This review revisits epidermal growth factor receptor (EGFR) inhibition as treatment for squamous non-small cell lung cancer. EGFR remains a valid therapeutic target in unselected/EGFR wild-type squamous cell carcinoma of the lung.
Keywords: Squamous, Non-small cell lung cancer, Epidermal growth factor receptor, Small molecule, Monoclonal antibodies, Meta-analysis
Abstract
Molecular therapies targeting epidermal growth factor receptor (EGFR) have had a profound impact on the management of advanced non-small cell lung cancer (NSCLC). EGFR inhibition with EGFR tyrosine kinase inhibitors (EGFR-TKIs) and anti-EGFR monoclonal antibodies (mAbs) in squamous NSCLC (sqNSCLC) remains controversial in patients whose tumors are not known to harbor EGFR mutations. Recent meta-analyses of EGFR-inhibition randomized trials that are adequately powered for histological subgroup analysis and anti-EGFR trials limited to patients with squamous histology afford the opportunity to revisit EGFR treatment in sqNSCLC. In unselected patients with sqNSCLC who are not eligible for chemotherapy, EGFR-TKI therapy is a valid treatment option over placebo or best supportive care, with improved progression-free survival noted in randomized controlled trials in both the first- and second-line setting and improved overall survival (OS) in the second-line setting. In patients eligible for chemotherapy, first-line combination regimens with anti-EGFR mAbs have been shown to improve OS over chemotherapy alone in patients with squamous histology in meta-analysis and more recently in the SQUIRE sqNSCLC trial (chemotherapy with and without necitumumab). In sqNSCLC patients who respond to induction chemotherapy, maintenance therapy with erlotinib delays disease progression and may improve the survival of patients with stable disease. In the second-line setting, survival outcomes are comparable between chemotherapy and EGFR-TKIs in meta-analysis, with the latter being more tolerable as a second-line therapy. Newer-generation EGFR-TKI therapies may further benefit patients with sqNSCLC who have failed first-line chemotherapy, given the positive trial results from LUX-Lung 8 (afatinib vs. erlotinib). EGFR is a valid therapeutic target in unselected/EGFR wild-type patients with squamous cell carcinoma of the lung. With the recent approval of immune checkpoint inhibitors in the second-line management of advanced sqNSCLC and their adoption as a new standard of care, there exists an opportunity for novel combination therapies to increase therapeutic efficacy and durable tumor control. As more targeted agents are approved, combination regimens that include an anti-EGFR agent should be evaluated, and the optimal sequencing of targeted therapies should be defined.
Implications for Practice:
Anti-epidermal growth factor receptor (EGFR) therapies remain controversial in unselected/wild-type EGFR squamous non-small cell lung cancer (NSCLC). Recent meta-analyses and squamous-only NSCLC EGFR-inhibition trials have overcome the power limitations of early trials and can now inform the management of squamous NSCLC with anti-EGFR therapies. With the approval of immunotherapeutics in the second-line management of squamous NSCLC, there exists an opportunity for novel combination therapies to improve efficacy and durable tumor control. The optimal timing and sequencing of available second-line targeted therapies, however, have yet to be defined. This review analyzes randomized clinical trials of EGFR inhibition in NSCLC and meta-analyses of these trials, with a focus on patients with squamous histology.
Abstract
摘要
针对表皮生长因子受体 (EGFR) 的分子疗法已对进展期非小细胞肺癌 (NSCLC) 的治疗产生了深远的影响。有关使用 EGFR 酪氨酸激酶抑制剂 (EGFR-TKI) 和抗 EGFR 单克隆抗体 (mAb) 抑制 EGFR 在鳞状细胞 NSCLC (sqNSCLC) 中的应用, 在未知肿瘤是否 EGFR 突变的患者中仍然存有争议。近期一项 meta 分析纳入了具有足够统计学效能进行组织学亚组分析的抑制 EGFR 治疗的随机临床试验, 此外, 还要求纳入患者组织学为鳞癌, 并且能够充分地再次回顾 sqNSCLC 中的 EGFR 治疗。在未经选择的不适合接受化疗的 sqNSCLC 患者中, EGFR-TKI 治疗是一种优于安慰剂及最佳支持治疗的有效治疗选择。在随机临床试验中, EGFR-TKI一线和二线治疗改善了无进展生存, 并且在二线治疗中改善了总生存 (OS)。在符合化疗标准的患者中, meta 分析和近期的 SQUIRE sqNSCLC 研究 (化疗± necitumumab) 均显示, 与单用化疗相比, 化疗联合抗 EGFR mAb 方案作为一线治疗改善了 OS。在对诱导化疗有治疗反应的 sqNSCLC 患者中, 使用厄洛替尼维持治疗推迟了疾病进展, 并且可能改善疾病稳定患者的生存。在二线治疗中, meta 分析显示化疗与 EGFR-TKI 治疗的生存转归相似, 而 EGFR-TKI 二线治疗的耐受性更好一些。鉴于 LUX-Lung 8 研究 (阿法替尼vs.厄洛替尼) 获得了阳性结果, 新一代 EGFR-TKI 疗法可能进一步为一线化疗失败的 sqNSCLC 患者带来获益。EGFR 是未经选择/EGFR 野生型肺鳞癌患者的有效靶向治疗方案。近期免疫检查点抑制剂获批用于二线治疗进展期 sqNSCLC 并且已作为新的标准治疗, 新的联合疗法有望提高治疗有效性和改善持续肿瘤控制。由于更多的靶向药物获得批准, 有必要对包含一个抗 EGFR 药物的联合方案进行评价, 同时也应确定最佳的靶向治疗顺序。The Oncologist 2016;21:205–213
对临床实践的提示: 抗表皮生长因子受体 (EGFR) 治疗在未经选择/野生型 EGFR 鳞状细胞非小细胞肺癌 (NSCLC) 患者中仍然存有争议。近期的 meta 分析和仅纳入鳞状细胞 NSCLC 的 EGFR 抑制剂研究中, 已克服了早期临床试验的检验效能局限性, 已能够为抗 EGFR 疗法在鳞状细胞 NSCLC 中的使用提供有力证据。随着免疫疗法在鳞状细胞 NSCLC 二线治疗中的获批, 新的联合方案有望改善有效性和肿瘤持续控制。但现有二线靶向疗法的最佳使用时机和治疗顺序仍然有待明确。本综述针对组织学为鳞癌的患者, 分析了在 NSCLC 中开展的 EGFR 抑制剂随机临床试验和针对这些临床试验的 meta 分析。
Introduction
Lung cancer is the leading cause of cancer-related deaths worldwide [1]. Non-small cell lung cancer (NSCLC) represents 85% of all lung cancers, of which 20%–30% are squamous cell carcinoma [2]. Up to two thirds of patients with NSCLC present with locally advanced or advanced disease that is not amenable to surgery and, if left untreated, has a median survival of 7 months [3]. In patients with advanced stage IIIb/IV NSCLC, chemotherapy has been shown to improve survival to beyond a year in select patients [4]. Although historically NSCLC has been treated uniformly as one disease, recent data suggest that NSCLC histology plays an important role in determining toxicity profiles and treatment responses in the advanced disease setting [5–7]. For example, the vascular endothelial growth factor (VEGF) inhibitor bevacizumab, which when combined with chemotherapy in advanced NSCLC has been shown to delay disease progression [4], is contraindicated in patients with squamous histology because of the increased risk of pulmonary hemorrhage [5]. In addition, despite pemetrexed being an established therapy in advanced NSCLC as monotherapy [8, 9] and in combination with chemotherapy [6], it is not approved in patients with squamous histology because of inferior efficacy [7].
As a result of the above therapeutic limitations, standard chemotherapy regimens for squamous NSCLC (sqNSCLC) consist of a platinum agent and gemcitabine, paclitaxel, or vinorelbine as first-line therapy and docetaxel in the second-line setting [10]. Given the limited efficacy of conventional chemotherapies, however, therapeutic alternatives in squamous cell carcinoma of the lung have been investigated, including agents targeting epidermal growth factor receptor (EGFR). Also known as ErbB1, EGFR is overexpressed in 85% of NSCLC, most commonly in patients with squamous histology [11, 12]. Together with other members of the ErbB family (ErbB2, ErbB3, and ErbB4), EGFR plays an important role in cellular proliferation of NSCLC, and EGFR protein overexpression is associated with poor prognosis [13]. Blockade of EGFR activity has been investigated as a therapeutic strategy in NSCLC using both small molecule EGFR tyrosine kinase inhibitors (EGFR-TKIs) and anti-EGFR monoclonal antibodies (mAbs). Both classes of drugs have been shown to decrease signal transduction of the EGFR pathway, albeit through different mechanisms of action [11, 14, 15]. Mutations that activate the EGFR signaling pathway, namely the L858R mutation in exon 21 and exon 19 deletions, sensitize tumors and are used as biomarkers to preferentially identify patients for EGFR-TKI therapy. Most recently, irreversible multitargeted pan-HER EGFR-TKIs have been developed with the aim to provide sustained total EGFR blockade and specifically target resistance mutations (e.g., T790M).
