Abstract
Background
Depression is known to run in families, but the effects of parental history of other psychiatric diagnoses on depression rates are less well studied. Few studies have examined the impact of parental psychopathology on depression rates in older age groups.
Methods
We established a population-based cohort including all individuals born in Denmark after 1954 and alive on their 10th birthday (N=2,976,264). Exposure variables were maternal and paternal history of schizophrenia, bipolar disorder, depression, anxiety or ‘other’ psychiatric diagnoses. Incidence rate ratios (IRR) were estimated using poisson regressions.
Results
Parental history of any psychiatric diagnosis increased incidence rates of outpatient (maternal: IRR = 1.88, p < .0001; paternal: IRR = 1.68, p < .0001) and inpatient (maternal: IRR = 1.99, p < .0001; paternal: IRR = 1.83, p < .0001) depression relative to no parental history. IRRs for parental history of non-affective disorders remained relatively stable across age groups, while IRRs for parental affective disorders (unipolar or bipolar) decreased with age from 2.29–3.96 in the youngest age group to 1.53–1.90 in the oldest group. IRR estimates for all parental diagnoses were similar among individuals 41+ (IRR range: 1.51–1.90).
Conclusions
Parental history of any psychiatric diagnosis is associated with increased incidence rates of unipolar depression. In younger age groups, parental history of affective diagnoses is more strongly associated with rates of unipolar depression than non-affective diagnoses, however this distinction disappears after age 40, suggesting that parental psychopathology in general, rather than any one disorder, confers risk for depression in middle life.
Keywords: unipolar depression, parental history, survival analysis, register-based research
Introduction
Previous research has established definitively that unipolar depression runs in families. Studies from clinical (Gershon et al. 1982; Mitchell et al. 1989; Orvaschel et al. 1988; Puig-Antich et al. 1989; Weissman et al. 1982, 1984a; Weller et al. 1994; Welner & Rice 1988) and community (Beardslee et al. 1988; Kendler et al. 1997; Klein et al. 2001, 2005; Low et al. 2012) samples show that the odds of having a first-degree relative with depression are 2–3 times higher among depressed individuals compared with control subjects. Prospective studies following participants for between 1 and 20 years found that the risk of depression among children of depressed parents was 2–3 times higher than the risk in children of controls (Beardslee et al. 1996; Hammen et al. 1990; Lieb et al. 2002; Radke-Yarrow et al. 1992; Weissman et al. 1997, 2006).
These findings are consistent with results from twin studies, which suggest that depression is around 30–40% heritable (Sullivan et al. 2000). Genetic studies also suggest, however, that the underlying genetic architecture of depression may overlap with that of other psychiatric diagnoses including anxiety (Cerda et al. 2010; Demirkan et al. 2011; Middeldorp et al. 2005), bipolar disorder (Lee et al. 2013; McGuffin et al. 2003) and schizophrenia (Argyropoulos et al. 2008; Lee et al. 2013). This raises the possibility that parental history of psychiatric diagnoses besides depression may also confer risk for depression in offspring. While the majority of studies on the effects of parental psychopathology focused exclusively on parental history of affective disorders (Beardslee et al. 1988; Billings & Moos 1986; Hammen et al. 1990; Klein et al. 1988; Lieb et al. 2002; Orvaschel et al. 1988; Radke-Yarrow et al. 1992; Weissman et al. 1984b, 1987, 1997, 2006; Welner & Rice 1988), several studies found evidence suggesting that parental history of anxiety (Biederman et al. 2001; Low et al. 2012; Mitchell et al. 1989; Weller et al. 1994), bipolar disorder (Henin et al. 2005), substance abuse (Todd et al. 1996; Welner & Rice 1988) and non-affective psychosis (Dean et al. 2010) also confer risk for depression in offspring either alone, or when comorbid with depression (Merikangas et al. 1988, 1994; Puig-Antich et al. 1989; Weissman et al. 1984c).
Most of the studies examining the impact of parental psychopathology on offspring depression risk focused on children (Billings & Moos 1986; Hammen et al. 1990; Weissman et al. 1992) and adolescents (Beardslee et al. 1996; Weissman et al. 1997), but epidemiologic evidence suggests that the average age of onset for unipolar depression is 32 years (Kessler et al. 2005). Because these studies did not evaluate the impact of parental psychopathology during the peak timeframe for depression onset in offspring, they may have failed to capture the full impact of parental psychopathology on depression risk. In addition, they may have missed differences in the effects of parental history on depression risk in older vs. younger individuals.
