Abstract
Objective
Women of low socioeconomic status (SES) diagnosed with early stage breast cancer experience decision-making, treatment and outcome disparities. Evidence suggests that decision aids can benefit underserved patients, when tailored to their needs. Our aim was to develop and test the usability, acceptability and accessibility of a pictorial encounter decision aid targeted at women of low SES diagnosed with early stage breast cancer.
Design
Community-based participatory research (CBPR) using think-aloud protocols (phases 1 and 2) and semistructured interviews (phase 3).
Setting
Underserved community settings (eg, knitting groups, bingo halls, senior centres) and breast clinics.
Participants
In phase 1, we recruited a convenience sample of clinicians and academics. In phase 2, we targeted women over 40 years of age, of low SES, regardless of breast cancer history, and in phase 3, women of low SES, recently diagnosed with breast cancer.
Intervention
The pictorial encounter decision aid was derived from an evidence-based table comparing treatment options for breast cancer (http://www.optiongrid.org).
Outcome measures
We assessed the usability, acceptability and accessibility of the pictorial decision aid prototypes using the think-aloud protocol and semistructured interviews.
Results
After initial testing of the first prototype with 18 academics and health professionals, new versions were developed and tested with 53 lay individuals in community settings. Usability was high. In response to feedback indicating that the use of cartoon characters was considered insensitive, a picture-only version was developed and tested with 23 lay people in phase 2, and 10 target users in phase 3.
Conclusions and relevance
Using CBPR methods and iterative user testing cycles improved usability and accessibility, and led to the development of the Picture Option Grid, entirely guided by multiple stakeholder feedback. All women of low SES recently diagnosed with early stage breast cancer found the Picture Option Grid usable, acceptable and accessible.
Keywords: decision support techniques, breast cancer disparities, pictorial superiority, Low socioeconomic status, encounter decision aids, usability
Strengths and limitations of this study.
Community-based participatory approach to developing a pictorial encounter decision aid.
Engagement of a variety of key stakeholders in iterative testing cycles.
New prototype development entirely guided by user feedback.
Lack of diversity of phase 3 participants.
Comparison difficulties generated by iterative development and testing processes.
Introduction
Breast cancer is the most commonly diagnosed malignancy and second leading cause of death in women.1 2 Despite improvements in breast cancer survival, disparities in treatment, decision-making, health outcomes and mortality persist.3–6 Women of low socioeconomic status (SES) are more likely to undergo mastectomy, to receive suboptimal care, to play a passive role in treatment decision-making and to experience higher mortality, compared with women of higher SES.3 7–11 They also report poorer knowledge, poorer doctor–patient communication, higher decision regret and tend to have lower health literacy.5 9 10 12 Communicating complex health issues, clinical equipoise and promoting patient engagement in treatment decisions is particularly complex and challenging in women of low SES and low health literacy.12 Is it possible to overcome the challenges of low health literacy and the lack of patient engagement in this group by designing decision aids that rely on images as well as simple words, targeted at women of low SES diagnosed with early stage breast cancer?
According to the Institute of Medicine, patient participation in decision-making should be promoted to improve the quality of healthcare.13 In the context of early stage breast cancer (stages I to IIIA), evidence confirms equivalent survival between mastectomy and breast conserving surgery (BCS), thus warranting patient involvement in treatment decision-making.14–17 Decision aids have been developed to promote and support patients’ involvement in preference sensitive healthcare decisions, where there is no single best healthcare option available and several options with known harms and benefits are being considered. Decision aids have been shown to influence treatment decisions, increase BCS uptake, reduce decisional conflict, increase knowledge and satisfaction with the decision-making process, and improve quality of life.18–20 Recent systematic review evidence indicates that shared decision-making is beneficial to underserved patients, especially when decision aids are tailored to their needs.21 Unfortunately, most decision aids for breast cancer have overlooked the needs of women of low SES and low literacy. For the purpose of this study, and consistent with previous literature, we define low SES according to insurance status, median household income and highest educational attainment.22 23 Among people of low SES, many will have low literacy and limited health literacy.24 25
Underserved patients may prefer and benefit more from shorter paper-based interventions used in the clinical encounter (also called encounter decision aids), compared with more complex, digital interventions, which require higher levels of literacy and numeracy, and are more difficult to embed in clinic visits.26 There is evidence to confirm that encounter decision aids create meaningful conversations about essential trade-offs between available options and increase patient knowledge and patient participation in decision-making with a variable effect on choice and adherence to treatment.27–30 It has also been hypothesised that encounter decision aids may overcome current barriers to decision aid implementation.31 Encounter decision aids such as Option Grids have been shown to increase patients’ knowledge and shared decision-making without lengthening the consultation.27 31 32 The usability, acceptability and accessibility of encounter decision aids in patients of low SES and low literacy have never been evaluated.
Pictorial superiority is defined as the tendency to remember concrete items more easily when presented as pictures rather than words.33 Pictures are also known to facilitate conceptual processing and to demand less cognitive effort than words.34 35 There is evidence of visual literacy in people of lower textual literacy and research confirming that the use of pictures in people of low literacy promotes understanding, health information recall and compliance.36 37 Pictorial encounter decision aids that are adapted to women of low SES are more likely to benefit them and may in turn reduce healthcare disparities.21 Our aim was to develop and test the usability, acceptability and accessibility of a pictorial encounter decision aid targeted at women of low SES diagnosed with early stage breast cancer.
