Abstract
Objective
To report findings from a proof-of-concept trial designed to examine the feasibility and estimate the efficacy of the “Be Well, Work Well” workplace intervention.
Methods
The intervention included consultation for nurse managers to implement changes on patient care units and educational programming for patient care staff to facilitate improvements in safety and health behaviors. We used a mixed-methods approach to evaluate feasibility and efficacy.
Results
Using findings from process tracking and qualitative research, we observed challenges to implementing the intervention due to the physical demands, time constraints and psychological strains of patient care. Using survey data, we found no significant intervention effects.
Conclusions
Beyond educating individual workers, system-wide initiatives that respond to conditions of work may be needed to transform the workplace culture and broader milieu in support of worker health and safety.
Introduction
Every year, nursing employees in the United States experience more than 35,000 back and other injuries that are severe enough to result in missing work.1 In both acute- and long-term care settings, overexertion resulting from the need to lift and move patients accounts for the majority of these injuries.2 The risks are compounded by staff shortages and working long hours, often during night shifts, as well as psychosocial factors such as limited control over decisions on the job.3-6 As a result, a growing number move out of this field of work that has chronic labor shortages.7
Improving and protecting the health and well-being of healthcare workers requires addressing key risks in the work environment as well as promoting safe and healthy behaviors. The risk of musculoskeletal disorders (MSDs) increases in the presence of risk-related behaviors such as insufficient sleep, physical inactivity, and dietary patterns associated with being overweight or obese.8-17 These behaviors are also shaped by the conditions of work. For example, poor sleep among nurses has been associated with shift work, the emotional demands of care-giving, and the challenges to unwinding after 12-hour shifts.18,19 Traditional approaches to mitigating these risks have generally used uncoupled efforts to either reduce workplace-related MSD risk or improve individual’s health behaviors; workplace programs to promote healthy behaviors have often ignored the role of the work context.20,21 A growing literature, however, has highlighted the benefits that may be derived from integrated policies, programs and practices addressing both workplace and personal health, reflected, for example, by the Total Worker HealthTM (TWH) Program of the National Institute for Occupational Safety and Health.22 Nonetheless, little research has systematically examined the potential for integrated interventions for healthcare providers, and there is insufficient evidence to determine the most effective ways to address the combined effects of these safety and health risks for this group of workers.
This manuscript describes the “Be Well, Work Well” (BWWW) intervention, designed in response to these concerns. This intervention aimed to reduce MSD risk and improve health-related behaviors, including physical activity, sleep, and dietary patterns, by promoting supportive policies and practices and fostering healthy and safe behaviors through programs for workers in direct patient care units within an acute care hospital. The purpose of this paper is to report findings from a proof-of-concept (PoC) trial designed to examine the feasibility and estimate the efficacy of the BWWW intervention. A PoC trial is conducted to demonstrate feasibility or efficacy, typically on a small scale as a milestone toward full development of a “concept.” 23-26 This mixed methods paper reports findings from process evaluation, qualitative research, and surveys of workers examining changes in MSD symptoms, physical activity, diet, and sleep, and a set of secondary outcomes potentially influenced by the intervention (e.g., improved ergonomic practices).
Methods
The BWWW study was conducted by the Harvard T.H. Chan School of Public Health, Center for Work, Health and Wellbeing, in collaboration with Partners HealthCare. Eight inpatient care units from one large academic hospital in the Boston area were selected and randomly assigned to intervention or control conditions. The conceptual model used to guide intervention development was adapted from the Center’s overarching conceptual framework.21 This study was approved by the Harvard Chan School’s Institutional Review Board.
Study Sample
The eight patient care units for this study were randomly selected from 80 eligible units in the hospital. Patient care units were defined as those providing clinical care to patients formally admitted to the hospital assigned to a medical, surgical, or intensive care unit (ICU). Ineligible units included operating room, emergency department, post-anesthesia care, and units undergoing significant changes. These eight units were randomly assigned to intervention or control after baseline data collection. The intervention group consisted of one surgical unit, one non-surgical unit, and two ICUs. The control group consisted of three non-surgical units and one ICU.
This evaluation focused on patient care workers employed on the study units, who were eligible to participate in the survey and qualitative data collection. Patient care workers included registered nurses, licensed practical nurses, and Patient Care Assistants (PCAs). Workers on an extended absence greater than 12 weeks, per diem workers, and contract nurses were ineligible.
Be Well Work Well (BWWW) Intervention
We developed the intervention to be responsive to the work experiences and priorities of direct patient care workers, based on extensive formative research, including a review of the literature, a cross-sectional survey of patient care workers,3-6,8,17,27-36 and focus groups with nurse managers and patient care workers.37 Our prior research highlighted common pathways through which conditions of work may be associated with MSDs, physical activity, sleep, and obesity risk.4,5,29,33,34,38 In addition, we sought to link the intervention to other hospital priorities; for example, the hospital’s high priority initiative around safe patient movement provided a leverage point for promoting the use of mechanical transfer devices such as ceiling lifts, key to MSD prevention.
We used the formative research to design the intervention targeting the unit and individual levels (Figure 1). For example, our survey findings as well as qualitative research pointed to the importance of patient care needs, lack of control over job demands, the role of co-worker and supervisor support, barriers to using available ceiling lifts and attention to ergonomic factors as important correlates of pain, physical activity and sleep among patient care workers. Accordingly, unit-level targets addressed the physical work environment, such as improved safety and ergonomic practices, as well as the work organization and policies, including improved organizational culture and increasing supervisor support for workers’ health and well-being. Individual-level targets focused on increasing self-efficacy and skills to make behavior changes within the work context, and aimed to increase understanding of the links between the conditions of work and health and safety. In addition, building from our qualitative findings, we employed an overarching theme for patient care workers focused on the importance of “taking care of yourself in order to better care for your patients.” We also developed messages that linked or integrated MSD prevention and promoting health behavior change, which were used throughout the intervention.
Figure 1.
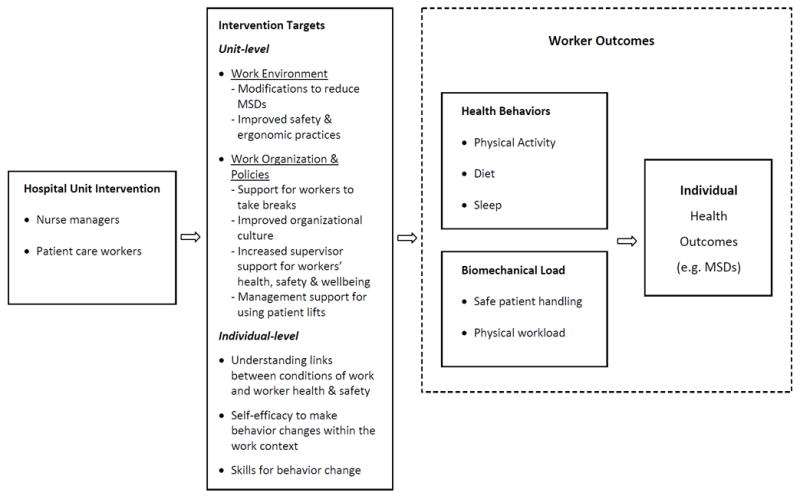
Conceptual Model
At the unit-level, we conducted an ergonomic walkthrough and work organization assessment on each unit and provided feedback to nurse managers about modifiable risks to provide foundations for action plans. The intervention targets included work environment (e.g., modifications to reduce MSD risk), work organization (e.g., support for workers to take breaks), and support for individual health and safety behaviors (e.g., management support for using patient lifts). To assist nurse managers in providing leadership and support for their workers, we engaged a management consultant39 well-versed in the hospital’s work culture to provide individual consultation to nurse managers. Up to four consultations were offered, including conducting an organizational assessment; discussion of a report that integrated the results of the ergonomic walk-through and work organization assessment; development of an Action Plan based on these assessments; and planning for next steps.
