Abstract
Background
Added sugar intake in the form of sugar-sweetened beverages (SSB) has been considered a contributor to weight gain and cardiometabolic dysfunction in adults and youth. Adolescents are some of the highest consumers of added sugars, taking in ~16% of their total calories from added sugars with ~40% of these calories coming from SSB. Youth’s food preferences and self-regulation of dietary intake can be influenced by parents.
Objective
To evaluate the Theory of Planned Behavior’s (TPB) effectiveness in understanding and predicting adolescents' SSB consumption, identify which constructs are the most important when evaluating SSB consumption in adolescents, and determine if and how adolescents' beverage choices are influenced by parents' reactions to their beverage choices.
Design
Measurements for this cross-sectional study included four record-assisted 24-hour dietary recalls and responses to a SSB-specific TPB questionnaire from 100 adolescents. Consenting parents completed a beverage intake questionnaire, a TPB questionnaire, and Parent Response to Beverage Choice Questionnaire.
Results
The TPB explained 34% of the variance in adolescents' and parents' intention to limit SSB to less than one cup per day. Parents' perceived behavioral control (b=1.35, p=0.002) and adolescents' subjective norms (b=0.57, p=0.001) were the strongest predictors of intention, and intention was the strongest predictor of SSB consumption in both adolescents and parents (b=−37, p=0.026, b=−49, p=0.003). The TPB explained more variance in parent SSB consumption (R2=0.38) than adolescents (R2=0.22). Parents did more discouraging of SSB and encouraging of non-SSB. Adolescents' intention to limit SSB moderated the relationship between parents' reactions encouraging SSB and adolescents' predicted SSB consumption (p=0.021).
Conclusions
The TPB explained a small, but significant amount of variance in adolescents' SSB consumption. When addressing adolescent SSB intake, people in addition to parents may influence their intentions and SSB consumption.
Keywords: adolescents, parents, sugar-sweetened beverages, sugary drinks, Theory of Planned Behavior
Introduction
Adolescence is a time characterized by dramatic changes psychologically, socially, and physiologically.1 Despite adolescents' attempts to become autonomous,2 with greaterfreedom and responsibility, parents remain primary sources of nourishment physically and emotionallyby providing food, economic support, and empathy.1 More specifically, during adolescence there is greater consumption of energy-dense foods and conventional eating patterns can be shunned, 2,3 potentially resulting in overweight and obesity.
About one-third of US youth are overweight or obese,4 and excessive weight gain in youth may track into adulthood and contribute to cardiovascular risk.5 The development of overweight and obesity in youth may result from overconsumption of added sugars, specifically sugar-sweetened beverages (SSB),6 which are beverages that contain added caloric sweeteners and include soda, energy drinks, sweet tea, sports drinks, and fruit drinks.7 Ervin and colleagues found that 2-18 year olds consume about 16% of total energy from added sugars with approximately 41% of these calories coming from SSB.8 However, the Scientific Report of the 2015 Dietary Guidelines Advisory Committee has recommendations for limiting added sugar intake, which includes SSB, to a maximum of 10% of daily calories.9 In adolescents, excessive SSB intake has been associated with increased risk of diabetes10 and cardiovascular disease risk.11
Youth aged 2-19 years consume approximately 155 kcal, or about 12 fl. oz. of soda, per day from SSB,12 which is in excess of the American Heart Association's recommendation of 450 kcal per week from added sugars.13 While consumption of soda, previously the highest contributor to SSB intake in adolescents,14 has recently decreased,12 100% fruit juice,15 sweetened coffee and tea, and sports and energy drink12 consumption has increased. Sports and energy drink consumption has increased threefold since 198814 and continues to rise, especially in adolescents.12 Sports drink consumption has also been associated with increases in youth’s BMI.16 The American Academy of Pediatrics recommends that sports and energy drinks not be consumed regularly by adolescents, as these beverages can contribute to excessive energy intake.17
Parents are known to help mold youth's attitudes and beliefs about food and eating practices.18 Modeling overconsumption and parent feeding practices that are controlling or restrictive have detrimental effects on children's BMI19 and food regulatory behaviors and preferences.20 Thus, parents may play a crucial role influencing food beliefs and behaviors inadolescents.21
Theory-based models for predicting health behaviors may be more successful when examining health behavior change, compared to those not grounded in theory.22 The Theory of Planned Behavior (TPB)23 is one psychosocial theory that can be used to address adolescent eating behaviors. According to the TPB, behavioral action occurs from the influence attitude, subjective norm, and perceived behavioral control have on intention, the most proximal determinant of behavior.23 The Theory has been successful in predicting and understanding many health-related behaviors,24-26 and the information gained from application of the TPB can help create customized, relevant, and possibly more effective interventions.25 A recent review of the TPB’s use in predicting and understanding youth’s diet-related behaviors identified eight publications that investigated sugary drink intake; however, many were conducted outside the United States, have limitations on SSB consumption assessment, and did not directly measure parents’ responses to their child’s sugary beverage consumption.27
The purpose of this investigation was to evaluate the TPB’s ability to predict adolescents' and parents' SSB consumption, identify which constructs are the most important when evaluating SSB consumption in adolescents and parents, and determine the degree to which adolescents' beverage choices are associated with parents' reactions to their beverage choices. Also explored was the mediating role the TPB played when examining the potential relationship between parental response and adolescents SSB consumption. It is hypothesized that 1) all TPB constructs will be correlated to adolescents' intention, 2) attitude will be the strongest predictor of adolescents' behavioral intention, 3) behavioral intention will be the strongest predictor of adolescents' behavior (i.e., SSB intake), 4) adolescents and parents will have different TPB constructs emerge as the most predictive of intention to limit SSB intake, and 5) adolescents' attitude and intention will moderate the relationship between parental responses to adolescents' beverage choices and SSB consumption.
Methods
A convenience sample of 102 adolescents aged 12-18 years were recruited through email listservs, community newspapers, paper flyers, and word of mouth for participation in this cross-sectionalinvestigation. A sample of this size can provide adequate power to detect associations between individual's nutrient intakes and have the greatest statistical precision when each participant provides three days or more of dietary information.28 Interested adolescents were included once parental permission was obtained and if they met the specified age criteria; could read, write, and speak English; and were willing to comply with study procedures. Adolescents were targeted in this investigation due to their obesity prevalence rate4 and known high added sugar and SSB consumption.8 Furthermore, in the National Health and Nutrition Examination Survey (NHANES)29 adolescents do not need proxy reporters (i.e. parents) when disclosing their dietary intake. Parents accompanying children were also invited to participate and completed questionnaires at their child’s first study visit.
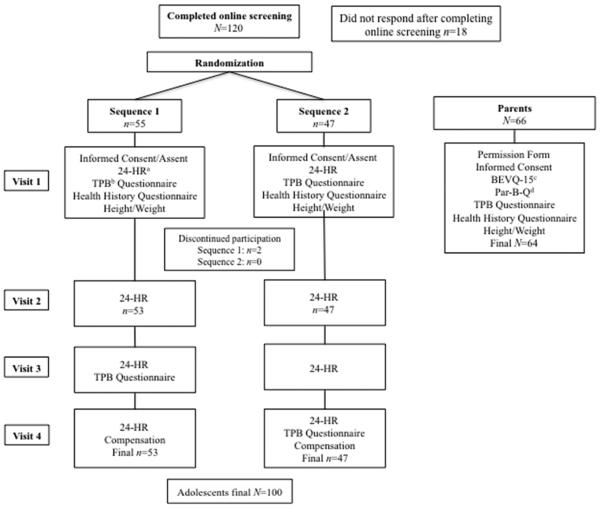
This investigation was part of a larger, ongoing dietary assessment trial, which included randomizing visit sequences; thus, adolescent participants were randomized to one of two visit sequences, and completed four laboratory sessions within a one to three week period (Figure 1). Overthe entire study duration, adolescents completed four 24-hour dietary recalls (24HR), the TPB questionnaire at two separate visits, a health history questionnaire, and had their height and weight measured. Consenting parents completed a health history questionnaire, the beverage intake questionnaire(BEVQ-15)30, the TPB tool31, the Parent Response to Beverage Choice Questionnaire (Par-B-Q), and had their height and weight measured. For both adolescents and parents, height was measured and recorded in centimeters without shoes using a wall mounted stadiometer (Seca 216, Hamburg, Germany), and body weight was measured in light clothing without shoes, to the nearest 0.1 kg using a digital scale (Scale-Tronix, Wheaton, IL). Body mass index (BMI) [kg/m2] and BMI-for-age percentile were calculated for each adolescent,32 and BMI was calculated for each parent. Study procedures and questionnaires were pilot tested with three adolescents and their parents; modifications were made according to their feedback. The Virginia Polytechnic Institute and State University Institutional Review Board approved the study protocol. Adolescent participants provided written assent or informed consent depending on age (below or above the age of 18, respectively) and parent participants provided informed consent prior to any data collection.