Methods
We used a community-based participatory research (CBPR) approach.38–40 CBPR requires partnership and shared responsibility among patients, clinicians, nurses, administrators and other community stakeholders, to maximise the applicability, usability and implementation of the findings in community settings.38 The study was divided in three phases: (1) prototype development and initial testing with health professionals and academics, (2) iterative prototype testing in underserved community settings and (3) final prototype (Picture Option Grid) testing with target users.
Setting and participants
In phase 1, we recruited a convenience sample of relevant health professionals, community stakeholders and academics with expertise in breast cancer and shared decision-making. They were approached and interviewed at their workplace. In phase 2, participants were recruited in urban and rural community settings in the Upper Valley area in New Hampshire, USA. We primarily targeted women over 40 years of age, of lower educational attainment and SES, regardless of breast cancer history. We also invited men and younger women. Participants were primarily approached in urban and rural community settings serving low SES populations: knitting groups, bingo halls, senior centres, community dinners, cafes, bible groups and community health clinics. For the purpose of phase 2, we inferred low SES according to the community settings where data collection took place: low income, underserved rural and urban area. We did not collect information about the insurance status, education and household income of the participants. In phase 3, a purposive sample of women of low SES diagnosed with early stage breast cancer (stages I to IIIA) was identified by social workers and breast surgeons at a large cancer centre in a rural area (Lebanon, New Hampshire, USA), and by primary care physicians at a primary care healthcare centre serving a diverse, underserved population in an urban area (Chelsea, Massachusetts, USA). We used insurance status and highest educational attainment to determine women's SES. They were interviewed over the phone or met with the researcher at the breast clinic. The phase 3 interviews were part of a broader pilot study of the acceptability and feasibility of several encounter decision aids, reported separately (Alam S, Elwyn G, Percac Lima S, et al. Assessing the acceptability and feasibility of encounter decision aids targeted at patients of low socioeconomic status diagnosed with early stage breast cancer. Under review. 2015). For the purpose of this study, we are only reporting results associated with the Picture Option Grid. All think-aloud protocols and interviews were conducted by trained health service researchers with expertise in interviewing techniques and CBPR (M-AD, SA and SWG).
Data collection
In phase 1, a convenience sample of health professionals and academics were asked to provide feedback on the layout, images and textual content of the initial pictorial encounter decision aid prototypes. They were contacted via email or approached directly in the workplace, and asked to review the prototypes and provide feedback in a one-to-one or group meeting, which took place in the authors’ research building or in the neighbouring hospital. In phase 2, using iterative cycles of think-aloud interviews, subsequent versions of the pictorial encounter decision aid were piloted in community settings.41–43 The think-aloud protocol was used, and required participants to communicate their thoughts as they used the encounter decision aids, and provide insight into the usability of the interventions and impact on cognition and emotions. Each participant was approached in community settings and asked whether they would spend 10–15 min looking at the pictorial decision aid prototype(s) and sharing their thoughts about the design, layout, content, usability and acceptability of each prototype shown. In phase 3, a purposive sample of women who had been diagnosed with early stage breast cancer in the past 5 years was selected by health professionals at participating clinics (Lebanon, New Hampshire, USA; and Boston, Massachusetts, USA). All women were sent an information sheet and contacted by a researcher (SA) on the phone, a week after receiving the information sheet. They were given a choice of taking part in a telephone or face-to-face interview, scheduled on the phone. All interviews were audio-recorded. All women provided written consent prior to the telephone or face-to-face interview, and were sent a copy of the pictorial encounter decision aid. During the interview, they were asked to review the pictorial encounter decision aid with the researcher. The interview schedule consisted of nine open-ended questions and related probes, examining women's reactions to the pictorial encounter decision aid, usability, acceptability and accessibility of the content and layout, appearance of the tool and understanding of the pictures and icon arrays portraying the risk of cancer recurrence and reincision (see online supplementary file 1). The questions also assessed the picture Option Grid's acceptability in the clinic visit, with the breast surgeons, and feasibility of using it routinely with other patients. The interview guide was derived from piloted and published materials used in previous studies assessing the usability and acceptability of patient decision aids.44 Interviews were conducted until data saturation was reached. Data (across all phases) were collected between January and August 2015.
Data analysis
Data collected in phases 1 and 2 were analysed using a thematic analysis. For data collected in phase 3, we used a two-step thematic analysis derived from descriptive phenomenology, assisted by the computer software ATLAS–ti.45–47 First, the transcripts were coded to identify all elements that pertained to the usability, acceptability and accessibility of the intervention. In a second and more detailed analysis, the interview transcripts were coded according to all the themes discussed in the interviews, including spontaneously emerging themes. Similar codes were merged and subsequently grouped into families of codes and networks. In order to ensure reliability of coding and to agree on the themes and family of codes, two researchers (M-AD and SA) independently coded all transcripts. Discrepancies among raters were discussed until agreement was reached.