We coordinated these consultations with interventions for individual workers, taking into account workers’ schedules and the competing patient care demands. In order to ensure that the intervention activities did not interfere with patient care responsibilities, leadership on the units requested that the intervention be limited to two monthly visits, once during the day shift and once during the night shift. Eight major events were planned: (1) a kick-off BWWW health event; (2) safe patient handling training; (3) a healthy eating question and answer session (“EatWell”); (4) a presentation and conversation with a sleep expert; (5) a pedometer challenge that promoted competition among the units to be physically active; (6) ergonomic talks and individual assistance related to safe patient handling, equipment and workstation setup, and prevention of slips, trips and falls; (7) goal setting and promotion of health coaching (“Plan Well”); and (8) identifying ways to support co-workers’ health and safety goals (“Together We Are Well”).
The intervention incorporated complementary opportunities for participation outside work hours. Units were invited to participate in the hospital’s nutrition and fitness program, called “Be Fit,” which included ten weekly 30-minute group educational sessions offered on the unit during the day shift, as well as access to a fitness center, personal trainer and nutritionist. In addition, BWWW offered personalized telephone health coaching sessions on diet, physical activity, sleep hygiene and ergonomics. The health coaching, based on motivational interviewing methods,40 focused on goal-setting and skill-building for health behavior changes. Intervention staff also developed a social media page for each unit to support the intervention messages, and provided materials with integrated messages intended to be motivational.
Process evaluation
Study staff completed process tracking forms to document intervention delivery including the types and content of activities, number of times offered, number of participants, date and length of the activity, estimated length of participant attendance, and adaptations made to the activity. Tracking forms for the unit-level intervention included the date and the length of the activity, the content (e.g., ergonomics assessment, action plan meetings), the job categories of those attending the meetings, and the number in each job category.
We assessed program coverage as the proportion of workers who attended at least one activity, measured as the highest participation rate for any single intervention activity on a unit. For each intervention activity, we computed the participation rate based on the total number of workers who attended any event for a given activity on each intervention unit, divided by the number of patient care workers employed on the unit. We did not track individual participation; therefore, it was not possible to determine whether the number of attendees per session represented repeat or new attendees. We also estimated the amount of time on average that participants spent at each intervention activity.
Qualitative methods
Qualitative data were collected by a trained BWWW staff member and included:
Pre-Intervention focus groups
Prior to the start of the intervention, we conducted six one-hour focus groups, including at this hospital and another affiliated hospital, with workers from units not assigned to the PoC units, including focus groups with each of three employee groups: staff nurses (n=7), PCAs (n=6), and Nurse managers (n=9). The objectives of these focus groups were to identify workers’ perceptions of unit practices, including scheduling, breaks, and safe patient handling; explore workers’ priorities for the targeted health behaviors; and assess workers’ priorities and suggestions for the intervention.
Post-Intervention focus groups
Two focus groups, one each for nursing and PCA staff, were completed on each of the three of the four intervention units that agreed to participate, with the exception of one unit that does not utilize PCAs. In total, 25 nurses and four PCAs participated in the post-intervention focus groups. The objectives were to assess awareness of and general impressions of the BWWW intervention; identify barriers and facilitating factors for program participation and for embedding individual-level activities into existing structures and daily practice on the unit; and explore awareness of unit-level intervention with the nurse managers.
Post-Intervention interviews with nurse managers on the intervention units
Three key informant interviews were conducted with nurse managers from three of the four of the intervention unit; one unit refused. The objectives were to identify barriers to staff participation in the intervention and ways nurse directors were able to support their participation, explore perceptions of the intervention, document any changes made to it, and identify ways that the hospital could support implementation of the intervention. They also discussed ways to embed individual-level activities into daily practice and additional leadership approaches to supporting worker health and safety behaviors.
In addition, after the intervention, study staff debriefed on their experiences implementing the intervention and discussed potential changes to improve its delivery.
Patient-care worker surveys
We conducted two self-administered surveys of patient care workers: at baseline (September 2012 through January 2013), and follow-up (March through June 2014).
Data collection
Invitations to participate in the self-administered surveys were delivered to individuals’ work emails, and a link was provided to take the survey on-line. Two reminders were sent to non-responders at approximately weekly intervals. After two reminders, a paper copy of the survey was sent to workers’ home addresses with a stamped return envelope, followed by up to four additional email reminders.
Sample
At baseline, we surveyed all patient care workers employed at least 20 hours over the last 9 of 13 weeks in any in-patient care unit, and who had worked at least one hour in one of the eight participating units (response rates: Intervention: 84% (n=206/245); Control: 84% (n=198/237)). At follow-up, we surveyed all workers included in the baseline sample plus any new workers employed on these units at the time of survey administration, using the same eligibility criteria as baseline. (response rates: Intervention: 75% (n=228/306); Control: 75% (n=224/298)). (See Figure 2.)
Figure 2.
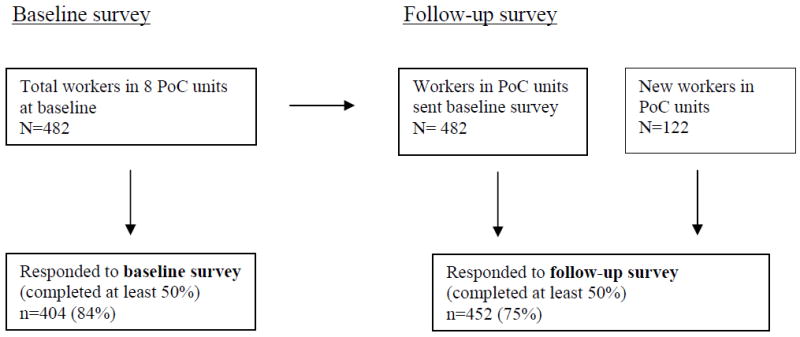
Participant flow, baseline and follow-up surveys.
Measures used from the patient care worker surveys included the following:
Outcomes
Physical Activity was measured using an adapted version of the Centers for Disease Control and Prevention Behavioral Risk Factor and Surveillance System Physical Activity measure,41 and included time spent walking and participating in both vigorous and moderate physical activities for at least 10 minutes at a time both at home and at work during last 7 days. Time spent sitting was presented in minutes and derived from the question: “How much time in total did you usually spend sitting on a week day?”
Sleep deficiency was operationalized using both quantity and quality of sleep, with questions adapted from the Pittsburgh Sleep Quality Index.42 Sleep deficiency was defined as the presence of short sleep duration (<6 hrs/day), insomnia symptoms (i.e., difficulty falling asleep, waking up in the middle of the night or early in the morning), or insufficient sleep (i.e., feeling rested upon waking).43
Diet was measured using the Health in Common Study survey,44,45 which assessed the frequency of consuming fruits/vegetables, red meat, sugary snacks, sugar sweetened beverages, and fast food in the last 7 days. Response categories in the last 7 days were converted to servings per day.
