Abstract
Introduction
People from working poor families are at high risk of poor health partly due to limited healthcare access. Health empowerment, a process by which people can gain greater control over the decisions affecting their lives and health through education and motivation, can be an effective way to enhance health, health-related quality of life (HRQOL), health awareness and health-seeking behaviours of these people. A new cohort study will be launched to explore the potential for a Health Empowerment Programme to enable these families by enhancing their health status and modifying their attitudes towards health-related issues. If proven effective, similar empowerment programme models could be tested and further disseminated in collaborations with healthcare providers and policymakers.
Method and analysis
A prospective cohort study with 200 intervention families will be launched and followed up for 5 years. The following inclusion criteria will be used at the time of recruitment: (1) Having at least one working family member; (2) Having at least one child studying in grades 1–3; and (3) Having a monthly household income that is less than 75% of the median monthly household income of Hong Kong families. The Health Empowerment Programme that will be offered to intervention families will comprise four components: health assessment, health literacy, self-care enablement and health ambassador. Their health status, HRQOL, lifestyle and health service utilisation will be assessed and compared with 200 control families with matching characteristics but will not receive the health empowerment intervention.
Ethics and dissemination
This project was approved by the University of Hong Kong—the Hospital Authority Hong Kong West Cluster IRB, Reference number: UW 12-517. The study findings will be disseminated through a series of peer-reviewed publications and conference presentations, as well as a yearly report to the philanthropic funding body–Kerry Group Kuok Foundation (Hong Kong) Limited.
Keywords: PREVENTIVE MEDICINE, PRIMARY CARE, PUBLIC HEALTH
Strengths and limitations of this study.
A prospective health empowerment programme with four components.
Focus on working poor families, a group receiving limited support, for example, financial assistance.
Evaluate the effect of the health empowerment programme on both adults and children in a family.
Apart from the health assessment in which every family must be involved, some intervention families with poor compliance may show little interest in other components of the health empowerment programme.
We will not limit our participants from joining other programmes conducted by other organisations or institutions.
Introduction
Poverty is a worldwide problem that is inextricably related to ill health,1 with poorer individuals having higher mortality rates.2 In addition to limited access to food, clean water and safe shelter, children raised in poverty experience limitations in development and have fewer learning opportunities, all of which may extend into adulthood.3 4 Difficulty in access to healthcare is another common problem among poor families. Payment for healthcare can divert the limited disposable income from other educational and social needs of these families. Thus, it is not surprising that poverty and poor health can become a vicious cycle,5–7 lasting for generations in one family.
The WHO Alma-Ata Declaration in 1978 stated that ‘primary healthcare is the key to health for all’,8 which was re-emphasised as ‘Primary Health Care—Now More than Ever’ in the 2008 WHO World Health Report.9 Primary healthcare starts with self-care to promote health, prevent disease and manage illnesses. Health empowerment, a central component of health promotion and disease prevention, refers to a process through which people can gain greater control over the decisions affecting their lives and health.10 The concept of health empowerment is to educate and enable individuals and families so that they can have the knowledge (health literacy), motivation, self-efficacy, means of action and resources to stay healthy, to self-care and to seek health services appropriately.11 Previous research showed that a successful empowerment programme could enable chronic patients to better cope with their disease by improving their self-image and self-efficacy in maintaining their health.12 Cumulative evidences demonstrated that health empowerment had a beneficial effect on enhancing participants’ well-being and health.13 14 Nevertheless, no similar health empowerment intervention study has been conducted among working poor people to the best of our knowledge.
Hong Kong is recognised as a developed region with a per capita gross domestic product (GDP) of 273 550 Hong Kong Dollar (HKD) (around US$35 120) in 2011. However, it has a high Gini coefficient of 0.537, indicating wide income inequalities.15 In 2012, the Hong Kong Government set up the Commission of Poverty and, for the first time, defined the poverty line—a cut-off line where the families’ monthly household incomes are below that of the Hong Kong median.16 It was estimated that around 1.3 million Hong Kong citizens were living in poverty, representing one-fifth of the whole population, to whom some financial subsidiaries are usually provided.16 However, those whose monthly household incomes are between 50% and 75% of the Hong Kong median monthly household income are often the working poor who suffer from a lot of stress but do not receive much government support.
Tung Chung is a developing satellite residential area located on an outlying island of Hong Kong (figure 1), where access to healthcare services is limited. Before 2013, only one public primary care clinic with three consulting doctors and seven private medical practitioners served all the residents in Tung Chung. The public regional hospital has just been established in 2013, providing primary care, emergency, internal medicine, psychiatric and allied health services. Routine health checks are not provided by public primary care providers and thus not available to residents who cannot afford the cost of private medical care. The combination of poverty and poor healthcare access may greatly impact on the health of these Tung Chung residents.
Figure 1.
Map of Hong Kong showing the location of Tung Chung and location of available healthcare services for Tung Chung residents. According to the 2011 census, around 78 000 residents were living in Tung Chung new town. To satisfy the shelter demands, three public housing estates, Fu Tung Estate, Yat Tung (I) Estate and Yat Tung (II) Estate, have been established to provide more than 13 000 residential units to Tung Chung residents. However, since it is located on the north-western coast of Lantau Island in Hong Kong, a minimum of 45 minutes travelling time using the Mass Transit Railway (MTR) metro system is required for residents to travel to Hong Kong's business centre in Central, other commercial centres or the nearest regional hospital with full medical services (the Princess Margaret Hospital). (The map was drawn using the software R V.3.1.1.).
In this context, Kerry Group Kuok Foundation (Hong Kong) Limited (KGKF) has initiated the Trekkers Family Enhancement Scheme in 2012 that aims to enable working poor families in Tung Chung to develop their full potentials by providing support and opportunities in health, education, employment and environmental harmony. In terms of health support, a Health Empowerment Programme consisting of four inter-related programmes, namely Health Assessment Programme, Health Literacy Programme, Self-care Enablement Programme and Health Ambassador Programme, will be delivered to these Trekkers families.