Figure 1.
Study procedures for a Mixed Methods Analysis of Beverage Choices in Adolescents and Their Parents using the Theory of Planned Behavior with participation.
aRecord assisted 24-hour dietary recall
bTheory of Planned Behavior
cBeverage intake questionnaire-1530
dParent response to beverage choice questionnaire
Adolescent and Parent Beverage Intake Assessment
Adolescents had a record-assisted 24HR administered at each study session. Adolescents' dietary intake is known to vary from day-to-day;33 thus, four 24HR were collected since this has been identified as optimal for examining usual intake of most nutrients and foods in youth.34,35 Recalls were obtained on non-consecutive days using the automated multiple pass method (AMPM), similar to procedures used in NHANES.29 The AMPM provides a more accurate diet recall with decreased subject burden,36 when administered by a trained individual. Participants were provided with a food-recording booklet that was to be used the day prior to each study session, and would serve as a reference when being administered the 24HR. Participants were told they can record as much information as they felt necessary, but were asked to provide the time, location, and list of foods and beverages consumed minus portion sizes and descriptions.37 Sessions were scheduled to collect data from weekdays and weekend days since added sugar intake in children and adolescents is known to be higher on Fridays and Saturdays versus other days of the week.35 Recalls were entered and analyzed using nutritional analysis software (Nutrition Data System for Research [NDS-R], University of Minnesota, Minneapolis, MN, 2013). The average water fluid ounces (fl. oz.), SSB fl. oz. and kcal, and total beverage fl. oz., and kcal consumed were calculated from the four 24HR.
Parents completed the Beverage Intake Questionnaire (BEVQ-15) at their visit, which typically was the adolescents' first session. The BEVQ-15 is a quantitative food frequency questionnaire providing an estimate of habitual beverage intake across 15 beverage categories that evaluates total beverage and SSB intake (i.e., grams and kcal).30 This tool is valid and reliable in adults30 and is sensitive to detect changes in beverage intake patterns over time.38It includes individual items for soda, diet soda, 100% fruit juice, sports and energy drinks,coffee and tea with added cream and sweetener, and coffee and tea without added cream and/or sweetener, among others. Water included drinking water from the tap, bottles, and fountains, not water found in foods. Beverages with added sugars (i.e. sweetened juice beverage/drinks, regularsoft drinks, sweetened tea, coffee/tea with added creamer and/or sugar, mixed alcoholic drinks, and energy and sports drinks) were considered SSB.30
Parent and Adolescent Theory of Planned Behavior Questionnaires
Parents and their children were administered different TPB questionnaires, and the reference behavior was "less than one cup of sugar-sweetened drinks each day." Adolescents were administered the TPB questionnaire two times (time 1=TPB 1, time 2=TPB 2), with anywhere from threeto 14 days between measures, to assess test-re-test reliability. The TPB questionnaire previously validated and used in adults31 was modified for adolescents to relate to their language andcognitive capacity since during the pilot testing participants expressed confusion with some of the wording contained within items. For example, the seven-point semantic differential scale used in theadult TPB tool was reduced to five responses omitting the "slightly…" categories from each question and changing the "quite…" responses to "sort-of…" and the word “value” was replaced with “care about” in subjective norm items. Internal consistency was evaluated for each of the TPB constructs at both time 1 and time 2 using Cronbach's alpha (α).39 While this metric has received criticism40 it is widely accepted for assessing internal reliability of questionnaires and surveys used in research. Values below 0.50 may beacceptable in original research41 and values less than 0.7042 can be acceptable in psychological research. Attitude was measured with six categories of responses (e.g. enjoyable-unenjoyable, healthy-unhealthy, unsatisfying-satisfying, wise-unwise, boring-exciting, and harmful-beneficial) to the prompt ‘For you, drinking less than 1 cup of SSB each day would be….’ Cronbach (α) for attitude on TPB 1 and 2 increased to 0.64 and 0.67, respectively, after deletion of the third belief measure. Three items each were used to assess subjective norm (e.g. ‘Most people who are important to you want you to drink less than 1 cup of sugary drinks each day.’; α TPB 1=0.55, TPB 2=0.70) and perceived behavior control (e.g.‘You have complete personal control over limiting your sugary drinks to less than 1 cup each day, if you really wanted to.’; α TPB 1=0.64, α TPB 2=0.62after deletion of barrier three), and four items for intention (e.g. ‘How motivated are you to limit your sugary drinks to less than 1 cup each day?’; α TPB 1=0.81, α TPB 2=0.88 after removing motivation item 2).
The parents' TPB questionnaire was used to elicit their attitudes, subjective norms, and perceived behavioral control, and behavioral intention constructs in relation to drinking "less than one sugar-sweetened drink each day."31 Prior work evaluating the TPB questionnaire in adults revealed that the primary TPB constructs explained an acceptable amount of variance (R2=0.38, p<.05) in SSB consumption and had moderate to high internal consistency (Cronbach αs ranging from 0.51 with perceived behavioral control to 0.93 with intentions).31
Parent Response to Beverage Choice Questionnaire (Par-B-Q)
The Par-B-Q was adapted from the validated Coping with Children's Negative Emotions Scale (CCNES).43 The CCNES contains six subscales demonstrating various responses to hypotheticaltroublesome circumstances parents may experience with their child/children; it is a self-reported measure of parents' reactivity to their child's emotions during bothersome situations.43
The questionnaire was tailored to parents' responses to their child drinking the following beverages "at home" or "outside the home," since adolescents consume more SSB at home versus out of the home:8,12 coffee-type, sports or energy drinks, regular soda, juice drinks (all considered SSB), diet soda, and 100% fruit juice (both considered non-SSB). The Par-B-Q was pilot tested in three parents and has not been validated. It retains five of the original CCNES subscales (i.e. distress reaction: "get angry or upset"; punitive reaction: "take it away or restrict him/her from drinking [specific beverage]"; expressive encouragement: "encourage him/her to drink [specific beverage]"; problem-focused reaction: "offer a different drink or ask why he/she chose that drink"; minimization reaction: "do nothing") adapted for relation to beverages. Responses for each respective beverage and subscale ranged from one (i.e. "Very Unlikely") to seven (i.e. "Very Likely"). Mean scores for subscales suggesting encouragement of SSB consumption (i.e. Expressive Encouragement and Minimization Reaction) and subscales suggestive of discouraging SSB intake (i.e. Distress Reaction, Punitive Reaction, Problem Focused Reaction) were calculated for SSB and non-SSB in and outside of the home. Cronbach alphas were acceptable (i.e. α>0.70)44 for all constructs measuring discouraging SSB and non-SSB in and out ofthe home, while constructs measuring encouraging SSB and non-SSB intake in and out of the home were lower (αs ranged from 0.18-0.63). Responses from the Par-B-Q were primarily used to answer the question: are parents' responses to adolescents' beverage choices more discouraging of SSB or encouraging of non-SSB at home/out of the home?