Pain was assessed using multiple constructs. The presence of any pain over the previous 3 months was assessed using a modified question from the Pro-Care Survey (NordicQ).46 Work interference was measured by the question, “In general how much did this pain interfere with your normal work?” and was considered present when the individual responded moderately, quite a bit, or extremely, rather than not at all or a little bit. Musculoskeletal pain severity was also assessed during the past week using an adapted DASH questionnaire47 based on pain location (i.e., in the low back; arm, shoulder, or hand pain; tingling in their arm, shoulder, or hand; pain in their legs or knees; and pain in their feet); responses were on a five point scale from “0 = none” to “4 = extreme” and summed to provide a measure of pain severity during the past week.
Proximal outcomes
We additionally assessed a set of proximal outcomes based on measures used in prior surveys, including ergonomic practices,28 supervisor and co-worker support,17,48,49 safety practices,28 and meal break frequency.36
Independent Variables
Occupation included staff nurse, patient care associate, clinical nurse specialist, and other (operations coordinator and other). Work shift was assessed using the following categories: “regular days,” “regular evenings,” “’regular nights,” and “other.” Hours worked was assessed by asking how many hours worked in a “typical week.” Socio-demographic variables included gender and age.
Analyses
To compare the intervention and control groups with regard to mean changes in survey responses from baseline to follow-up, we computed mixed effect linear models for each measure with fixed effects for time (pre- or post), intervention group and the interaction of time and intervention group. Random effects were included for participants who answered both surveys and for the clustering of workers in units. The p-value for the interaction of time and intervention group provided the test of the null hypothesis of no difference between groups. For continuous measures, such as pain severity, we used general linear mixed models assuming a Gaussian distribution. This assumption was evaluated and the measure transformed if necessary.
For binary measures, such as any pain, we used a generalized mixed model assuming a binomial distribution with a logit link function.
Results
Process Evaluation Results
The BWWW intervention was delivered on the four inpatient care units randomly assigned to the intervention condition between January 2013 and January 2014.
At the unit level, the ergonomic walk-through and work organization assessment were conducted on all four intervention units. The BWWW team distributed reports of results to nurse managers on all four units, and discussed them with managers on three of the units. Following the reports, one nurse manager declined further participation in the unit-level intervention due to turnover in nursing leadership. Two managers in two units participated in two consultations, and one manager participated in three consultations lasting approximately one hour each. Across these three units, priorities addressed in the action plans included increased work-breaks on the unit, increased worker awareness of existing resources, and safety and ergonomic improvements. At the completion of the intervention, adoption of these action plans was still in process and few recommendations from the action plans had been implemented.
For the individual-level intervention, there was considerable variability in the number of intervention events offered on each unit (range: 11-29; see Table 1). Of note, the units with fewer events were both ICU’s, where intervention delivery faced particular challenges in light of heavy patient care demands.
Table 1.
Summary of Intervention Activities by Unit
| Intervention activity | Unit 1: Medical Oncology | Unit 2: Thoracic Surgery | Unit 3: Medical ICU | Unit 4: Neonatal ICU | Total |
|---|---|---|---|---|---|
| n=54 | n=48 | n=66 | n=53 | n=221 | |
| Kickoff | |||||
| N events | 2 | 2 | 2 | 2 | 8 |
| Total n participants (participation rate, %) | 35(64.8) | 37(77.1) | 56(84.8) | 33(62.3) | 161(72.8) |
| Mean minutes for participants | 7 | 7 | 5 | 5 | 6 |
| Safe patient handling training | |||||
| N events | 3 | 4 | 1 | 1 | 9 |
| Total N participants (participation rate) | 11(20.4) | 28(58.3) | 11(16.7) | 6(11.3) | 56(25.3) |
| Mean minutes for participants | 60 | 49 | 15 | 30 | 47 |
| Eat Well | |||||
| N events | 3 | 2 | 2 | 2 | 9 |
| Total N participants (participation rate) | 49(90.7) | 36(75.0) | 26(39.4) | 28(52.8) | 139(62.9) |
| Mean minutes for participants | 4 | 4 | 4 | 6 | 4 |
| Exercise Challenge | |||||
| N events | 2 | 2 | 0 | 2 | 6 |
| Total N participants (participation rate) | 37(68.5) | 19(39.6) | 15(28.3) | 71(45.8)* | |
| Mean minutes for participants | 8 | 8 | -- | 5 | 7 |
| Conversation w/Ergonomist | |||||
| N events | 2 | 2 | 2 | 0 | 6 |
| Total N participants (participation rate) | 18(33.3) | 10(20.8) | 26(39.4) | 54(32.1)* | |
| Mean minutes for participants | 6 | 7 | 8 | -- | 7 |
| Conversation w/Sleep Expert | |||||
| N events | 2 | 2 | 2 | 2 | 8 |
| Total N participants (participation rate) | 20(37.0) | 19(39.6) | 22(33.3) | 23(43.4) | 84(38.0) |
| Mean minutes for participants | 35 | 30 | 30 | 45 | 35 |
| Plan Well | |||||
| N events | 2 | 3 | 2 | 2 | 9 |
| Total N participants (participation rate) | 19(35.2) | 19(39.6) | 18(27.3) | 16(30.2) | 72(32.6) |
| Mean minutes for participants | 10 | 12 | 9 | 10 | 10 |
| Together Well | |||||
| N events | 2 | 2 | 0 | 2 | 6 |
| Total N participants (participation rate) | 20(37.0) | 15(31.3) | 15(28.3) | 50(32.3)* | |
| Mean minutes for participants | 9 | 8 | -- | 9 | 9 |
| ALL ACTIVITIES | |||||
| N events | 18 | 19 | 11 | 13 | 61 |
| Estimated number of unique workers who attended at least one event (i.e., max N and % from above) | 49(90.7) | 37(77.1) | 56(84.8) | 33(62.3) | 161(72.8) |
of 3 sites
Table 1 also presents the estimated number of unique workers who attended at least one event, using the maximum participation rate for any intervention activity, which across all events was 73% (range 62-91%). The kickoff activity garnered the overall highest rate of participation (73% overall); however, the typical length of time participants spend at the kickoff was 6 minutes. Most events were attended by fewer than 50% of workers on the units. The average number of minutes participants spent at an activity was highest for the safe patient handling activity (47 minutes), which constituted a one-on-one training, although the participation rate for this activity (25%) was low relative to other intervention activities. For all other intervention activities, participants consistently spent under 10 minutes at each activity.
Two of the units opted to participate in the “Be Fit” program, including a total of 42 workers. Across the four units, seven patient care workers signed up for the BWWW telephone health coaching calls, each receiving on average two ten-minute phone coaching calls.
Qualitative findings
We combined findings across these data sources to identify three overarching themes:
Conditions of work influencing health and safety practices/ behaviors
The feasibility of the intervention was influenced by the challenges these workers faced on the job, including the need for providing round-the-clock care (including on weekends and holidays), psychological distress associated with patient care, and physical demands often requiring long periods of standing. Focus group participants observed, for example, that work significantly affects their sleep, recognizing that intense 12- hour shifts or night shifts take a toll on how rested they may feel, and that the emotional intensity of healthcare work can impact sleep quality, placing them at greater risk of injuries at work. For example, one nurse observed that when she is tired from multiple shifts, she feels:
“…Tired, and it’s like, “Okay, let’s pull that patient up.” You don’t even think about what you’re doing and you’re, “Okay. Ooof. Oh, my back!”
