Abstract
We report a rare case of a 61-year-old homeless man with a 15-year history of multiple trichilemmal cysts that served as a forerunner for the emergence of a malignant proliferating pilar tumour. The patient presented multiple, large, purulent, ulcerated lesions ranging from 10 to 150 mm in diameter, covering most of the scalp, with large areas superimposed by extensive myiasis infestation. The patient presented with no other major clinical findings. A CT scan showed no detectable signs of local or distant metastatic invasion. Initial supportive treatment was implemented. Given the extent of the injury, further surgical excision was considered, which required transfer to a specialised surgical centre. This social case is of educational value, as it can raise clinician awareness about the ability of trichilemmal cysts to undergo malignant transformation. Additionally, it highlights the importance of adequate social assistance structures for patients in need.
Background
Trichilemmal (pilar) cysts are common benign intradermal or subcutaneous cysts found in clinical practice. Malignant transformation of the aforementioned cysts is a rare phenomenon and even fewer cases describing ulceration of the cystic roof have been reported.
In this case report, we present a patient with a history of multiple trichilemmal cysts, the largest of which underwent transformation to a malignant proliferating pilar tumour. Despite the rarity of this case, it is a reminder that trichilemmal cysts can develop malignancy and highlights the possible consequences of neglecting such cysts. This is particularly important in the current social context, where the assistance to individuals with financial difficulties has become increasingly challenging.
Case presentation
A 61-year-old homeless man presented to the emergency department for evaluation of head lesions associated with ongoing pain for 3 days before admission.
The patient presented a 15-year history of multiple, slowly enlarging cystic scalp formations that would spontaneously burst and drain, leaving small openings. There were no further symptoms or detectable complications. The patient referred no history of trauma and did not mention redness or tenderness in any of the lesions throughout the 15-year period, at least not to the extent of what was now apparent. No medical practitioner had followed this process. The patient also mentioned that the large frontoparietal ulcer originated from an unusually large cystic formation, of approximately 150 mm in diameter, which had burst and drained 3 years earlier. He also stated that the overlying dome slowly degenerated until it presented with moderate pain, 3 days before admission.
The patient's medical history was otherwise unremarkable, with no signs of alcoholism, no drug abuse and no past mental illness. Family history on the maternal side revealed multiple dome-like structures on the head.
On examination, a large, purulent, ulcerated wound (approximately 150×150 mm) was observed covering the frontoparietal aspect of the patient's head. Extensive myiasis infestation was present (figure 1). The lesion was firm and tender on palpation. Accompanying this lesion were five, well circumscribed satellite dome-like formations of various sizes, ranging from approximately 10–100 mm, on the parietal and occipital epicranium (figure 2). The formations were firm, smooth and moderately mobile. They exhibited typical pitting signs, were non-tender on palpation and were covered with hair. Physical examination revealed no palpable cervical or parotid lymphadenopathy, and no further skin findings. The rest of the examination was unremarkable, as the patient presented systemically well with all observations within normal range. Since the patient appeared generally unaware of the severity of his condition, a thorough mental evaluation was performed, with no evidence of mental illness.
Figure 1.

Macroscopic view of the main lesion on admission. The ulcerated area (150×150 mm) covers the frontoparietal aspect of the patient's head. One of the larvae removed from the lesion is also observable.
Figure 2.

Macroscopic view of the satellite lesions. Five dome-like formations of various sizes are noticeable on the parietal and occipital epicranium.
Given the clinical and history findings, a conditional diagnosis of squamous cell carcinoma was made, originating from a background of chronic inflammation over a large degenerated cyst. Follow-up therapeutic options were discussed.
Investigations
Biochemical and haematological investigations disclosed a mild, hypochromic, microcytic anaemia and a C reactive protein elevation without leukocytosis. A mild elevation in fasting blood glucose was also detected.
A 30 mm diameter cystic formation was surgically excised and sent for histopathological interpretation. Microscopically it showed evidence of being a trichilemmal cyst (figure 3).
Figure 3.