The Par-B-Q last section contained open-ended questions for the parents to complete. The first question was “How often do you talk with your child about beverage choices she/he makes?” with responses of “Often,” “Sometimes,” and “Never.” Other questions pertained to the beverages parents allowed or did not allow their child to drink or purchase, why they discussed beverage choices with their children, and what was important to discuss with their child/children about in regards to beverage choices. Qualitative analyses were conducted with an inductive approach.45 Briefly, themes were identified through open coding and grouping categories and frequency of responses were recorded in Microsoft Excel. Attempts were made to preserve the quality of data while reducing its length (i.e. condensation). Major themes were considered similar responses from ≥50% of parent participants, whileminor themes were considered similar responses from 25-49% of parent participants. 46
Statistical Analyses
Descriptive statistics including means, standard deviations (for TPB responses), standard errors of the mean, and frequencies were used to summarize responses for continuous variables. The assumption of univariate normality was checked by examining skewness and kurtosis for all variables using a cutoff of +/− 3. Simple and bivariate correlations, paired and independent samplet-tests, frequencies, and analysis of variance (ANOVA) were used to assess associations among variables and group differences (e.g., sequence, gender, weight status). To explore the relationship of beverage choices between parent-child dyads, Pearson correlations were assessed for water fl. oz., SSB kcal, and total beverage kcal. Step-wise multiple regression was conducted to assess the TPB questionnaire's utility in predicting adolescents' and parents' SSB consumption. Four separate steps were generated to predict SSB intake using intention in the first, adding perceived behavioral control in the second, then adding attitude and subjective norm in the third, and gender, age, and BMI percentile (BMI for parents) in the fourth. Gender was dummy coded. The resulting correlation and regression coefficients and confidence intervals are presented. Adjusted R2 is also reported due to the acknowledged limitations of using R2 (e.g. overestimation of population variance) in TPB research.47
A moderator analysis was conducted to determine if adolescents' attitude and intention moderated the relationship between parents' responses to adolescents' beverage choices in and out of the home (e.g. encouraging or discouraging SSB and non-SSB consumption in the home, out of the home, andoverall [i.e. combination of responses in or out of the home]) and adolescents' SSB consumption. The SPSS PROCESS macro 48 was used to conduct the moderator and mediator analyses. For the moderator analysis, the PROCESS macro centers variables and creates interaction terms. If the interaction terms were statistically significant a simple slopes analysis, which involves fitting regression equations for the predictor and outcome variables at high (one standard deviation above the mean), average (mean), and low (one standard deviation below the mean), of the moderator wasused to assess the conditional effect a predictor has on an outcome.48,49 Adolescents' attitude towards SSB and intention to limit sugary beverage intake to less than one cup per day were chosen as moderators because these constructs were found to be the most consistently associated with adolescents' dietary intentions and behaviors, respectively.27,50
For the mediation analysis, we examined whether adolescents' TPB constructs mediated the relationship between parental response and adolescents' SSB intake. The significance of the mediation effects was tested using bias-corrected bootstrapping of confidence intervals.49,51 This method is more powerful than other commonly used mediation tests and has more accurate Type 1 error rates because it computes asymmetric confidence limits based on the distribution of the product rather than the normal dispersion, thus correcting for minor asymmetries in the distribution.51 Indirect effects were considered significant when the 95% confidence interval did not include zero.51 An a priori significance level of p≤0.05 was chosen and all statistical analyses were carried out using PASW Statistics (version 22, SPSS Inc., Chicago, IL, 2013).
Results
Demographics
One hundred-twenty individuals completed an online screening form and 18 did not respond to communications for scheduling the first study session (Figure 1). Fifty-five adolescents wererandomized to sequence one and 47 to sequence two; two participants from sequence one discontinued participation after the initial session, leaving 53 sequence one adolescents for data analyses (Figure 1). The total number of adolescent participants enrolled was 102 and 100 completed all study procedures.
Adolescent participants were primarily white (93%) and of normal weight (75%) with just over half being male (52%) (Table 1). Twenty adolescents each reported theirlast completed grade as 7th and 8th, 15 each reported 6th and 11th, 13 reported 10th, 11 reported 9th, and two reported 12th as their last grade completed. There were no significant differences between sequences in gender, age, and BMI-for-age classification.
Table 1.
Demographics and mean beverage intake and Theory of Planned Behavior scores of adolescent and parent participants from a Mixed Methods Analysis of Beverage Choices in Adolescents and Parents using the Theory of Planned Behavior.
| Characteristic | Adolescents
(N=100) |
Parents (N=66) |
|---|---|---|
| Gender, n (%) | ||
| Male | 52 (52) | 9 (14) |
| Female | 48 (48) | 57 (86) |
| Age, years | ||
| Mean age±SE | 14±0.2 | 46±0.7 |
| Race/ethnicity, n (%) | ||
| White | 93 (93) | 64 (97) |
| Black | 2 (2) | 0 |
| Asian | 2 (2) | 1 (1.5) |
| Hispanic | 0 | 2 (3) |
| More than one race | 2 (2) | 0 |
| Not sure | 0 | 1 (1.5) |
| Other | 1 (1) | 0 |
| BMI status, n(%) | ||
| Underweight | 3 (3) a | 4 (6) b |
| Normal weight | 75 (75) a | 29 (45) b |
| Overweight | 15 (15) a | 18 (28) b |
| Obese | 7 (7) a | 14 (21.5) b |
| Beverage Categoryc | ||
| Water,d fl. oz. (SE) | 28 (2) | 32 (2) |
| Sugar-sweetened beverage,e fl. oz.
(SE) |
9 (2) | 12 (2) |
| Sugar-sweetened beverage,e kcal
(SE) |
118 (11) | 118 (16) |
| Total beverage, fl. oz. (SE) | 50 (2) | 63 (3) |
| Total beverage, kcal (SE) | 291 (21) | 285 (27) |
| Theory of Planned Behaviorf | ||
| Attitude (SE) | 3.44 (0.06) | 4.85 (0.16) |
| Subjective norm (SE) | 3.59 (0.07) | 4.56 (0.15) |
| Perceived behavioral control (SE) | 4.48 (0.06) | 6.52 (0.08) |
| Intention (SE) | 3.45 (0.84) | 5.69 (0.22) |
Adolescent BMI-for-age categories: Underweight: <5th percentile, Normal weight: 5th percentile to the 85th percentile, Overweight: 85th to less than 95th percentile, Obese: Equal to or greater than the 95th percentile.
Parent BMI=body mass index; calculated as kg/m2. Underweight: <18.5, Normal weight: 18.5-24.9, Overweight: 25-29.9, Obese≥30.
Adolescent beverage intake was determined using the average of four interviewer-administered 24-hour recalls; parent beverage intake was determined using the beverage intake questionnaire (BEVQ-15).30
Water included drinking water from the tap, bottles, and fountains, not water found in foods.
Sugar-sweetened beverages include regular soft drinks, juice drinks, sweetened tea, coffee/tea with cream and/or sugar, mixed alcoholic drinks, and energy and sports drinks.30
Responses to the Theory of Planned Behavior questionnaire were scored using a seven-point semantic differential scale in parents (i.e. "1" to "7") and a five-point semantic differential scale in adolescents (i.e. "1" to "5").
A total of 66 parents consented to participate in the study. The majority of parents were female (86%), white (97%), married (88%), highly educated (97%) (Table 1), and reported a household income of ≥$55,000 (n=52, 80%). Just under half of parents were considered of normal weight (45%) and BMI ranged from 16-53 kg/m2 (mean±SE=26±1).
Beverage Intake of Adolescents and Parents
Table 1 outlines adolescents' and parents' intake of major beverage categories (i.e. water, SSB, and total beverages). No significant differences were observed in parents when examiningBMI category and main beverage categories from the BEVQ-15. In adolescents, there were no significant differences between sequences in water, SSB, and total beverage intake. However, there were significant differences between genders on SSB and total beverage intake, with females having lower SSB and total beverage fl. oz. and kcal versus males (all p<0.05). On average, male adolescents consumed 57 fl. oz. (SE=3) of total beverages per day, 31 fl. oz. (SE=3) of water,and 12 fl. oz. (SE=1) of SSB. Females drank, on average, 43 fl. oz. (SE=2) of total beverages, 26 fl. oz. (SE=3) of water, and 6 fl. oz. (SE=0.0) of SSB daily. Significant differences were observed between adolescents of differing BMI classifications for total beverage fl.oz. consumption (F(3,96)=3.69, p=0.01) with underweight participants drinking more than normal (p=0.02) and overweight (p=0.03) adolescents, respectively. After splitting the data by last grade completed (i.e. middle school: ≤8th and high school: 9th-12th), differences were observed in water intake with high school participants consuming more than middle school participants (p<0.041; data not shown).
Sixty-four parent-adolescent dyads were available for assessment of correlated beverage intake. No associations were noted between parent and child water (r=0.10, p>0.05), SSB kcal (r=0.12, p>0.05), and total beverage kcal (r=0.17, p>0.05). After splitting the sample according to adolescent age (i.e. ≤14 years and ≥15years) correlations were reassessed; no statistically significant associations were noted between beverage intake in younger adolescents and parents (water: r=0.20, SSB kcal: r=0.13, total beverage kcal: r=0.16, all p>0.05), or between older adolescents and parents (water: r=0.03, SSB kcal: r=0.14, total beverage kcal: r=0.27, all p>0.05).