Results
Phase 1: prototype development and preliminary testing
The pictorial encounter decision aid prototypes were derived from the Option Grid for early stage breast cancer and used the same evidence (see figure 1). The latter is a one-page, evidence-based summary of available options presented in a tabular format, listing the trade-offs or frequently asked questions that patients normally consider when making treatment decisions for early stage breast cancer (http://www.optiongrid.org). It was iteratively developed with patients and clinicians. The Picture Option Grid uses the same evidence, tabular format and integrates images that illustrate each answer to nine frequently asked questions (eg, Will cancer come back in the breast? What is removed in the breast?). In phase 1, an illustrator was commissioned to develop a pictorial version of the Option Grid, using comic strips of a patient and clinician discussing options and providing answers to each frequently asked question. The rationale for developing a pictorial intervention was based on extensive evidence of pictorial superiority in the general population, and especially in people of lower textual literacy.34–37 Two prototypes with comic strips (a black and white prototype: V.A1.0, and a colour version: V.A1.1) were initially developed and tested with a convenience sample of 18 researchers and clinicians, with expertise in shared decision-making and early stage breast cancer. All 18 researchers and clinicians who were approached agreed to participate. They unanimously preferred the black and white prototype (see figure 2). The colour version was therefore abandoned to test the black and white comic strip version (V.A2.0) in underserved community settings.
Figure 1.
Option Grid for early stage breast cancer.
Figure 2.
Comic strip prototype development–phases 1 and 2 (frequently asked question 1 only).
Phase 2: prototype testing in underserved community settings
We approached 59 people and recruited 53 in three rounds of think-aloud interviews, over a period of 16 weeks. In the first round, prototype V.A2.0 (see figure 2) was tested with 22 participants. The majority of participants liked the clean, simple layout and design of the prototype. They felt that images and icon arrays representing outcome probabilities were very effective at conveying complex medical information. Although usability and acceptability of the intervention were high, multiple revisions were made: expressions and attitudes of the doctor and patient characters, textual content, overall layout, images included in the thought bubbles and font size (see figure 2). For example, participants felt that the expressions of the patient character needed to be consistent across the lumpectomy and mastectomy columns, to avoid biases. The content of the thought bubbles was revised to be more representative of everyday life in the communities we visited (eg, represent a woman watching TV instead of sitting on a sofa with a cup of coffee). The images of the breast were revised to more realistically represent the anatomy of a 50-year-old woman. V.A3.0 was created to incorporate those revisions, and tested with eight participants.
The use of images was not considered patronising. It was perceived as one of the most valuable features of the prototype. However, 3 out of 22 people disliked the cartoon-like appearance of the doctor and patient characters. They found it insensitive and inappropriate given the clinical context of breast cancer surgery, and anxiety and distress typically associated with a cancer diagnosis. Consequently, in addition to V.A3.0 comic strip, we developed a new prototype, the Picture Option Grid, which included images and text that did not portray a doctor and patient as cartoon characters.
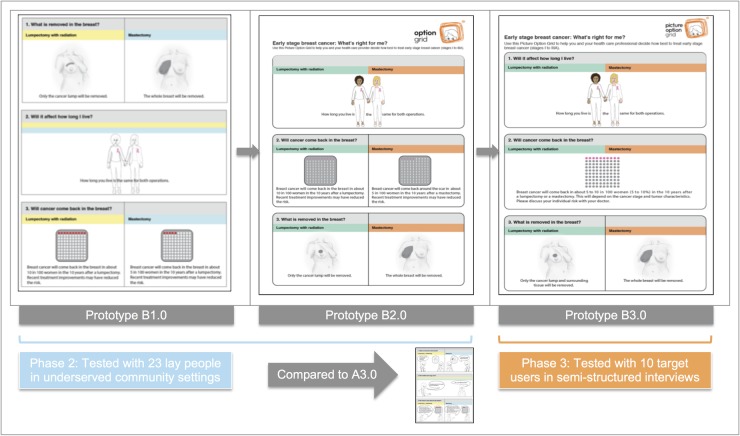
In round 3, the Picture Option Grid (V.B1.0 and V.B2.0) was tested with 23 participants, and compared with V.A3.0 of the comic strip prototype (see figure 3). Minor changes were made to the Picture Option Grid to create V.B3.0. The majority of participants preferred the Picture Option Grid. This version was therefore tested with target users in the next phase of this study.
Figure 3.
Picture Option Grid development–phases 2 and 3 (page 1 only).
Phase 3: Picture Option Grid testing with target users
We approached 25 women and recruited 10 women who had been diagnosed with early stage breast cancer in the past 5 years. Interviews lasted between 18 and 48 min (33.46 min in average). Six interviews were conducted on the phone and four were conducted face to face. Eight women attended the interview alone and two were accompanied by a close relative (partner/family member). The mean age was 56.8. Demographic characteristics of the participants are summarised in table 1. The majority of patients reviewed the Picture Option Grid content in 5 min or less, with few patients spending up to 15 min. The following three themes emerged, and are summarised in table 2: (1) benefits of the Picture Option Grid, (2) feasibility and acceptability of the Picture Option Grid, (3) improving the Picture Option Grid.
Table 1.