A number of EGFR-TKIs are currently approved in the first-line treatment of NSCLC patients whose tumors harbor activating EGFR mutations (erlotinib, gefitinib, afatinib) and as second-line therapy in unselected NSCLC (erlotinib, gefitinib). Anti-EGFR mAbs (cetuximab, matuzumab, panitumumab, necitumumab) have been investigated in advanced NSCLC in combination with chemotherapy with some success [16, 17] but, as yet, have not received widespread regulatory approval.
Despite the disease’s high level of EGFR expression, EGFR inhibition in unselected sqNSCLC remains controversial [18, 19]. In the case of small molecule EGFR inhibitors, uptake has been limited by early reports suggesting a low frequency of sensitizing EGFR mutations (∼3%) in sqNSCLC [20]. Clinical responses in EGFR wild-type NSCLC patients, however, have been reported in retrospective analysis of most of the early EGFR-TKI trials [13, 21, 22], and more recently erlotinib has been shown to improve overall survival (OS) in meta-analysis in patients with EGFR wild-type disease after induction chemotherapy [23], suggesting that mutation-independent mechanisms likely also contribute to the observed efficacy of EGFR-TKI therapy [24].
The ability to definitively establish EGFR inhibition as a viable therapeutic strategy in advanced sqNSCLC has been hampered by a lack of power in the early EGFR-inhibition trials, as patients with squamous histology usually made up only 20%–30% of the study population [13, 16, 25]. Recently, a number of meta-analyses of the early EGFR-inhibition trials in advanced NSCLC have been undertaken, allowing for subgroup analysis by NSCLC histology [18, 26–29]. Combined with emerging data from a number of clinical trials limited to patients with squamous histology [30, 31], a review of the current evidence for EGFR inhibition as a therapeutic strategy in sqNSCLC is timely. Herein, we present a summary of the evidence from randomized trials of EGFR inhibition with EGFR-TKIs and anti-EGFR mAbs in advanced sqNSCLC in the front-line setting and beyond. The aim of this review is to guide the future management of advanced sqNSCLC with EGFR-targeted therapies. However, with the recent publication of the sqNSCLC Checkmate 017 study findings showing improved survival with the anti-PD-1 inhibitor nivolumab over docetaxel (9.2 vs. 6.0 months, hazard ratio [HR] 0.59, p < .001) [32], immune checkpoint blockade is redefining the second-line treatment of sqNSCLC and has created therapeutic optimism for overall future management. Therefore, the anti-EGFR trial data presented in this review must be considered in the context of a rapidly evolving field of research in sqNSCLC.
EGFR Inhibition as First-Line Therapy in Advanced Squamous NSCLC
EGFR-TKI monotherapy
Despite the high proportion of patients with advanced NSCLC who are medically unfit to undergo chemotherapy, few randomized trials have evaluated the clinical efficacy of EGFR-TKIs over best supportive care (BSC). Although mainly limited to small phase II randomized trials [33–37], one large phase III placebo-controlled trial (TOPICAL) evaluated the role of erlotinib as a front-line management strategy in NSCLC patients not eligible for chemotherapy [38]. Although that study demonstrated improved progression-free survival (PFS) in patients receiving erlotinib (2.8 vs. 2.6 months adjusted PFS, HR 0.80, 95% confidence interval [CI] 0.68–0.93) in the full study population, the median OS between treatment arms did not differ (3.7 vs. 3.6 months, HR 0.94, 95% CI 0.81–1.10) [38]. Improvement in OS was limited to the 59% of patients who developed a first-cycle rash to erlotinib (6.2 vs. 4.1 months, HR OS 0.76, 95% CI 0.63–0.92) [38], a finding not unique to the study [39, 40]. Patients with nonadenocarcinoma histology (not limited to squamous) and a first-cycle rash also had longer PFS (HR 0.77, 95% CI 0.61–0.97), albeit in the absence of improved OS (HR 0.91, 95% CI 0.72–1.15) [38]. Although it increased the rates of diarrhea, hair loss, and constipation, treatment with erlotinib significantly improved quality of life and disease-related symptoms, including chest pain and dyspnea [38], which in the context of advanced lung cancer are important considerations.
In patients eligible for chemotherapy, EGFR-TKI therapy is not recommended in the first-line setting in NSCLC patients whose tumors are not known to harbor EGFR mutations [41, 42]. The inferiority of EGFR-TKIs as a front-line strategy has been demonstrated in phase III trials in both unselected NSCLC [43] and patients with EGFR wild-type disease [44–46]. In fact, the inferiority of up-front EGFR-TKI therapy compared with chemotherapy in the TORCH trial in unselected NSCLC patients resulted in its early termination after a planned interim analysis. After a median follow-up of 24.3 months for the 760 patients enrolled before the trial’s premature closure, the adjusted overall survival was 11.6 vs. 8.6 months (HR 1.24, 95% CI 1.04–1.47) favoring chemotherapy [43]. Of note, in that study, comparable treatment effects were also noted in patients with squamous/large cell/undefined histology (HR OS 1.08, 95% CI 0.84–1.39) [43]. As such, platinum-based chemotherapy doublets remain the most appropriate first-line treatment strategy in patients with advanced NSCLC whose tumors are not known to harbor activating EGFR mutations, including those with squamous histology.
EGFR-TKI Combination Therapy
As part of a combined regimen with chemotherapy in unselected NSCLC, EGFR-TKI therapy has also failed to demonstrate clinical superiority over chemotherapy alone in the first-line setting, with post hoc univariate analyses across all trials consistently reporting no survival differences between treatments by NSCLC histology [47–50]. These findings have been supported in a meta-analysis of six randomized controlled trials, which showed that combination therapy in unselected patients with advanced NSCLC resulted in comparable OS of 10.6 vs. 11.0 months (HR OS 1.04, 95% CI 0.96–1.13) [51]. Antagonism between the cytostatic EGFR-TKI agent and cell cycle-dependent chemotherapeutics has been advanced as a mechanism to explain these findings [52], which have to date prevented concurrent administration of chemotherapy and EGFR-TKIs as first-line treatment. Although intercalated regimens have been investigated [53, 54], preliminary evidence suggests that the therapeutic benefit of this strategy will be limited to patients with activating EGFR mutations and adenocarcinoma histology [54], limiting its relevance in the management of advanced sqNSCLC.
Anti-EGFR Monoclonal Antibody Therapy in Squamous NSCLC
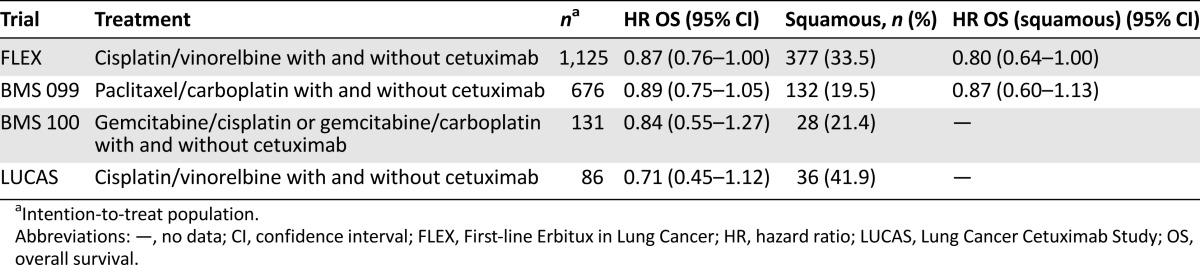
Anti-EGFR monoclonal antibodies have not been evaluated as monotherapy in the front-line management of patients with advanced NSCLC because of their limited single-agent activity (response rate ∼4%) [55]. As part of a combination regimen, four trials (BMS-099, FLEX [First-line Erbitux in Lung Cancer], LUCAS [Lung Cancer Cetuximab Study], and BMS-100) have evaluated cetuximab, a chimeric (mouse:human) IgG1 monoclonal antibody against EGFR, versus chemotherapy alone as first-line treatment in advanced NSCLC (Table 1) [16, 17, 56, 57]. Although generally favoring combination therapy [16, 17], an overall survival benefit with the addition of cetuximab in unselected NSCLC has only recently been established in a meta-analysis, based on the pooled analysis of individual patient data from these four trials (10.3 vs. 9.4 months, HR OS 0.88, 95% CI 0.79–0.97) [26]. Of relevance to this review, that meta-analysis also confirmed the greater survival benefit with cetuximab in patients with sqNSCLC (9.9 vs. 9.0 months, HR 0.77, 95% CI 0.64–0.93), despite not delaying disease progression in this patient subgroup (HR PFS 0.90, 95% CI 0.74–1.09) [26]. The superior efficacy of this combination regimen in patients with squamous histology may be caused by their high EGFR expression. Indeed, the results of the FLEX trial showed better OS (12.0 vs. 9.6 months) in patients with high EGFR expression, among whom patients with squamous histology were found to benefit most from cetuximab (11.2 vs. 8.9 months, HR 0.62, 95% CI 0.43–0.88) [58]. The potential benefit of cetuximab to patients with squamous histology, however, must be considered within the context of the increased grade 3 and 4 toxicities in NSCLC patients receiving combination therapy [58].
Table 1.