Predicting Sugary Beverage Consumption in Adolescents and Parents: the Theory of Planned Behavior
There were no significant differences between sequences in mean TPB scores; however, adolescent females had higher mean scores on attitude (p=0.030), subjective norm (p=0.018), and intention (p=0.001) scores versus male adolescents. Middle school participants had significantly lower mean attitude and perceived behavioral control scores versus high school participants (both p≤0.01; Online Supplemental Table). Interestingly, normal weight and obese parents differed in their responses to perceptions of control on the TPB questionnaire (F(3,61)=5.00, p=0.004), with obese individuals having less perceptionof control versus their normal weight counterparts (mean difference=−.710, p=0.003; Online Supplemental Table). All other TPB constructs were not different between BMI categories.
The intercorrelations between sugary beverage intake and TPB constructs of adolescents and parents are displayed in Table 2. Test-re-test reliability of the TPB in adolescents was acceptable with Pearson correlation coefficients ranging from moderate (r=0.39 with perceived behavioral control) to strong (r=0.79 with intention, all p<0.001). As hypothesized, all TPB constructs were significantly correlated with adolescents' intentions. Intention had the strongest relationship with SSB consumption in both adolescents and parents (both p<0.001). In adolescents, subjective norm (p<0.001) had the highest correlation with behavioral intention, while in adults perceived behavioral control had the highest correlation with intention. In both adolescents and parents attitude had the lowest correlation with behavioral intention (adolescents p=0.019; parents p=0.018).
Table 2.
Intercorrelations (r-values) for adolescent (A, N=100) and parent (B, N=65) Theory of Planned Behavior constructs from a Mixed Methods Analysis of Beverage Choices in Adolescents and Parents using the Theory of Planned Behavior.
| A. |
| Variables | 1 Behavior (SSBa kcal) |
2 Intention |
3 Perceived behavioral control |
4 Subjective norm |
5 Attitude |
|---|---|---|---|---|---|
| 1. Behavior (SSB kcal) | --- | −0.36*** | −0.01 | −0.30*** | −0.11 |
| 2. Intention | --- | 0.32*** | 0.52*** | 0.21* | |
| 3. Perceived behavioral control | --- | 0.09 | 0.18* | ||
| 4. Subjective norm | --- | 0.34*** | |||
| 5. Attitude | --- |
| B. |
| Variables | 1 Behavior (SSBa kcal) |
2 Intention |
3 Perceived behavioral control |
4 Subjective norm |
5 Attitude |
|---|---|---|---|---|---|
| 1. Behavior (SSB kcal) | --- | −0.58*** | −0.27* | −0.04 | −0.03 |
| 2. Intention | --- | 0.55*** | 0.25* | 0.21* | |
| 3. Perceived behavioral control | --- | 0.24* | 0.14 | ||
| 4. Subjective norm | --- | 0.106 | |||
| 5. Attitude | --- |
Sugar-sweetened beverage; includes regular soft drinks, juice drinks, sweetened tea, coffee/tea with cream and/or sugar, mixed alcoholic drinks, and energy and sports drinks.30
p<0.05
p≤0.001
Thirty-two percent of the variance in adolescents' (F(3,96)=16.81, p<0.001) and 31% of the variance in parents' (F(3,62)=10.57, p<0.001) intention to limit sugary beverage consumption to less than one cup per day could be accounted for by the TPB's three main constructs (i.e. attitude, subjective norms, and perceived behavioralcontrol). As hypothesized, different TPB constructs emerged as the most predictive of intention to limit SSB to less than one cup per day between adolescents and parents. The strongest and only significant predictor of behavioral intention in parents was perceived behavioral control (b±SE=1.35±0.36, 95% bias corrected and accelerated CI [95% BCa]=0.67, 2.07, p=0.002), while different from what was hypothesized, subjective norm was the strongest predictor in adolescents (b±SE=0.57±0.11, 95% BCa=0.35, 0.72, p=0.001). Also, a significant predictor in adolescents was perceived behavioral control (b±SE=0.39±0.11, 95% BCa=0.18, 0.62, p=0.002).
The multiple linear regression results for TPB constructs with SSB kcal consumption in adolescents and parents are presented in Table 3. The Durbin-Watson test statistics of 2.03 and 1.86 for adolescent and parent models, respectively suggests the assumption of independent errors is met,49 and average variance inflation factors of 1.26 and 1.36 suggests the regression models for adolescents and parents, respectively is not biased.49 Each of the models overallwere statistically significant (Table 3). Parent R2 and adjusted R2 values were higher than those observed for adolescents at all steps of the regression model (Table 3); meaning that more variance in SSB consumption could be accounted for by the TPBin parents versus adolescents. In both adolescents and parents, intention was a significant predictor of SSB consumption, although stronger in parents (Table 3; adolescents: b=−37, p=0.026; parents: b=−49, p≤0.003). For every one-point increase in adolescents' and parents' intention to limit sugary beverages, SSB consumption is predicted to decrease by 37 and 49 kcal, respectively. In adolescents, gender was a significant predictor of intention to limit sugary beverages to less than one cup every day (b=− 49, p=0.033); females consumed 49 kcal less per day of SSB than their male counterparts.
Table 3.
Linear models for predictors of sugar-sweetened beveragea (SSB) consumption from the Theory of Planned Behavior (TPB) constructs in adolescents (panel A) and parents (panel B) with 95% bias corrected and accelerated confidence intervals (95% BCa) and statistically significant interactions from the moderator analysis of the Parent Response to Beverage Choice Questionnaire on adolescent TPB constructs and SSBa intake (panel C). Confidence intervals and standard errors for linear models are based on 1000 bootstrap samples.
| A. Adolescents | |||||
|---|---|---|---|---|---|
| Predictor Variable |
R2
(Adj R2) |
Final Model b (95% BCa) |
Final Model SE B |
Final Model β |
F |
| Step 1 Intention | 0.13 | −37* | 16 | −0.27 | 14.65*** |
| (0.12) | (−70, −7) | ||||
| Step 2 Perceived behavioral control |
0.14 | 16 | 20 | 0.09 | 7.99*** |
| (0.12) | (−24, 57) | ||||
| Step 3 Subjective norms | 0.16 | −15 | 20 | −0.10 | 4.43** |
| (0.12) | (−52, 28) | ||||
| Step 3 Attitude | 0.16 | −3 | 18 | −0.01 | 4.43** |
| (0.12) | (−36, 35) | ||||
| Step 4 Gender | 0.22 | −49* | 22 | −0.22 | 3.77*** |
| (0.16) | (−90, −10) | ||||
| Step 4 Age | 0.22 | 9 | 6 | −.15 | 3.77*** |
| (0.16) | (−4, 21) | ||||
| Step 4 BMI percentile | 0.22 | 0 | 0 | 0.02 | 3.77*** |
| (0.16) | (−1, 1) | ||||
| B. Parents | |||||
| Predictor Variable |
R2
(Adj
R2) |
Final
Model b (95% CI) |
Final Model
SE B |
Final Model
β |
F |
| Step 1 Intention | 0.33 | −49** | 14 | −0.63 | 31.43*** |
| (0.32) | (−75, −17) | ||||
| Step 2 Perceived behavioral control |
0.34 | 17 | 31 | 0.08 | 15.72** |
| (0.32) | (−47, 68) | ||||
| Step 3 Subjective norms | 0.36 | −7 | 12 | 0.06 | 8.25** |
| (0.31) | (−14, 30) | ||||
| Step 3 Attitude | 0.36 | 11 | 10 | 0.10 | 8.25** |
| (0.31) | (−11, 31) | ||||
| Step 4 Gender | 0.38 | −41 | 56 | −0.11 | 5.03*** |
| (0.31) | (−154, 60) | ||||
| Step 4 Age | 0.38 | −1 | 2 | −0.02 | 5.03*** |
| (0.31) | (−6, 7) | ||||
| Step 4 BMIb | 0.38 | 3 | 4 | 0.13 | 5.03*** |
| (0.31) | (−4, 7) | ||||
|
C. Moderation
Analysis |
R2 |
b
(95% CI) |
SE B | F | |
| Main effect: Adolescent intention |
--- | −80** | 16 | ||
| (−112, −48) | |||||
| Main effect: Parent encouragement of SSBa overall |
--- | 17 | 16 | ||
| (−14, 48) | |||||
| Interaction: Parent encouragement of SSBa overall X adolescent intention |
0.34 | −43* | 18 | 10.98** | |
| (−80, −7) | |||||
| Main effect: Adolescent intention |
--- | -81** | 14 | ||
| (−109, −54) | |||||
| Main effect: Parent encouragement of SSBa outside of home |
--- | 26* | 13 | ||
| (−0, 51) | |||||
| Interaction: Parent encouragement of SSBa outside the home X adolescent intention |
0.40 | −55** | 14 | 14.22** | |
| (−83, −28) | |||||
Sugar-sweetened beverages include regular soft drinks, juice drinks, sweetened tea, coffee/tea with cream and/or sugar, mixed alcoholic drinks, and energy and sports drinks.30
Body mass index
p≤0.05
p≤0.01
p≤0.001
Moderator and Mediator Analysis
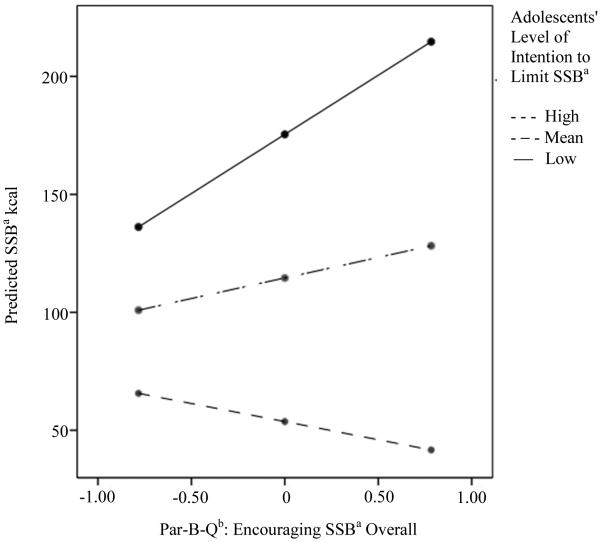
Two adolescent participants discontinued participation in the study after the initial visit and the associated parent data was not included in the moderator or mediator analyses, leaving 64 parent participants with useable responses for the moderator and mediator analyses. Two moderator models were statistically significant (Table 3): the interactions between adolescent intention and parental encouragement of sugary beverage intake 1) overall (b=−43, p=0.02), and 2) outside the home (b=−55, p<0.01). Contrary to hypotheses, no parental response to adolescents' beverage choice in or out of the home had a significant interaction with adolescents' attitude toward SSB.