Aim and objectives
The aims of this study are to investigate, analyse and evaluate the effect of the Health Empowerment Programme on the health, health-related quality of life (HRQOL), lifestyle and health-seeking behaviours among working poor families. The objectives are:
To find out and compare the short-term and long-term changes in the health, health enablement, HRQOL, cardiovascular risk factors, lifestyle, illness rates, health-seeking behaviours and health service utilisation of participants (trekkers) and non-participants of the Health Empowerment Programme.
To find out the effect of participation in one or more components of the Health Empowerment Programme on health, health enablement, HRQOL, cardiovascular risk factors, lifestyle, illness rates, health-seeking behaviours and health service utilisation.
Hypothesis
Individuals participating in the Health Empowerment Programme will have better health, health enablement, HRQOL, lifestyle and health-seeking behaviours, fewer illness rates, health service utilisation and cardiovascular risk factors than non-participants over time.
Individuals participating in one or more components of the Health Empowerment Programme will have better health, health enablement, HRQOL, lifestyle and health-seeking behaviours, fewer illness rates, health service utilisation and cardiovascular risk factors.
Method/design
Study design
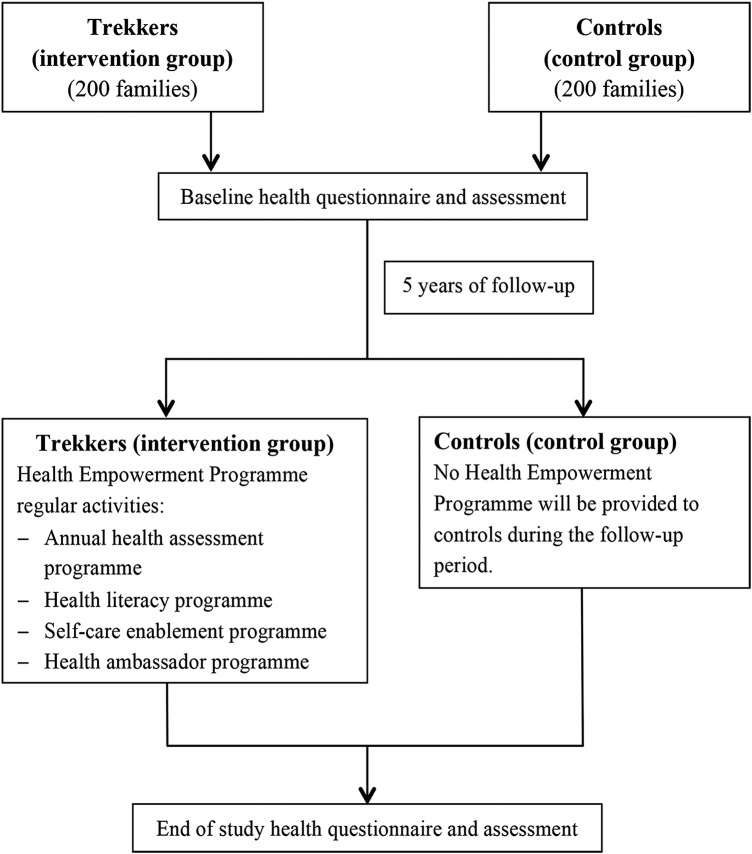
This is a prospective cohort study comparing two groups of working poor nuclear families with young children studying in grades 1–3 at the time of recruitment. Both groups will be followed up for 5 years (figure 2). Families enrolled in the Trekkers Family Enhancement Scheme (referred to as ‘Trekkers families’ or ‘Trekkers family’ in the remainder of the paper) will be offered a comprehensive health assessment every year and different components of the Health Empowerment Programme. To evaluate the effectiveness of the programme, control families with similar sociodemographic backgrounds (referred to as ‘control families’ or ‘control family’ in the remainder of the paper) will be recruited from various Hong Kong subdistricts for comparison. Control families will not be invited to join our Health Empowerment Programme; nevertheless, a comprehensive health assessment will be provided at the beginning and end of the programme for collecting various health variables.
Figure 2.
Cohort study design and participant flows.
Study population and recruitment
All participants from the Trekkers families will be identified from the registration list of the Kerry Group Kuok Foundation (Hong Kong) Limited (KGKF) Trekkers Family Enhancement Scheme. The following inclusion criteria will be used: (1) Participants must be part of a family where all family members are residents in Tung Chung; (2) The family must have at least one family member working full-time or part-time; (3) The family monthly household income does not exceed 75% of Hong Kong's median monthly household income; (4) At least one child is studying in grade 1, 2 or 3 at the time of recruitment; (5) At least one adult family member is willing to participate in the long-term follow-up study; and (6) Only fathers, mothers and children aged 6 years or above will be included in this study.
Control subjects will be identified and recruited with the help of non-government organisations that provide community services in Tung Chung and Kwai Chung (an area with sociodemographic background similar to that of Tung Chung), for example, Neighbourhood Advice Action Council, Hong Kong Sheng Kung Hui, and Hong Kong Outlying Island Women's Association. The following inclusion criteria will be used: (1) Participants must be part of a family, all of whose family members are residents in Hong Kong; (2) The family monthly household income does not exceed 75% of Hong Kong's median monthly household income; (3) At least one child is studying in grade 1, 2 or 3 at the time of recruitment; and (4) Only fathers, mothers and children aged 6 or above will be included in this study. Each control family will receive an HKD 100 (equal to US$13) coupon on completion of the baseline health questionnaire and assessment, and they will receive another HKD 100 at the end of 5 years when they complete the second health questionnaire and assessment as incentives. Trekkers families will not receive any financial incentives.
All adult participants in both groups must provide written consent before participating in this study. Parents or guardians will provide consents for participants under the age of 18 years. Individuals will be excluded if (1) No family members can understand or communicate in Chinese; and (2) Families have adopted children.