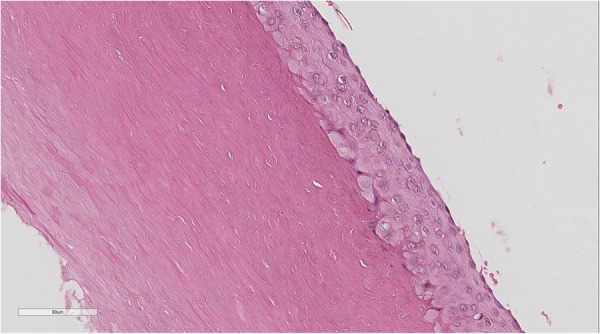
Microscopic view of trichilemmal (pilar) cyst wall. The cyst contains amorphous, dense and compact homogenised keratin. There is no granular layer. (H&E ×100).
Biopsy of three fragments removed from the main lesion showed multiple lobules composed of squamous epithelium and pilar keratinisation. Other areas displayed features of malignant proliferating pilar tumours with areas of a carcinomatous infiltrating component, increase of nuclear and cytoplasmic pleomorphism, along with mitotic figures and foci of necrosis (figure 4A). This carcinomatous component deeply infiltrated the reticular dermis and subcutis with dissection of the eccrine sweat glands (figure 4B).
Figure 4.
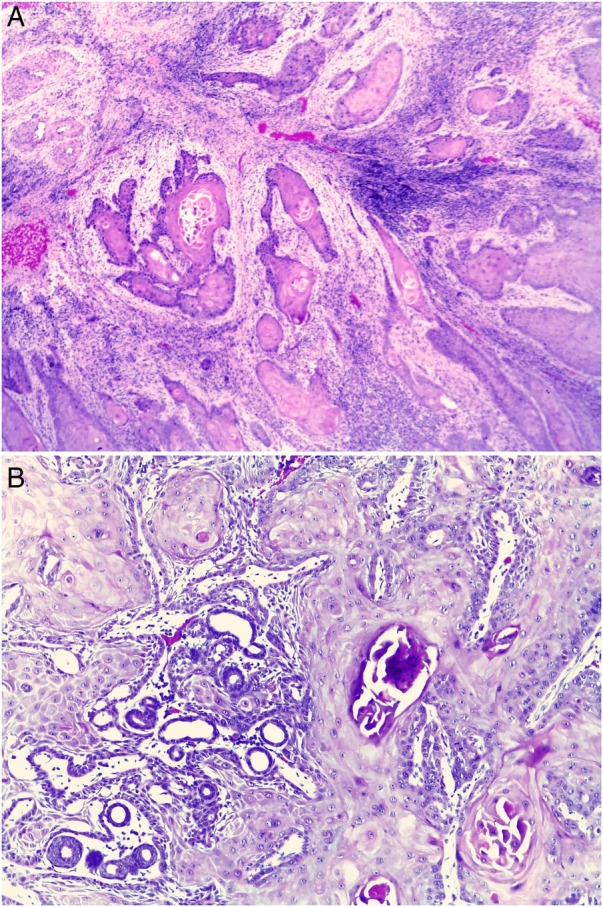
(A) Microscopic view of the main tumour. Carcinomatous infiltrating component along with cytological atypia and mitosis. (H&E ×100). (B) Microscopic view of the main tumour. Carcinomatous infiltrating component, dissecting eccrine sweat glands. (H&E ×200).
Although malignant proliferating pilar tumours are histologically similar to squamous cell carcinomas, some features are helpful in distinguishing these entities from each other. These features include trichilemmal keratinisation, dystrophic calcification, cyst formation and absence of epidermal premalignant lesion.1 2
Consequently, the presumptive diagnosis of squamous cell carcinoma was discarded, and a definitive diagnosis of malignant proliferating pilar tumour was made.