The conditional effect of parent responses that are suggestive of encouraging adolescents' SSB overall on adolescent SSB consumption at low, average [i.e. mean], and high values of adolescent intention to limit SSB intake (i.e. the simple slopes) is depicted in Figure 2. When parents' responses encouraging SSB are high and adolescents' intention to limit sugary beverages is low, adolescents' predicted SSB kcal intake is highest (i.e. 214 kcal). Similar patterns emerged for beverage consumption outside of the home.
Figure 2.
Simple slopes for conditional effect of parent responses encouraging sugar-sweetened beverage (SSB)a in and out of the home combined (i.e., overall) on predicted SSBa consumption (kcal) at low (−1 standard deviation [SD]), average (i.e., mean), and high values (+1 SD) of adolescents' intention to limit SSBa.
aSugar-sweetened beverages include regular soft drinks, juice drinks, sweetened tea, coffee/tea with cream and/or sugar, mixed alcoholic drinks, and energy and sports drinks.30
bParent Response to Beverage Choice Questionnaire
All indirect effects' confidence intervals contained zero suggesting mediation was not present (data not shown). Thus, further analyses were ceased.
Parent Response to Adolescents' Beverage Choices
No significant differences were observed when examining BMI category and means responses on the Par-B-Q. The means and SEs for encouraging and discouraging SSB and non-SSB in and out of the home and overall are depicted in Table 4. Overall parents did significantly more discouraging of SSB and encouraging of non-SSB, as apposed to encouraging SSB and discouraging non-SSB (both p≤0.01). When considering environment, parents' responses suggest they did more encouragingof non-SSB (M=2.95) versus discouraging of SSB (M=2.49) out of the home (t(65)=−2.69, p=0.009). However, at home parents' reactions are more discouraging of SSB (M=3.17) compared to encouraging non-SSB (M=2.95; t(65)=3.69, p<0.001).
Table 4.
Means and standard errors of parent response to beverage choice questionnaire (Par-B-Q) subscales for sugar-sweetened beveragesa (A) and non-sugar-sweetened beverages (B) in and out of the home.
| A. Par-B-Q Subscale for Sugar-sweetened Beverages | M b | SE |
| At Home | ||
| Encouraging intake | 2.26 | 0.09 |
| Discouraging intake | 3.17 | 0.13 |
| Out of Home | ||
| Encouraging intake | 2.62 | 0.10 |
| Discouraging intake | 2.49 | 0.13 |
| Overall encouraging intake | 2.58 | 0.10 |
| Overall discouraging intake | 3.19 | 0.13 |
| B. Par-B-Q Subscale for Non-Sugar-sweetened Beverages | M | SE |
| At Home | ||
| Encouraging intake | 2.53 | 0.11 |
| Discouraging intake | 2.40 | 0.12 |
| Out of Home | ||
| Encouraging intake | 2.95 | 0.10 |
| Discouraging intake | 2.06 | 0.13 |
| Overall encouraging intake | 2.95 | 0.10 |
| Overall discouraging intake | 2.39 | 0.15 |
Sugar-sweetened beverages include regular soft drinks, juice drinks, sweetened tea, coffee/tea with cream and/or sugar, mixed alcoholic drinks, and energy and sports drinks.30
Responses to the Par-B-Q are scaled from "1"= very unlikely to "7"=very likely.
Qualitative Results
Sixty-five percent of parents (n=42) stated they speak with their child "sometimes," ~32% (n=21) stated "often," and ~3% (n=2) "never" speak totheir child about beverage choices. One major and one minor theme emerged from parent responses to why they spoke with their child about beverage choices: they believed "health was impacted by choices" (55% of responses), and they wanted to "have a positive influence on beverage choices" (35% of responses). Parents thought it was important to speak with children about "how choices can impact their [i.e. the child's] health" (45% of responses), "how sugary drinks are not good/too much sugar is not good" (38% of responses), to "encourage water/water is important for health" (34% of responses), and "moderation" (28% of responses). Beverages parents permitted their child to drink or purchase included water (71% of responses), 100% fruit juice (63% of responses), soda on special occasions (58% ofresponses), milk (48% of responses), sports drinks (including low-calorie sports drinks, 31% of responses), and sweet tea/lemonade (26% of responses). Beverages that parents do not like their child to drink or purchase included energy drinks (62% of responses), soda (46% of responses), coffee (32% of responses), caffeinated drinks (29% of responses), SSB/sweet tea (28% of responses), and artificially sweetened drinks/diet soda (25% of responses).
Discussion
The present investigation found the TPB to be an effective means to understand and predict adolescent and parent SSB consumption. Subjective norm in adolescents and perceptions of control in parents were the strongest predictors of intention to limit SSB, and intention was the strongest predictor of adolescents' and parents' SSB consumption. Results from the moderation analysis revealed that at lower levels of adolescent's intention to limit SSB and higher levels of parents' encouragement of SSB, adolescents' predicted SSB intake was highest, suggesting that some adolescents are influenced by their parents when making decisions to drink SSB.
Adolescent and Parent Beverage Intake
Male and female adolescents drank less than established upper limits for SSB52,53and this is consistent with recent research indicating that youth's SSB consumption has been declining.12 Parents' SSB consumption exceeded recommendations of less than eight ounces per day;53 however, their level was less than that recently reported.12 This sample reported a high income and education attainment which may also contribute to these findings versus that of others. Continuing to target reducing SSB intake and increasing water consumption, as emphasized in the Scientific Report of the 2015 Dietary Guidelines Advisory Committee,9 may promote weight management and optimal health and well-being in youth and adults.
Effectiveness of the Theory of Planned Behavior in Adolescents and Parents
Research supports the usefulness of the TPB in the prediction of intention and behavior for a wide variety of health behaviors.24-26 and the present results are similar to one studyassessing soft drink consumption in adolescents.54 In the present sample, the TPB explained a significant amount of variance in adolescents' and parents' SSB consumption; however, a majority of the variance remains unexplained. Adolescents' health behaviors may include two processes (i.e.“heuristic” and evaluative) and a theoretical model incorporating both operations may be more effective in predicting adolescents' health behaviors versus a traditional expectancy-value model, such as the TPB.55 Adding behavioral willingness to the TPB model may help to better understand adolescents SSB consumption.55 Future research attempting to understand adolescents' SSB consumption can include incorporating this “dual-processing perspective,”55 which may provide further reasoning as to why adolescents choose specific beverages over others.