Many also observed that not getting enough sleep contributed to less healthy eating. Participants also observed that working 12-hour shifts was a significant barrier to being physically active during non-work time, although many thought they were getting enough physical activity on the job already. They also observed that the relationships between their health behaviors and work were reciprocal, noting that not eating well or not getting enough sleep can lead to being tired on the job. Participants also reported that not having enough staff increased job stress, resulting in being more tired and prone to injury. As one PCA stated:
“I find what stresses me out and ruins my sleep and diet and eating habits so much is days when there’s not enough of us, and like, there’s so much running around going on.”
The implications of work conditions on intervention delivery and participation
These job demands presented barriers to workers’ participation in intervention activities; had implications for the time and attention available to follow through on implementing recommended changes in the ergonomic environment; and presented challenges to regular break-taking practices. We observed through these focus groups and our interactions on the units that the dominant culture of patient care providers had them “put their patients first,” sacrificing time for work breaks to care for patients. The pervasive work ethic focusing attention to the needs of patients often meant there was not the flexibility during work time to participate in intervention activities. Focus group participants reported that significant barriers to participating included scheduling, time, and getting away from patient care to take part in program activities. These potential barriers varied depending on patient census level, patient acuity, and staffing levels.
Perceptions of the BWWW program
Focus group results indicated that patient care workers perceived the BWWW intervention as predominantly educational activities for patient care staff, and were not generally aware of the interventions with nurse managers to improve policies and practices at the unit level. Despite efforts of the intervention team to ensure an integrated focus to the intervention, focus group participants described the individual focal points for each outcome, but the messages that integrated MSDs and promoting health behavior change could have been strengthened. In addition, participants suggested that it may be helpful to tighten the focus by covering fewer topics in greater depth and better linking messages across risks.
To help overcome scheduling and timing barriers, focus group participants recommended conducting program activities during “protected” time when staff could leave the patient care unit with coverage for their responsibilities. Some participants suggested program activities occur off the floor in one four-hour training session; include incentives such as continuing education credits; and incorporate web-based components. Nurse managers similarly suggested alternate delivery modalities, including 10-15 minute modules accompanied by food and two-to-four hour off-unit programs that occurred on paid time with staff coverage. Participants reported that programs need buy-in and support from upper management for interventions to be successful, especially in regards to resource allocation and accommodations, including protected time for participating in such activities. For instance, managers could allow for extra staffing to provide coverage for those who leave the floor to take part in the program. One nurse noted, for example:
“Do you guys have… support of … administrators? That, like, are truly … passionate about like Be Well, Work Well, and like want to see these changes on the floor?… Because we see how… passionate they are about how we do … our documenting and… they spare no cost for that. But it’ll take until they see the importance of it, I don’t think anything is really going to happen.”
Nurse managers similarly reported the need for support from upper leadership to ensure program activities are effective. For example, one nurse manager observed that it required someone “higher than me… who can really say, ‘Yeah,’… to make sure it happens.” Priorities for unit level changes need to be supported by and congruent with hospital level priorities. While the approval and support by upper management was obtained prior to this intervention, the continuous involvement by upper management in the hospital may be needed to support nurse managers’ efforts on the patient care units. For example, additional resources and staff for intervention units could give managers and staff flexibility for attending events and implementing changes, support break practices, as well as communicate priorities of upper management in an environment with competing priorities. Notably, this intervention did not include consultation with upper management about these possibilities. Upper management did express its full support of the intervention, as proposed.
Patient care worker survey results
We observed few differences between the intervention and control units at baseline (see Table 2).
Table 2.
Selected characteristics of survey respondents by time of survey and intervention condition: Frequency (and %) or mean (and standard deviation) or median (and IQR)
| Intervention | Control | |||
|---|---|---|---|---|
| Characteristic | Pre-Ix Survey (N=206) No. (%) or Mean (± SD) or Median [IQR] | Post-Ix Survey (N=228) No. (%) or Mean (± SD) or Median [IQR] | Pre-Ix Survey (N=198) No. (%) or Mean (± SD) or Median [IQR] | Post-Ix Survey (N=224) No. (%) or Mean (± SD) or Median [IQR] |
| PAIN OUTCOMES | ||||
| Pain Severity Scale | 2.5 (± 2.54) | 2.7 (± 2.78) | 2.6 (± 2.39) | 2.3 (± 2.17) |
| Any Pain | ||||
| No | 45 (21.8%) | 51 (22.4%) | 37 (18.8%) | 57 (25.4%) |
| Yes | 161 (78.2%) | 177 (77.6%) | 160 (81.2%) | 167 (74.6%) |
| Work Interference | ||||
| No | 153 (75.4%) | 168 (75.7%) | 150 (76.1%) | 184 (84.4%) |
| Yes | 50 (24.6%) | 54 (24.3%) | 47 (23.9%) | 34 (15.6%) |
| DIET OUTCOMES | ||||
| Fruit/Veggie Servings per day | 2.9 (± 1.59) | 2.9 (± 1.46) | 2.8 (± 1.38) | 2.9 (± 1.37) |
| At least 5 daily Fruit/Veggie servings? | ||||
| No | 177 (86.3%) | 201 (88.2%) | 181 (91.9%) | 197 (87.9%) |
| Yes | 28 (13.7%) | 27 (11.8%) | 16 (8.1%) | 27 (12.1%) |
| Sugary Snacks Servings per day | 0.3 (± 0.39) | 0.3 (± 0.34) | 0.3 (± 0.32) | 0.3 (± 0.33) |
| Sugary Drink Servings per day | 0.5 (± 0.61) | 0.5 (± 0.63) | 0.4 (± 0.58) | 0.4 (± 0.57) |
| Fast Food per day | 0.1 (± 0.18) | 0.1 (± 0.15) | 0.0 (± 0.09) | 0.0 (± 0.10) |
| SLEEP OUTCOME | ||||
| Sleep Deficiency | ||||
| No | 68 (33.2%) | 79 (34.6%) | 71 (35.9%) | 91 (40.6%) |
| Yes | 137 (66.8%) | 149 (65.4%) | 127 (64.1%) | 133 (59.4%) |
| PHYSICAL ACTIVITY OUTCOMES | ||||
| Minutes of Combined Moderate/Vigorous Activity (weekly) | 240.0 [90.0, 540.0] | 270.0 [80.0, 480.0] | 255.0 [90.0, 480.0] | 240.0 [90.0, 420.0] |
| Minutes of Walking (weekly) | 360.0 [140.0, 840.0] | 337.5 [140.0, 840.0] | 360.0 [140.0, 840.0] | 315.0 [120.0, 840.0] |
| Minutes of Sitting (daily) | 180.0 [120.0, 300.0] | 180.0 [120.0, 300.0] | 180.0 [120.0, 300.0] | 205.0 [120.0, 300.0] |
| DEMOGRAPHICS | ||||
| Gender | ||||
| 1: Male | 13 (6.3%) | 19 (8.4%) | 3 (1.5%) | 3 (1.4%) |
| 2: Female | 192 (93.7%) | 207 (91.6%) | 195 (98.5%) | 215 (98.6%) |
| Age | 37.3 (± 11.07) | 37.0 (± 11.09) | 38.4 (± 11.04) | 37.5 (± 11.39) |
| Occupation | ||||
| 1: Staff Nurse | 182 (88.8%) | 197 (86.4%) | 180 (90.9%) | 200 (89.3%) |
| 2: Patient Care Associate | 14 (6.8%) | 22 (9.6%) | 8 (4.0%) | 7 (3.1%) |
| 3: Clinical Nurse Specialist | 5 (2.4%) | 3 (1.3%) | 5 (2.5%) | 4 (1.8%) |
| 4: Other | 4 (2.0%) | 6 (2.6%) | 5 (2.5%) | 13 (5.8%) |
| Hours Worked | ||||
| 1: less than 30 hours | 37 (18.0%) | 41 (18.0%) | 54 (27.3%) | 51 (22.8%) |
| 2: 30-34 hours | 14 (6.8%) | 15 (6.6%) | 13 (6.6%) | 19 (8.5%) |
| 3: 35-39 hours | 98 (47.6%) | 108 (47.4%) | 87 (43.9%) | 105 (46.9%) |
| 4: 40-44 hours | 51 (24.8%) | 58 (25.4%) | 39 (19.7%) | 44 (19.6%) |
| 5: over 44 hours | 6 (2.9%) | 6 (2.6%) | 5 (2.5%) | 5 (2.2%) |
| Typical Shift | ||||
| 1: Day | 31 (15.0%) | 36 (15.8%) | 46 (23.2%) | 64 (28.6%) |
| 2: Evening | 6 (2.9%) | 5 (2.2%) | 2 (1.0%) | 1 (0.4%) |
| 3: Night | 45 (21.8%) | 43 (18.9%) | 48 (24.2%) | 58 (25.9%) |
| 4: Other | 124 (60.2%) | 144 (63.2%) | 102 (51.5%) | 101 (45.1%) |
In general, the magnitude of the changes in the primary outcomes was small and there were no significant between-group differences (Table 3). The findings were similar when we included only the embedded cohort of survey respondents who completed both surveys and were present on the units for the entire intervention period (data not shown).