National registries provide an excellent source of data for addressing these types of research questions because they include information on entire populations over long periods of time. The Danish National Registry System (Thygesen et al. 2011) includes data on all inpatient and outpatient treatment, as well as information linking parents and offspring, for 8 million people. Previous studies have used this data to explore the effects of parental psychopathology in one, both or neither parent (Dean et al. 2010) on mental illness in offspring, as well as specificity of transmission (i.e. family aggregation) for mental disorders in cases with onset in childhood or adolescence (Steinhausen et al. 2009). To our knowledge, no previous study in either this or any other dataset has examined the specific effects of a range of psychiatric diagnoses on offspring depression rates across age groups.
The goals of this study were to 1) examine the associations between parental history of psychiatric diagnoses including anxiety, depression, bipolar disorder, and schizophrenia, and incidence rates of outpatient and inpatient unipolar depression in the Danish psychiatric registry, 2) identify any differences in these associations across age groups and 3) evaluate the extent to which these associations differ based on the gender of the parent (i.e. mothers and fathers) and the gender of the offspring (male and female).
Methods
Data Sources
All live-born children and new residents in Denmark are assigned a unique personal identification (CRS) number, which can be used to link information within and across registers. Data for the current study were obtained from the Danish Civil Registry (Pedersen et al. 2006, 2011), which contains information on sex, date of birth, place of birth, vital status, and parents’ CRS numbers, and the Danish Psychiatric Central Research Register (Mors et al. 2011), which contains information on all psychiatric inpatient admission dates and diagnoses since 1969 and all outpatient admission dates and diagnoses since 1995. Psychiatric diagnoses are based on the International Classification of Diseases 8th Revision (World Health Organization 1971) for admissions occurring between 1969 and 1993 and the International Classification of Diseases 10th Revision (World Health Organization 1994) for admissions occurring after 1993. There are no private psychiatric inpatient facilities in Denmark, which ensures that all psychiatric admissions are represented in the register.
Study Design
We established a population-based cohort that included all individuals born in Denmark in 1955 or later with links to both parents in the registries who were alive on their 10th birthday. Only individuals born after 1955 were included in the study sample because these individuals have a high probability of registered links to both parents in the Civil Registry. We followed this cohort from their 10th birthday (at which point they became ‘at risk’ for depression) or January 1, 1995, whichever came later, until the date of their first unipolar depression diagnosis, the date of death, the date of emigration/disappearance or January 1, 2012, whichever came first.
Measures
Exposures
We created 2 categorical variables one for mothers and one for fathers - where 0 = no psychiatric diagnosis, 1 = other psychiatric diagnoses (ICD-8 codes 290.0–315.9 besides those in other categories; ICD-10 F-codes not included in other categories), 2 = anxiety (ICD-8 code 300 (excludes 300.4); ICD-10 codes F40, F41, F42), 3 = unipolar depression (ICD-8 codes 296.0, 296.2, 298.0, 300.4; ICD-10 codes F32, F33), 4 = bipolar disorder (ICD-8 codes 296 (excluding: 296.0, 296.2, 296.8), 298.1; ICD-10 codes F30, F31) and 5 = schizophrenia (ICD-8 codes 295 (excluding: 295.7; ICD-10 codes F20). These variables were hierarchical, meaning that parents were placed in the category of their most severe diagnosis, and time dependent, meaning that if a parent was diagnosed with a psychiatric disorder during the follow-up period, or received a more severe psychiatric diagnosis during the follow-up period, he or she could switch from one level of the categorical variable to another.
To illustrate what this hierarchical operationalization means in practice, a parent in the depression category may have previously received an anxiety diagnosis, but he or she would not have received a bipolar or schizophrenia diagnosis. Someone in the schizophrenia category may have a previous history of other psychiatric diagnoses or they may not, but the analyses will treat them the same as someone who only ever received a schizophrenia diagnosis. To illustrate what we mean by time-dependent, if a mother received a diagnosis of depression before her child was born, the child would contribute to the ‘mother with depression category’ starting when he or she reached the age of 10 and became at risk for unipolar depression. But if the mother went on to receive a diagnosis of schizophrenia when her child was 15, the child would contribute to the ‘mother with schizophrenia’ category (and not the ‘mother with depression’ category) from that point onward.”
Outcomes
The primary outcomes of interest were the incidence rates of outpatient and inpatient depression (ICD-10 codes F32, F33). Individuals admitted for inpatient and outpatient treatment on the same day were included in the inpatient group.
Statistical analyses
We conducted survival analyses using Poisson regressions (Andersen et al., 1993), with the logarithm of person-years as an offset variable. This method is equivalent to the Cox regression under the assumption of piecewise constant incident rates (Andersen et al. 1993; Laird & Olivier 1981). The exponentiated estimate in a Poisson regression is the incidence rate ratio (IRR). Analyses were conducted using the GENMOD procedure in SAS software version 9.2 (SAS Institute Inc, Cary, NC). P values were based on the Wald test statistic (p < .05 was considered statistically significant), and 95% confidence intervals (CIs) were based on the assumption of the lognormal distribution of the IRR estimate.