The explained variance in behavioral intention is comparable between adolescents and parentsas seen in prior work.26 Intentions can change over time; thus, the closer intention is measured to behavioral action, the more likely it can predict behavior.56 Adolescents' andparents' behavioral intention was the strongest predictor of SSB consumption, and this may be because SSB intake (i.e. behavior) was measured at the same time as intention. Previous works show similarpatterns in adults24-26 and adolescents.26 As age increases processing of stimuli changes from being emotional-based to more rational/evaluative57 and adolescents’ may be in the midst of this transition. Perceived behavioral control in parents and subjective norm in adolescents having the strongest association with behavioral intention may further support this idea. Adolescents' affect might be more heavily influenced by peers and social acceptance,and the persona they portray may be important to them during this life stage, which can then influence beverage choices and ultimately health. Forthcoming work can elicit the normative beliefs and motivation to comply with important social factors influencing adolescents' SSB consumption and then incorporate these revelations into an intervention possibly delivered by the important social influencers.
Disinhibition, the loss of control when consuming foods that are typically considered "off-limits",58 is associated with increased energy intake,59 weight gain in those with depression,60 and dietary helplessness.58 Furthermore, disinhibition has been observed to be the strongest factor distinguishing between obese and non-obese women.59 Thus, obese parents having less perceptions of control versus normal weight parents might represent their beliefs that dietary behaviors, specifically SSB intake, are immutable; they can hold an entity theory.61 That is, their lack of control around SSB intake may be viewed as being unchangeable; some may believe they are predetermined to drink such beverages in excess. Lay theories (i.e. theories that posit the changeability of personal characteristics) have been investigated in dieters and understanding which lay theory individuals' hold (e.g. incremental or entity) might facilitate weight loss and setting sustaining and achievable weight management goals.61,62 Taking the present results into account, distinguishing between entity and incremental theorists61 in future work can provide further direction for creating strategies to decrease excessive SSB consumption in parents. This approach may impact adolescents since parents, who hold specific beliefs about self-control, sometimes unintentionally project their beliefs onto their children.63 This in turn could influence beverage choices.
Moderation Analysis and Parent Responses to Adolescents' Beverage Choices
The moderation analysis suggests that when adolescents' intentions to limit SSB are low or moderate, parents' encouragement to consume SSB matters (and is associated with increased SSB consumption by adolescents), but when adolescents' intentions to limit SSB are high, parents' encouragement may not affect adolescents' SSB intake. Some teens may have the autonomy typically sought during this developmental stage of life2 and this may be the reason for the difference observed inpredicted SSB consumption at high levels of intention versus low levels of intention. Subsequent work can evaluate adolescents' perception and level of autonomy and how this may influence SSB consumption.
Considering over 95% of parents spoke to their child about beverage choices indicatesthat, like previous work, parents may influence some adolescents' SSB intake.64,65 However, parents reported drinking more than the recommended upper limits of SSB indicating that availability is an area for attention. It has been suggested that positive modeling may be the best approach to promote healthy diet choices in youth.66 An intervention might target parents of low intention teens to encourage non-SSB intake and reduce SSB availability. On the other hand, some teens that hold greater intentions to limit SSB might have influences beyond parents. Peers have been shown to influence children's soft drink intake67 and future work can investigate how much of an impact adolescents' peer network, older family members, those in authority (e.g. religious leaders, captains on sports teams, and coaches), and other role models have on SSB intake using the TPB.
The Par-B-Q qualitative results suggest that parents may be aware of the health benefits of water consumption68,69 and seek to have a positive influence on their child's health through beverage choices. This may be further exemplified by energy drinks being the most frequently identified beverage parents do not like their child to drink or purchase. Understanding how adolescents' perceive their parents' parenting practices around beverage choices might lend more insight into how this pressure influences adolescents' decision processes in relation to SSB intake.
Strengths and Limitations
Despite the varied age distribution, and high retention rate of the current investigation, some limitations are acknowledged. First, the cross-sectional design does not permit casual relationships. Second, in adolescents there is not one method of diet evaluation that is considered superior to another,33 and obtaining accurate dietary intake data can be challenging due to youth's day-to-day variability in food intake, poor ability to estimate portion sizes, and decreased recall ability.33,37 However, the present analysis used four record-assisted 24HR, a dietary assessment method suggested to better estimate food intake at the individual level in adolescents70 and provide satisfactory nutrient and food data representative of regular consumption patterns.34,35 Third, the sample of adolescents and parents were from the Blacksburg, VA area; thus, results may not generalize to others of different regions or socioeconomic status. Approximately 15% and 12% of VA's adolescents are considered overweight and obese respectively,and our sample having 7% of participants being identified as obese is below the state average.71 Fourth, Cronbach αs for some Par-B-Q constructs measuring parent responses encouraging SSB and non-SSB consumption in and out of the home were low; responses from the questionnaire, and thus, the moderation analysis should be considered in light of this limitation as the questionnaire may need modifications to better evaluate parents' reactions to their child's beverage choices. Fifth, Ajzen highlights the importance of conducting formative research when developing a TPB questionnaire72 and this sample of adolescents may hold different salient beliefs than those identified for development of the administered TPB tool.31
Practice Implications
The current findings add to the literature on parent and adolescent SSB intake and provide potential guidance on how registered dietitians/nutritionists and other health professionals can strategize nutrition therapy provided to parents and adolescents related to beverage intake. A Behavioral Family Systems therapy approach73 and including motivational interviewing techniques74,75 and problem solving skill training74 can be used with parents who lack perceptions of control and adolescents who lack intentions to limit SSB. These techniques and approaches might facilitate self-led changes in parent’s and adolescent’s beverage choices directly and indirectly. Registered dietitians/nutritionists and other health professionalscan highlight alternative beverage choices and help parent clients feel more empowered to change unhealthy beverage choices through decreasing SSB availability, which can potentially be transmitted tochildren with the hopes of increasing teen’s intentions around SSBs and improving health outcomes and quality of life.
Conclusions
In summary, the TPB explains a significant amount of variance in adolescents' SSB consumption and intention to limit SSB. Contrary to hypotheses, subjective norm was the strongest predictor ofadolescents' intention to limit SSB while, as hypothesized, intention was the strongest predictor ofSSB consumption. No TPB constructs mediated the relationship between parent responses to adolescents' beverage choices and adolescent SSB consumption. However, the moderator analysis suggests that adolescents with low intentions to limit SSB have the highest SSB consumption when parent responses areencouraging of SSB. In addition to parents, social figures such as older role models in the community, on sports teams, within the family, and in classrooms, can be targeted in future investigations attempting to limit adolescents' SSB intake. Together, parents and other social influences can directly deliver interventions promoting decreased SSB consumption using motivational strategies to promote consumption of healthy beverage options in adolescents.
Supplementary Material
Acknowledgements
The authors would like to thank all subjects and parents who participated in this study. We also specifically acknowledge the valuable assistance of Valisa Hedrick, PhD, RD, and Andrew Hayes, PhD, who provided insight for statistical analyses with this study.
Funding Disclosure: This work was in part funded by the National Institute of Health grant R21HD078636-01A1 and Graduate Assistant support from (Institution's name blinded) Interdisciplinary Graduate Education Program.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosure
No authors of the manuscript titled "A mixed methods analysis of beverage choices in adolescents and their parents using the Theory of Planned Behavior" report a conflict of interest.
Contributor Information
Carly MacDougall, Email: carlym@vt.edu.
Catelyn Hill, Email: cate93@vt.edu.
Paul A Estabrooks, Email: estabrkp@vt.edu.
Julie C Dunsmore, Email: jdunsmor@vt.edu.
Jyoti Savla, Email: jsavla@vt.edu.
Madlyn I Frisard, Email: frisardm@vt.edu.
Andrea M Dietrich, Email: andread@vt.edu.
Brenda M Davy, Email: bdavy@vt.edu.