Table 3.
Adjusted mean or percent of primary outcome measures by time of survey and intervention condition, change from baseline to follow-up and p-value for test of difference in change between intervention and control units.
| Primary Outcomes | Adjusted Means and Percents | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Intervention Units (4) | Control Units (4) | p-value | |||||
| Pre | Post | Change | Pre | Post | Change | ||
| Pain severity (mean) | 2.43 | 2.68 | +0.25 | 2.57 | 2.41 | -0.15 | 0.09 |
|
| |||||||
| Any pain (%) | 79.01% | 78.65% | -0.36% | 82.34% | 75.68% | -6.65% | 0.27 |
|
| |||||||
| Work Interference (%) | 24.14% | 23.87% | -0.27% | 23.16% | 15.30% | -7.85% | 0.15 |
|
| |||||||
| Fruit / Veggies (servings per day) | 2.86 | 2.87 | +0.01 | 2.78 | 2.90 | +0.12 | 0.46 |
|
| |||||||
| Sugary Snacks (servings per day) | 0.32 | 0.29 | -0.03 | 0.27 | 0.28 | +0.01 | 0.38 |
|
| |||||||
| Sugary Drinks (servings per day) | 0.50 | 0.52 | +0.02 | 0.46 | 0.41 | -0.05 | 0.25 |
|
| |||||||
| Fast Food (servings per day) | 0.06 | 0.06 | +0.00 | 0.04 | 0.04 | +0.01 | 0.77 |
|
| |||||||
| Combined Weekly PA Minutes 1 (Mod + Vig) | 154.60 | 157.60 | +3.00 | 168.90 | 145.80 | -23.10 | 0.36 |
|
| |||||||
| Weekly Minutes of Walking 1 | 277.70 | 269.40 | -8.30 | 299.90 | 269.30 | -30.60 | 0.62 |
|
| |||||||
| Daily Minutes of Sitting 1 | 168.40 | 165.50 | -2.90 | 173.10 | 181.60 | +8.50 | 0.58 |
|
| |||||||
| Sleep Deficiency (%) | 65.85% | 63.32% | -2.53% | 63.19% | 58.04% | -5.15% | 0.72 |
-Mixed models include time of survey (pre or post) and intervention / control unit for all workers in the 8 units
Adjusted for clustering of participants in units and for the repeated measures.
- The PA minutes variables were transformed to the Log scale to meet the assumptions of the model. The adjusted means estimates displayed are transformed back to the minutes scale.
The magnitude of the changes in the proximal outcomes, suggested by the conceptual model in Figure 1, also was small, and in general there were no significant between-group differences, with one unexpected exception (Table 4). Safety practices declined in the intervention units relative to controls, although the magnitude of change was small. Findings were similar for the embedded cohort (data not shown).
Table 4.
Adjusted mean or percent of proximal outcome measures by time of survey and intervention condition, change from baseline to follow-up and p-value for test of difference in change between intervention and control units
| Proximal Outcomes | Adjusted Means and Percents | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Intervention Units (4) | Control Units (4) | p-value | |||||
| Pre | Post | % Change | Pre | Post | % Change | ||
| Ergonomic Practices | 3.30 | 3.27 | -0.03 | 3.25 | 3.32 | +0.07 | 0.24 |
|
| |||||||
| Supervisor Support | 10.71 | 10.67 | -0.04 | 11.99 | 12.13 | +0.14 | 0.58 |
|
| |||||||
| Coworker Support | 8.64 | 8.62 | -0.01 | 8.79 | 8.79 | +0.00 | 0.91 |
|
| |||||||
| Safety Practices | 4.05 | 3.83 | -0.22 | 4.07 | 4.07 | +0.00 | 0.004 |
|
| |||||||
| Meal Break Frequency | 2.60 | 2.70 | +0.10 | 2.68 | 2.71 | +0.03 | 0.36 |
-Mixed models include time of survey (pre or post) and intervention / control unit for all workers in the 8 units
Adjusted for clustering of participants in units and for the repeated measures.
Discussion
This paper reports results of a PoC trial that examined the feasibility and estimated the efficacy of an integrated intervention designed to reduce MSD risk and promote healthy behaviors, including physical activity, diet and sleep, with the aim of understanding factors affecting intervention implementation. The BWWW intervention included consultation for nurse managers to implement changes on their patient care units that would protect and promote worker health and safety, as well as educational programming for patient care staff to facilitate improvements in safety and health behaviors. We used a mixed-methods approach to evaluate feasibility and efficacy, drawing on findings from our qualitative research, process evaluation of intervention implementation, and surveys of workers examining changes in our targeted outcomes. Based on these data, this PoC study identified barriers to the feasibility of this intervention and found no significant intervention effects.
We encountered significant challenges to implementing the intervention, arising particularly from the physical demands2 and psychological challenges in patient care. 50-52 From our qualitative data, it was clear that both nurse managers and their staff were well aware of the health and safety implications related to the physical and emotional demands of caring for patients around the clock. In the face of these demands it is not surprising that nurse managers restricted the frequency and amount of time the BWWW team could be present on the patient care units to no more than one visit per shift each month. In addition, for most intervention activities, participants’ exposure was for less than ten minutes. Understanding these time constraints, we incorporated other opportunities for engaging staff members outside work time. Participation in these activities, however, was quite low; for example, across all four intervention units, only seven individuals (of approximately 220 eligible) signed up for telephone coaching calls intended to support health and safety behavior changes. We observed particular challenges to intervention delivery and participation in the two ICU’s, where patient care demands were greatest.