We first examined the overall effects of having a mother or father with any psychiatric diagnosis, after which we examined the effects of individual diagnoses separately by including mutually exclusive dichotomous indicator variables in the analyses with 0 = no psychiatric diagnosis as the reference category. All models were mutually adjusted for maternal and paternal history of psychiatric diagnoses as well as sex, age in one year bands (10, 11, 12, …, 60), calendar time in one year bands (1995, 1996, 1997, …, 2011), place of birth (Capital (i.e. Copenhagen), suburb of capital, provincial city; city with more than 100 000 inhabitants, provincial town; city with more than 10,000 inhabitants and rural areas) and maternal and paternal age at birth (<20, 20–24, 25–29, 30–34 and 35 +). Age and calendar time were treated as time-dependent variables, while all other variables were treated as fixed variables.
We tested for statistically significant differences (i.e. interactions) in the effects of maternal/paternal history of psychiatric diagnoses on the rates of outpatient and inpatient depression for different age groups and between genders. We also tested for differences in the effect of the interaction between age and parental gender on the rates of depression for outpatient vs. inpatient and for males vs. females (i.e. three-way interactions).
Results
Characteristics of the study sample
Sample characteristics are shown in Table 1. The study sample included 2,976,264 individuals, 1,535,097 male (52%) and 1,441,167 female (48%). Of these, 61,939 (2%) experienced an episode of unipolar depression after 1995: 47,562 (77%) outpatient and 14,377 (23%) inpatient. Average age of onset was 30.5 years (SD = 10.2 years) for outpatient and 33.6 years (SD = 9.7) for inpatient cases. 65% of outpatient and 58% of inpatient cases were female. Average age of first depression diagnosis was 30.28 years for females (SD = 9.95) and 32.77 years for males (SD = 10.27).
Table 1.
Sample characteristics: N or mean (% or SD)
| Total Sample | Outpatient Depression Cases | Inpatient Depression Cases | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Male (n=1,535,097) |
Female (n=1,441,167) |
Overall (N=2,976,264) |
Male (n=16,802) |
Female (n=30,760) |
Overall (n=47,562) |
Male (n=6,016) |
Female (n=8,361) |
Overall (n=14,377) |
|
| Age at first onset | - | - | - | 31.9(10.4) | 29.7(9.9) | 30.5(10.2) | 35.2(9.4) | 32.5(9.7) | 33.6(9.7) |
| Parental age at birth: | |||||||||
| Father | 30.1(6.2) | 30.0(6.2) | 30.05(6.17) | 29.5(6.5) | 29.4(6.4) | 29.5(6.4) | 29.5(6.6) | 29.4(6.6) | 29.5(6.4) |
| Mother | 27.0(5.2) | 27.0(5.2) | 26.98(5.20) | 26.3(5.4) | 26.2(5.3) | 26.3(5.3) | 26.1(5.5) | 26.1(5.4) | 26.1(5.4) |
| Place of birth: | |||||||||
| Capital | 233,966(15.2) | 219,000(15.2) | 452,966(15.2) | 2,992(17.8) | 4,892(15.9) | 7,884(16.6) | 1,042(17.3) | 1,489(17.8) | 2,531(17.6) |
| Suburb of capital | 165,409(10.8) | 157,755(11.0) | 323,164(10.9) | 1,787(10.6) | 3,349(10.9) | 5,136(10.8) | 527(8.8) | 917(10.9) | 1,444(10.0) |
| Provincial city | 192,801(12.6) | 181,726(12.6) | 374,527(12.6) | 2,180(13.0) | 3,817(12.4) | 5,997(12.6) | 779(13.0) | 1,045(12.5) | 1,824(12.7) |
| Provincial town | 502,466(32.7) | 471,174(32.7) | 973,640(32.7) | 5,752(34.2) | 10,616(34.5) 16,368(34.4) | 2,199(36.6) | 2,870(34.3) | 5,069(35.3) | |
| Rural areas | 440,455(28.7) | 411,512(28.6) | 851,967(28.6) | 4,091(24.4) | 8,086(26.3) | 12,177(25.6) | 1,469(24.4) | 2,040(24.4) | 3,509(24.4) |
Parental psychiatric diagnoses and rate of outpatient depression
Both maternal (IRR = 1.88, 95% CI [1.83, 1.93]; p < .0001) and paternal (IRR = 1.68, 95% CI [1.63, 1.72]; p < .0001) histories of psychiatric diagnoses significantly increased the incidence rate of outpatient depression relative to no maternal or paternal history of psychiatric diagnosis. As shown in Table 2, the pattern of results for the different diagnostic categories was similar for maternal and paternal history: Overall, parental history of affective disorders (unipolar depression and bipolar disorder) had a greater impact on incidence rates of outpatient depression than parental history of anxiety, schizophrenia, or other psychiatric diagnoses. There was a statistically significant overall interaction between the effects of maternal history and gender (χ2(5, N = 2,976,264) = 13.90, p = .02), and an almost significant overall interaction between the effects of paternal history and gender (χ2(5, N = 2,976,264) = 10.74, p = .06). With the exceptions of maternal history of schizophrenia and ‘other’ diagnoses, parental history exerted a stronger effect on the incidence rate of outpatient depression in males than in females (Table 2).