Demographic characteristics of phase 3 participants (n=10)
| Characteristics | Categories | |
|---|---|---|
| Age | Mean 56.8; range 31–75 | |
| Breast cancer stage | Stage 1 | 4 |
| Stage 2 | 3 | |
| Stage 3 | 3 | |
| Ethnicity | Hispanic or Latino | 1 |
| Not Hispanic or Latino | 9 | |
| Race | Caucasian | 10 |
| Highest educational attainment | Graduate school | 1 |
| Some college or technical school | 2 | |
| High school graduate | 2 | |
| Some high school | 5 | |
| Health insurance coverage | Public insurance | 10 |
| Surgery type | Lumpectomy | 7 |
| Mastectomy | 3 |
Table 2.
Themes identified in phase 3 interviews
| Themes | Subthemes |
|---|---|
| Benefits of the Picture Option Grid | Pictorial superiority Promotes engagement in decision-making Preparing for upcoming treatments |
| Acceptability and feasibility of the Picture Option Grid | Before or during the consultation Beneficial for all |
| Improving the Picture Option Grid | – |
Benefits of the Picture Option Grid
Nine out of 10 participants highlighted the benefits of pictures in facilitating understanding and information processing. What those participants described in their own words is also known as pictorial superiority. Participants felt that the pictures simplified and clarified the textual content and layout, were more explanatory than words alone, and easier to understand. Pictures accurately conveyed important and detailed information while simplifying information processing for the patient.
I sometimes think when people come in and they have someone talking to them, they don’t always hear everything they say, and I think seeing a visual sometimes is more helpful. It will make you understand more what’s going on. (Patient, 75, stage 3 breast cancer, mastectomy)
And sometimes when people explain things it sounds different but to see the pictures and to have an idea of what actually was happening I think would help a lot of people. (Patient, 60, stage 3 breast cancer, mastectomy)
They also reported that the benefits of the pictures, and of the Picture Option Grid, were even greater when patients were anxious and emotional, as a result of a recent cancer diagnosis, and unable to process information rationally and efficiently.
I just couldn’t grasp things like I normally did. Partly from having had two kind of big surgeries within two weeks and a lot of anesthesia, partly from adjusting to diagnosis, your stress level about it kind of slows all that down. So the easier it is to look at and take in that information, the more they’re going to get out of it at that time. (Patient, 56, stage 1 breast cancer, lumpectomy)
Further, six participants found the icon arrays representing the risk of cancer recurrence helpful in understanding and clarifying risks associated with each treatment option.
Well the second one underneath the two girls…that one was good for the percentage stuff. (Patient, 74, stage 2A breast cancer, lumpectomy)
Seven participants considered that another benefit of the Picture Option Grid was to promote patient engagement in decision-making. The Picture Option Grid was perceived to facilitate a discussion between the patient and surgeon, to help patients formulate and ask questions, improve confidence, and clarify their preferences about available treatment options. Participants also felt that the frequently asked questions included in the Picture Option Grid encompassed all the questions and concerns that they had at the time, when making this important treatment decision.
It leaves room for you to ask questions. I mean it puts things into your—into perspective for you to understand more and to be more comfortable asking your doctor, I think. (Patient, 68, stage 1B breast cancer, lumpectomy)
In addition to promoting patient engagement in decision-making, three women felt that the Picture Option Grid could potentially change the conversation and interaction occurring between the patient and health professional, empowering women to discuss what truly mattered to them.
Finally, nine participants considered that another major benefit of the Picture Option Grid was to prepare women for the upcoming treatments, know what to expect and make a treatment decision that is informed by the perceived impact that each treatment will have on them, their body, their lifestyle and quality of life. Six women felt that the Picture Option Grid provided a detailed, precise and realistic portrayal of breast cancer treatments.
It’s like in the book that I have, it did talk about the radiation but it didn’t have pictures, like this has, to show what actually [happens]… (Patient, 75, stage 3 breast cancer, mastectomy)
With the graphics of the mastectomy, I think that’s a great graphic to have there. I mean, that was one of those things I said, well, I want to see what it would look like if you do this and what it would look like if I did that, to give me an idea at that time. (Patient, 56, stage 1 breast cancer, lumpectomy)
They felt that the pictures would have prepared them for the treatment and its aftermath, and would have relieved some of the fears of the unknown, and concerns about the consequences of treatment (appearance of the breast after surgery, radiation, chemotherapy, ability to resume usual activities) that several patients had after their cancer diagnosis.
I mean that, whether people are aware or not, it kind of gives you a little bit of familiarity with the unknown that’s coming up. And then for the chemo picture, you’ve got a picture of someone in the chair with the pump and the IV. It just kind of gives you an idea, puts you there, you know. (Patient, 56, stage 1 breast cancer, lumpectomy)
In all the pages, it shows that you either take part of your breast or all of your breast, then it shows you how long it takes, then it shows you the radiation, so I know what’s coming…that was my fear, what is coming. (Patient, 74, stage 2A breast cancer, lumpectomy)
One participant explained that using the Picture Option Grid would have alleviated some of her fears, whereas the book that had been provided by the hospital had made her more anxious.