References
- 1.Berk LE. Development through the lifespan. Allyn and Bacon; Boston, MA: 2007. [Google Scholar]
- 2.Truswell AS, Darnton-Hill I. Food habits of adolescents. Nutr Rev. 1981 Feb;39(2):73–88. doi: 10.1111/j.1753-4887.1981.tb06736.x. [DOI] [PubMed] [Google Scholar]
- 3.Bull NL. Dietary habits, food consumption, and nutrient intake during adolescence. J Adolesc Health. 1992 Jul;13(5):384–388. doi: 10.1016/1054-139x(92)90034-9. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012 Feb 1;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sinaiko AR, Donahue RP, Jacobs JDR, Prineas RJ. Relation of weight and rate of increase in weight during childhood and adolescence to body size, blood pressure, fasting insulin, and lipids in young adults. The Minneapolis Children's Blood Pressure Study. Circulation. 1999;99(11):1471–1476. doi: 10.1161/01.cir.99.11.1471. [DOI] [PubMed] [Google Scholar]
- 6.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013 Oct;98(4):1084–1102. doi: 10.3945/ajcn.113.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United States Department of Agriculture and United States Department of Health and Human Services . Dietary Guidelines for Americans. 7th. U.S. Government Printing Office; Washington, DC: 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ervin RB, Kit BK, Carroll MD, Ogden CL. Consumption of Added Sugar among US Children and Adolescents, 2005-2008. National Center for Health Statistics. 2012 Mar; doi: 10.3945/an.112.002279. NCHS Data Brief. No. 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.United States Department of Agriculture and United States Department of Health and Human Services Scientific Report of the 2015 Dietary Guidelines Advisory Committee. 2015 http://www.health.gov/dietaryguidelines/2015-scientific-report/. Updated March 11, 2015. Accessed March 11, 2015.
- 10.Wang J, Light K, Henderson M, et al. Consumption of added sugars from liquid but not solid sources predicts impaired glucose homeostasis and insulin resistance among youth at risk of obesity. J Nutr. 2014 Jan;144(1):81–86. doi: 10.3945/jn.113.182519. [DOI] [PubMed] [Google Scholar]
- 11.Ambrosini GL, Oddy WH, Huang RC, Mori TA, Beilin LJ, Jebb SA. Prospective associations between sugar-sweetened beverage intakes and cardiometabolic risk factors in adolescents. Am J Clin Nutr. 2013 Aug;98(2):327–334. doi: 10.3945/ajcn.112.051383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999-2010. Am J Clin Nutr. 2013;98(1):180–188. doi: 10.3945/ajcn.112.057943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010 Feb 2;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 14.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988-2004. Pediatrics. 2008 Jun;121(6):e1604–1614. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 15.Beck AL, Patel A, Madsen K. Trends in sugar-sweetened beverage and 100% fruit juice consumption among California children. Acad Pediatr. 2013 Jul-Aug;13(4):364–370. doi: 10.1016/j.acap.2013.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Field AE, Sonneville KR, Falbe J, et al. Association of sports drinks with weight gain among adolescents and young adults. Obesity. 2014;22(10):2238–2243. doi: 10.1002/oby.20845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Academy of Pediatrics: Committee on Nutrition and the Council on Sports Medicine Fitness Sports Drinks and Energy Drinks for Children and Adolescents: Are They Appropriate? Pediatrics. 2011 Jun 1;127(6):1182–1189. doi: 10.1542/peds.2011-0965. [DOI] [PubMed] [Google Scholar]
- 18.Rhee K. Childhood Overweight and the Relationship between Parent Behaviors, Parenting Style, and Family Functioning. Ann Am Acad Pol Soc Sci. 2008;615:12–37. [Google Scholar]
- 19.Couch SC, Glanz K, Zhou C, Sallis JF, Saelens BE. Home food environment in relation to children's diet quality and weight status. J Acad Nutr Diet. 2014;114(10):1569–1579. doi: 10.1016/j.jand.2014.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: conception to adolescence. J Law Med Ethics. 2007;35(1):22–34. doi: 10.1111/j.1748-720X.2007.00111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Watts AW, Mâsse LC, Barr SI, Lovato CY, Hanning RM. Parent-child associations in selected food group and nutrient intakes among overweight and obese adolescents. J Acad Nutr Diet. 2014;114(10):1580–1586. doi: 10.1016/j.jand.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 22.Painter JE, Borba CP, Hynes M, Mays D, Glanz K. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med. 2008 Jun;35(3):358–362. doi: 10.1007/s12160-008-9042-y. [DOI] [PubMed] [Google Scholar]
- 23.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991 Dec;50(2):179–211. [Google Scholar]
- 24.Armitage CJ, Conner M. Efficacy of the Theory of Planned Behaviour: A meta-analytic review. Br J Soc Psychol. 2001 Dec;40(4):471. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 25.Godin G, Kok G. The theory of planned behavior: a review of its applications to health-related behaviors. Am J Health Promot. 1996 Nov-Dec;11(2):87–98. doi: 10.4278/0890-1171-11.2.87. [DOI] [PubMed] [Google Scholar]
- 26.McEachan RRC, Conner M, Taylor NJ, Lawton RJ. Prospective prediction of health-related behaviours with the theory of planned behaviour: A meta-analysis. Health Psychol Rev. 2011;5(2):97–144. [Google Scholar]
- 27.Riebl SK, Estabrooks PA, Dunsmore JC, et al. A systematic literature review and meta-analysis: The Theory of Planned Behavior's application to understand and predict nutrition-related behaviors in youth. Eat Behav. 2015 Jun 16;18:160–178. doi: 10.1016/j.eatbeh.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 28.Willett W. Nutritional Epidemiology. 3rd Oxford University Press; New York: 2013. [Google Scholar]
- 29.Centers for Disease Control and Prevention/National Center for Health Statistics National Health and Nutrition Examination Survey (NHANES) MEC In-Person Dietary Interviewers Procedures Manual. January 2008; http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_dietarymec.pdf. Updated April 6, 2012. Accessed June 11, 2013.
- 30.Hedrick VE, Savla J, Comber DL, et al. Development of a Brief Questionnaire to Assess Habitual Beverage Intake (BEVQ-15): Sugar-Sweetened Beverages and Total Beverage Energy Intake. J Acad Nutr Diet. 2012;112(6):840–849. doi: 10.1016/j.jand.2012.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zoellner J, Estabrooks PA, Davy BM, Chen YC, You W. Exploring the Theory of Planned Behavior to Explain Sugar-sweetened Beverage Consumption. J Nutr Educ Behav. 2011 Dec 7;44(2):172–177. doi: 10.1016/j.jneb.2011.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baylor College of Medicine -USDA/ARS Children's Nutrition Research Center Age-based Pediatric Growth Reference Charts. 2015 https://www.bcm.edu/bodycomplab/Flashapps/bmiVAgeChartpage.html (Archived by WebCite® at http://www.webcitation.org/6VbSTezHj). Accessed January 15, 2015.