Randomized trials of first-line cetuximab plus chemotherapy in advanced non-small cell lung cancer
The modest clinical benefit in individual cetuximab and chemotherapy trials, combined with the increased toxicity of combination therapy, has until now limited its regulatory approval in the front-line setting. However, a large phase III trial of combination therapy of the second-generation IgG1 anti-EGFR fully human antibody necitumumab with cisplatin-gemcitabine chemotherapy in NSCLC patients with squamous histology (SQUIRE) has recently demonstrated improved overall survival over chemotherapy alone (11.5 vs. 9.9 months, HR OS 0.84, 95% CI 0.74–0.96) and was generally better tolerated than cetuximab, with fewer skin toxicities and thromboembolic events observed [31]. Given the lack of treatment options in the first-line setting for patients with squamous histology and the limited efficacy of conventional chemotherapy regimens, a reassessment of this combination strategy may be warranted, given the superior efficacy and improved tolerability of the newer EGFR mAbs.
In summary, even among patients whose tumors are not known to harbor EGFR mutations, EGFR inhibition is an important strategy in the front-line management of patients with advanced sqNSCLC. In unselected chemotherapy-ineligible patients, single-agent EGFR-TKIs are a valid treatment option that may delay disease progression and improve disease-related symptoms over BSC. Where chemotherapy is a treatment option, unselected/EGFR wild-type squamous NSCLC patients should be managed with a platinum-based doublet, as data suggest superior outcomes with chemotherapy in the absence of EGFR mutations. Although concurrent use of EGFR-TKIs and chemotherapy may be antagonistic, adding anti-EGFR mAbs in the front-line setting has been shown to improve OS in sqNSCLC in meta-analysis, and more recently in the SQUIRE trial. Against a chemotherapy backbone, the addition of newer-generation anti-EGFR mAbs may be a valid therapeutic strategy in patients with squamous histology to improve treatment outcomes, given their improved tolerability as part of a combination regimen.
Where chemotherapy is a treatment option, unselected/EGFR wild-type squamous NSCLC patients should be managed with a platinum-based doublet, as data suggest superior outcomes with chemotherapy in the absence of EGFR mutations.
EGFR Inhibition as Second/Third-Line Therapy in Advanced Squamous NSCLC
EGFR-TKI Monotherapy
Compared with placebo or BSC, second-line erlotinib has been shown to improve PFS and OS in both unselected patients with advanced NSCLC and those with tumors of squamous histology [13, 59]. The definitive BR.21 trial of erlotinib versus placebo in the treatment of advanced NSCLC patients who had failed one or two lines of chemotherapy showed that erlotinib improved OS in the full study population (6.7 vs. 4.7 months, HR OS 0.70, 95% CI 0.58–0.85) [13]. In subgroup analysis of the 222 patients with tumors of squamous histology, erlotinib was also shown to improve OS (5.6 vs. 3.6 months, HR OS 0.67, 95% CI 0.50–0.90) [59], an improvement comparable to that of second-line chemotherapy in patients with squamous histology [60]. A similar phase III trial with gefitinib (ISEL), however, did not show an overall survival benefit in either the full study population (HR OS 0.89, 95% CI 0.77–1.02) or patients with nonadenocarcinoma histology (HR OS 0.92, 95% CI 0.75–1.12), not limited to patients with squamous histology [25]. The reason for the different results obtained in BR.21 and ISEL is unclear and is a matter of ongoing debate [61].
Given the improved efficacy of the newer-generation small molecule inhibitors against EGFR, EGFR-TKIs will likely continue to play an important role in the management of patients with squamous histology who have failed induction chemotherapy. Supporting this contention are the recent results of the LUX-Lung 8 trial in patients with sqNSCLC that compared the second-generation pan-HER irreversible EGFR-TKI, afatinib, with erlotinib in the second-line setting. That trial demonstrated a statistically significant improvement in PFS (2.4 vs. 1.9 months, HR PFS 0.82, 95% CI 0.676–0.998) [30] and OS (7.9 vs. 6.8 months, HR 0.81, 95% CI 0.69–0.95) for afatinib versus erlotinib [30]. With the recent approval of PD-1 inhibitors in the second-line management of patients with squamous NSCLC (discussed later under Other Approaches), the identification of sqNSCLC patients most likely to benefit from EGFR-TKI therapy will be increasingly important. In this respect, the correlative translational studies being conducted under the LUX-Lung 8 trial will be particularly informative.
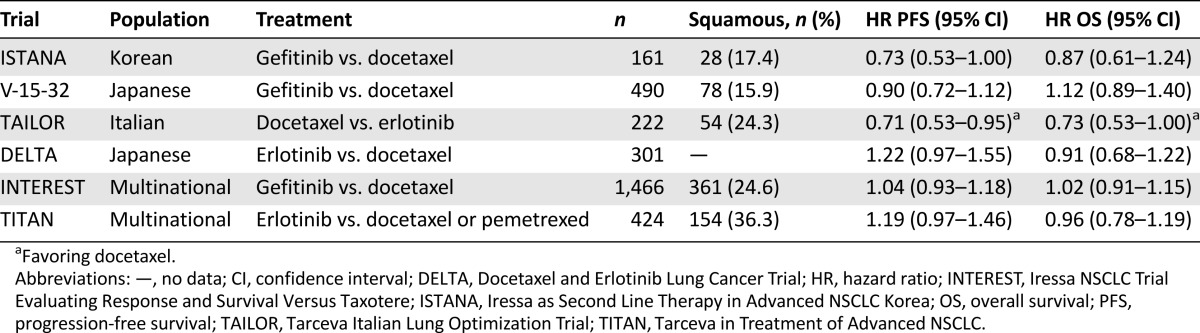
The role of second-line EGFR-TKI therapy in chemotherapy-eligible patients with unselected/wild-type EGFR sqNSCLC remains controversial. In this setting, a number of head-to-head trials comparing EGFR-TKIs to chemotherapy have been conducted, with mixed results (Table 2) [62–67]. One such trial compared survival in patients with advanced NSCLC treated with gefitinib or docetaxel after induction chemotherapy [66]. INTEREST was a large (n = 1,433) noninferiority trial in which patients were randomized 1:1 to daily oral gefitinib (250 mg) or 75 mg/m2 intravenous infusions of docetaxel every 3 weeks until disease progression. The final analysis of OS established noninferiority of these two regimens (7.6 vs. 8.0 months, HR OS 1.02, 96% CI 0.905–1.15), with results being consistent across histologic subgroups, including patients with nonadenocarcinoma histology (6.4 vs. 6.9 months) [66]. Although another smaller second-line trial (n = 222) of erlotinib versus docetaxel did suggest a survival difference favoring docetaxel in patients with EGFR wild-type NSCLC tumors (8.2 vs. 5.4 months, adjusted HR OS 0.73, 95% CI 0.53–1.00, p = .05), among patients with sqNSCLC there was no difference in OS (HR OS 0.90, 95% 0.49–1.65) [64]. More recently, a meta-analysis of second-line EGFR-TKI versus chemotherapy trials has reported comparable overall survival of these two treatment strategies in unselected NSCLC patients (HR OS 1.00, 95% CI 0.92–1.08) and in the EGFR wild-type population (HR OS 0.96, 95% CI 0.77–1.19); however, results were not reported separately by histology [29].
Table 2.
Select randomized trials of second-line epidermal growth factor receptor tyrosine kinase inhibitor versus chemotherapy in advanced non-small cell lung cancer
In trials comparing EGFR-TKIs to chemotherapy, EGFR-TKI therapy is generally found to be more tolerable as second-line therapy [28, 29]. In the metastatic NSCLC setting, relief of disease-related symptoms and minimization of treatment-associated toxicities in successive lines of treatment is particularly important. Although the results from more recent trials using more sensitive EGFR mutation platforms that may better define EGFR wild-type and mutant subgroups suggest that chemotherapy may result in longer PFS in EGFR wild-type NSCLC, in most of these trials the OS remained comparable [64, 68]. With the recent approval of PD-1 inhibitors for sqNSCLC, chemotherapy is an even less attractive treatment alternative in the second-line setting and is no longer an appropriate comparator for future second-line trials.
Anti-EGFR Monoclonal Antibodies
The limited single-agent activity of EGFR mAbs and concerns regarding toxicity of combination cytotoxic therapy beyond first-line therapy has limited investigations of anti-EGFR mAb therapies in the second-line management of advanced NSCLC, including those with squamous histology. This has been confirmed by the results of the SELECT trial, which showed no overall survival benefit by adding cetuximab to docetaxel or pemetrexed in pretreated patients with advanced NSCLC, with notable increases in adverse events across all histologies [69].