Acceptability and feasibility of the Picture Option Grid
All women felt that the Picture Option Grid was very acceptable and would benefit a wide range of women diagnosed with early stage breast cancer, irrespective of their literacy levels and SES. All women liked the pictures, the overall design, the layout of the tool and the colour scheme, which was described as soothing and calming by one of the participants. All participants stated that they would wholeheartedly recommend the Picture Option Grid to other newly diagnosed patients with breast cancer.
I think this is a great tool, and I hope people get them soon. (Patient, 56, stage 2 breast cancer, lumpectomy)
Given the emotional context of the cancer diagnosis and diversity of people affected, several participants felt that the simplicity and clarity of the content, pictures and layout were particularly valuable, and enhanced the intervention's acceptability, accessibility and usability, for all patients facing this complex treatment decision.
Some people don’t like to sit and read stuff and it’s easier with the picture grid to go through everything. (Patient, 60, stage 3 breast cancer, lumpectomy)
Seven women felt that offering the Picture Option Grid routinely was feasible and would be particularly beneficial if provided prior to the surgical consultation, mailed to patients in advance, immediately after the biopsy results or given to patients in the waiting room, before the visit.
I’d like to have something like this in the mail before I go and see my surgeon. (Patient, 74, stage 2 breast cancer, lumpectomy)
I’d have to have a few minutes to read through it so I could come up with questions. (Patient, 60, stage 3 breast cancer, lumpectomy)
They also felt that it would be very helpful to use the Picture Option Grid in the consultation, as a reference, to guide their questions and discussions with the surgeon.
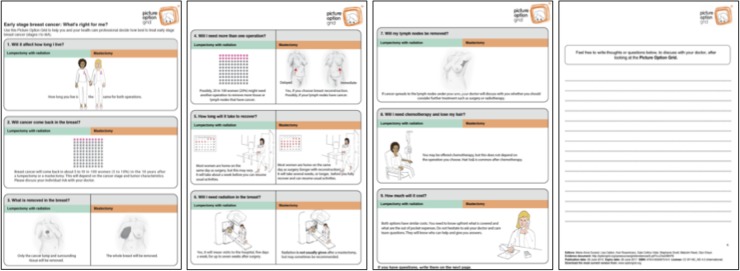
Improving the Picture Option Grid
Seven women suggested improvements to the content and format of the Picture Option Grid. Two participants suggested specifying that surrounding tissue (as well as the cancer lump) will be removed as part of a lumpectomy. Other participants suggested reordering the frequently asked questions (n=1), brightening the colours of the pictures (n=1), providing more information about chemotherapy and hair loss (n=1), and adding a page at the end where patients can write questions and other thoughts (n=1). Most suggested changes were made to create the Picture Option Grid V.B4.0 (see figure 4).
Figure 4.
Picture Option Grid—V.B4.0.
Discussion
The study findings suggest that a CBPR approach, involving iterative design and testing cycles with multiple stakeholders (health professionals, academics, lay people of low SES and target users) maximised the usability and acceptability of the intervention, leading to the development of a new, and more acceptable prototype. Community testing with women of low SES significantly shaped and redirected the design and content of the intervention, to abandon the doctor/patient comic strips and create a version that was most acceptable and usable to both lay people (who were also potential users) and women of low SES recently diagnosed with early stage breast cancer. The comments received in community settings mirrored those provided by clinicians, academics and women of low SES diagnosed with breast cancer. The new prototype (Picture Option Grid) was deemed most acceptable, accessible and feasible in the clinic visit. Most participants highlighted the benefits of integrating simple, yet detailed pictures that clarified information, facilitated understanding and helped patients prepare for the upcoming treatments while engaging in an informed discussion about surgery options with their surgeon.
The strengths of the study were the iterative CBPR approach used to collect and integrate feedback from a variety of stakeholders in several cycles of design and testing. This study is innovative in following a CBPR approach that targeted both experts (n=18), lay people in underserved community settings (n=53), and target users: women of low SES who have been recently diagnosed with early stage breast cancer (n=10). As far as can be determined, very few studies have integrated design and testing cycles that included both the lay community (who may become target users), experts and supporters (academics and health professionals) as well as patients who have faced the decision addressed by the decision aid.48 49 A limitation of the study was the lack of diversity of phase 3 participants (Caucasian). Another potential weakness was the comparison difficulties generated by the iterative approach of the development and testing processes.
The International Patient Decision Aids Standards (IPDAS) state that decision aids should be developed with regular patient and clinician involvement.50 51 However, practical guidance and best practice for user-centered design applied to the development of patient decision aid are scarce and lack detail.49 Only half of patient decision aids included in the 2014 Cochrane review of patient decision aids included patients and potential users in the development process.48 52 User-centered or human-centered design principles target potential users in iterative cycles of testing that are conducted early and often. The CBPR approach we used followed the same principles and demonstrated the value of involving a variety of stakeholders (including potential users and those who support them: partners, family members) in the very early stages of development, and early enough to develop a new version of the prototype that addressed potential users’ concerns, and maximises usability and acceptability.