Health Empowerment Programme
The Health Empowerment Programme will consist of four inter-related programmes, including Health Assessment, Health Literacy, Self-care Enablement and Health Ambassador Programmes. These programmes share the same objective of nurturing health ambassadors. Except for the Health Assessment Programme in which all trekkers must be involved annually, participation in the Health Literacy Programme, Self-care Enablement Programme and Health Ambassador Programme is on a voluntary base. Participants from the control group will be required to attend two comprehensive health assessments at the beginning and end of this study.
The Health Assessment Programme will screen for common health problems or risk factors for ill health among the participants, so that early intervention can be introduced. Participants will be informed of their individual health risks and problems, and advised on the necessary follow-up measures or lifestyle changes. The assessment will be repeated annually to monitor the progress of the trekkers and provided to controls only at the beginning and end of this study. The ultimate aim of the Health Assessment Programme is to empower these participants by being more aware of their own health status, knowing what they can or need to do to improve their health and having a better understanding on the importance of primary prevention.
The Health Literacy Programme will be delivered in the form of seminars conducted by medical professionals, followed by interactive activities that encourage participants to apply health-related knowledge in real-life scenarios. These seminars aim to improve participants’ knowledge on health and health services in order to promote health, prevent illness, facilitate self-care and optimise the use of health-related community services. Topics will cover a wide range of common health problems including upper respiratory tract infections, common eye problems, mental health problems, and women's and children's health. New topics will be introduced on the basis of health problems found to be prevalent among Trekkers families during their ongoing health assessments. Each year, two to four health seminars will be organised to disseminate health messages and modify their concepts of health. All Trekkers families will be invited to attend the health seminars through text messages, posters and newsletter; in addition, participants with specific health problems will be contacted by telephone and encouraged to attend seminars on relevant topics.
The aim of our Self-care Enablement Programme is to empower participating families to maintain and improve their health, to build up self-efficacy, self-management and help-seeking skills and to generate a spirit of mutual support among families. It will also train leaders to provide long-term and sustainable support for families in Tung Chung. It is developed with established psychological theories, including the resilience model,17 transactional model of stress and coping18 and conceptualisation of self-views,19 to enable families to look after their own health in order to keep them healthy. The programmes, which will focus on physical well-being, psychological health and family harmony, comprise six–eight sessions and will be held in weekly or bi-weekly intervals with each activity lasting for 1–2 hour(s). These will be offered to participants with respective health problems identified from the health assessment or those who are interested in the programmes. Participants and lay leaders who have attended the Self-care Enablement Programme may later be upskilled to become health ambassadors. The programmes will be repeated for different participants for at least 2 years.
The Health Ambassador Programme aims to train up a group of adults recruited from the Trekker families to act as a lay advisor for other families on health issues. Participants who have completed the Health Literacy and Self-care Enablement Programme will be invited to take part in this programme. Two training sessions will be provided to train around 10–20 ‘Health Ambassadors’ in order to equip each ambassador to serve about 10 intervention families.
Evaluation of the effectiveness of the Health Empowerment Programme
Primary outcome
Health enablement measured by the Chinese (Hong Kong) Patient Enablement Instrument (PEI).20 21
Secondary outcomes
HRQOL measured by the Chinese version of 12-item Short-Form Health Survey—the second version (SF-12v2).22–24
Health Status (global health, mental health) measured by Depression Anxiety Stress Scales (DASS).25 26
Lifestyle (smoking, drinking, physical activities, and dietary habits).
Health parameters (eg, blood pressure, body mass index (BMI), lipid profiles, blood glucose and complete blood count only for adults).
Health service utilisation pattern (having a family doctor, self-care, use of public primary care clinics (ie, the general outpatient clinic (GOPC)) and accident and emergency service).
Sample size and rationale for calculation
The sample size is calculated on the basis of expected detection of a Cohen's small effect size difference of 0.3 in the PEI scores between participants and non-participants of health intervention activities among intervention families. A sample size of 176 participants will be required in each group in order to have 80% power and 5% type I error. According to the clustering effect among family members, at least 211 participants (or 70 families) will be required in each group assuming an average of three members in each family and an estimate of intraclass correlation of 0.1. Therefore, the number of required families will be increased to 158 allowing for a 15% annual attrition rate over 5 years of follow-up. We allowed for an approximately 80% participation rate in one or more health intervention activities so as to have a total of 200 intervention families. Control families will be recruited at a ratio of 1:1, compared to intervention families.
Measurement
Participant-reported outcomes and sociodemographics
The 6-item PEI will be used to measure the participant's enablement in coping with illness and life.21 Each item is rated on a 3-point (0, 1, and 2) scale. The sum of each item score gives the final PEI score, with higher scores indicating better enablement. The Chinese version has been shown to be valid and reliable among Chinese patients in primary care.20
The HRQOL will be measured with the Chinese version of SF-12v2.22–24 It consists of 12 items that cover 8 subscales, namely physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE) and mental health (MH). The eight subscale scores can be aggregated into physical component summary (PCS) and mental component summary (MCS).
The Chinese version of the 42-item DASS will be used to isolate and identify any emotional disturbances from depression, anxiety or stress.25 26 It consists of 42 self-reported items, each with a four-point Likert scale asking about the frequency or severity of a negative emotional symptom.
The Global Rating Scale (GRS) will be used to assess a person's global perception of any change in the overall health condition on a seven-point scale (−3, −2, −1, 0, 1, 2 and 3) over the past 6 months.27
The general self-efficacy (GSE) scales will be used to assess optimistic self-beliefs to cope with a variety of difficult demands in life.28–30 It contains 10 items, each item rated on 4 options of ‘not at all true’, ‘hardly true’, ‘moderately true’ and ‘exactly true’.