Table 2.
Parental history of psychiatric disorders and incidence rate ratios of inpatient and outpatient unipolar depression
| Outpatient Depression Cases | Inpatient Depression Cases | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Male | Female | Overall | Male | Female | Overall | |
|
| ||||||
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Mothers: | ||||||
| No diagnosis | 1.00 (ref) | 1.00(ref) | 1.00(ref) | 1.00 (ref) | 1.00(ref) | 1.00(ref) |
| Other diagnosis | 1.73 (1.63, 1.83) | 1.76 (1.69, 1.84) | 1.75 (1.69, 1.81) | 1.79 (1.63, 1.98) | 1.81 (1.67, 1.97) | 1.80 (1.69, 1.92) |
| Anxiety | 1.84 (1.66, 2.04) | 1.70 (1.57, 1.84) | 1.75 (1.64, 1.86) | 1.60 (1.32, 1.92) | 1.95 (1.68, 2.25) | 1.80 (1.61, 2.02) |
| Depression | 2.22 (2.08, 2.37) | 2.09 (1.99, 2.20) | 2.14 (2.05, 2.22) | 2.29 (2.06, 2.54) | 2.29 (2.09, 2.50) | 2.29 (2.14, 2.45) |
| Bipolar disorder | 2.41 (2.10, 2.75) | 1.87 (1.66, 2.09) | 2.06 (1.89, 2.25) | 2.24 (1.79, 2.81) | 2.30 (1.90, 2.79) | 2.28 (1.97, 2.63) |
| Schizophrenia | 1.54 (1.26, 1.89) | 1.88 (1.64, 2.16) | 1.76 (1.57, 1.97) | 1.92 (1.42, 2.61) | 2.10 (1.63, 2.71) | 2.02 (1.66, 2.46) |
| Fathers: | ||||||
| No diagnosis | 1.00 (ref) | 1.00(ref) | 1.00(ref) | 1.00 (ref) | 1.00(ref) | 1.00(ref) |
| Other diagnosis | 1.64 (1.55, 1.73) | 1.51 (1.44, 1.57) | 1.55 (1.50, 1.61) | 1.63 (1.48, 1.79) | 1.59 (1.46, 1.72) | 1.60 (1.51, 1.71) |
| Anxiety | 1.84 (1.56, 2.16) | 1.66 (1.47, 1.89) | 1.72 (1.56, 1.90) | 1.97 (1.52, 2.57) | 1.92 (1.53, 2.95) | 1.94 (1.64, 2.30) |
| Depression | 2.08 (1.91, 2.25) | 1.88 (1.76,2.00) | 1.95 (1.85, 2.05) | 2.47 (2.18, 2.79) | 2.19 (1.96, 2.44) | 2.30 (2.12, 2.50) |
| Bipolar disorder | 2.22 (1.88, 2.62) | 1.91 (1.67, 2.18) | 2.02 (1.82, 2.24) | 2.26 (1.73, 2.95) | 1.73 (1.34, 2.24) | 1.95 (1.62, 2.35) |
| Schizophrenia | 1.80 (1.45, 2.29) | 1.69 (1.44, 1.98) | 1.73 (1.52, 1.96) | 2.32 (1.65, 3.25) | 2.53 (1.94, 3.25) | 2.44 (1.98, 3.01) |
Note. IRR = incidence rate ratio, CI = confidence interval. Incidence rate ratio estimates originate from an analytic model which included main effects for sex, age, calendar time, place of birth, mothers age at birth, father’s age at birth, mother’s and father’s hierarchical psychiatric diagnoses variables and the interactions of these with sex. Overall estimates obtained from an analytical model with the same parameters, but without the interaction terms.