In summary, in the second-line setting, EGFR-TKIs have been shown to improve OS over BSC in patients with squamous histology and remain a therapeutic option for patients who are not eligible for chemotherapy. In second and subsequent lines of therapy, this represents and increasingly bigger proportion of the sqNSCLC population. EGFR-TKIs also remain a viable treatment alternative in the management of chemotherapy-eligible sqNSCLC patients who have failed first-line chemotherapy, given the comparable survival outcomes of EGFR-TKI and chemotherapy in the second-line setting. With the recent approval of anti-PD-1 agents as second-line therapy in patients with squamous histology, docetaxel will likely be relegated to third-line therapy moving forward. Although not directly comparable, the similar median survival of sqNSCLC patients receiving nivolumab (9.2 months) and the newer EGFR-TKI afatinib (7.9 months) in Checkmate 017 and LUX-Lung 8 trials, respectively, supports both of these targeted agents as valid treatment options in the second-line setting in the absence of results of their head-to-head comparison. The important issue is that for the first time there are multiple therapeutic options for advanced sqNSCLC in the second-line setting. The type of regimen (single agent vs. combination therapy) and sequencing of available targeted therapies that will optimize outcomes for sqNSCLC patients who have failed induction chemotherapy have yet to be defined, but new treatment opportunities exist for this historically neglected subgroup of NSCLC patients.
With the recent approval of anti-PD-1 agents as second-line therapy in patients with squamous histology, docetaxel will likely be relegated to third-line therapy moving forward.
EGFR Inhibition as Maintenance Therapy in Advanced Squamous NSCLC
Up to half of the patients with advanced NSCLC who benefit from first-line chemotherapy are not eligible for second-line chemotherapy at the time of disease progression [6, 70]. Having squamous histology is a negative predictor for treatment beyond first-line therapy in advanced NSCLC, with only a third of patients with squamous histology receiving subsequent therapies [71]. Maintenance therapy has recently been introduced as a strategy in advanced NSCLC to enhance the number of patients receiving treatment beyond induction chemotherapy and improve survival outcomes in the 40%–50% of patients whose best response to chemotherapy is stable disease. Given the low likelihood of second-line treatment in patients with sqNSCLC, maintenance therapy is a particularly attractive therapeutic strategy. The use of EGFR-TKIs as long-term maintenance therapy is supported by preclinical data suggesting a relationship between cytotoxic resistance and activation of the EGFR pathway [72, 73] and by its manageable toxicity profile.
SATURN is the largest trial to date investigating EGFR-TKI treatment as maintenance therapy in unselected NSCLC patients with stable disease or partial/complete response (PR/CR) after induction chemotherapy. Among the 889 patients randomized, erlotinib was shown to improve PFS in both patients with stable disease (12.1 vs. 11.3 weeks, HR PFS 0.68, p < .0001) and those with PR/CR (12.4 vs. 11.1 weeks, HR PFS 0.74, p > .0059) [74]. Erlotinib was also found to delay disease progression in patients with squamous histology (n = 360), irrespective of response to induction chemotherapy (PFS HR 0.76, 95% CI 0.60–0.95) [75]. Improved OS, however, was noted only in the 55% of patients with stable disease (11.9 vs. 9.6 months, HR OS 0.72, 95% CI 0.59–0.89) [74]. Among patients with stable disease, the greatest overall survival benefit was in patients with tumors of squamous histology (HR OS 0.67, 95% CI 0.48–0.92) [74]. This trial has been criticized because of the high proportion of patients in the placebo arm who never received second-line treatment; however, it is unclear whether this is a shortcoming of the study or an accurate reflection of the treatment paradigm for patients with advanced NSCLC. In a smaller three-arm study of gemcitabine continuation maintenance or erlotinib switch maintenance, both erlotinib (PFS 2.9 vs. 1.9 months, HR 0.82, 95% CI 0.73–0.93) and gemcitabine (3.8 vs. 1.9 months, HR 0.55, 95% CI 0.43–0.70) were shown to improve PFS over observation, with the benefit being similar in patients with nonadenocarcinoma histology (erlotinib: PFS HR 0.88, 95% CI 0.72–1.08; gemcitabine: PFS HR 0.56, 95% CI 0.37–0.85) [76].
Clinical trials of maintenance gefitinib after induction chemotherapy have also demonstrated improved PFS in a number of studies [77, 78]; however, these have not translated into improved overall survival in the individual trials. The limited number of patients with squamous histology in the gefitinib trials [77, 78] has limited interpretation of these findings for this subgroup. However, in a recent meta-analysis of EGFR-TKI maintenance trials (erlotinib or gefitinib), EGFR-TKIs were shown to reduce the risk of disease progression in unselected patients with advanced NSCLC (PFS HR 0.63, 95% CI 0.50–0.76), with the benefit being similar in patients with nonadenocarcinoma histology (HR 0.77, 95% CI 0.64–0.90) [79].
In summary, maintenance therapy is a particularly attractive therapeutic strategy in advanced sqNSCLC given the low likelihood of receiving second-line therapy. EGFR-TKI maintenance trials suggest that these agents delay disease progression in patients who respond to first-line chemotherapy, including those with squamous histology. Given the poor prognosis of patients with stable disease after induction chemotherapy, maintenance EGFR-TKIs may represent an important therapeutic strategy in the management of sqNSCLC. With the introduction of new targeted therapies in the second-line setting, the timing of additional therapies (immediate versus deferred until progression) and the sequencing of available treatments will need to be defined.
Other Approaches in the Management of Squamous Cell Carcinoma of the Lung
Although historically at a therapeutic disadvantage compared with patients with nonsquamous NSCLC, a number of treatment strategies for advanced sqNSCLC are being developed and are under clinical investigation. Although it is not possible to address these in depth, it is important to acknowledge these emerging strategies in the management of squamous cell carcinoma of the lung.
The poor outcomes following conventional cytotoxic chemotherapy and the lack of treatment alternatives in sqNSCLC have prompted the evaluation of combination therapies aimed at enhancing the efficacy of established cytotoxic therapies. In the first-line setting, combination therapy of a platinum doublet with agents such as iniparib, a poly-ADP ribose polymerase inhibitor, has failed to demonstrate improved overall survival (ECLIPSE) [80]. In the second-line setting, the antiangiogenic inhibitor ramucirumab has recently been shown to improve survival by 1.4 months (10.5 vs. 9.1 months, HR OS 0.86, 95% CI 0.75–0.98) when used in combination with docetaxel in the REVEL study, with comparable efficacy noted in sqNSCLC in subgroup analysis (9.5 vs. 8.2 months, HR OS 0.88, 95% CI 0.69–1.13) [81]. The impact of this combination in the overall management of patients with squamous histology is, however, uncertain.
Treatment with combinations of targeted agents in the second-line setting has also been evaluated as a strategy to improve clinical outcomes over EGFR-TKI monotherapy. Although mostly limited to phase II trials [82–86], there is some evidence that combination therapies that target multiple pathways may enhance treatment efficacy in sqNSCLC. Although an OS benefit of this approach has yet to be established [87], results from a phase III trial of erlotinib and sunitinib in previously treated sqNSCLC patients demonstrated a numerically superior PFS with combination therapy (HR PFS 0.80, 95% CI 0.61–1.05) [88]. At this time, however, this combination regimen is not approved in the second-line setting.
Finally, a number of molecular targets other than EGFR have recently been identified in sqNSCLC using comprehensive genome analysis [89]. Although a number of therapies targeting these molecular aberrations are currently under investigation in the LUNG MAP master protocol [90], their approval for the management of patients with sqNSCLC may be several years away. Immunotherapies that target immune checkpoints are also increasingly being investigated in lung cancer. Encouraging data on two PD-1 inhibitors (nivolumab and pembrolizumab) and a PD-L1 inhibitor (MPDL3280A [atezolizumab]) in NSCLC have recently been published [32, 91–95], with atezolizumab receiving FDA breakthrough designation in NSCLC patients with PD-L1-positive tumors progressing after induction chemotherapy, based on encouraging preliminary results [96]. Pembrolizumab has also received breakthrough designation in the second-line management of advanced NSCLC based on the results of the phase Ib trial (KEYNOTE-001) [97]. More recently, nivolumab has received FDA approval as a second-line therapy for metastatic sqNSCLC [98] based on the superior OS of sqNSCLC patients treated with nivolumab compared with docetaxel (9.2 vs. 6.0 months, HR 0.59, p < .001) in CHECKMATE 017, a randomized open-label trial [32, 91]. Although these results are encouraging, given the shorter-than-expected survival in the docetaxel arm in CHECKMATE 017 compared with previous reports [60], these early results require external validation. Nonetheless, PD-1/PD-L1 therapies are particularly exciting because of durable responses in excess of 1 year that have been documented in a percentage of patients on trial [32]. Although these possibilities expand the treatment options for patients with advanced sqNSCLC who have failed chemotherapy, the treatment strategy that will optimize therapeutic outcomes using these agents has not yet been defined, and the unique toxicities associated with this class of immune-modulating agents are still under investigation.
Discussion
Despite their established efficacy in unselected/EGFR wild-type NSCLC, EGFR-TKIs are increasingly being used in biomarker-selected patients where their efficacy is more pronounced [99, 100]. This shift in the management strategy in advanced NSCLC puts patients with squamous histology at a disadvantage because of the belief that their tumors rarely harbor EGFR mutations, and further limits their treatment options. Accumulating data of EGFR inhibition in NSCLC has afforded the opportunity to revisit anti-EGFR treatment in sqNSCLC and has confirmed a role for these agents in sqNSCLC management. Combined with emerging data from trials limited to patients with squamous histology, the role of EGFR inhibition in patients with squamous cell carcinoma of the lung is being redefined.