Sociodemographic information including marital status, education background, occupation and monthly household income will be collected. The knowledge score, consisting of five questions related to the content of individual health literacy talk, will be used to assess participants’ health knowledge. The total count of correct answers will be compared before and after the talks.
Lifestyle
Physical activity will be assessed using the International Physical Activity Questionnaire (IPAQ)—short form.31 32 The IPAQ-short form consists of questions regarding the duration (in minutes) and frequency (days) of walking, moderate-intensity and vigorous-intensity activities. Information on smoking, drinking and illicit substance use will be collected. Dietary habits including frequency of having breakfast, lunch and dinner and frequency of having vegetables, fruit and milk per week will be assessed.
Health parameters
Cardiovascular risks
Body weight and height will be measured with an electronic scale and stadiometer (ZT-150A; Nanjing Jolly IMP & EXP CO, LTD, China), and will be read to the nearest 0.1 kg and 0.1 cm, respectively. Body mass index (BMI) will be calculated as the ratio of body weight (kg) to the square of body height (m2). Waist circumference will be measured with an anthropometric tape 1 inch above the navel at the end of a normal expiration, while hip circumference will be measured at the level of the widest portion of the buttocks. Both parameters will be measured to the nearest 0.5 cm.
Blood pressure (BP) will be measured by an automated blood pressure measurement device (UA-853; A&D Medical; China) on the participant’s right arm (unless not suitable) with a cuff placed at the level of the heart after at least 10 minutes of rest. The mean value of two repeated measurements will be used for data collection.
Fasting venous blood samples for glucose and full lipid profile will be collected from adult participants after overnight fasting for at least 8 hours. Fasting blood glucose will be measured by the hexokinase method. Serum total cholesterol, triglycerides and high-density lipoprotein (HDL)-cholesterol will be measured using enzymatic techniques. Low-density lipoprotein (LDL)-cholesterol will be calculated using the Friedewald equation based on total cholesterol, triglycerides and HDL-cholesterol.33
General health
Lung function will be assessed with spirometry by an experienced pulmonary function technician using the Spirolab III Spirometer (Medical International Research; Italy). Spirometry data (peak expiratory flow rate, forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC)) will be recorded electronically and analysed with Hong Kong's reference values.34 35
Visual acuity will be assessed using the Snellen visual acuity chart (for distant vision) and Rosenbaum hand-held visual acuity chart (for near vision). Ishihara colour vision test plates (concise version—14 plates) will be used to detect for colour vision deficiency.36 A Hirschberg test will be performed on children to detect strabismus.37 Amsler grid test will be used to detect for potential macular degeneration among adults.38
Hearing capacity will be assessed using a pure tone audiogram (PTA) (GSI-18 Portable Screening Audiometer; Grason Stadler; USA) at 500, 1000, 2000 and 4000 Hz. Participants with abnormal hearing thresholds (>25 dB at any frequency) will receive Rinne test and Weber's test for differentiating conductive from sensorineural hearing loss.39
Oral health will be evaluated by trained research nurses for the presence of mucosal, gum, teeth problems or suboptimal oral hygiene.
For participants older than 65 years, a timed up and go (TUG) test will be used to determine the functional mobility and the risk of falls.40
Venous blood samples will be collected for the following tests: renal function test (creatinine and electrolytes), liver function test (total bilirubin, alanine aminotransferase (ALT), aspartate aminotransferase (AST) and alkaline phosphatase), complete blood picture and hepatitis B (HB) surface antigen test.
Mental and cognitive skill
Cognitive skills of children studying in grades 1–3 in the intervention and control groups will be screened by clinical psychologists using the Wechsler Intelligence Scale for Children Fourth Edition—Hong Kong (Short Form) (WISC-IV-HK-SF). This instrument is an individually administered intelligence test for children that has been validated in Hong Kong.41 42 The short form can reduce the assessment time to 25 minutes and the correlation coefficient of WISC-IV-HK-SF is 0.92 compared with the full set of the Wechsler Intelligence Scale.
Behaviour and psychosocial well-being of children studying in grades 1–3 in the intervention and control groups will be assessed with the validated Chinese version of Strengths and Difficulties Questionnaire (SDQ)43 44 and Child Health Questionnaire (CHQ), a generic quality of life measure.45 46 Both questionnaires would be completed by the parents of participating children.
Patient Health Questionnaire (PHQ)—9 will be used to measure depression scales in participants older than 14 years.47 48 The 5-item Abuse Assessment Screen (AAS) questionnaire covering physical, sexual and emotional abuse will be used to screen for intimate partner violence.49 The modified abbreviated mental test (AMT) for Chinese will be used to assess the likelihood of dementia among elderly participants (above 65 years).50
Urinary problems
The presence of lower urinary tract symptoms will be screened with International Prostate Symptom Score (IPSS) Hong Kong version 2.51 52 It contains 7 symptom questions with scores from 1 to 5 (a total of maximum 35 points), and a 6-point (score 1–6) quality of life question. To evaluate the symptoms and impact of urinary incontinence, the International Consultation on Incontinence Questionnaire urinary incontinence short form (ICIQ UI SF) will be used.53 54 It is a short and simple questionnaire that evaluates the level, impact and perceived cause of symptoms of urinary incontinence. It contains four items on the frequency, amount and circumstances of incontinence.
Health service utilisation
Health service utilisation will be assessed using rates of having acute disease in the past month, their frequency of doctor consultation, emergency department attendance or hospital admission, the possession of a family doctor,55 56 their choices of selecting health services and their frequency of having regular body checks.
Data collection
Health assessment
Participant-reported outcomes, sociodemographic data, health parameters, lifestyle and health service utilisation will be collected by an annual telephone health survey or during their scheduled comprehensive health assessment (ie, annually for Trekker families, at baseline and at the end of the study for control families). The telephone surveys will be conducted by trained interviewers at the University of Hong Kong's Social Science Research Centre (SSRC). The comprehensive health assessment including a questionnaire, a physical examination and venesection will be performed by a team of research nurses, trained technicians and research assistants at different assessment centres with strict adherence to the research protocol. Training on questionnaire administration and physical examination technique will be provided to all involved staff members prior to study initiation. Table 1 shows the measurements taken in the comprehensive health assessment for the Health Empowerment Programmes.