CT scan of the head displayed five epicranial oval lesions, consistent with the physical examination. These were of various sizes, the smallest being 14.5×15 mm and the largest, 85×80 mm, with non-pure heterogeneous liquid-air content, forming multiple fluid-air levels. Some masses presented coarse areas of calcification. These findings were consistent with multiple trichilemmal cysts with superimposed infection. There was also a marked asymmetric, irregular and heterogeneous thickening of the soft tissue of the epicranium with a larger extension to the left, consistent with the main tumour (figure 5A–C). There was no evidence of cranial invasion, haematic densities or midline deviations. Cervical and chest CT scans were performed for the tumour staging process, revealing no significant findings.
Figure 5.
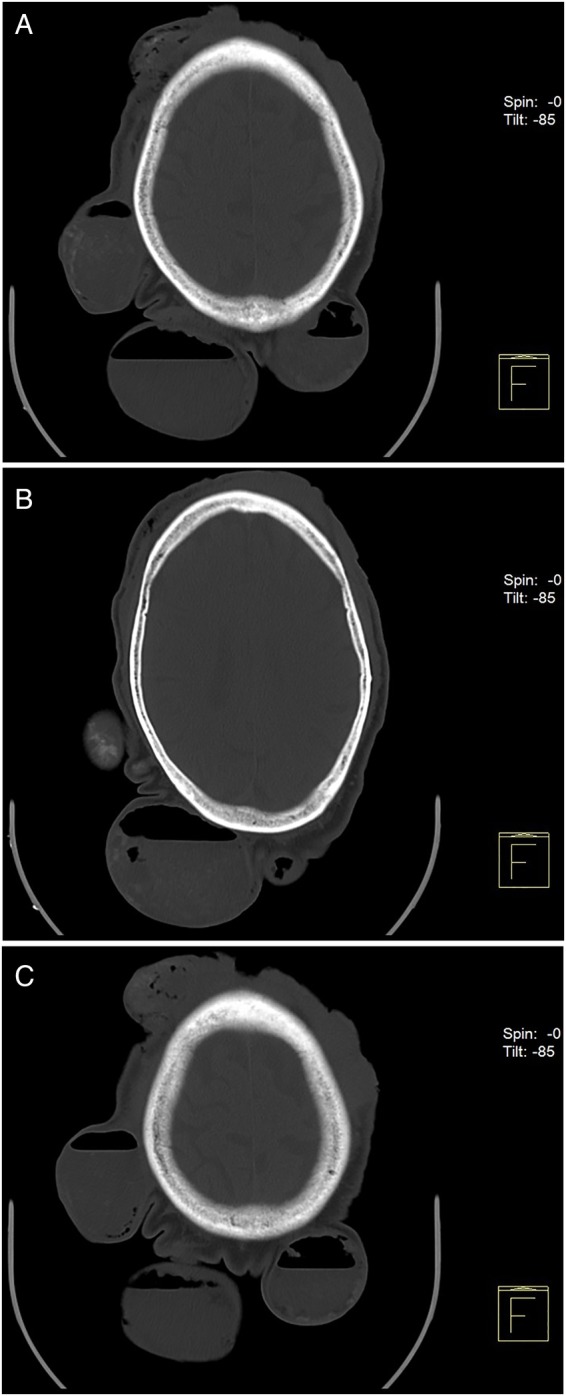
(A–C) CT scan of the head. Five epicranial oval lesions of various sizes, the smallest lesion being 14.5×15 mm, and the largest, 85×80 mm in diameter, with non-pure heterogeneous liquid-air content, forming multiple fluid-air levels. There are no discernable signs of regional tumour invasion.
Differential diagnosis
The differential diagnoses that were considered prior to histopathological evaluation included:
Squamous cell carcinoma
Proliferating pilar tumour
Basal cell carcinoma
Cylindroma
Treatment
Before the diagnosis of a malignant tumour was made, surgical debridement of necrotic tissue was performed, the larvae were removed and the lesion was cleaned. The patient began treatment with albendazole. Multiple fatty gauze dressings were used, alternating between chemical debridement and silver alginate, according to the developmental phase of the lesion.
A week later, the infestation was controlled and the lesions showed evidence of improvement, with fibrinous and granulation tissue covering most of the affected ulcerated areas (figure 6).
Figure 6.