Time constraints and limited bandwidth to attend to issues beyond patient care also appeared to deter implementation of recommended changes to unit practices, such as those resulting from the ergonomic hazards assessments. In addition, because the intervention tested in this PoC trial was implemented on only four inpatient care units, rather than hospital-wide, it may have missed opportunities for organization-wide support. Since action plans were still being adopted at the end of the intervention period, we cannot definitely determine the extent to which the recommended changes were ultimately implemented; turnover of key managers may have been a contributing factor to inadequate implementation during the study period. Nonetheless, the qualitative data clearly underscored the need for upper management support and commitment for any changes to be initiated and implemented. Indeed, successful implementation of an integrated health protection-health promotion intervention may require continuous involvement from upper management at the hospital level.53 While this study received full endorsement by upper management, the limited reach of this intervention centering on a small number of units made it difficult to involve upper management on a continuous basis in terms of hospital-wide communication and in the continuous visibility of leadership support. Recent reviews54 and best practice guidelines53 have demonstrated that injuries can be reduced by comprehensive programs that engage multiple departments and are supported by upper management. Coupled together, these recommendations and our findings suggest that the conceptual model presented in Figure 1 might be modified to include hospital-level intervention targets.
In light of the considerable challenges to intervention delivery, it is not surprising that we did not see significant improvements in our intervention outcomes, based on patient care workers’ reports of pain, work interference, physical activity, dietary patterns, and sleep deficiency in the intervention and comparison units. The conceptual model provides a structure for understanding these results in terms of a process-to-outcome evaluation. As illustrated in Figure 1, we anticipated that the intervention would influence the outcomes by effecting change in the intervention targets at the unit level, including the work environment and the work organization, and at the individual level. At the unit level, despite assessments of the work environment and organization that informed recommendations, few changes in work practices were implemented during the study period. Based on the survey results, there were no significant changes in ergonomic practices, supervisor support or break practices, as shown in Table 4. Unexpectedly, reported safety practices declined significantly on the intervention units. This result may reflect an increased awareness of optimal practices accompanied by a recognition that actual practices fell short of optimal. Alternatively, this result may reflect a true unintended result. In either case, it warrants further exploration. At the individual level, exposure to the intervention was generally lower than expected. These findings suggest that the intervention was not effective in changing the intervention targets, underscoring our conclusion that beyond the unit level, there is a need for system-wide involvement and upper management support in order for interventions in this setting to influence worker health outcomes effectively.
The literature supports our conclusion about the centrality of system-wide policies and practices. Others have observed the importance of the hospital safety climate to safe work practices, including the need for upper management commitment,55 support from one’s immediate supervisor,56 and adequate staffing.4,57-59 Nonetheless, despite efforts to improve health and safety for patient care workers through MSD prevention, many gaps in the literature remain.60 Recent systematic reviews of this literature have found few high quality studies, with little strong evidence to support the efficacy of any interventions.54,61 Although manual handling training alone does not appear to be effective54,61-63 and there is little consistent support for “no lift” policies,61,64 multi-dimensional interventions have found some support.54,61,63,65 There is also moderate support for exercise interventions as part of MSD prevention.54,66 These studies further highlight the need for systemic changes that go beyond piece-meal supports.
As a proof-of-concept trial, assessment of feasibility was a primary objective, and identification of challenges to implementation of the intervention was central to this research. This study was not statistically powered to determine efficacy, although the magnitude of the changes observed suggests that refinements to intervention delivery will be needed before a full scale test of a similar intervention in this setting may be warranted. In addition, as a further limitation to this study, because we did not track individual participation as part of the process tracking, we do not know the proportion of workers who attended multiple intervention events.
These findings have implications for future interventions with direct patient care workers. As with any work setting, it is imperative that interventions to protect and promote worker health be designed around an understanding of the conditions of work. For these workers, the pressing demands of patient care combined with a cultural commitment to putting the interests of the patient before those of the healthcare worker create a high-pressured environment, challenging both emotional resilience as well as physical stamina. Building a supportive work environment in the face of these demands requires top management commitment that goes well beyond the unit level to foster system-wide norms and infrastructure supports that can be translated to the unit level.21 Also, based on findings here, planning for unit-based interventions within a supportive infrastructure may need to focus the intervention on a few selected outcomes. Targeting multiple health and safety behaviors in this intervention resulted in a somewhat diffuse effect, limiting the depth of exposure around any single intervention target. Given the complexity of the job demands, simple intervention messages, delivered in a sustained manner and that address fewer intervention targets may be needed, and attention to job stress and building resiliency may be important for policies and practices as well as for programs for individual workers.
In conclusion, this proof-of-concept trial conducted at the patient care unit level was not effective in changing worker safety and health outcomes. Findings from our process tracking indicate that workers’ exposure to the intervention was generally less than ten minutes per month, reflecting the competing demands and pressured environment of direct patient care, as described in focus groups and key informant interviews. For nurse managers of patient care units as well as their staff, these competing demands and time constraints were a major challenge to implementation of the BWWW intervention. As a result of the challenges to implementation of the intervention, we also did not observe improvements in supervisor support, ergonomic and safety practices, and break frequency. Our qualitative findings agree with systematic reviews and best practice guidelines that system-wide initiatives that respond to the conditions of work may be needed to transform the workplace culture and broader milieu in support of worker health and safety. By re-shaping policies and practices across the organization, it may be possible to foster a unit-level climate that will facilitate unit managers’ implementation of effective practices to protect and promote worker health, support workers’ engagement in educational activities, and ultimately contribute to improved safety, health and wellbeing for workers.
Acknowledgments
This work was supported by a grant from the National Occupational Safety and Health (U19 OH008861) for the Harvard T.H. Chan School of Public Health Center for Work, Health and Well-being and by a grant from the National Cancer Institute (R25 CA057713). This study would not have been accomplished without the participation of Partners HealthCare System and leadership from Dennis Colling and Kurt Westerman. The authors would like to thank Partners Occupational Health Services including Marlene Freeley for her guidance, Elizabeth Taylor for her work on the involved hospital units, and Terry Orechia for programming support. We also thank individuals at the hospital including Jeanette Ives Erickson in Patient Care Services leadership, and Jeff Davis in Human Resources. We also thank Karen Hopcia, Caitlin Caspi Eicher, and Evan McEwing for their contributions to intervention planning; Linnea Benson-Whelan for her assistance with the production of this manuscript and contributions to project management; Ruth Lederman for her leadership in survey data collection; Joshua Gagne for his work on the qualitative research; and the Health Communication Core and Survey and Data Management Core at the Dana-Farber/Harvard Cancer Center.
References
- 1.Bureau of Labor Statistics. Number, incidence rate, and median days away from work for nonfatal occupational injuries and illnesses involving days away from work and musculoskeletal disorders by selected worker occupation and ownership 2013. 2013 http://www.bls.gov/news.release/osh2.t18.htm.
- 2.Bureau of Labor Statistics. Occupational Injuries, Illnesses, and Fatalities among Nursing, Psychiatric, and Home Health Aides 1995-2004. 2006 http://www.bls.gov/opub/mlr/cwc/occupational-injuries-illnesses-and-fatalities-among-nursing-psychiatric-and-home-health-aides-1995-2004.pdf.