Table 1.
Health parameter measurements at baseline and follow-up for intervention and control groups.
| Baseline* |
Follow-up* |
|||
|---|---|---|---|---|
| Intervention | Control | Intervention | Control | |
| 1. Telephone health survey | ||||
| Empowerment, quality of life and well-being† | ||||
| PEI | × | × | × | × |
| SF-12v2 | × | × | × | × |
| DASS | × | × | ||
| GSE | × | × | ||
| GRS | × | × | × | × |
| Socioeconomic status† | ||||
| Marital status | × | × | ||
| Education background | × | × | ||
| Occupation | × | × | ||
| Monthly household income | × | × | × | × |
| Health service utilisation | ||||
| Having a family doctor | × | × | × | × |
| Doctor consultation | × | × | × | × |
| Emergency department attendance and hospital admission | × | × | × | × |
| 2. Clinical assessment | ||||
| Health questionnaire | ||||
| Physical activity (IPAQ-short form) | × | × | × | × |
| Smoking status | × | × | × | × |
| Alcohol consumption | × | × | × | × |
| Illicit substance use | × | × | × | × |
| Medical history | ||||
| History of drug allergy | × | × | × | × |
| Current medication | × | × | × | × |
| Immunisation record | × | × | × | × |
| Previous use of health tests | × | × | × | × |
| Medical history | × | × | × | × |
| Family history of possible hereditary disease | × | × | ||
| Lower urinary tract symptoms (IPSS and ICIQ UI SF)† | × | × | × | × |
| Depression (PHQ-9)‡ | × | × | × | × |
| Domestic violence (AAS-5†/AAS-2§) | × | × | × | × |
| Physical assessments | ||||
| Anthropometric measurement | ||||
| Weight and height | × | × | × | × |
| Waist circumference and hip circumference | × | × | × | × |
| Blood pressure and pulse | × | × | × | × |
| Vision | ||||
| Hyperopia/myopia | × | × | × | × |
| Colour blindness (Ishihara Colour Vision Test) | × | × | ||
| Strabismus (Hirschberg test)§ | × | × | ||
| Macular degeneration (Amsler grid test)† | × | × | × | × |
| Hearing | ||||
| PTA | × | × | × | × |
| Rinne test | × | × | × | × |
| Weber's test | × | × | × | × |
| Oral health | × | × | × | × |
| Spirometry | × | × | × | × |
| Elderly mobility (TUG)¶ | × | × | × | × |
| Cognitive assessments | ||||
| Intellectual ability (WISC-IV-HK-SF)** | × | × | ||
| Behaviour and psychosocial well-being (SDQ and CHQ-50)** | × | × | ||
| Dementia (AMT)¶ | × | × | × | × |
| Laboratory measures† | ||||
| Fasting blood glucose | × | × | × | × |
| Lipid profile (total cholesterol, HDL and LDL cholesterol, triglyceride) | × | × | × | × |
| Liver function (total bilirubin, ALT, AST, alkaline phosphatase) | × | × | × | × |
| Kidney function (urea, creatinine, potassium, sodium) | × | × | × | × |
| HBs antigen | × | × | × | × |
| Haematology profile (WCC, RBC, haemoglobin, PCV, platelets, MCV, MCH, MCHC) | × | × | × | × |
| Differential count (neutrophil, lymphocyte, monocyte, eosinophil, basophil, peripheral blood film) | × | × | × | × |
*The assessments will be carried out annually in the intervention group, but only at baseline and at the end of the study for controls.
†Only apply to participants aged over 18 years.
‡Only apply to participants aged over 14 years.
§Only apply to participants aged under 18 years.
¶Only apply to participants aged over 65 years.
**Only apply to children studying in grades 1–3.
AAS, Abuse Assessment Screen; ALT, alanine aminotransferase; AMT, Abbreviated mental test; AST, aspartate aminotransferase; CHQ, Child Health Questionnaire; DASS, Depression Anxiety Stress Scales; GRS, Global Rating Scales; GSE, General self-efficacy; HDL, high-density lipoprotein; ICIQ UI SF, the International Consultation on Incontinence Questionnaire urinary incontinence short form; IPAQ, International Physical Activity Questionnaire; IPSS, International Prostate Symptom Score; LDL, low-density lipoprotein; MCH, mean cell haemoglobin; MCHC, mean cell haemoglobin concentration; MCV, mean cell volume; PCV, packed cell volume; PEI, patient enablement instrument; PHQ, Patient Health Questionnaire; PTA, Pure tone audiogram; RBC, red blood cell; SDQ, Strengths and Difficulties Questionnaire; SF-12v2, Short-Form Health Survey—the second version; TUG, Timed up and go; WCC, White cell count; WISC-IV-HK-SF, Wechsler Intelligence Scale for Children—Hong Kong (Short Form).
Health Literacy Programme
For the evaluation of the Health Literacy Programme, participants will be invited to complete a knowledge test before and after each health talk session. In addition, the participants will be invited to complete the PEI,20 21 the GRS27 and the satisfaction scale.
Self-care Enablement Programme
Each Self-care Enablement Programme will include several sessions. The immediate, short-term and long-term effects of the programme will be evaluated with the GRS27 and PEI20 21 during the last session, at 3 and 12 months after each programme. The HRQOL will be measured with the Chinese version of SF-12v2.22–24 Details regarding these measurement items are listed in table 2.
Table 2.