Macroscopic view of the main lesion 7 days after supportive treatment. The ulcerated area presents signs of improvement, with fibrinous and granulation tissue covering the ulcerated depression.
Outcome and follow-up
Given the diagnosis of malignant proliferating pilar tumour, surgical and medical approaches were considered.
Since scalp reconstruction after wide tumour excision is particularly challenging, and our team has little experience in reconstructive surgery to the extent that was required, the patient was referred to an external specialised oncological and surgical centre. He was considered eligible for a wide-margin surgical excision and graft placement.
In order to provide an adequate environment for the complete recovery of this patient, social services were contacted in an attempt to provide him with acceptable housing, hygiene and nutrition.
The patient was expected to return for a scheduled follow-up consultation, which he missed, and contacting the patient has proven to be unsuccessful.
Discussion
A proliferating pilar tumour, also known as proliferating trichilemmal cyst, is a rare neoplasm that originates in the outer root sheath of the hair follicle, usually within a pre-existing trichilemmal cyst.3 4 Wilson-Jones first acknowledged this neoplasm in 1966, referring to it as a proliferating epidermoid cyst, denoting its histological ability to simulate squamous cell carcinoma. It is most commonly found in the elderly, and usually located in the scalp area.3 5 6 Other lesion sites have been described and are generally associated with a poorer prognosis.6 7 The tumours are large (10–250 mm), undergoing slow and progressive growth over months to years.8 The lesions may be asymptomatic or present with inflammatory signs, ulceration, bleeding or discharge.2 4 8 9
Although generally benign, infrequent malignant transformation of proliferating pilar tumours is possible and starts with an adenomatous stage (trichilemmal cyst), followed by an epitheliomatous stage (proliferating trichilemmal cyst), and, finally, a carcinomatous stage (malignant proliferating pilar tumour).4 10 Hypothesised triggers for this malignant transformation include insults such as inflammation and trauma.10
A recent clinicopathological study of 76 cases with proliferating pilar tumour by Ye et al8 proposes stratification of the lesions into three groups, based on five characteristics: tumour contour, necrosis, nuclear atypia, degree of stromal invasion and mitotic rate. The first group is classified as having a benign behaviour, the second group presents a low risk of local recurrence and the third group potentially recurs regionally and metastasises.8
Histopathological analysis usually shows a well-limited neoplasm, with a lobular proliferation of squamous epithelium.2 11 Areas of trichilemmal keratinisation and focal epidermal keratinisation are typically present.7 Other potential features include vacuolated or clear glycogen-rich cells, cytological atypia of different degrees, squamous eddies, keratin pearls, focal cystic areas and calcifications.2 12 13 The peripheral cells tend to palisade and mitotic rate is generally high.2 14 Occasionally, the tumour mimics squamous cell carcinoma by extending nests of squamous cells into contiguous connective tissue instead of proliferating only into the cyst.2
The treatment of choice is generally surgical excision. Lesions of the second and third group may require other interventions such as radiotherapy (in recurrence prophylaxis) or chemotherapy (for metastatic disease).8 9 15 Nevertheless, the reduced number of cases described in the literature limits the efficacy evaluation of alternative treatments.3 6 Clinical follow-up is required subsequent to surgical intervention in order to monitor local recurrence and lymph node metastasis.6 15
Learning points.
Malignant proliferating pilar tumours are neoplasms of slow growth usually deriving from pre-existing trichilemmal cysts, and most likely caused by stimuli such as trauma and inflammation.
Histologically, this tumour mimics squamous cell carcinoma, creating a diagnostic challenge for pathologists, who should be watchful during histopathological examination of suspected cases.
The treatment of choice for malignant proliferating pilar tumours is wide-margin surgical excision, withholding chemotherapy and radiation therapy for cases in which metastatic disease and/or recurrence is present.
Clinicians and patients should be aware of the ability trichilemmal cysts have to develop malignancy and the ensuing consequences of neglecting them.
Public health bodies must be aware of the importance of providing social support to economically and socially disadvantaged patients.
Acknowledgments
Maria Guilherme Canivete Semedo and Joana Cristina Ferreira Pinto, for provided information regarding the current case.