In patients not eligible for chemotherapy, first-line EGFR-TKI treatment with erlotinib has been shown to improve quality of life and delay progression compared with BSC in unselected NSCLC. Erlotinib has also been shown to improve PFS and OS in patients with sqNSCLC who have failed first-line chemotherapy. Second-line EGFR-TKIs have survival outcomes comparable to those of chemotherapy and better tolerability in advanced NSCLC, including in wild-type disease and nonadenocarcinoma/squamous histology. Maintenance EGFR-TKI therapy has been shown to delay disease progression in patients who respond to induction chemotherapy and to improve survival in meta-analyses in unselected NSCLC and in patients with squamous histology and is an important therapeutic option for sqNSCLC patients who may deteriorate too quickly to be eligible for second-line chemotherapy.
In chemotherapy-eligible patients, EGFR inhibition is an important component of a first-line strategy in the management of patients with squamous histology. Specifically, in a meta-analysis of cetuximab trials and more recently in a large phase III trial with necitumumab, anti-EGFR mAbs in combination with chemotherapy were shown to improve PFS and OS in sqNSCLC. Although survival benefits are modest, they are noteworthy because they enhance the efficacy of the only approved first-line therapy for advanced sqNSCLC.
The biologic mechanism accounting for the efficacy of EGFR inhibition in sqNSCLC is likely multifactorial. First, genomic alterations of EGFR may be more common than previously suspected. Specifically, in the two thirds of sqNSCLC with activation of the phosphatidylinositol 3-kinase/receptor tyrosine kinase/Ras pathways, recent genomic analyses suggest that EGFR alterations occur with a frequency of ∼9% [89]. This may, in part, explain the efficacy of EGFR inhibition in sqNSCLC in the early EGFR-TKI trials. Second, second-generation EGFR-TKIs, such as afatinib, which irreversibly bind to enzymatically active ErbB receptors, likely enable sustained Erb family blockade including receptor activation, dimerization, and resistance inhibition and account for their enhanced efficacy over erlotinib in sqNSCLC. Third, the improved efficacy of anti-EGFR mAbs in squamous cell carcinoma of the lung is mostly likely caused by their higher EGFR expression, which is consistent with the efficacy of anti-EGFR mAbs in other high-EGFR-expressing tumors such as squamous cell carcinoma of the head and neck.
Although EGFR inhibition is a valid therapeutic approach in the management of advanced sqNSCLC patients, the benefits are modest and overall prognosis remains poor. The evaluation of therapies aimed at novel molecular targets in sqNSCLC has recently been enabled by comprehensive genomic characterization by The Cancer Genome Atlas project. Moving forward, combination therapies targeting multiple oncogenic pathways appear to be a rational approach to improve therapeutic efficacy. Given the manageable toxicities of anti-EGFR therapies, combinations of EGFR inhibitors with other targeted agents is feasible. With the encouraging results of PD-1/PD-L1 immune checkpoint inhibition in NSCLC, including in squamous histology, anti-EGFR combination regimens that include an immune checkpoint inhibitor may be a valid strategy. In this respect, combination therapy with anti-EGFR monoclonal antibodies may be a rational therapeutic approach, given that anti-EGFR mAbs have been shown to activate a number of immune mechanisms resulting in cellular cytotoxicity [101]. The sequencing of available targeted therapies that will optimize outcomes for sqNSCLC patients has yet to be defined but offers exciting treatment opportunities in their future management.
With the encouraging results of PD-1/PD-L1 immune checkpoint inhibition in NSCLC, including in squamous histology, anti-EGFR combination regimens that include an immune checkpoint inhibitor may be a valid strategy.
Conclusion
Patients with advanced sqNSCLC have historically been at a therapeutic disadvantage. Recent meta-analyses have definitively established the role of anti-EGFR therapies in their treatment. Combined with the positive phase III results of newer anti-EGFR therapies, such as afatinib in the second-line setting and necitumumab in combination with chemotherapy in the first-line setting, EGFR-targeted therapies are a valid therapeutic strategy in sqNSCLC. As more targeted agents are approved, novel combination regimens that include an anti-EGFR therapy should be evaluated, and the optimal sequencing of available targeted therapies should be defined.
Author Contributions
Conception/Design: Glenwood D. Goss, Johanna N. Spaans
Provision of study material or patients: Johanna N. Spaans
Collection and/or assembly of data: Glenwood D. Goss, Johanna N. Spaans
Data analysis and interpretation: Glenwood D. Goss, Johanna N. Spaans
Manuscript writing: Glenwood D. Goss, Johanna N. Spaans
Final approval of manuscript: Glenwood D. Goss, Johanna N. Spaans
Disclosures
Glenwood D. Goss: AstraZeneca, Roche, Boehringer Ingelheim Pharmaceuticals, Inc., Bristol-Myers Squibb, Pfizer (C/A, H), AstraZeneca (RF). The other author indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1.World Health Organization. Cancer Fact Sheet no. 297. Available at http://www.who.int/mediacentre/factsheets/fs297/en/. Accessed March 3, 2015.
- 2.Travis WD. Pathology of lung cancer. Clin Chest Med. 2011;32:669–692. doi: 10.1016/j.ccm.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 3.Wao H, Mhaskar R, Kumar A, et al. Survival of patients with non-small cell lung cancer without treatment: A systematic review and meta-analysis. Syst Rev. 2013;2:10. doi: 10.1186/2046-4053-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355:2542–2550. doi: 10.1056/NEJMoa061884. [DOI] [PubMed] [Google Scholar]
- 5.Johnson DH, Fehrenbacher L, Novotny WF, et al. Randomized phase II trial comparing bevacizumab plus carboplatin and paclitaxel with carboplatin and paclitaxel alone in previously untreated locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol. 2004;22:2184–2191. doi: 10.1200/JCO.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 6.Scagliotti GV, Parikh P, von Pawel J, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol. 2008;26:3543–3551. doi: 10.1200/JCO.2007.15.0375. [DOI] [PubMed] [Google Scholar]
- 7.Scagliotti G, Brodowicz T, Shepherd FA, et al. Treatment-by-histology interaction analyses in three phase III trials show superiority of pemetrexed in nonsquamous non-small cell lung cancer. J Thorac Oncol. 2011;6:64–70. doi: 10.1097/JTO.0b013e3181f7c6d4. [DOI] [PubMed] [Google Scholar]
- 8.Peterson P, Park K, Fosella F, et al. Is pemetrexed more effective in adenocarcinoma and large cell lung cancer than in squamous cell carcinoma? A retrospective analysis of a phase III trial of pemetrexed vs docetaxel in previously treated patients with advanced non-small cell lung cancer (NSCLC) J Thorac Oncol. 2007;2:S851. [Google Scholar]
- 9.Ciuleanu T, Brodowicz T, Zielinski C, et al. Maintenance pemetrexed plus best supportive care versus placebo plus best supportive care for non-small-cell lung cancer: A randomised, double-blind, phase 3 study. Lancet. 2009;374:1432–1440. doi: 10.1016/S0140-6736(09)61497-5. [DOI] [PubMed] [Google Scholar]
- 10.Al-Farsi A, Ellis PM. Treatment paradigms for patients with metastatic non-small cell lung cancer, squamous lung cancer: First, second and third-line. Front Oncol. 2014;4:1–5. doi: 10.3389/fonc.2014.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pirker R. EGFR-directed monoclonal antibodies in non-small cell lung cancer. Target Oncol. 2013;8:47–53. doi: 10.1007/s11523-012-0244-7. [DOI] [PubMed] [Google Scholar]
- 12.Hirsch FR, Varella-Garcia M, Bunn PA, Jr, et al. Epidermal growth factor receptor in non-small-cell lung carcinomas: Correlation between gene copy number and protein expression and impact on prognosis. J Clin Oncol. 2003;21:3798–3807. doi: 10.1200/JCO.2003.11.069. [DOI] [PubMed] [Google Scholar]
- 13.Shepherd FA, Rodrigues Pereira J, Ciuleanu T, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med. 2005;353:123–132. doi: 10.1056/NEJMoa050753. [DOI] [PubMed] [Google Scholar]
- 14.Mendelsohn J, Baselga J. Epidermal growth factor receptor targeting in cancer. Semin Oncol. 2006;33:369–385. doi: 10.1053/j.seminoncol.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 15.Leung L, Mok TSK, Loong H. Combining chemotherapy with epidermal growth factor receptor inhibition in advanced non-small cell lung cancer. Ther Adv Med Oncol. 2012;4:173–181. doi: 10.1177/1758834012440015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lynch TJ, Patel T, Dreisbach L, et al. Cetuximab and first-line taxane/carboplatin chemotherapy in advanced non-small-cell lung cancer: Results of the randomized multicenter phase III trial BMS099. J Clin Oncol. 2010;28:911–917. doi: 10.1200/JCO.2009.21.9618. [DOI] [PubMed] [Google Scholar]