- 33.Thompson FE, Subar AF. Nutrition in the Prevention and Treatment of Disease. Third Academic Press; 2013. Chapter 1 - Dietary Assessment Methodology; pp. 5–46. [Google Scholar]
- 34.Carroll RJ, Midthune D, Subar AF, et al. Taking advantage of the strengths of 2 different dietary assessment instruments to improve intake estimates for nutritional epidemiology. Am J Epidemiol. 2012 Feb 15;175(4):340–347. doi: 10.1093/aje/kwr317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Trolle E, Amiano P, Ege M, et al. Evaluation of 2 × 24-h dietary recalls combined with a food-recording booklet, against a 7-day food-record method among schoolchildren. Eur J Clin Nutr. 2011 Jul;65(Suppl 1):S77–83. doi: 10.1038/ejcn.2011.90. [DOI] [PubMed] [Google Scholar]
- 36.Blanton C, Moshfegh A, Baer D, Kretsch M. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. The Journal of nutrition. 2006;136(10):2594–2599. doi: 10.1093/jn/136.10.2594. [DOI] [PubMed] [Google Scholar]
- 37.Lytle LA, Nichaman MZ, Obarzanek E, et al. Validation of 24-hour recalls assisted by food records in third-grade children. The CATCH Collaborative Group. J Am Diet Assoc. 1993 Dec;93(12):1431–1436. doi: 10.1016/0002-8223(93)92247-u. [DOI] [PubMed] [Google Scholar]
- 38.Hedrick VE, Comber DL, Ferguson KE, et al. A rapid beverage intake questionnaire can detect changes in beverage intake. Eat Behav. 2013 Jan;14(1):90–94. doi: 10.1016/j.eatbeh.2012.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. [Google Scholar]
- 40.Sijtsma K. On the use, the misuse, and the very limited usefulness of Cronbach's alpha. Psychometrika. 2009;74(1):107–120. doi: 10.1007/s11336-008-9101-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nunnally JC. Psychometric theory. McGraw-Hill; New York: 1967. [Google Scholar]
- 42.Kline P. The handbook of psychological testing. Routledge; New York; London: 1993. [Google Scholar]
- 43.Fabes RA, Poulin RE, Eisenberg N, Madden-Derdich DA. The Coping with Children’s Negative Emotions Scale (CCNES): Psychometric Properties and Relations with Children’s Emotional Competence. Marriage Fam Rev. 2002 Jun;34(3-4):285–310. [Google Scholar]
- 44.Field AE. Discovering Statistics Using IBM SPSS Statistics. 4th Sage; Thousand Oaks, California: 2013. Exploring Factor Analysis; pp. 665–719. [Google Scholar]
- 45.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 46.Bogdan R, Biklen SK. Qualitative research for education: an introduction to theory and methods. 5th Pearson/Allyn and Bacon; Needham Heights, MA: 2007. [Google Scholar]
- 47.Hankins M, French D, Horne R. Statistical guidelines for studies of the theory of reasoned action and the theory of planned behaviour. Psychol Health. 2000;15(2):151. [Google Scholar]
- 48.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. http://www.afhayes.com/introduction-to-mediation-moderation-and-conditional-process-analysis.html. Accessed January 31, 2015.
- 49.Field AE. Discovering Statistics Using IBM SPSS Statistics. 4th Sage; Thousand Oaks, California: 2013. Moderation, Mediation and More Regression; pp. 392–428. [Google Scholar]
- 50.McClain AD, Chappuis C, Nguyen-Rodriguez ST, Yaroch AL, Spruijt-Metz D. Psychosocial correlates of eating behavior in children and adolescents: a review. Int J Behav Nutr Phys Act. 2009;6:54. doi: 10.1186/1479-5868-6-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008 Aug;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 52.Pinard CA, Davy BM, Estabrooks PA. Beverage intake in low-income parent-child dyads. Eat Behav. 2011 Dec;12(4):313–316. doi: 10.1016/j.eatbeh.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 53.Popkin BM, Armstrong LE, Bray GM, Caballero B, Frei B, Willett WC. A new proposed guidance system for beverage consumption in the United States. Am J Clin Nutr. 2006 Mar;83(3):529–542. doi: 10.1093/ajcn.83.3.529. [DOI] [PubMed] [Google Scholar]
- 54.de Bruijn GJ, Kremers SP, de Vries H, van Mechelen W, Brug J. Associations of social-environmental and individual-level factors with adolescent soft drink consumption: results from the SMILE study. Health Educ Res. 2007 Apr;22(2):227–237. doi: 10.1093/her/cyl066. [DOI] [PubMed] [Google Scholar]
- 55.Gibbons FX, Houlihan AE, Gerrard M. Reason and reaction: the utility of a dual-focus, dual-processing perspective on promotion and prevention of adolescent health risk behaviour. Br J Health Psychol. 2009 May;14(Pt 2):231–248. doi: 10.1348/135910708X376640. [DOI] [PubMed] [Google Scholar]
- 56.Ajzen I. From Intentions to Actions: A Theory of Planned Behavior. In: Kuhl J, Beckmann J, editors. Action Control. Springer Berlin Heidelberg; 1985. pp. 11–39. [Google Scholar]
- 57.Killgore WD, Yurgelun-Todd DA. Developmental changes in the functional brain responses of adolescents to images of high and low-calorie foods. Dev Psychobiol. 2005 Dec;47(4):377–397. doi: 10.1002/dev.20099. [DOI] [PubMed] [Google Scholar]
- 58.Carmody TP, Brunner RL, St Jeor ST. Dietary helplessness and disinhibition in weight cyclers and maintainers. Int J Eat Disord. 1995;18(3):247–256. doi: 10.1002/1098-108x(199511)18:3<247::aid-eat2260180306>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 59.Lindroos AK, Lissner L, Mathiassen ME, et al. Dietary intake in relation to restrained eating, disinhibition, and hunger in obese and nonobese Swedish women. Obes Res. 1997;5(3):175–182. doi: 10.1002/j.1550-8528.1997.tb00290.x. [DOI] [PubMed] [Google Scholar]
- 60.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 61.Beruchashvili M, Moisio R, Heisley DD. What are you dieting for? The role of lay theories in dieters' goal setting. Journal of Consumer Behaviour. 2014;13(1):50–59. [Google Scholar]
- 62.Burnette JL, Finkel EJ. Buffering against weight gain following dieting setbacks: An implicit theory intervention. J Exp Soc Psychol. 2012;48(3):721–725. [Google Scholar]
- 63.Mukhopadhyay A, Yeung CWM. Building character: effects of lay theories of self-control on the selection of products for children. Journal of Marketing Research. 2010;47(2):240–250. [Google Scholar]
- 64.Bere E, Sørli Glomnes E, te Velde SJ, Klepp K-I. Determinants of adolescents’ soft drink consumption. Public Health Nutr. 2008;11(01):49–56. doi: 10.1017/S1368980007000122. [DOI] [PubMed] [Google Scholar]
- 65.Campbell KJ, Crawford DA, Salmon J, Carver A, Garnett SP, Baur LA. Associations Between the Home Food Environment and Obesity-promoting Eating Behaviors in Adolescence. Obesity. 2007;15(3):719–730. doi: 10.1038/oby.2007.553. [DOI] [PubMed] [Google Scholar]
- 66.Scaglioni S, Salvioni M, Galimberti C. Influence of parental attitudes in the development of children eating behaviour. Br J Nutr. 2008 Feb;99(Suppl 1):S22–25. doi: 10.1017/S0007114508892471. [DOI] [PubMed] [Google Scholar]
- 67.Grimm GC, Harnack L, Story M. Factors associated with soft drink consumption in school-aged children. J Am Diet Assoc. 2004;104(8):1244–1249. doi: 10.1016/j.jada.2004.05.206. [DOI] [PubMed] [Google Scholar]
- 68.Dennis EA, Dengo AL, Comber DL, et al. Water consumption increases weight loss during a hypocaloric diet intervention in middle-aged and older adults. Obesity (Silver Spring) 2010 Feb;18(2):300–307. doi: 10.1038/oby.2009.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Muckelbauer R, Sarganas G, Gruneis A, Muller-Nordhorn J. Association between water consumption and body weight outcomes: a systematic review. Am J Clin Nutr. 2013 Aug;98(2):282–299. doi: 10.3945/ajcn.112.055061. [DOI] [PubMed] [Google Scholar]
- 70.Livingstone MB, Robson PJ, Wallace JM. Issues in dietary intake assessment of children and adolescents. Br J Nutr. 2004 Oct;92(Suppl 2):S213–222. doi: 10.1079/bjn20041169. [DOI] [PubMed] [Google Scholar]
- 71.U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (CDC), National Center for Chronic Disease Prevention and Health Promotion, Division of Nutrition, Physical Activity and Obesity. Nutrition, Physical Activity, and Obesity Data, Trends and Maps web site. 2015 http://www.cdc.gov/nccdphp/DNPAO/index.html. Accessed March 30, 2015.
- 72.Ajzen I. Constructing a Theory of Planned Behavior Questionnaire. 2006 http://people.umass.edu/aizen/pdf/tpb.measurement.pdf. Accessed November 30, 2013.
- 73.Wysocki T, Harris MA, Buckloh LM, et al. Randomized, controlled trial of Behavioral Family Systems Therapy for Diabetes: maintenance and generalization of effects on parent-adolescent communication. Behav Ther. 2008 Mar;39(1):33–46. doi: 10.1016/j.beth.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 74.Seid M, D'Amico EJ, Varni JW, et al. The in vivo adherence intervention for at risk adolescents with asthma: report of a randomized pilot trial. J Pediatr Psychol. 2012 May;37(4):390–403. doi: 10.1093/jpepsy/jsr107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.D'Amico EJ, Fromme K. Brief prevention for adolescent risk-taking behavior. Addiction. 2002 May;97(5):563–574. doi: 10.1046/j.1360-0443.2002.00115.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.