Parental psychiatric diagnosis and risk for inpatient depression
As with outpatient depression, having either a maternal (IRR = 1.99, 95% CI [1.90, 2.08]; p < .0001) or a paternal (IRR = 1.83, 95% CI [1.74, 1.92]; p < .0001) history of any psychiatric diagnosis significantly increased the incidence rate of inpatient depression. As shown in Table 2, this pattern was similar for maternal and paternal history with respect to other diagnoses, anxiety diagnoses and unipolar depression; however the effect of parental history of bipolar disorder appeared stronger when the affected parent was the mother, and the effect of parental history of schizophrenia appeared stronger when the affected parent was the father. Parental history of schizophrenia and affective disorders had a greater effect on the rate of inpatient depression compared to that of parental history of anxiety or other diagnoses. There were no significant overall interactions between the effects of gender and either maternal (χ2(5, N = 2,976,264) = 2.95, p = .71) or paternal (χ2(5, N = 2,976,264) = 4.09, p = .54) histories.
Parental history of psychiatric disorders by age group
There were no significant three-way interactions between the effects of age, parental history and depression severity (outpatient vs. inpatient) for either maternal (χ2(25, N = 2,976,264) = 36.18, p = .07) or paternal (χ2(25, N = 2,976,264) = 24.33, p = .50) history; therefore all depression cases were analyzed together in subsequent analyses. Likelihood ratio tests comparing models with parental history x age interactions that did not distinguish by parent gender to models which did were statistically significant for both inpatient (LR χ2(41) = 88.77, p < .0001) and outpatient (LR χ2(89) = 297.27, p < .0001) cases, therefore we continued to include separate variables for maternal and paternal history.
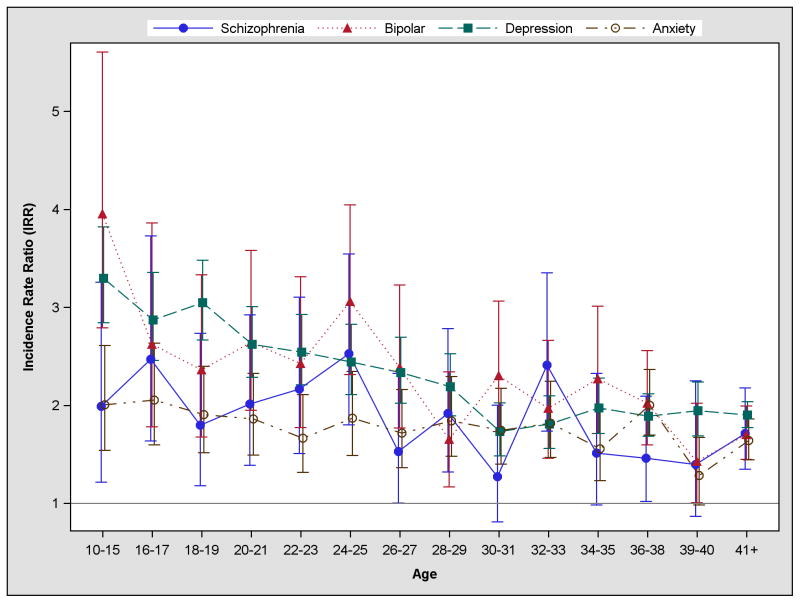
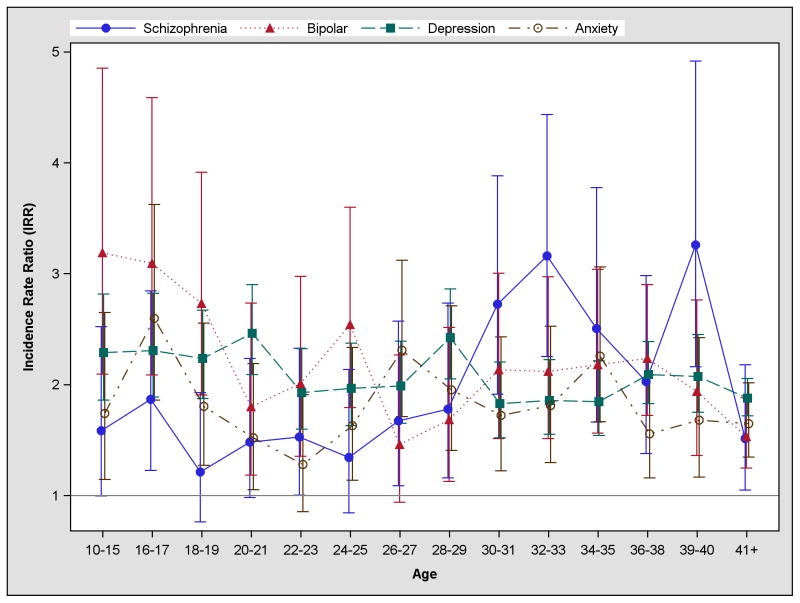
As shown in Figure 1, the effect of maternal history of affective disorders (unipolar and bipolar depression) was strongest in the youngest age group and then decreased steadily with offspring age. The effect of maternal history of anxiety was fairly stable across age groups, while the effect of maternal history of schizophrenia was more variable, but still somewhat stable across age groups. As shown in Figure 2, the effect of paternal history of affective disorders was also strongest at younger ages and decreased over time, although this pattern was less pronounced than for maternal affective disorders (particularly for paternal history of unipolar depression). The effect of paternal anxiety was more variable, but more or less constant across age groups, while the effect of paternal schizophrenia was lower at younger ages and increased with age, peaking among individuals between the ages of 30 and 40 years old. After age 40, the effects of all maternal and paternal diagnoses were more or less equal, ranging from 1.51 (95% CI [1.05, 2.18]) for paternal history of schizophrenia to 1.90 (95% CI [1.77, 2.04]) for maternal history of depression.