In the context of breast cancer, only 1 out of 11 available decision aids for early stage breast cancer was designed to address the needs of underserved patients.19 20 53 The computerised decision support system developed by Jibaja-Weiss et al54 targeted multiethnic women of low health literacy diagnosed with early stage breast cancer. The decision aid included soap opera episodes and interactive learning modules. Iterative cycles of user testing with patients and health professionals were seemingly not part of the development process.54 Consistent with the present study, it was usable and acceptable to women of low literacy. The time commitment required to use the intervention was high; from 1 to 2 h. When evaluated in a randomised controlled trial, the decision aid was shown to improve knowledge, and increased mastectomy uptake compared with the control group.53 The intervention had no effect on satisfaction with the surgical decision or the decision-making process and proved difficult to incorporate in routine clinical practice. Given the study did not measure decision quality and did not show an effect on the decision-making process, it is difficult to determine whether the higher uptake of mastectomy was aligned with the patient's values and preferences or attributable to other factors. Further research is needed to determine whether a pictorial decision aid can improve decision quality, reduce disparities in decision-making and treatment that affects women of low SES, and be successfully embedded in routine clinical care. Next steps will aim to determine the effectiveness of the Picture Option Grid encounter decision aids in all women, and differentially by SES, in order to infer its effect on disparities in decision quality and treatment that disproportionately burden women of low SES.
Conclusions
CBPR was successfully used to develop and test a pictorial encounter decision aid for underserved patients with breast cancer. Consistent with human-centered design principles, a CBPR approach integrated comments from community members (and potential users), experts, health professionals, other stakeholders and target users, considering each contribution as equally valuable, thereby improving the usability and acceptability of the intervention across all potential users. The Picture Option Grid that was developed as a result of iterative testing cycles in community settings and breast clinics was considered beneficial in facilitating information processing and understanding, while preparing patients for the upcoming treatments and promoting patient engagement in the clinic visit. A pictorial encounter decision aid that is usable and acceptable to women of low SES may overcome current barriers to patient engagement affecting underserved women, potentially addressing disparities in breast cancer treatment and decision-making.
Acknowledgments
The authors would like to thank all people who have agreed to participate in phases 1 and 2, and all women who agreed to take part in the semistructured interviews in phase 3. They also want to thank all members of the Preference Lab at Dartmouth College, Dr Vidal, Dr Rosenkrantz, Dr Angeles, Dr Barth and Dr Jarvis (Dartmouth-Hitchcock Medical Center) for their insightful feedback on the content and design of the comic strip prototype and Picture Option Grid. They would also like to thank Sanja Percac-Lima, Ellen Curri, Rachel Panicker and Rebecca Lach for their help with recruitment and data collection.
Footnotes
Contributors: M-AD planned and designed the study, and conceptualised the pictorial encounter decision aid. SA, SWG and M-AD collected data in community settings. SA conducted all semistructured interviews. M-AD and SA analysed all data. GE provided advice and guidance on the design, data collection and analysis. M-AD drafted the manuscript. All authors contributed to writing, and approved the final draft of the manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Ethics approval: Phases 1 and 2 of the study received ethical approval from Dartmouth College Committee for the Protection of Human Subjects (CPHS) on 19 December 2014 (STUDY00028541). Phase 3 of the study received ethical approval from Dartmouth CPHS on 22 April 2015 (MOD00001820) and from Massachusetts General Hospital on 1 April.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.American Cancer Society. What are the key statistics about breast cancer? 2015 (cited 25 March 2015). http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-key-statistics
- 2.Donepudi MS, Kondapalli K, Amos SJ et al. Breast cancer statistics and markers. J Cancer Res Ther 2014;10:506–11. 10.4103/0973-1482.137927 [DOI] [PubMed] [Google Scholar]
- 3.Baquet CR, Commiskey P. Socioeconomic factors and breast carcinoma in multicultural women. Cancer 2000;88(5 Suppl):1256–64. [DOI] [PubMed] [Google Scholar]
- 4.Bradley CJ, Given CW, Roberts C. Race, socioeconomic status, and breast cancer treatment and survival. J Natl Cancer Inst 2002;94:490–6. 10.1093/jnci/94.7.490 [DOI] [PubMed] [Google Scholar]
- 5.Hurd TC, James T, Foster JM. Factors that affect breast cancer treatment: underserved and minority populations. Surg Oncol Clin N Am 2005;14:119–30, vii. 10.1016/j.soc.2004.08.001 [DOI] [PubMed] [Google Scholar]
