Abstract
A 33-year-old HIV-positive Indian man presented with multiple bluish and erythematous papulo-nodules on his right leg and foot. A diagnosis of Kaposi's sarcoma was suspected clinically. Biopsy of the cutaneous lesions showed features of melanoma. On careful re-examination, an irregular brown-black macule, of which the patient was unaware, was noted on the ipsilateral sole. Histological examination of the sole lesion also showed features of melanoma. Systemic evaluation revealed extensive nodal and visceral metastases.
Background
Cutaneous melanomas are uncommon in the Asian population, thus atypical presentations may be misdiagnosed in these patients. We report an unusual presentation of acral lentiginous melanoma in a young Indian man. The cutaneous lesions were initially mistaken for Kaposi's sarcoma, not only due to the striking morphological similarity, but also because of his positive HIV status.
Case presentation
A 33-year-old Indian man had gradually progressing asymptomatic papules on his right foot for the past 1 year. For the last few months, the lesions increased rapidly and involved his right leg. He lost about 10 kg weight during this course. He had a medical history of pulmonary tuberculosis, treated 2 years prior. At the same time, he was found to have HIV serology positivity, but had not received anti-retroviral treatment. Examination revealed multiple bluish-erythematous papules, grouped near the medial aspect of the right foot, with overlying ulceration. There were multiple discrete bluish and dusky-red papules scattered over the right shin, on a background of indurated skin with overlying loss of hair. There was mild pitting oedema on the right shin. A single brown-coloured firm plaque with overlying nodules was present on the right thigh (figure 1A, B). Bilateral inguinal lymph nodes were enlarged (size 2–2.5 cm), hard and mobile. Systemic examination was normal.
Figure 1.
(A) Multiple ulcerated papules grouped near the medial aspect of the foot. Discrete bluish and erythematous papules scattered on the shin. (B) Hyperpigmented plaques with overlying nodules on the thigh. (C) Brown-black macule with variegated colour on the sole, with adjacent ulcerated papules and nodules.
Investigations
Routine investigations were unremarkable. Serology for HIV-1 was positive, and CD4 count was 586/µL. Histopathological examination of the shin papule and the thigh plaque showed features of melanoma, confirmed by immunohistochemistry as HMB-45 and S-100. A lymph node biopsy also showed features consistent with melanoma (figure 2A–D). On careful re-examination of the skin, a previously deemed insignificant brown-black macule, of which the patient was unaware, with variegated colour and irregular margins, was noted on the posterior sole (figure 1C). Biopsy of the sole lesion also showed features of melanoma. A whole body positron emission tomography scan showed multiple hypermetabolic cutaneous and subcutaneous nodules in the right lower limb, and multiple lymph nodes along with liver, lumbar and brain metastases (figure 2E, F). A final diagnosis of acral lentiginous melanoma with extensive nodal and visceral metastases was made.
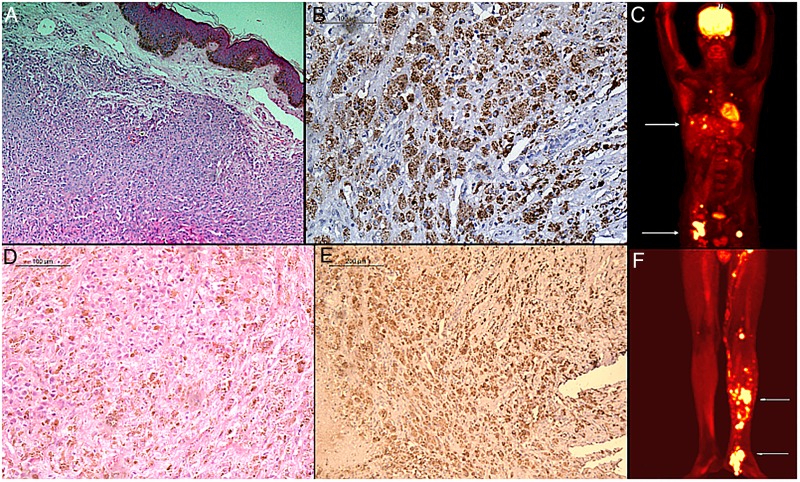
Figure 2.
(A) Skin biopsy from one of the papules showing nests of tumour cells in the dermis having large polygonal cells with large nuclei and prominent nucleoli (H&E stain, ×100). (B) Intracytoplasmic melanin pigment within the atypical cells (HMB-45 stain, ×200). (C and D) Inguinal lymph node biopsy showing sheets of large polygonal cells with melanin pigment and many mitotic figures (H&E stain, ×200; HMB-45 stain, ×100). (E and F) Positron emission tomography scan showing increased uptake in multiple cutaneous and subcutaneous sites, multiple lymph nodes and liver.
Differential diagnosis
The dusky red papulo-nodules on an oedematous lower extremity made us suspect a vascular tumour, probably Kaposi's sarcoma or angiosarcoma. The positive HIV status of our patient tilted the diagnosis in favour of the former. Similar ‘vascular-appearing’ lesions may also be seen in bacillary angiomatosis in such a setting. A possibility of cutaneous metastases should also be considered, given the significant weight loss and lymphadenopathy.