- 3.Hopcia K, Dennerlein JT, Hashimoto D, Orechia T, Sorensen G. Occupational injuries for consecutive and cumulative shifts among hospital registered nurses and patient care associates: a case-control study. Workplace health & safety. 2012;60(10):437–444. doi: 10.3928/21650799-20120917-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim SS, Okechukwu CA, Dennerlein JT, et al. Association between perceived inadequate staffing and musculoskeletal pain among hospital patient care workers. Int Arch Occup Environ Health. 2014;87(3):323–330. doi: 10.1007/s00420-013-0864-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sembajwe G, Tveito TH, Hopcia K, et al. Psychosocial stress and multi-site musculoskeletal pain: a cross-sectional survey of patient care workers. Workplace health & safety. 2013;61(3):117–125. doi: 10.1177/216507991306100304. [DOI] [PubMed] [Google Scholar]
- 6.Reme SE, Dennerlein JT, Hashimoto D, Sorensen G. Musculoskeletal pain and psychological distress in hospital patient care workers. J Occup Rehabil. 2012;22(4):503–510. doi: 10.1007/s10926-012-9361-5. PMCID 3671916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stone PW, Clarke SP, Cimiotti J, Correa-de-Araujo R. Nurses’ Working Conditions: Implications for Infectious Disease. Emerging Infectious Diseases. 2004;10(11):1984–1989. doi: 10.3201/eid1011.040253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buxton OM, Hopcia K, Sembajwe G, et al. Relationship of sleep deficiency to perceived pain and functional limitations in hospital patient care workers. J Occup Environ Med. 2012;54(7):851–858. doi: 10.1097/JOM.0b013e31824e6913. PMCID 3720240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hildebrandt VH, Bongers PM, Dul J, van Dijk FJ, Kemper HC. The relationship between leisure time, physical activities and musculoskeletal symptoms and disability in worker populations. Int Arch Occup Environ Health. 2000;73:507–518. doi: 10.1007/s004200000167. [DOI] [PubMed] [Google Scholar]
- 10.Hartvigsen J, Christensen K. Active lifestyle protects against incident low back pain in seniors: a population-based 2-year prospective study of 1387 Danish twins aged 70-100 years. Spine (Phila Pa 1976) 2007;32(1):76–81. doi: 10.1097/01.brs.0000250292.18121.ce. [DOI] [PubMed] [Google Scholar]
- 11.Stroyer J, Jensen LD. The role of physical fitness as risk indicator of increased low back pain intensity among people working with physically and mentally disabled persons: a 30-month prospective study. Spine (Phila Pa 1976) 2008;33(5):546–554. doi: 10.1097/BRS.0b013e3181657cde. [DOI] [PubMed] [Google Scholar]
- 12.Canivet C, Ostergren PO, Choi B, et al. Sleeping problems as a risk factor for subsequent musculoskeletal pain and the role of job strain: results from a one-year follow-up of the Malmo Shoulder Neck Study Cohort. Int J Behav Med. 2008;15(4):254–262. doi: 10.1080/10705500802365466. [DOI] [PubMed] [Google Scholar]
- 13.Jones EA, McBeth J, Nicholl B, et al. What characterizes persons who do not report musculoskeletal pain? Results from a 4-year Population-based longitudinal study (the Epifund study) J Rheumatol. 2009;36(5):1071–1077. doi: 10.3899/jrheum.080541. [DOI] [PubMed] [Google Scholar]
- 14.Jones F, O’Connor DB, Conner M, McMillan B, Ferguson E. Impact of daily mood, work hours, and iso-strain variables on self-reported health behaviors. J Appl Psychol. 2007;92(6):1731–1740. doi: 10.1037/0021-9010.92.6.1731. [DOI] [PubMed] [Google Scholar]
- 15.Caruso C, Hitchcock E, Dick R, Russo J, Schmitt J. Overtime and extended work shifts: recent findings on illnesses injuries, and health behaviors. [October 25, 2010];2004 :1–38. http://www.cdc.gov/niosh/docs/2004-143/default.html.
- 16.Trinkoff AM, Storr CL, Lipscomb JA. Physically demanding work and inadequate sleep, pain medication use, and absenteeism in registered nurses. J Occup Environ Med. 2001;43(4):355–363. doi: 10.1097/00043764-200104000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Sorensen G, Stoddard AM, Stoffel S, et al. The role of the work context in multiple wellness outcomes for hospital patient care workers. J Occup Environ Med. 2011;53(8):899–910. doi: 10.1097/JOM.0b013e318226a74a. PMCID 3693572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geiger-Brown J, Trinkoff A, Rogers VE. The impact of work schedules, home, and work demands on self-reported sleep in registered nurses. J Occup Environ Med. 2011;53(3):303–307. doi: 10.1097/JOM.0b013e31820c3f87. [DOI] [PubMed] [Google Scholar]
- 19.Sonnentag S. Psychological detachment from work during off-job time: the role of job stressors, job involvement & recovery-related self-efficacy. Eur J Work Organ Psychol. 2006;15:197–217. [Google Scholar]
- 20.Sorensen G, McLellan D, Dennerlein J, et al. Integration of Health Protection and Health Promotion: Rationale, Indicators, and Metrics. J Occup Environ Med. 2013 Dec;55(12 Suppl):S12–18. doi: 10.1097/JOM.0000000000000032. PMCID 4184212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sorensen G, McLellan D, Dennerlein J, et al. Integrating Worksite Health Protection and Health Promotion: A Conceptual Model for Intervention and Research. Am J Public Health in review. doi: 10.1016/j.ypmed.2016.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anger WK, Elliot DL, Bodner T, et al. Effectiveness of Total Worker Health interventions. J Occup Health Psychol. 2015;20(2):226–247. doi: 10.1037/a0038340. [DOI] [PubMed] [Google Scholar]
- 23.Audeh MW, Carmichael J, Penson RT, et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancer: a proof-of-concept trial. Lancet. 2010;376(9737):245–251. doi: 10.1016/S0140-6736(10)60893-8. [DOI] [PubMed] [Google Scholar]
- 24.Litz BT, Engel CC, Bryant RA, Papa A. A randomized, controlled proof-of-concept trial of an Internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. Am J Psychiatry. 2007;164(11):1676–1683. doi: 10.1176/appi.ajp.2007.06122057. [DOI] [PubMed] [Google Scholar]
- 25.Elble RJ, Biondi DM, Ascher S, Wiegand F, Hulihan J. Carisbamate in essential tremor: brief report of a proof of concept study. Mov Disord. 2010;25(5):634–638. doi: 10.1002/mds.22872. [DOI] [PubMed] [Google Scholar]
- 26.Chen W, Akay M. A Low Cost and Customizable Electronic Medical Records for Developing Nations. IEEE Trans Inf Technol Biomed. 2010 [Google Scholar]
- 27.Boden LI, Sembajwe G, Tveito TH, et al. Occupational injuries among nurses and aides in a hospital setting. Am J Ind Med. 2012;55(2):117–126. doi: 10.1002/ajim.21018. [DOI] [PubMed] [Google Scholar]
- 28.Dennerlein JT, Hopcia K, Sembajwe G, et al. Ergonomic practices within patient care units are associated with musculoskeletal pain and limitations. Am J Ind Med. 2012;55(2):107–116. doi: 10.1002/ajim.21036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim SS, Okechukwu CA, Buxton OM, et al. Association between work-family conflict and musculoskeletal pain among hospital patient care workers. Am J Ind Med. 2013;56(4):488–495. doi: 10.1002/ajim.22120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Caspi CE, Dennerlein JT, Kenwood C, et al. Results of a pilot intervention to improve health and safety for healthcare workers. J Occup Environ Med. 2013;55:1449–1455. doi: 10.1097/JOM.0b013e3182a7e65a. PMCID 3858503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Umukoro PE, Arias O, Stoffel SD, Hopcia K, S G, Dennerlein JT. Physical activity at work contributes little to patient care workers’ weekly totals. J Occup Environ Med. 2013;55(12 Suppl):S63–68. doi: 10.1097/JOM.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 32.Jacobsen HB, Reme SE, Sembajwe G, et al. Work stress, sleep deficiency, and predicted 10-year cardiometabolic risk in a female patient care worker population. Am J Ind Med. 2014 May 8; doi: 10.1002/ajim.22340. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tveito T, Sembajwe G, Boden L, et al. Impact of organizational policies and practices on workplace injuries in a hospital setting. Journal of Occupational and Environmental Medicine. 2014;56(8):802–808. doi: 10.1097/JOM.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 34.Reme SE, Shaw WS, Boden LI, et al. Worker assessments of organizational practices and psychosocial work environment are associated with musculoskeletal injuries in hospital patient care workers. Am J Ind Med. 2014;57(7):810–818. doi: 10.1002/ajim.22319. [DOI] [PubMed] [Google Scholar]
- 35.Jacobsen H, Reme S, Sembajwe G, et al. Work-family conflict, psychological distress, and sleep deficiency among patient care workers. Workplace health & safety. 2014;62(7):282–291. doi: 10.3928/21650799-20140617-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hurtado D, Nelson CC, Hashimoto D, Sorensen G. Supervisors’ support for nurses’ meal breaks and mental health. Workplace health & safety. 2015;63(3):107–115. doi: 10.1177/2165079915571354. [DOI] [PubMed] [Google Scholar]
- 37.National Institute for Occupational Safety and Health. Essential Elements of Effective Workplace Programs and Policies for Improving Worker Health and Wellbeing. [July 7, 2010];2009 http://www.cdc.gov/niosh/worklife/essentials.html.