Figure 1.
Effects of maternal history of psychiatric diagnoses on the rate of unipolar depression (moderate or severe) by age group
Note. Maternal history of psychiatric diagnosis operationalized as a time-dependent, hierarchical variable, meaning participants were classified based on the most severe psychiatric diagnoses their mothers had received to date. Reference category = no maternal psychiatric diagnosis. Vertical lines represent 95% confidence intervals. Incidence rate ratio estimates originate from a single analytical model which included both the mother’s and the father’s hierarchical psychiatric diagnosis variable. Model adjusted for sex, calendar time, place of birth and paternal psychiatric diagnoses.
Figure 2.
Effects of paternal history of psychiatric diagnoses on the rate of unipolar depression (moderate or severe) by age group
Note. Paternal history of psychiatric diagnosis operationalized as a time-dependent, hierarchical variable, meaning participants were classified based on the most severe psychiatric diagnoses their fathers had received to date. Reference category = no paternal psychiatric diagnosis. Vertical lines represent 95% confidence intervals. Model adjusted for sex, calendar time, place of birth and maternal psychiatric diagnoses.
Discussion
Our goal in this study was to examine the associations between parental psychiatric diagnoses (anxiety, unipolar depression, bipolar disorder and schizophrenia) and incidence rates of inpatient and outpatient unipolar depression by age and gender. The main findings of the study are as follows: first, all parental psychiatric diagnoses increased rates of inpatient and outpatient unipolar depression relative to no parental history of psychiatric disorders. Second, the effect of parental history of affective disorders (unipolar or bipolar) was strongest at younger ages, and decreased as the cohort aged, while the effects of maternal and paternal history of anxiety and the effect of maternal history of schizophrenia were more stable across age groups and the effect of paternal history of schizophrenia was actually stronger when offspring were older. Finally, at younger ages the effect of parental history of affective disorders was stronger than the effect of parental history of other psychiatric disorders; however after age 40, the effects of the different parental diagnoses on rates of depression were more or less equal.
To our knowledge, only two previous studies have examined the association between parental psychopathology and depression risk among offspring of older ages: Dean et al. (2010) used data from the Danish psychiatric registry to examine the impact of having 0, 1 or both parents with a history of non-affective psychosis, affective psychosis or ‘other’ diagnoses on psychopathology in offspring ages 14–42 and found a 1.52–2.91 fold increase in rates of affective disorders associated with all three categories. Weissman et al. (2006) followed 151 offspring of depressed parents from childhood until a mean age of 35 and found a 3-fold increase in risk for depression among children of depressed parents relative to children of controls. This is slightly larger than the effect of parental affective disorders found in the present study, which was closer to a 2-fold increase. When we examined the associations separately by age, however, we saw an approximately 3-fold increase in depression rates for younger age groups, similar to that observed by Weissman and colleagues. Weissman et al. (2006) also found evidence consistent with the current findings that depression risk among the offspring of depressed parents was higher at younger ages, although this effect was not statistically significant.
Parental history and age of onset of depression
The idea that parental history of depression is associated with earlier age of depression onset is far from new: family studies suggested early on that the prevalence of depression was higher among first-degree relatives of depressed individuals with an earlier age of onset (Puig-Antich et al. 1989; Weissman et al. 1984d; Wickramaratne & Weissman 1998). One such study (Weissman et al. 1984d) also found that the prevalence of depression in relatives of depressed probands with an age of onset around 40 was almost equivalent that of the relatives of control subjects, suggesting that the association between parental depression and offspring depression risk may shrink to nothing as offspring approach middle life (Weissman et al. 1984d). In the current study, parental history remained a statistically significant risk factor for depression among individuals over 40; however the effect was demonstrably attenuated relative to the effect in younger age groups. The effects of all types of parental psychopathology on depression rates were roughly equal after age 40, which raises the possibility that it may be parental psychopathology in general, rather than any one disorder in particular, which confers risk for depression in middle life.
