 57.Cho M., Hunt T. K., Hussain M. Z. Hydrogen peroxide stimulates macrophage vascular endothelial growth factor release. The American Journal of Physiology—Heart and Circulatory Physiology. 2001;280(5):H2357–H2363. doi: 10.1152/ajpheart.2001.280.5.H2357. [DOI] [PubMed] [Google Scholar]
- 58.Abas R., Othman F., Thent Z. C. Protective effect of Momordica charantia fruit extract on hyperglycaemia-induced cardiac fibrosis. Oxidative Medicine and Cellular Longevity. 2014;2014:8. doi: 10.1155/2014/429060.429060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yang Y., Gao X., Wang X., Su L., Xing H. Total Flavonoids of Fructus Chorspondiatis inhibits collagen synthesis of cultured rat cardiac fibroblasts induced by angiotensin II: correlated with NO/cGMP signaling pathway. European Journal of Pharmaceutical Sciences. 2012;47(1):75–83. doi: 10.1016/j.ejps.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 60.Yu F.-X., Teng Y.-Y., Zhu Q.-D., Zhang Q.-Y., Tang Y.-H. Inhibitory effects of capsaicin on hepatic stellate cells and liver fibrosis. Biochemistry and Cell Biology. 2014;92(5):406–412. doi: 10.1139/bcb-2014-0036. [DOI] [PubMed] [Google Scholar]
- 61.Jobara K., Kaido T., Hori T., et al. Whey-hydrolyzed peptide-enriched immunomodulating diet prevents progression of liver cirrhosis in rats. Nutrition. 2014;30(10):1195–1207. doi: 10.1016/j.nut.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 62.Zhu B., Ma A. Q., Yang L., Dang X. Atorvastatin attenuates bleomycin-induced pulmonary fibrosis via suppressing iNOS expression and the CTGF (CCN2)/ERK signaling pathway. International Journal of Molecular Sciences. 2013;14(12):24476–24491. doi: 10.3390/ijms141224476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tanaka M., Koyama Y.-I., Nomura Y. Effects of collagen peptide ingestion on UV-B-induced skin damage. Bioscience, Biotechnology and Biochemistry. 2009;73(4):930–932. doi: 10.1271/bbb.80649. [DOI] [PubMed] [Google Scholar]
- 64.Zhuang Y., Hou H., Zhao X., Zhang Z., Li B. Effects of collagen and collagen hydrolysate from jellyfish (Rhopilema esculentum) on mice skin photoaging induced by UV irradiation. Journal of Food Science. 2009;74(6):H183–H188. doi: 10.1111/j.1750-3841.2009.01236.x. [DOI] [PubMed] [Google Scholar]
- 65.Kwon M. J., Lee K. Y., Lee H. W., Kim J., Kim T. SOD3 variant R213G altered SOD3 function, leading to ROS mediated inflammation and damage in multiple organs of premature aging mice. Antioxidants & Redox Signaling. 2015;23(12):985–999. doi: 10.1089/ars.2014.6035. [DOI] [PubMed] [Google Scholar]
- 66.Kwon M.-J., Han J., Kim B. H., Lee Y. S., Kim T.-Y. Superoxide dismutase 3 suppresses hyaluronic acid fragments mediated skin inflammation by inhibition of toll-like receptor 4 signaling pathway: superoxide dismutase 3 inhibits reactive oxygen species-induced trafficking of toll-like receptor 4 to lipid rafts. Antioxidants & Redox Signaling. 2012;16(4):297–313. doi: 10.1089/ars.2011.4066. [DOI] [PubMed] [Google Scholar]
- 67.Miller E. R., III, Pastor-Barriuso R., Dalal D., Riemersma R. A., Appel L. J., Guallar E. Meta-analysis: high-dosage vitamin E supplementation may increase all-cause mortality. Annals of Internal Medicine. 2005;142(1):37–46. doi: 10.7326/0003-4819-142-1-200501040-00110. [DOI] [PubMed] [Google Scholar]
- 68.Liang J., Li Q., Lin B., et al. Comparative studies of oral administration of marine collagen peptides from Chum Salmon (Oncorhynchus keta) pre- and post-acute ethanol intoxication in female Spraque-Dawley rats. Food & Function. 2014;5(9):2078–2085. doi: 10.1039/c4fo00161c. [DOI] [PubMed] [Google Scholar]
- 69.Ayala A., Muñoz M. F., Argüelles S. Lipid peroxidation: production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxidative Medicine and Cellular Longevity. 2014;2014:31. doi: 10.1155/2014/360438.360438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kostyuk V., Potapovich A., Stancato A., et al. Photo-oxidation products of skin surface squalene mediate metabolic and inflammatory responses to solar UV in human keratinocytes. PLoS ONE. 2012;7(8) doi: 10.1371/journal.pone.0044472.e44472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bindoli A., Rigobello M. P. Principles in redox signaling: from chemistry to functional significance. Antioxidants & Redox Signaling. 2013;18(13):1557–1593. doi: 10.1089/ars.2012.4655. [DOI] [PubMed] [Google Scholar]
- 72.Passi S., De Pità O., Puddu P., Littarru G. P. Lipophilic antioxidants in human sebum and aging. Free Radical Research. 2002;36(4):471–477. doi: 10.1080/10715760290021342. [DOI] [PubMed] [Google Scholar]
- 73.Kim E. J., Jin X.-J., Kim Y. K., et al. UV decreases the synthesis of free fatty acids and triglycerides in the epidermis of human skin in vivo, contributing to development of skin photoaging. Journal of Dermatological Science. 2010;57(1):19–26. doi: 10.1016/j.jdermsci.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 74.Thiele J. J., Weber S. U., Packer L. Sebaceous gland secretion is a major physiologic route of vitamin E delivery to skin. Journal of Investigative Dermatology. 1999;113(6):1006–1010. doi: 10.1046/j.1523-1747.1999.00794.x. [DOI] [PubMed] [Google Scholar]
- 75.Korkina L., Pastore S. The role of redox regulation in the normal physiology and inflammatory diseases of skin. Frontiers in Bioscience—Elite Edition. 2009;1:123–141. doi: 10.2741/E13. [DOI] [PubMed] [Google Scholar]
- 76.De Luca C., Valacchi G. Surface lipids as multifunctional mediators of skin responses to environmental stimuli. Mediators of Inflammation. 2010;2010:11. doi: 10.1155/2010/321494.321494 [DOI] [PMC free article] [PubMed] [Google Scholar]