Outcome and follow-up
The patient was counselled about the disease, but refused further treatment, and was subsequently lost to follow-up.
Discussion
Acral lentiginous melanoma, which is overall the least common type of the four major histological variants, accounts for the highest proportion of all melanomas in dark-skinned individuals.1 2 The lesions appear as asymmetric brown-black macules with irregular borders and colour variation, usually affecting the palms, soles or nail apparatus. A large proportion of acral lentiginous melanomas are diagnosed at an advanced stage, probably due to a close clinical resemblance to benign lesions, coupled with location of the lesions at sites not frequently examined by the patients, thus presenting late to the clinician.3 Our patient was not even aware of the pigmented lesion on his sole—he consulted us only after he had started developing papulo-nodular lesions on his leg. It was only when the biopsy showed features of metastatic melanoma that we suspected the sole lesion to be the primary. Additionally, the bluish and violaceous-red lesions on our patient's leg closely resembled the lesions of Kaposi's sarcoma. We could find only a few reports of cutaneous melanoma metastases resembling Kaposi's sarcoma in the literature.4 5 Although Kaposi's sarcoma is quite rare in the Indian population,6 our patient's positive HIV status, apart from the clinical manifestations, made us favour this diagnosis. Interestingly, Amerson et al7 found that clinical diagnoses of Kaposi's sarcoma are often incorrect among HIV-infected East African patients.
A meta-analysis found HIV patients to be at a significant risk of melanoma, which has remained unchanged in the HAART era.8 The increased risk of melanoma in patients with HIV is related not only to immunosuppression, but also immune dysregulation, including chronic immune activation and its effect on immune surveillance. Another factor contributing to the perceived increased melanoma risk in the HIV population could be the increased surveillance for skin lesions in these patients. Apart from the increased risk, it has been observed that melanoma in HIV patients may behave more aggressively, as compared to that in HIV-negative individuals.9
To conclude, the cutaneous melanoma metastases in our case had a striking similarity to Kaposi's sarcoma. Owing to the poor predictive value of clinical suspicion of such lesions, histopathological examination is essential to confirm the diagnosis. Although uncommon in dark-skinned individuals, melanoma should be suspected for any atypical pigmented lesion, especially on the sole.
Learning points.
The differential diagnosis for vascular-appearing papules and nodules may include cutaneous melanoma metastases, in the appropriate setting.
Histopathological examination is essential for diagnosis, owing to a broad range of clinical differential diagnoses for such lesions.
Melanoma should be ruled out for atypical pigmented lesions on acral sites, even in dark-skinned individuals.
Patients are often unaware of such lesions at these neglected sites, and present with advanced disease.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bradford PT, Goldstein AM, McMaster ML et al. Acral lentiginous melanoma: incidence and survival patterns in the United States, 1986–2005. Arch Dermatol 2009;145:427–34. 10.1001/archdermatol.2008.609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cormier JN, Xing Y, Ding M et al. Ethnic differences among patients with cutaneous melanoma. Arch Intern Med 2006;166:1907–14. 10.1001/archinte.166.17.1907 [DOI] [PubMed] [Google Scholar]
- 3.Nestle FO, Halpern AC. Melanoma. In: Bolognia JL, Jorizzo JL, Rapini RP, eds. Dermatology. 2nd edn. Mosby, Spain, 2008;1745–71. [Google Scholar]
- 4.Lancer HA, Bronstein BR, Sober AJ. Multiple cutaneous melanoma metastases of an extremity resembling Kaposi's sarcoma: use of regional perfusion. J Dermatol Surg Oncol 1984;10:196–9. 10.1111/j.1524-4725.1984.tb01206.x [DOI] [PubMed] [Google Scholar]
- 5.Bassioukas K, Zioga A, Konstantinou E et al. Amelanotic subungual malignant melanoma with multiple nodular local skin metastases. Cutis 2002;69:353–6. [PubMed] [Google Scholar]
- 6.Vaishnani JB, Bosamiya SS, Momin AM. Kaposi's sarcoma: a presenting sign of HIV. Indian J Dermatol Venereol Leprol 2010;76:215 10.4103/0378-6323.60542 [DOI] [PubMed] [Google Scholar]
- 7.Amerson E, Woodruff CM, Forrestel A et al. Accuracy of clinical suspicion and pathologic diagnosis of Kaposi sarcoma in East Africa. J Acquir Immune Defic Syndr 2015. Epub ahead of print. 10.1097/QAI.0000000000000862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olsen CM, Knight LL, Green AC. Risk of melanoma in people with HIV/AIDS in the pre- and post-HAART eras: a systematic review and meta-analysis of cohort studies. PLoS ONE 2014;9:e95096 10.1371/journal.pone.0095096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rodrigues LKE, Klencke BJ, Vin-Christian K et al. Altered clinical course of malignant melanoma in HIV-positive patients. Arch Dermatol 2002;138:765–70. 10.1001/archderm.138.6.765 [DOI] [PubMed] [Google Scholar]