Parental history and depression severity
In addition to differences in average age of onset, several studies have found evidence suggesting that parental history of depression is associated with greater severity of depression in offspring (Lieb et al. 2002; Orvaschel et al. 1988). The results of the current study were mixed in this regard: overall the effects of parental psychiatric diagnoses were similar for inpatient and outpatient cases. The exception was parental history of schizophrenia (particularly paternal history of schizophrenia), which had a stronger impact on rates of inpatient depression than on outpatient depression. One possible explanation for this is that a family history of schizophrenia confers risk for a more severe type of depression, which is more likely to require inpatient treatment. Another possibility is that individuals who exhibit psychotic features, and are therefore more likely to be treated in an inpatient setting, may have received a depression diagnoses in error. Research suggests that as many as 16% of individuals originally diagnosed with depression in the Danish registers will receive a diagnosis of a schizophrenia-spectrum disorder by their 10th contact with the treatment system (Kessing 2005). Whether this indicates that the original diagnosis was mistaken, or that depression may for some individuals represent a prodromal phase of schizophrenia, is unclear from the data at hand.
Mechanisms of Transmission
Some of the association between parental psychopathology and depression is certainly due to genetic factors, however there are other possible mechanisms through which psychiatric disorders in parents can influence depression risk in offspring, particularly younger offspring: Depression has been shown to negatively impact parenting behavior in both mothers (Goodman 2007; Lovejoy et al. 2000) and fathers (Wilson & Durbin 2010), which has in turn been shown to increase risk for depression in offspring (Browne et al. 1995). Parental psychopathology, particularly depression, has also been shown to be associated with marital discord and divorce (Burke 2003), which are associated with offspring depression risk (Donahue et al. 2010). As with most of the parental history literature, the majority of studies of psychosocial mechanisms have focused exclusively on parental history of depression. A notable exception is a study by Johnson et al. (2001) in which the authors demonstrated that maladaptive parental behavior mediated the association between a wide array of parental psychiatric disorders including anxiety, depression, disruptive behavior, personality disorders and substance abuse, and risk for psychiatric disorders (including depression) in offspring. In addition, parental history of other psychiatric disorders besides depression, particularly severe disorders like bipolar disorder or schizophrenia which require extended periods of hospitalization, may expose children to stressful circumstances including prolonged parental separation, which is associated with depression later in life (Culpin et al. 2013; Roy 1985).
Parental history, depression and gender
Literature on the potential role of gender (both of the parent and of the offspring) as a moderator of the effects of parental history of psychiatric disorders on offspring depression risk is mixed. While some studies have found evidence to suggest that maternal psychopathology has a greater impact on offspring risk than paternal psychopathology (Johnson et al. 2006; Landman-Peeters et al. 2008; Low et al. 2012; Merikangas et al. 1988), other studies have found no evidence that the effect is different for mothers and fathers (Dean et al. 2010; Kendler et al. 1997; Lieb et al. 2002; Weissman et al. 1987). Similarly, there is disagreement in the literature regarding the effect of offspring gender: several studies found evidence that parental psychopathology has a greater impact on depression risk for girls (Klein et al. 1988; Landman-Peeters et al. 2008; Morris et al. 2014), while others found no evidence of gender differences (Ohannessian et al. 2005). In this study, we found a significant interaction between parental history and offspring gender, but in the opposite direction from previous studies: parental history of affective disorders had a greater effect on males than on females. This suggests that even if, as previous studies have suggested, parental history has a greater impact on depression risk in girls than in boys, parental history may have a greater impact on rates of treatment seeking for males than for females (at least in cases of moderate depression). Stigma towards mental health treatment seeking is generally higher among men than among women (Coppens et al. 2013). It is possible that having a parent with a history of mental illness helps men to overcome their stigma towards seeking treatment for their own depressive symptoms; however this theory requires further study.
We also found a statistically significant three-way interaction between parental history, offspring age and parental gender. This finding might be a simple statistical vagary; however there is precedent from both the biological and behavioral literatures suggesting that the impact of parental psychopathology on offspring depression risk at different ages may vary depending on whether the affected parent is the individual’s mother or father. From a biological perspective, studies on genetic imprinting in mice have found that the same allele may be expressed differently depending on whether it was inherited from the mother or the father (Garfield et al. 2011), and there is evidence in humans that gene expression changes with age (Steegenga et al. 2014). From a behavioral perspective, a mother is typically her child’s primary caregiver during childhood and adolescence, therefore it is to be expected that mothers’ mental states will have a greater impact than fathers’ on rates of depression in younger offspring.