- 17.Pirker R, Pereira JR, Szczesna A, et al. Cetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): An open-label randomised phase III trial. Lancet. 2009;373:1525–1531. doi: 10.1016/S0140-6736(09)60569-9. [DOI] [PubMed] [Google Scholar]
- 18.Ameratunga M, Pavlakis N, Gebski V, et al. Epidermal growth factor receptor-tyrosine kinase inhibitors in advanced squamous cell carcinoma of the lung: A meta-analysis. Asia Pac J Clin Oncol. 2014;10:273–278. doi: 10.1111/ajco.12231. [DOI] [PubMed] [Google Scholar]
- 19.Scagliotti GV, Novello S, Rapetti S, et al. Current state-of-the art therapy for advanced squamous cell lung cancer ASCO Educational Book 2013354–358. [DOI] [PubMed]
- 20.Marchetti A, Martella C, Felicioni L, et al. EGFR mutations in non-small-cell lung cancer: analysis of a large series of cases and development of a rapid and sensitive method for diagnostic screening with potential implications on pharmacologic treatment. J Clin Oncol. 2005;23:857–865. doi: 10.1200/JCO.2005.08.043. [DOI] [PubMed] [Google Scholar]
- 21.Douillard JY, Kim ES, Hirsh V, et al. Phase III randomized, open-label, parallel group study of oral gefitinib (IRESSA) versus intravenous docetaxel in patients with locally advanced or metastatic non-small cell lung cancer who have previously received platinum-based chemotherapy (INTEREST) Eur J Cancer. 2007;5:2. [Google Scholar]
- 22.Hirsch FR, Varella-Garcia M, Bunn PA, Jr, et al. Molecular predictors of outcome with gefitinib in a phase III placebo-controlled study in advanced non-small-cell lung cancer. J Clin Oncol. 2006;24:5034–5042. doi: 10.1200/JCO.2006.06.3958. [DOI] [PubMed] [Google Scholar]
- 23.Jazieh AR, Al Sudairy R, Abu-Shraie N, et al. Erlotinib in wild type epidermal growth factor receptor non-small cell lung cancer: A systematic review. Ann Thorac Med. 2013;8:204–208. doi: 10.4103/1817-1737.118503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Laurie SA, Goss GD. Role of epidermal growth factor receptor inhibitors in epidermal growth factor receptor wild-type non-small-cell lung cancer. J Clin Oncol. 2013;31:1061–1069. doi: 10.1200/JCO.2012.43.4522. [DOI] [PubMed] [Google Scholar]
- 25.Thatcher N, Chang A, Parikh P, et al. Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: Results from a randomised, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer) Lancet. 2005;366:1527–1537. doi: 10.1016/S0140-6736(05)67625-8. [DOI] [PubMed] [Google Scholar]
- 26.Pujol JL, Pirker R, Lynch TJ, et al. Meta-analysis of individual patient data from randomized trials of chemotherapy plus cetuximab as first-line treatment for advanced non-small cell lung cancer. Lung Cancer. 2014;83:211–218. doi: 10.1016/j.lungcan.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 27.Arruda LM, Cruz FM, David WJ, et al. Meta-analysis of EGFR-TKI as maintenance therapy in non-small cell lung cancer (NSCLC) J Clin Oncol. 2014;32(suppl):e19081. [Google Scholar]
- 28.Lee CK, Brown C, Gralla RJ, et al. Impact of EGFR inhibitor in non-small cell lung cancer on progression-free and overall survival: A meta-analysis. J Natl Cancer Inst. 2013;105:595–605. doi: 10.1093/jnci/djt072. [DOI] [PubMed] [Google Scholar]
- 29.Li N, Yang L, Ou W, et al. Meta-analysis of EGFR tyrosine kinase inhibitors compared with chemotherapy as second-line treatment in pretreated advanced non-small cell lung cancer. PLoS One. 2014;9:e102777. doi: 10.1371/journal.pone.0102777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soria JC, Felip E, Cobo M, et al. Afatinib versus erlotinib as second-line treatment of patients with advanced squamous cell carcinoma of the lung (LUX-Lung 8): An open-label randomised controlled phase 3 trial. Lancet Oncol. 2015;16:897–907. doi: 10.1016/S1470-2045(15)00006-6. [DOI] [PubMed] [Google Scholar]
- 31.Thatcher N, Hirsch FR, Luft AV, et al. Necitumumab plus gemcitabine and cisplatin versus gemcitabine and cisplatin alone as first-line therapy in patients with stage IV squamous non-small-cell lung cancer (SQUIRE): An open-label, randomised, controlled phase 3 trial. Lancet Oncol. 2015;16:763–774. doi: 10.1016/S1470-2045(15)00021-2. [DOI] [PubMed] [Google Scholar]
- 32.Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small cell lung cancer. N Engl J Med. 2015;373:123–135. doi: 10.1056/NEJMoa1504627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Giaccone G, Gallegos Ruiz M, Le Chevalier T, et al. Erlotinib for frontline treatment of advanced non-small cell lung cancer: A phase II study. Clin Cancer Res. 2006;12:6049–6055. doi: 10.1158/1078-0432.CCR-06-0260. [DOI] [PubMed] [Google Scholar]
- 34.Lee DH, Kim SW, Suh C, et al. Phase II study of erlotinib for chemotherapy-naïve patients with advanced or metastatic non-small cell lung cancer who are ineligible for platinum doublets. Cancer Chemother Pharmacol. 2011;67:35–39. doi: 10.1007/s00280-010-1280-6. [DOI] [PubMed] [Google Scholar]
- 35.Niho S, Kubota K, Goto K, et al. First-line single agent treatment with gefitinib in patients with advanced non-small-cell lung cancer: A phase II study. J Clin Oncol. 2006;24:64–69. doi: 10.1200/JCO.2005.02.5825. [DOI] [PubMed] [Google Scholar]
- 36.Yang CH, Yu CJ, Shih JY, et al. Specific EGFR mutations predict treatment outcome of stage IIIB/IV patients with chemotherapy-naive non-small-cell lung cancer receiving first-line gefitinib monotherapy. J Clin Oncol. 2008;26:2745–2753. doi: 10.1200/JCO.2007.15.6695. [DOI] [PubMed] [Google Scholar]
- 37.Goss G, Ferry D, Wierzbicki R, et al. Randomized phase II study of gefitinib compared with placebo in chemotherapy-naive patients with advanced non-small-cell lung cancer and poor performance status. J Clin Oncol. 2009;27:2253–2260. doi: 10.1200/JCO.2008.18.4408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee SM, Khan I, Upadhyay S, et al. First-line erlotinib in patients with advanced non-small-cell lung cancer unsuitable for chemotherapy (TOPICAL): A double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2012;13:1161–1170. doi: 10.1016/S1470-2045(12)70412-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Petrelli F, Borgonovo K, Cabiddu M, et al. Relationship between skin rash and outcome in non-small-cell lung cancer patients treated with anti-EGFR tyrosine kinase inhibitors: A literature-based meta-analysis of 24 trials. Lung Cancer. 2012;78:8–15. doi: 10.1016/j.lungcan.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 40.Liu HB, Wu Y, Lv TF, et al. Skin rash could predict the response to EGFR tyrosine kinase inhibitor and the prognosis for patients with non-small cell lung cancer: A systematic review and meta-analysis. PLoS One. 2013;8:e55128. doi: 10.1371/journal.pone.0055128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ettinger DS, Akerley W, Borghaei H, et al. Non-small cell lung cancer. J Natl Compr Canc Netw. 2012;10:1236–1271. doi: 10.6004/jnccn.2012.0130. [DOI] [PubMed] [Google Scholar]
- 42.Peters S, Adjei AA, Gridelli C, et al. Metastatic non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(Suppl 7):vii56–vii64. doi: 10.1093/annonc/mds226. [DOI] [PubMed] [Google Scholar]
- 43.Gridelli C, Ciardiello F, Gallo C, et al. First-line erlotinib followed by second-line cisplatin-gemcitabine chemotherapy in advanced non-small-cell lung cancer: The TORCH randomized trial. J Clin Oncol. 2012;30:3002–3011. doi: 10.1200/JCO.2011.41.2056. [DOI] [PubMed] [Google Scholar]
- 44.Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–957. doi: 10.1056/NEJMoa0810699. [DOI] [PubMed] [Google Scholar]
- 45.Fukuoka M, Wu YL, Thongprasert S, et al. Biomarker analyses and final overall survival results from a phase III, randomized, open-label, first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer in Asia (IPASS) J Clin Oncol. 2011;29:2866–2874. doi: 10.1200/JCO.2010.33.4235. [DOI] [PubMed] [Google Scholar]
- 46.Lee JK, Hahn S, Kim DW, et al. Epidermal growth factor receptor tyrosine kinase inhibitors vs conventional chemotherapy in non-small cell lung cancer harboring wild-type epidermal growth factor receptor: A meta-analysis. JAMA. 2014;311:1430–1437. doi: 10.1001/jama.2014.3314. [DOI] [PubMed] [Google Scholar]
- 47.Gatzemeier U, Pluzanska A, Szczesna A, et al. Phase III study of erlotinib in combination with cisplatin and gemcitabine in advanced non-small-cell lung cancer: The Tarceva Lung Cancer Investigation Trial. J Clin Oncol. 2007;25:1545–1552. doi: 10.1200/JCO.2005.05.1474. [DOI] [PubMed] [Google Scholar]
- 48.Herbst RS, Prager D, Hermann R, et al. TRIBUTE: A phase III trial of erlotinib hydrochloride (OSI-774) combined with carboplatin and paclitaxel chemotherapy in advanced non-small-cell lung cancer. J Clin Oncol. 2005;23:5892–5899. doi: 10.1200/JCO.2005.02.840. [DOI] [PubMed] [Google Scholar]
- 49.Herbst RS, Giaccone G, Schiller JH, et al. Gefitinib in combination with paclitaxel and carboplatin in advanced non-small-cell lung cancer: A phase III trial--INTACT 2. J Clin Oncol. 2004;22:785–794. doi: 10.1200/JCO.2004.07.215. [DOI] [PubMed] [Google Scholar]