Participant-reported outcome measurements used in Self-care Enablement Programme
| Post-programme |
||||
|---|---|---|---|---|
| Immediate effect | Short-term effect | Long-term effect | ||
| Time point | Pre-programme | Immediately after | 3 months after | 12 months after |
| Measurements | SF-12v2 | SF-12v2 PEI Satisfaction scale GRS |
SF-12v2 PEI Satisfaction scale GRS |
SF-12v2 PEI Satisfaction scale GRS |
GRS, Global Rating Scale; PEI, Patient Enablement Instrument; SF-12v2, Short-Form Health Survey—the second version.
Statistical analysis
Descriptive data will be presented as mean±SD or number (percentage), as appropriate. To compare the different outcomes between the Trekkers and control groups, an independent samples t-test or a Mann-Whitney U-test will be used for continuous data, and a χ2 test will be used for categorical data. To compare the changes between baseline and follow-up, paired t-tests or Wilcoxon signed rank tests will be used for continuous data and McNemar's test will be used for categorical variables. Multiple linear regressions will be used to determine the independent effect of participating in health empowerment intervention activities, controlling for clinical and sociodemographic factors, on the PEI scores and changes in the SF-12v2 scores and other secondary outcomes over the time period from baseline to follow-up. All statistical analyses will be performed using the IBM SPSS Windows V.20.0 program. A p-value less than 0.05 will be considered statistically significant.
Discussion
In this study, we assume that our Health Empowerment Programme will be effective in educating and enabling individuals and families to improve their health literacy and to seek health services appropriately. Designed as a participatory-action research where participation of the Trekkers in the different components of the Health Empowerment Programme will be on a voluntary base apart from the Health Assessment Programme, our study may also provide useful information on the acceptability and applicability of our programme in the community setting.57 Uptake of each health empowerment activity will depend on the participants’ willingness, interest, motivation, as well as capacity to use the activity to enhance their health. By allowing voluntary participation in our different empowerment activities, the popularity of each activity and the feedback from the participants will inform the research team on the needs to modify or revise the format and content of the activities to better suit our participants. Moreover, we will not limit the Trekkers to participate in our Health Empowerment Programme only; they may also join other health-related activities available in the community. The total time spent by the Trekkers on health-related activities can be compared to that by the control families who may also join health-related activities in their community freely, and will serve as an indicator of their health awareness.
On the other hand, it can be anticipated that these working poor nuclear families have limited free time to attend many different activities, due to the long working hours and childcare. In order to maximise access to the health assessment and health seminars, we have assembled a professional ambulatory health assessment team, consisting of registered nurses and nursing students, experienced technicians, trained research assistants and clinical or educational psychologists, to provide comprehensive assessments at a clinic in Tung Chung during weekends or late weekday evenings. Discussions on the health problems detected during the health assessment will be conducted over the phone by registered nurses at a time convenient to participants. All the health seminars or self-care enablement programmes will be conducted on Saturday afternoons at various community facilities in Tung Chung. In order to promote participation, posters will be put up in the neighbourhood where most of the Trekkers families reside, and short text messages will be sent to trekkers a few days prior to each activity as a reminder. In addition, targeted participants with specific health problems detected during the ongoing health assessments will be called and invited to join related seminars and self-care enablement activities. Last but not least, we have set up a hotline for participants to discuss their health issues with our registered nurses at their most preferred time.
With the expected widening of the income inequality and the close relationship between poverty and poor health, helping the working poor people by empowering them on health issues, including improving health awareness and health-seeking behaviour, is essential for healthcare services planning and expansion. If this is proven to be effective, similar health empowerment programme care models can be developed and publicised. Studies looking to establish evidence for this Health Empowerment Programme will be of considerable interest to healthcare providers and policy makers.
Acknowledgments
The authors are most grateful to Kerry Group Kuok Foundation (Hong Kong) Limited. Our special thanks go to the Neighborhood Advice-Action Council (NAAC) and Yat Tung (I/II) Estate Property Management, HKFEW Wong Cho Bau School, Project Concern Hong Kong—Yat Tung Estate Dental Clinic for the provision of facilities and other assistance for the Health Literacy, Self-Care Enablement and Health Assessment programmes. The authors received great help from the Hong Kong Sheng Kung Hui Tung Chung Integrated Services (HKSKH), the NAAC, the Hong Kong Outlying Island Women's Association (OIWA), the Tung Chung Safe and Healthy City (TCSHC) and TWGHs Ko Ho Ning Memorial Primary School in the recruitment of comparison families. Our thanks also go to Dr Rainbow TH Ho and Dr. Terri Chan for their expert advice. The hard work of our clinical colleagues (Dr Ben Fong, Ms Anna Lam, Ms Teresa Lau and Mr Lo Kan Ming), research assistants (Ms Charlotte Yu, Mansy Sham) and administrative staff (Mr Nam Tat and Ms Rosanna Tsui) must be acknowledged.
Footnotes
Contributors: CLKL initially conceived the study. CSCF and EYTY are the principal investigators of the study. CLKL, CSCF, EYTY, VYG, CKHW, PI, DYTF, DCLL, WCWW, SKMT and AFYT helped with the design and implementation of the programmes. CLKL, EYTY, CSCF, VYG, CKHW, SYH and LYL coordinated the project. VYG, CSCF and EYTY drafted and revised the manuscript; CKHW, KK, SYH, LYL, PI, DYTF, DCLL, WCWW, SKMT and AFYT revised the manuscript. All authors approved the final version.
Funding: This work is supported by Kerry Group Kuok Foundation (Hong Kong) Limited.
Competing interests: None declared.