- 38.Sabbath EL, Hurtado DA, Okechukwu CA, et al. Occupational injury among hospital patient-care workers: What is the association with workplace verbal abuse? American journal of industrial medicine. 2014;57(2):222–232. doi: 10.1002/ajim.22271. [DOI] [PubMed] [Google Scholar]
- 39.Grant AM, Zackon R. Executive, workplace, and life-coaching: Findings from a large-scale survey of International Coach Federation members. Int J Evidence-based Coaching and Mentoring. 2004;2:1–15. [Google Scholar]
- 40.Miller WR, Rollnick S. Motivational interviewing : helping people change. New York, NY: Guilford Press; 2013. [Google Scholar]
- 41.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia: 2009. [Google Scholar]
- 42.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 43.Buxton OM, Quintiliani LM, Yang MH, et al. Association of sleep adequacy with more healthful food choices and positive workplace experiences among motor freight workers. Am J Public Health. 2009;99(Suppl 3):S636–643. doi: 10.2105/AJPH.2008.158501. PMCID 2774168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harley AE, Yang M, Stoddard AM, et al. Patterns and predictors of health behaviors among racially/ethnically diverse residents of low-income housing developments. Am J Health Promot. 2014;29(1):59–67. doi: 10.4278/ajhp.121009-QUAN-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Prochaska JJ, Velicer WF, Nigg CR, Prochaska JO. Methods of quantifying change in multiple risk factor interventions. Prev Med. 2008;46(3):260–265. doi: 10.1016/j.ypmed.2007.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kuorinka I, Jonsson B, Kilbom A, et al. Standardized Nordic Questionnaires for the analysis of musculoskeletal symptoms. Applied Ergonomics. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 47.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 48.Karasek R, Theorell T. Healthy work: Stress, productivity, and the reconstruction of working life. New York, NY: Basic Books; 1990. [Google Scholar]
- 49.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 50.Grant L, Kinman G. The importance of emotional resilience for staff and students in the ‘helping’ professions: developing an emotional curriculum. The Higher Education Academy - Health and Social Care. 2013 [Google Scholar]
- 51.Aiken L, Sermeus W, Van den Heede K, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012;344e:1717. doi: 10.1136/bmj.e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McCann CM, Beddoe E, McCormick K, et al. Resilience in the health professions: A review of recent literature. Int J Wellbeing. 2013;3(1):60–81. [Google Scholar]
- 53.Massachusetts Department of Public Health OHSP. Moving into the Future: Promoting safe patient handling for worker and patient safety in Massachusetts hospitals. 2014 http://www.mass.gov/eohhs/docs/dph/occupational-health/ergo-sph-hospitals-2014.pdf.
- 54.Tullar JM, Brewer S, Amick BC, 3rd, et al. Occupational safety and health interventions to reduce musculoskeletal symptoms in the health care sector. J Occup Rehabil. 2010;20(2):199–219. doi: 10.1007/s10926-010-9231-y. [DOI] [PubMed] [Google Scholar]
- 55.Gershon RR, Karkashian CD, Grosch JW, et al. Hospital safety climate and its relationship with safe work practices and workplace exposure incidents. American journal of infection control. 2000;28(3):211–221. doi: 10.1067/mic.2000.105288. [DOI] [PubMed] [Google Scholar]
- 56.Eriksen W, Bruusgaard D, Knardahl S. Work factors as predictors of intense or disabling low back pain; a prospective study of nurses’ aides. Occup Environ Med. 2004;61(5):398–404. doi: 10.1136/oem.2003.008482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lipscomb J, Trinkoff A, Brady B, Geiger-Brown J. Health care system changes and reported musculoskeletal disorders among registered nurses. Am J Public Health. 2004;94(8):1431–1435. doi: 10.2105/ajph.94.8.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Geiger-Brown J, Trinkoff AM, Nielsen K, Lirtmunlikaporn S, Brady B, Vasquez EI. Nurses’ perception of their work environment, health, and well-being: a qualitative perspective. Aaohn J. 2004;52(1):16–22. [PubMed] [Google Scholar]
- 59.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 60.Waters T, Collins J, Galinsky T, Caruso C. NIOSH research efforts to prevent musculoskeletal disorders in the healthcare industry. Orthop Nurs. 2006;25(6):380–389. doi: 10.1097/00006416-200611000-00007. [DOI] [PubMed] [Google Scholar]
- 61.Dawson AP, McLennan SN, Schiller SD, Jull GA, Hodges PW, Stewart S. Interventions to prevent back pain and back injury in nurses: a systematic review. Occup Environ Med. 2007;64(10):642–650. doi: 10.1136/oem.2006.030643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hignett S. Intervention strategies to reduce musculoskeletal injuries associated with handling patients: a systematic review. Occup Environ Med. 2003;60(9):E6. doi: 10.1136/oem.60.9.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Burton AK, Balague F, Cardon G, et al. How to prevent low back pain. Best Pract Res Clin Rheumatol. 2005;19(4):541–555. doi: 10.1016/j.berh.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 64.Yassi A, Cooper JE, Tate RB, et al. A randomized controlled trial to prevent patient lift and transfer injuries of health care workers. Spine (Phila Pa 1976) 2001;26(16):1739–1746. doi: 10.1097/00007632-200108150-00002. [DOI] [PubMed] [Google Scholar]
- 65.Lagerstrom M, Hansson T, Hagberg M. Work-related low-back problems in nursing. Scand J Work Environ Health. 1998;24(6):449–464. doi: 10.5271/sjweh.369. [DOI] [PubMed] [Google Scholar]
- 66.Maul I, Laubli T, Oliveri M, Krueger H. Long-term effects of supervised physical training in secondary prevention of low back pain. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2005;14(6):599–611. doi: 10.1007/s00586-004-0873-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