- 50.Giaccone G, Herbst RS, Manegold C, et al. Gefitinib in combination with gemcitabine and cisplatin in advanced non-small-cell lung cancer: A phase III trial--INTACT 1. J Clin Oncol. 2004;22:777–784. doi: 10.1200/JCO.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 51.Chen P, Wang L, Liu B, et al. EGFR-targeted therapies combined with chemotherapy for treating advanced non-small-cell lung cancer: A meta-analysis. Eur J Clin Pharmacol. 2011;67:235–243. doi: 10.1007/s00228-010-0965-4. [DOI] [PubMed] [Google Scholar]
- 52.Piperdi B, Ling YH, Kroog G, et al. Schedule-dependent interaction between epidermal growth factor inhibitors (EGFRI) and G2/M Blocking chemotherapeutic agents (G2/Mb) on human NSCLC cell lines in vitro. J Clin Oncol. 2004;22:7028. [Google Scholar]
- 53.Mok TS, Wu YL, Yu CJ, et al. Randomized, placebo-controlled, phase II study of sequential erlotinib and chemotherapy as first-line treatment for advanced non-small cell lung cancer. J Clin Oncol. 2009;27:5080–5087. doi: 10.1200/JCO.2008.21.5541. [DOI] [PubMed] [Google Scholar]
- 54.Hirsch F, Camidge RD, Kabbinavar F, et al. Biomarker status correlates with clinical benefit: phase 2 study of signal-agent erlotinib or intercalated with carboplatin and paclitaxel in and EGFR biomarker selected NSCLC population. J Thorac Oncol. 2008;3:S267. [Google Scholar]
- 55.Hanna N, Lilenbaum R, Ansari R, et al. Phase II trial of cetuximab in patients with previously treated non-small cell lung cancer. J Clin Oncol. 2006;24:5253–5258. doi: 10.1200/JCO.2006.08.2263. [DOI] [PubMed] [Google Scholar]
- 56.Rosell R, Robinet G, Szczesna A, et al. Randomized phase II study of cetuximab plus cisplatin/vinorelbine compared with cisplatin/vinorelbine alone as first-line therapy in EGFR-expressing advanced non-small-cell lung cancer. Ann Oncol. 2008;19:362–369. doi: 10.1093/annonc/mdm474. [DOI] [PubMed] [Google Scholar]
- 57.Butts CA, Bodkin D, Middleman EL, et al. Randomized phase II study of gemcitabine plus cisplatin or carboplatin [corrected], with or without cetuximab, as first-line therapy for patients with advanced or metastatic non small-cell lung cancer. J Clin Oncol. 2007;25:5777–5784. doi: 10.1200/JCO.2007.13.0856. [DOI] [PubMed] [Google Scholar]
- 58.Pirker R, Pereira JR, von Pawel J, et al. EGFR expression as a predictor of survival for first-line chemotherapy plus cetuximab in patients with advanced non-small-cell lung cancer: Analysis of data from the phase 3 FLEX study. Lancet Oncol. 2012;13:33–42. doi: 10.1016/S1470-2045(11)70318-7. [DOI] [PubMed] [Google Scholar]
- 59.Leon L, Lee G. Comparative efficacy and safety of erlotinib in non-small cell lung cancer of squamous cell and adenocarcinoma histology in the phase 3 NCIC CTG BR21 and SATURN (Bo18192) Trials. Paper presented at: 37th ESMO Conference; September 28, 2012; Vienna, Austria; Abstract 1277p. [Google Scholar]
- 60.Shepherd FA, Dancey J, Ramlau R, et al. Prospective randomized trial of docetaxel versus best supportive care in patients with non-small-cell lung cancer previously treated with platinum-based chemotherapy. J Clin Oncol. 2000;18:2095–2103. doi: 10.1200/JCO.2000.18.10.2095. [DOI] [PubMed] [Google Scholar]
- 61.Thatcher N. The ISEL and BR21 trials—Outcomes similar or different? Eur J Cancer. 2006;4:23–24. [Google Scholar]
- 62.Lee DH, Park K, Kim JH, et al. Randomized Phase III trial of gefitinib versus docetaxel in non-small cell lung cancer patients who have previously received platinum-based chemotherapy. Clin Cancer Res. 2010;16:1307–1314. doi: 10.1158/1078-0432.CCR-09-1903. [DOI] [PubMed] [Google Scholar]
- 63.Maruyama R, Nishiwaki Y, Tamura T, et al. Phase III study, V-15-32, of gefitinib versus docetaxel in previously treated Japanese patients with non-small-cell lung cancer. J Clin Oncol. 2008;26:4244–4252. doi: 10.1200/JCO.2007.15.0185. [DOI] [PubMed] [Google Scholar]
- 64.Garassino MC, Martelli O, Broggini M, et al. Erlotinib versus docetaxel as second-line treatment of patients with advanced non-small-cell lung cancer and wild-type EGFR tumours (TAILOR): A randomised controlled trial. Lancet Oncol. 2013;14:981–988. doi: 10.1016/S1470-2045(13)70310-3. [DOI] [PubMed] [Google Scholar]
- 65.Okano Y, Ando M, Asami K, et al. Randomized phase III trial of erlotinib (E) versus docetaxel (D) as second-or third-line therapy in patients with advanced non-small cell lung cancer (NSCLC) who have wild-type or mutant epidermal growth factor (EGFR): Docetaxel and erlotinib lung cancer trial (DELTA) J Clin Oncol. 2013;31:8006. doi: 10.1200/JCO.2013.52.4694. [DOI] [PubMed] [Google Scholar]
- 66.Kim ES, Hirsh V, Mok T, et al. Gefitinib versus docetaxel in previously treated non-small-cell lung cancer (INTEREST): A randomised phase III trial. Lancet. 2008;372:1809–1818. doi: 10.1016/S0140-6736(08)61758-4. [DOI] [PubMed] [Google Scholar]
- 67.Ciuleanu T, Stelmakh L, Cicenas S, et al. Efficacy and safety of erlotinib versus chemotherapy in second-line treatment of patients with advanced, non-small-cell lung cancer with poor prognosis (TITAN): A randomised multicentre, open-label, phase 3 study. Lancet Oncol. 2012;13:300–308. doi: 10.1016/S1470-2045(11)70385-0. [DOI] [PubMed] [Google Scholar]
- 68.Kawaguchi T, Ando M, Asami K, et al. Randomized phase III trial of erlotinib versus docetaxel as second- or third-line therapy in patients with advanced non-small-cell lung cancer: Docetaxel and Erlotinib Lung Cancer Trial (DELTA) J Clin Oncol. 2014;32:1902–1908. doi: 10.1200/JCO.2013.52.4694. [DOI] [PubMed] [Google Scholar]
- 69.Kim ES, Neubauer M, Cohn A, et al. Docetaxel or pemetrexed with or without cetuximab in recurrent or progressive non-small-cell lung cancer after platinum-based therapy: A phase 3, open-label, randomised trial. Lancet Oncol. 2013;14:1326–1336. doi: 10.1016/S1470-2045(13)70473-X. [DOI] [PubMed] [Google Scholar]
- 70.Fidias PM, Dakhil SR, Lyss AP, et al. Phase III study of immediate compared with delayed docetaxel after front-line therapy with gemcitabine plus carboplatin in advanced non-small-cell lung cancer. J Clin Oncol. 2009;27:591–598. doi: 10.1200/JCO.2008.17.1405. [DOI] [PubMed] [Google Scholar]
- 71.Hensing TA, Schell MJ, Lee JH, et al. Factors associated with the likelihood of receiving second line therapy for advanced non-small cell lung cancer. Lung Cancer. 2005;47:253–259. doi: 10.1016/j.lungcan.2004.07.040. [DOI] [PubMed] [Google Scholar]
- 72.Benhar M, Engelberg D, Levitzki A. Cisplatin-induced activation of the EGF receptor. Oncogene. 2002;21:8723–8731. doi: 10.1038/sj.onc.1205980. [DOI] [PubMed] [Google Scholar]
- 73.Dai Q, Ling YH, Lia M, et al. Enhanced sensitivity to the HER1/epidermal growth factor receptor tyrosine kinase inhibitor erlotinib hydrochloride in chemotherapy-resistant tumor cell lines. Clin Cancer Res. 2005;11:1572–1578. doi: 10.1158/1078-0432.CCR-04-0993. [DOI] [PubMed] [Google Scholar]
- 74.Coudert B, Ciuleanu T, Park K, et al. Survival benefit with erlotinib maintenance therapy in patients with advanced non-small-cell lung cancer (NSCLC) according to response to first-line chemotherapy. Ann Oncol. 2012;23:388–394. doi: 10.1093/annonc/mdr125. [DOI] [PubMed] [Google Scholar]
- 75.Cappuzzo F, Ciuleanu T, Stelmakh L, et al. Erlotinib as maintenance treatment in advanced non-small-cell lung cancer: A multicentre, randomised, placebo-controlled phase 3 study. Lancet Oncol. 2010;11:521–529. doi: 10.1016/S1470-2045(10)70112-1. [DOI] [PubMed] [Google Scholar]
- 76.Perol M, Chouaid C, Milleron BJ, et al. Maintenance with either gemcitabine or erlotinib versus observation with predefined second-line treatment after cisplatin-gemcitabine induction chemotherapy in advanced NSCLC: IFCT-GFPC 0502 phase III study. J Clin Oncol. 2010;28(suppl 15):7507a. [Google Scholar]
- 77.Zhang L, Ma S, Song X, et al. Gefitinib versus placebo as maintenance therapy in patients with locally advanced or metastatic non-small-cell lung cancer (INFORM; C-TONG 0804): A multicentre, double-blind randomised phase 3 trial. Lancet Oncol. 2012;13:466–475. doi: 10.1016/S1470-2045(12)70117-1. [DOI] [PubMed] [Google Scholar]
- 78.Gaafar RM, Surmont VF, Scagliotti GV, et al. A double-blind, randomised, placebo-controlled phase III intergroup study of gefitinib in patients with advanced NSCLC, non-progressing after first line platinum-based chemotherapy (EORTC 08021/ILCP 01/03) Eur J Cancer. 2011;47:2331–2340. doi: 10.1016/j.ejca.2011.06.045. [DOI] [PubMed] [Google Scholar]
- 79.Xiaofeng C, Liu Y, Roe O, et al. Gefitinib or erlotinib as maintenance therapy in patients with advanced stage non-small cell lung cancer: A systematic review. PLoS One. 2013;8:e59314. doi: 10.1371/journal.pone.0059314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sanofi Provides Update on Phase 3 Studies of Two Investigational Compounds. Available at http://en.sanofi.com/Images/33127_20130603_rdupdate_en.pdf. Accessed March 10, 2015.