Ethics approval: This project was approved by the University of Hong Kong—the Hospital Authority Hong Kong West Cluster IRB, Reference number: UW 12-517.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Wagstaff A. Poverty and health sector inequalities. Bull World Health Organ 2002;80:97–105. [PMC free article] [PubMed] [Google Scholar]
- 2.Farmer FL, Stokes CS, Fiser RH et al. Poverty, primary care and age-specific mortality. J Rural Health 1991;7:153–69. 10.1111/j.1748-0361.1991.tb00716.x [DOI] [PubMed] [Google Scholar]
- 3.Duncan GJ, Yeung WJ, Brooks-Gunn J et al. How much does childhood poverty affect the life chances of children? Am Sociol Rev 1998;63:406–23. 10.2307/2657556 [DOI] [Google Scholar]
- 4.Brooks-Gunn J, Duncan GJ. The effects of poverty on children. Future Child 1997;7:55–71. 10.2307/1602387 [DOI] [PubMed] [Google Scholar]
- 5.Cheng YH, Chi I, Boey KW et al. Self-rated economic condition and the health of elderly persons in Hong Kong. Soc Sci Med 2002;55:1415–24. 10.1016/S0277-9536(01)00271-4 [DOI] [PubMed] [Google Scholar]
- 6.Sturm R, Gresenz CR. Relations of income inequality and family income to chronic medical conditions and mental health disorders: national survey. BMJ 2002;324:20–3. 10.1136/bmj.324.7328.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoshikawa H, Aber JL, Beardslee WR. The effects of poverty on the mental, emotional, and behavioral health of children and youth: implications for prevention. Am Psychol 2012;67: 272–84. 10.1037/a0028015 [DOI] [PubMed] [Google Scholar]
- 8.WHO. The Alma-Ata Conference on Primary Health Care. WHO Chron 1978;32:409–30. [PubMed] [Google Scholar]
- 9.World Health Organization. The world health report 2008: primary health care: now more than ever. Geneva, Switzerland: World Health Organization, 2008. [Google Scholar]
- 10.Nutbeam D. Health promotion glossary. Health Promot Int 1998;13:349–64. 10.1093/heapro/13.4.349 [DOI] [Google Scholar]
- 11.Anderson JM. Empowering patients: issues and strategies. Soc Sci Med 1996;43:697–705. 10.1016/0277-9536(96)00153-0 [DOI] [PubMed] [Google Scholar]
- 12.Wallerstein N. Powerlessness, empowerment, and health: implications for health promotion programs. Am J Health Promot 1992;6:197–205. 10.4278/0890-1171-6.3.197 [DOI] [PubMed] [Google Scholar]
- 13.Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clin Diabetes 2004;22:123–7. 10.2337/diaclin.22.3.123 [DOI] [Google Scholar]
- 14.Anderson RM, Funnell MM, Butler PM et al. Patient empowerment. Results of a randomized controlled trial. Diabetes Care 1995;18:943–9. 10.2337/diacare.18.7.943 [DOI] [PubMed] [Google Scholar]
- 15.Hong Kong Baptist University. Tipping Point: Hong Kong's Alarming Income Inequality. HKBU Horizons 2012–2013;2:12–17. [Google Scholar]
- 16.Goverment of the Hong Kong Special Administrative Region. Hong Kong Poverty Situation Report 2013. 2013:169.
- 17.Steinhardt M, Dolbier C. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. J Am Coll Health 2008;56:445–53. 10.3200/JACH.56.44.445-454 [DOI] [PubMed] [Google Scholar]
- 18.Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Springer, 1984. [Google Scholar]
- 19.Swann WB Jr, Chang-Schneider C, Larsen McClarty K. Do people's self-views matter? Self-concept and self-esteem in everyday life. Am Psychol 2007;62:84–94. 10.1037/0003-066X.62.2.84 [DOI] [PubMed] [Google Scholar]
- 20.Lam CLK, Yuen NYK, Mercer SW et al. A pilot study on the validity and reliability of the Patient Enablement Instrument (PEI) in a Chinese population. Fam Pract 2010;27:395–403. 10.1093/fampra/cmq021 [DOI] [PubMed] [Google Scholar]
- 21.Howie JG, Heaney DJ, Maxwell M et al. A comparison of a Patient Enablement Instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pract 1998;15:165–71. 10.1093/fampra/15.2.165 [DOI] [PubMed] [Google Scholar]
- 22.Fong DYT, Lam CLK, Mak KK et al. The Short Form-12 Health Survey was a valid instrument in Chinese adolescents. J Clin Epidemiol 2010;63:1020–9. 10.1016/j.jclinepi.2009.11.011 [DOI] [PubMed] [Google Scholar]
- 23.Lam CL, Tse EY, Gandek B. Is the standard SF-12 health survey valid and equivalent for a Chinese population? Qual Life Res 2005;14:539–47. 10.1007/s11136-004-0704-3 [DOI] [PubMed] [Google Scholar]
- 24.Lam ET, Lam CL, Fong DY et al. Is the SF-12 version 2 Health Survey a valid and equivalent substitute for the SF-36 version 2 Health Survey for the Chinese? J Eval Clin Pract 2013;19:200–8. 10.1111/j.1365-2753.2011.01800.x [DOI] [PubMed] [Google Scholar]
- 25.Chan RC, Xu T, Huang J et al. Extending the utility of the Depression Anxiety Stress scale by examining its psychometric properties in Chinese settings. Psychiatry Res 2012;200:879–83. 10.1016/j.psychres.2012.06.041 [DOI] [PubMed] [Google Scholar]
- 26.Lovibond SH LP. Manual for the depression anxiety stress scales. Sydney: Psychology Foundation, 1995. [Google Scholar]
- 27.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials 1989;10:407–15. 10.1016/0197-2456(89)90005-6 [DOI] [PubMed] [Google Scholar]
- 28.Schwarzer R, Jerusalem M. Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M, eds. Measures in health psychology: a user's portfolio causal and control beliefs. Windsor, UK: NFER-NELSON, 1995:35–7. [Google Scholar]
- 29.Zhang JX, Schwarzer R. Measuring optimistic self-beliefs—a Chinese Adaptation of the General Self-Efficacy Scale. Psychologia 1995;38:174–81. [Google Scholar]