- 6.Wheeler SB, Reeder-Hayes KE, Carey LA. Disparities in breast cancer treatment and outcomes: biological, social, and health system determinants and opportunities for research. Oncologist 2013;18:986–93. 10.1634/theoncologist.2013-0243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coburn N, Fulton J, Pearlman DN et al. Treatment variation by insurance status for breast cancer patients. Breast J 2008;14:128–34. 10.1111/j.1524-4741.2007.00542.x [DOI] [PubMed] [Google Scholar]
- 8.Hiotis K, Ye W, Sposto R et al. Predictors of breast conservation therapy: a statistical analysis of 29,000 patients: a statistical analysis of 29,000 patients. J Surg Res 2003;114:250 10.1016/j.jss.2003.08.161 [DOI] [Google Scholar]
- 9.Mac Bride MB, Neal L, Dilaveri CA et al. Factors associated with surgical decision making in women with early-stage breast cancer: a literature review. J Womens Health (Larchmt) 2013;22:236–42. 10.1089/jwh.2012.3969 [DOI] [PubMed] [Google Scholar]
- 10.Polacek GN, Ramos MC, Ferrer RL. Breast cancer disparities and decision-making among U.S. women. Patient Educ Couns 2007;65:158–65. 10.1016/j.pec.2006.06.003 [DOI] [PubMed] [Google Scholar]
- 11.Voti L, Richardson LC, Reis IM et al. Treatment of local breast carcinoma in Florida: the role of the distance to radiation therapy facilities. Cancer 2006;106:201–7. 10.1002/cncr.21557 [DOI] [PubMed] [Google Scholar]
- 12.McVea KLSP, Minier WC, Palensky JE. Low-income women with early-stage breast cancer: physician and patient decision-making styles. Psychooncology 2001;10:137–46. 10.1002/pon.503 [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington DC: 2001. [PubMed] [Google Scholar]
- 14.Fisher B, Anderson S, Bryant J et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002;347:1233–41. 10.1056/NEJMoa022152 [DOI] [PubMed] [Google Scholar]
- 15.Jatoi I, Proschan MA. Randomized trials of breast-conserving therapy versus mastectomy for primary breast cancer: a pooled analysis of updated results. Am J Clin Oncol 2005;28:289–94. 10.1097/01.coc.0000156922.58631.d7 [DOI] [PubMed] [Google Scholar]
- 16.Morris AD, Morris RD, Wilson JF et al. Breast-conserving therapy vs mastectomy in early-stage breast cancer: a meta-analysis of 10-year survival. Cancer J Sci Am 1997;3:6–12. [PubMed] [Google Scholar]
- 17.Poggi MM, Danforth DN, Sciuto LC et al. Eighteen-year results in the treatment of early breast carcinoma with mastectomy versus breast conservation therapy: the National Cancer Institute Randomized Trial. Cancer 2003;98:697–702. 10.1002/cncr.11580 [DOI] [PubMed] [Google Scholar]
- 18.Collins ED, Moore CP, Clay KF et al. Can women with early-stage breast cancer make an informed decision for mastectomy? J Clin Oncol 2009;27:519–25. 10.1200/JCO.2008.16.6215 [DOI] [PubMed] [Google Scholar]
- 19.Obeidat R, Finnell DS, Lally RM. Decision aids for surgical treatment of early stage breast cancer: a narrative review of the literature. Patient Educ Couns 2011;85:e311–21. 10.1016/j.pec.2011.03.019 [DOI] [PubMed] [Google Scholar]
- 20.Waljee JF, Rogers MA, Alderman AK. Decision aids and breast cancer: do they influence choice for surgery and knowledge of treatment options? J Clin Oncol 2007;25:1067–73. 10.1200/JCO.2006.08.5472 [DOI] [PubMed] [Google Scholar]
- 21.Durand MA, Carpenter L, Dolan H et al. Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. PLoS ONE 2014;9: e94670 10.1371/journal.pone.0094670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr 2006;84:707–16. [DOI] [PubMed] [Google Scholar]
- 23.Marcin JP, Schembri MS, He J et al. A population-based analysis of socioeconomic status and insurance status and their relationship with pediatric trauma hospitalization and mortality rates. Am J Public Health 2003;93:461–6. 10.2105/AJPH.93.3.461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albano JD, Ward E, Jemal A et al. Cancer mortality in the United States by education level and race. J Natl Cancer Inst 2007;99:1384–94. 10.1093/jnci/djm127 [DOI] [PubMed] [Google Scholar]
- 25.Berkman ND, Sheridan SL, Donahue KE et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107. 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- 26.Politi MC, Adsul P, Kuzemchak MD et al. Clinicians’ perceptions of digital vs. paper-based decision support interventions. J Eval Clin Pract 2015;21:175–9. 10.1111/jep.12269 [DOI] [PubMed] [Google Scholar]
- 27.Elwyn G, Pickles T, Edwards A et al. Supporting shared decision making using an Option Grid for osteoarthritis of the knee in an interface musculoskeletal clinic: a stepped wedge trial. Patient Educ Couns 2015;In Press. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 28.Hess EP, Knoedler MA, Shah ND et al. The chest pain choice decision aid: a randomized trial. Circ Cardiovasc Qual Outcomes 2012;5:251–9. 10.1161/CIRCOUTCOMES.111.964791 [DOI] [PubMed] [Google Scholar]
- 29.Montori VM, Shah ND, Pencille LJ et al. Use of a decision aid to improve treatment decisions in osteoporosis: the osteoporosis choice randomized trial. Am J Med 2011;124:549–56. 10.1016/j.amjmed.2011.01.013 [DOI] [PubMed] [Google Scholar]