- 81.Garon EB, Ciuleanu TE, Arrieta O, et al. Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): A multicentre, double-blind, randomised phase 3 trial. Lancet. 2014;384:665–673. doi: 10.1016/S0140-6736(14)60845-X. [DOI] [PubMed] [Google Scholar]
- 82.Lynch TJ, Fenton D, Hirsh V, et al. A randomized phase 2 study of erlotinib alone and in combination with bortezomib in previously treated advanced non-small cell lung cancer. J Thorac Oncol. 2009;4:1002–1009. doi: 10.1097/JTO.0b013e3181aba89f. [DOI] [PubMed] [Google Scholar]
- 83.Bennouna J, Besse B, Leighl NB, et al. Everolimus plus erlotinib versus erlotinib alone in previously treated patients with advanced non-small cell lung cancer (NSCLC). Ann oncol 2010;(suppl 21);419p. [DOI] [PubMed] [Google Scholar]
- 84.Sequist LV, von Pawel J, Garmey EG, et al. Randomized phase II study of erlotinib plus tivantinib versus erlotinib plus placebo in previously treated non-small-cell lung cancer. J Clin Oncol. 2011;29:3307–3315. doi: 10.1200/JCO.2010.34.0570. [DOI] [PubMed] [Google Scholar]
- 85.Ramalingam SS, Spigel DR, Chen D, et al. Randomized phase II study of erlotinib in combination with placebo or R1507, a monoclonal antibody to insulin-like growth factor-1 receptor, for advanced-stage non-small-cell lung cancer. J Clin Oncol. 2011;29:4574–4580. doi: 10.1200/JCO.2011.36.6799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Spigel DR, Burris HA, 3rd, Greco FA, et al. Randomized, double-blind, placebo-controlled, phase II trial of sorafenib and erlotinib or erlotinib alone in previously treated advanced non-small-cell lung cancer. J Clin Oncol. 2011;29:2582–2589. doi: 10.1200/JCO.2010.30.7678. [DOI] [PubMed] [Google Scholar]
- 87.Qi WX, Wang Q, Jiang YL, et al. Overall survival benefits for combining targeted therapy as second-line treatment for advanced non-small-cell-lung cancer: A meta-analysis of published data. PLoS One. 2013;8:e55637. doi: 10.1371/journal.pone.0055637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Scagliotti GV, Krzakowski M, Szczesna A, et al. Sunitinib plus erlotinib versus placebo plus erlotinib in patients with previously treated advanced non-small-cell lung cancer: A phase III trial. J Clin Oncol. 2012;30:2070–2078. doi: 10.1200/JCO.2011.39.2993. [DOI] [PubMed] [Google Scholar]
- 89.Cancer Genome Atlas Research Network Comprehensive genomic characterization of squamous cell lung cancers. Nature. 2012;489:519–525. doi: 10.1038/nature11404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Herbst RS, Gandara DR, Hirsch FF, et al. Lung master protocol (LUNG-MAP)—A biomarker-driven protocol for accelerating development of therapies for squamous cell lung cancer: SWOG S1400. Clin Cancer Res. 2015;21:1514–1524. doi: 10.1158/1078-0432.CCR-13-3473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Brahmer JR, Horn L, Gandhi L, et al. Nivolumab (anti-PD-1, BMS-936558, ONO-4538) in patients (Pts) with advanced non-small cell lung cancer (NSCLC): Survival and clinical activity by subgroup analysis. J Clin Oncol. 2014;32(suppl 5):8112a. [Google Scholar]
- 92.Garon EB, Gandhi L, Rizvi N et al. Antitumor activity of pembrolizumab (Pembro: MK-3475) and correlation with programmed death ligand 1 (PD-L1) expression in a pooled analysis of patients (pts) with advanced non-small cell lung cancer (NSCLC). Paper presented at: European Society of Medical Oncology Congress (ESMO); September 30, 2014; Madrid, Spain; LBA43. [Google Scholar]
- 93.Garon EB, Rizvi NA, Hui R, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med. 2015;372:2018–2028. doi: 10.1056/NEJMoa1501824. [DOI] [PubMed] [Google Scholar]
- 94.Soria JC, Cruz C, Bahleda R, et al. Clinical activity, safety and biomarkers of PD-L1 blockade in non-small cell lung cancer (NSCLC): Additional analysis from a clinical study of the engineered antibody MPDL3280A (anti-PD-L1) Eur J Cancer. 2013;49(suppl 2):3408a. [Google Scholar]
- 95.Horn L, Spigel DR., Gettinger SN, et al. Clinical activity, safety and predictive biomarkers of the engineered antibody MPDL3280A (anti-PD-L1) in non-small cell lung cancer (NSCLC): Update from a phase Ia study. J Clin Oncol. 2015;33(suppl):8029a. [Google Scholar]
- 96.FDA Grants Breakthrough Therapy Designation for Genentech’s Investigational Cancer Immunotherapy MPDL3280A (anti-PDL1) in Non-Small Cell Lung Cancer. Available at http://www.gene.com/media/press-releases/14583/2015-02-01/fda-grants-breakthrough-therapy-designat. Accessed September 10, 2015.
- 97.Merck Receives FDA Breakthrough Therapy Designation for KEYTRUDA® (pembrolizumab) in Advanced Non-Small Cell Lung Cancer. Available at http://www.mercknewsroom.com/news-release/oncology-newsroom/merck-receives-fda-breakthrough-therapy-designation-keytruda-pembroli. Accessed March 10, 2015.
- 98.FDA Approves Nivolumab for the Treatment of Metastatic Squamous Non-small Cell Lung Cancer. Available at http://lungdiseasenews.com/2015/03/09/fda-approves-nivolumab-for-the-treatment-of-metastatic-squamous-non-small-cell-lung-cancer/ Accessed March 10, 2015.
- 99.Keedy VL, Temin S, Somerfield MR, et al. American Society of Clinical Oncology provisional clinical opinion: Epidermal growth factor receptor (EGFR) Mutation testing for patients with advanced non-small-cell lung cancer considering first-line EGFR tyrosine kinase inhibitor therapy. J Clin Oncol. 2011;29:2121–2127. doi: 10.1200/JCO.2010.31.8923. [DOI] [PubMed] [Google Scholar]
- 100.Buettner R, Wolf J, Thomas RK. Lessons learned from lung cancer genomics: The emerging concept of individualized diagnostics and treatment. J Clin Oncol. 2013;31:1858–1865. doi: 10.1200/JCO.2012.45.9867. [DOI] [PubMed] [Google Scholar]
- 101.Loong HH, Ma BB, Chan AT. Update in antiepidermal growth factor receptor therapy in the management of metastatic colorectal cancer. J Oncol. 2009;2009:967920. doi: 10.1155/2009/967920. [DOI] [PMC free article] [PubMed] [Google Scholar]