- 30.Wang CK, Hu ZF, Liu Y. Evidences for reliability and validity of the Chinese version of general Self efficacy Scale. Chin J Appl Psychol 2001;7:37–40. [Google Scholar]
- 31.Craig CL, Marshall AL, Sjöström M et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381–95. 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 32.Deng HB, Macfarlane DJ, Thomas GN et al. Reliability and validity of the IPAQ-Chinese: the Guangzhou Biobank Cohort study. Med Sci Sports Exerc 2008;40:303–7. 10.1249/mss.0b013e31815b0db5 [DOI] [PubMed] [Google Scholar]
- 33.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18:499–502. [PubMed] [Google Scholar]
- 34.Ip MS, Ko FW, Lau AC et al. Updated spirometric reference values for adult Chinese in Hong Kong and implications on clinical utilization. Chest 2006;129:384–92. 10.1378/chest.129.2.384 [DOI] [PubMed] [Google Scholar]
- 35.Ip MS, Karlberg EM, Karlberg JP et al. Lung function reference values in Chinese children and adolescents in Hong Kong. I. Spirometric values and comparison with other populations. Am J Respir Crit Care Med 2000;162(2 Pt 1):424–9. 10.1164/ajrccm.162.2.9905057 [DOI] [PubMed] [Google Scholar]
- 36.Birch J. Efficiency of the Ishihara test for identifying red-green colour deficiency. Ophthalmic Physiol Opt 1997;17:403–8. 10.1111/j.1475-1313.1997.tb00072.x [DOI] [PubMed] [Google Scholar]
- 37.Hirschberg J. Beiträge zur Lehre vom Schielen und von der Schieloperation. Zentralblatt für Praktische Augenheilkunde. Leipzig: Verlag von Veit & Co. 1886:5–9. [Google Scholar]
- 38.Fine AM, Elman MJ, Ebert JE et al. Earliest symptoms caused by neovascular membranes in the macula. Arch Ophthalmol 1986;104:513–14. 10.1001/archopht.1986.01050160069013 [DOI] [PubMed] [Google Scholar]
- 39.Katz J. Handbook of clinical audiology. Vol 5 Philadelphia, PA: Lippincott Williams & Wilkins, 2002. [Google Scholar]
- 40.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142–8. 10.1111/j.1532-5415.1991.tb01616.x [DOI] [PubMed] [Google Scholar]
- 41.Wechsler D. Wechsler intelligence scale for children. 3rd edn, revised. New York: Psychological Corporation, 1991. [Google Scholar]
- 42.Axelrod BN, Randolph C, Donnell A et al. Rapidly administered short forms of the Wechsler adult intelligence scale-3rd edition. Clin Neuropsychol 2007;21:694–4. [DOI] [PubMed] [Google Scholar]
- 43.Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581–6. 10.1111/j.1469-7610.1997.tb01545.x [DOI] [PubMed] [Google Scholar]
- 44.Lai KY, Luk ES, Leung PW et al. Validation of the Chinese version of the strengths and difficulties questionnaire in Hong Kong. Soc Psychiatry Psychiatr Epidemiol 2010;45:1179–86. 10.1007/s00127-009-0152-z [DOI] [PubMed] [Google Scholar]
- 45.Landgraf JM, Abetz L, Ware JE. The CHQ: a user's manual (2nd printing). Boston, MA: HealthAct, 1999, 1996. 1st printing. Boston, MA: The Health Institute. (No longer in print. Now available as Child health Questionnaire Scoring and Interpretation Manual. 2008 HealthActCHQ Inc., Cambridge, MA, USA. [Google Scholar]
- 46.Ng JY, Landgraf JM, Chiu CS et al. Preliminary evidence on the measurement properties of the Chinese version of the Child Health Questionnaire, parent form (CHQ-pF50) and child form (CHQ-CF87). Qual Life Res 2005;14:1775–81. 10.1007/s11136-005-1005-1 [DOI] [PubMed] [Google Scholar]
- 47.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–13. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yu X, Tam WW, Wong PT et al. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr Psychiatry 2012;53:95–102. 10.1016/j.comppsych.2010.11.002 [DOI] [PubMed] [Google Scholar]
- 49.Tiwari A, Fong DY, Chan KL et al. Identifying intimate partner violence: comparing the Chinese Abuse Assessment Screen with the Chinese Revised Conflict Tactics Scales. BJOG 2007;114:1065–71. 10.1111/j.1471-0528.2007.01441.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing 1972;1:233–8. 10.1093/ageing/1.4.233 [DOI] [PubMed] [Google Scholar]
- 51.Barry MJ, Fowler FJ Jr., O'Leary MP et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 1992;148:1549–57; discussion 64. [DOI] [PubMed] [Google Scholar]
- 52.Choi EP, Lam CL, Chin WY. Validation of the International Prostate Symptom Score in Chinese males and females with lower urinary tract symptoms. Health Qual Life Outcomes 2014;12:1 10.1186/1477-7525-12-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Avery K, Donovan J, Peters TJ et al. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn 2004;23:322–30. 10.1002/nau.20041 [DOI] [PubMed] [Google Scholar]
- 54.Huang L, Zhang SW, Wu SL et al. The Chinese version of ICIQ: a useful tool in clinical practice and research on urinary incontinence. Neurourol Urodyn 2008;27:522–4. 10.1002/nau.20546 [DOI] [PubMed] [Google Scholar]
- 55.Lam CL, Leung GM, Mercer SW et al. Utilisation patterns of primary health care services in Hong Kong: does having a family doctor make any difference? Hong Kong Med J 2011;17(3 Suppl 3):28–32. [PubMed] [Google Scholar]
- 56.Fung CSC, Wong CKH, Fong DYT et al. Having a family doctor was associated with lower utilization of hospital-based health services. BMC Health Services Research 2015;15:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Baum F, MacDougall C, Smith D. Participatory action research. J Epidemiol Community Health 2006;60:854–7. 10.1136/jech.2004.028662 [DOI] [PMC free article] [PubMed] [Google Scholar]