Footnotes
Contributors: BM and NS contributed to the acquisition and analysis of clinical data, and to the preparation of the manuscript draft. PA contributed to the histopathological interpretation and was involved in drafting and reviewing the manuscript. AR contributed in patient management and review of the manuscript. All the authors reviewed and approved the final version of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Brownstein MH, Arluk DJ. Proliferating trichilemmal cyst: a simulant of squamous cell carcinoma. Cancer 1981;48:1207–14. [DOI] [PubMed] [Google Scholar]
- 2.Weedon D, Strutton G, Rubin AI. Weedon's skin pathology. 3rd edn Edinburgh: Churchill Livingstone/Elsevier, 2010:444. [Google Scholar]
- 3.Siddha M, Budrukkar A, Shet T et al. Malignant pilar tumor of the scalp: a case report and review of literature. J Cancer Res Ther 2007;3:240–3. 10.4103/0973-1482.39001 [DOI] [PubMed] [Google Scholar]
- 4.Sharma R, Verma P, Yadav P et al. Proliferating trichilemmal tumor of scalp: benign or malignant, a dilemma. J Cutan Aesthet Surg 2012;5:213–15. 10.4103/0974-2077.101394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones EW. Proliferating epidermoid cysts. Arch Dermatol 1966;94:11–19. 10.1001/archderm.1966.01600250017002 [DOI] [PubMed] [Google Scholar]
- 6.Goyal S, Jain BB, Jana S et al. Malignant proliferating trichilemmal tumor. Ind J Dermatol 2012;57:50–2. 10.4103/0019-5154.92679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cavaleiro LH, Viana Fde O, Carneiro CM et al. Proliferating trichilemmal tumor—case report. An Bras Dermatol 2011;86(4 Suppl 1):S190–2. 10.1590/S0365-05962011000700049 [DOI] [PubMed] [Google Scholar]
- 8.Ye J, Nappi O, Swanson PE et al. Proliferating pilar tumors: a clinicopathologic study of 76 cases with a proposal for definition of benign and malignant variants. Am J Clin Pathol 2004;122:566–74. 10.1309/21DK-LY2R-94H1-92NK [DOI] [PubMed] [Google Scholar]
- 9.Khoja AA, Yan B, Lee SJ et al. Proliferating tricholemmal tumour: clinicopathological aspects of a case. Singapore Med J 2011;52:e255–7. [PubMed] [Google Scholar]
- 10.Gulati HK, Deshmukh SD, Anand M et al. Low-grade malignant proliferating pilar tumor simulating a squamous-cell carcinoma in an elderly female: a case report and immunohistochemical study. Int J Trichol 2011;3:98–101. 10.4103/0974-7753.90818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feng Z, Zhu HG, Wang LZ et al. Tricholemmal carcinoma of the head and neck region: A report of 15 cases. Oncol Lett 2014;7:423–426. 10.3892/ol.2013.1726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shet T, Modi C. Nucleolar organizer regions (NORs) in simple and proliferating trichilemmal cysts (pilar cysts and pilar tumors). Indian J Pathol Microbiol 2004;47:469–73. [PubMed] [Google Scholar]
- 13.Rangel-Gamboa L, Reyes-Castro M, Dominguez-Cherit J et al. Proliferating trichilemmal cyst: the value of ki67 immunostaining. Int J Trichol 2013;5:115–17. 10.4103/0974-7753.125599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.López-Ríos F, Rodriguez-Peralto JL, Aguilar A et al. Proliferating trichilemmal cyst with focal invasion: report of a case and a review of the literature. Am J Dermatopathol 2000;22:183–7. 10.1097/00000372-200004000-00018 [DOI] [PubMed] [Google Scholar]
- 15.Aneiros-Fernandez J, Jimenez-Rodriguez JM, Martin A et al. Giant proliferating trichilemmal malignant tumor. Indian J Dermatol Venereol Leprol 2011;77:730 10.4103/0378-6323.86507 [DOI] [PubMed] [Google Scholar]