- 30.Mullan RJ, Montori VM, Shah ND et al. The diabetes mellitus medication choice decision aid: a randomized trial. Arch Intern Med 2009;169:1560–8. 10.1001/archinternmed.2009.293 [DOI] [PubMed] [Google Scholar]
- 31.Lloyd A, Joseph-Williams N, Edwards A et al. Patchy ‘coherence’: using normalization process theory to evaluate a multi-faceted shared decision making implementation program (MAGIC). Implement Sci 2013;8:102 10.1186/1748-5908-8-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fay M, Grande SW, Donnelly K et al. Using Option Grids: steps toward shared decision-making for neonatal circumcision. Patient Educ Couns 2015. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 33.Hockley WE. The picture superiority effect in associative recognition. Mem Cognit. 2008;36:1351–9. 10.3758/MC.36.7.1351 [DOI] [PubMed] [Google Scholar]
- 34.Delp C, Jones J. Communicating information to patients: the use of cartoon illustrations to improve comprehension of instructions. Acad Emerg Med 1996;3:264–70. 10.1111/j.1553-2712.1996.tb03431.x [DOI] [PubMed] [Google Scholar]
- 35.Michielutte R, Bahnson J, Dignan MB et al. The use of illustrations and narrative text style to improve readability of a health education brochure. J Cancer Educ 1992;7:251–60. 10.1080/08858199209528176 [DOI] [PubMed] [Google Scholar]
- 36.Alberto PA, Frederick L, Hughes M et al. Components of visual literacy: teaching logos. Focus Autism Other Dev Disabil 2007;22:234–43. 10.1177/10883576070220040501 [DOI] [Google Scholar]
- 37.Houts PS, Doak CC, Doak LG et al. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns 2006;61:173–90. 10.1016/j.pec.2005.05.004 [DOI] [PubMed] [Google Scholar]
- 38.Grande SW, Faber MJ, Durand MA et al. A classification model of patient engagement methods and assessment of their feasibility in real-world settings. Patient Educ Couns 2014;95:281–7. 10.1016/j.pec.2014.01.016 [DOI] [PubMed] [Google Scholar]
- 39.Israel BA, Schulz AJ, Parker EA et al. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health 1998;19:173–202. 10.1146/annurev.publhealth.19.1.173 [DOI] [PubMed] [Google Scholar]
- 40.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract 2006;7:312–23. 10.1177/1524839906289376 [DOI] [PubMed] [Google Scholar]
- 41.Cotton D, Gresty K. Reflecting on the think-aloud method for evaluating e-learning. Br J Educ Technol 2006;37:45–54. 10.1111/j.1467-8535.2005.00521.x [DOI] [Google Scholar]
- 42.Fonteyn M, Fisher A. Use of think aloud method to study nurses’ reasoning and decision making in clinical practice settings. J Neurosci Nurs 1995;27:124–8. 10.1097/01376517-199504000-00012 [DOI] [PubMed] [Google Scholar]
- 43.Funkesson KH, Anbacken EM, Ek AC. Nurses’ reasoning process during care planning taking pressure ulcer prevention as an example. A think-aloud study. Int J Nurs Stud 2007;44:1109–19. 10.1016/j.ijnurstu.2006.04.016 [DOI] [PubMed] [Google Scholar]
- 44.Durand MA, Boivin J, Elwyn E. Stakeholder field-testing of amnioDex, a person-centered decision support intervention for amniocentesis. The International Journal of Person Centered Medicine 2012;2:7–15. 10.1016/j.ijnurstu.2006.04.016 [DOI] [Google Scholar]
- 45.Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ 2000;320:114–16. 10.1136/bmj.320.7227.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Denzin NK, Lincoln YS. Handbook of qualitative research. 2nd edn Thousand Oaks: Sage Publications, 2000. [Google Scholar]
- 47.Holloway I. Qualitative research in health care. Maidenhead: Open University Press, 2005. [Google Scholar]
- 48.Coulter A, Stilwell D, Kryworuchko J et al. A systematic development process for patient decision aids. BMC Med Inform Decis Mak 2013;13(Suppl 2):S2 10.1186/1472-6947-13-S2-S2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Witteman HO, Dansokho SC, Colquhoun H et al. User-centered design and the development of patient decision aids: protocol for a systematic review. Syst Rev 2015;4:11 10.1186/2046-4053-4-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Elwyn G, O'Connor A, Stacey D et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ 2006;333:417 10.1136/bmj.38926.629329.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Elwyn G, O'Connor AM, Bennett C et al. Assessing the quality of decision support technologies using the International Patient Decision Aid Standards instrument (IPDASi). PLoS ONE 2009;4:e4705 10.1371/journal.pone.0004705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stacey D, Legare F, Col NF et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2014;(1):CD001431 10.1002/14651858.CD001431.pub4 [DOI] [PubMed] [Google Scholar]
- 53.Jibaja-Weiss ML, Volk RJ, Granchi TS et al. Entertainment education for breast cancer surgery decisions: a randomized trial among patients with low health literacy. Patient Educ Couns 2011;84:41–8. 10.1016/j.pec.2010.06.009 [DOI] [PubMed] [Google Scholar]
- 54.Jibaja-Weiss ML, Volk RJ, Granch TS et al. Entertainment education for informed breast cancer treatment decisions in low-literate women: development and initial evaluation of a patient decision aid. J Cancer Educ 2006;21:133–9. 10.1207/s15430154jce2103_8 [DOI] [PubMed] [Google Scholar]