Limitations
Several methodological considerations should be taken into account when interpreting these results. First, only individuals who received treatment in a psychiatric facility (inpatient or outpatient) were counted as cases. Psychiatric treatment in Denmark is free, so there are few (if any) financial barriers to treatment. But individuals with milder symptoms may not have been treated in psychiatric facilities either because a) they did not perceive their symptoms as a mental illness and therefore did not seek treatment, or b) they chose to seek treatment via their primary care provider. Additionally, individuals with very severe depression who committed suicide without ever receiving treatment were also not included in the study sample. As a result, the cases in this sample may not reflect the true underlying distribution of depression severity within the Danish population.
Because the registry only includes outpatient data from 1995 onwards, some parents who experienced moderate psychopathology before 1995 may have been misclassified. This is more likely for disorders such as anxiety or depression which are often treated in an outpatient setting. In addition, parents with anxiety and depression may have been less likely to seek or receive treatment than parents with schizophrenia or bipolar disorder, meaning that misclassification may have been differential across psychiatric diagnoses. Finally, although all models were mutually adjusted for maternal and paternal diagnoses, they did not incorporate possible effects of psychiatric comorbidity in parents (i.e. depression and anxiety vs. depression alone). Exploring complex effects of comorbid disorders in parents on depression risk across the lifespan is beyond the scope of the current study, but would likely be a fruitful line of inquiry for future research.
The fact that cases were defined by treatment introduces a potential source of bias into the study, as the children of parents with a history of mental illness may be more likely to seek treatment for depressive symptoms than the children of families without a history of mental illness (Kendler 1995; Lieb et al. 2002). This may be particularly true for individuals with a parental history of affective disorders, as they may be more likely to recognize their symptoms as indicative of mental illness.
Conclusion
The results of this study suggest that parental history of any psychiatric diagnosis is associated with increased rates of depression relative to no parental history of psychopathology. The effect of parental history of affective disorders (unipolar or bipolar) is strongest at younger ages, while the effects of parental history of anxiety appear stable across age and the effect of paternal history of schizophrenia may actually be stronger at older ages. After age 40, the effects of different parental diagnoses are similar in magnitude, suggesting that it may be parental psychopathology in general, rather than any one disorder specifically, that confers risk for depression in middle life.
Acknowledgments
This work was supported by an unrestricted grant from the Lundbeck Foundation: The Lundbeck Foundation Initiative for Integrative Psychiatric Research (iPSYCH). The first author receives funding for doctoral training from the National Institute of Mental Health Psychiatric Epidemiology Institutional Training Grant (grant number 2T32MH014592-36). Dr. Trine Munk-Olsen receives funding from NIH grant number R01MH104468. The funding sources had no role in the design or conduct of the study; collection management, analysis or interpretation of the data; preparation, review or approval of the manuscript; or decision to submit the manuscript for publication. The authors have no conflicts of interest, financial or otherwise, to disclose. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Andersen PK, Borgen O, Gill RD, Keiding N. Statistical models based on counting processes. New York, NY: Springer-Verlag; 1993. [Google Scholar]
- Argyropoulos SV, Landau S, Kalidindi S, Toulopoulou T, Castle DJ, Murray RM, Picchioni MM. Twins discordant for schizophrenia: Psychopathology of the non-schizophrenic co-twins. Acta Psychiatrica Scandinavica. 2008;118:214–219. doi: 10.1111/j.1600-0447.2008.01205.x. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Keller MB, Seifer R, Lavori PW, Staley J, Podorefsky D, Shera D. Prediction of adolescent affective disorder: Effects of prior parental affective disorders and child psychopathology. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:279–288. doi: 10.1097/00004583-199603000-00008. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Keller MB, Lavori PW, Klerman GK. Psychiatric disorder in adolescent offspring of parents with affective disorder in a non-referred sample. Journal of Affective Disorders. 1988;15:313–322. doi: 10.1016/0165-0327(88)90028-6. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Hirschfeld-Becker DR, Friedman D, Robin JA, Rosenbaum JF. Patterns of psychopathology and dysfunction in high-risk children of parents with panic disorder and major depression. American Journal of Psychiatry. 2001;158:49–57. doi: 10.1176/appi.ajp.158.1.49. [DOI] [PubMed] [Google Scholar]
- Billings AG, Moos RH. Children of parents with unipolar depression: A controlled 1-year follow-up. Journal of Abnormal Child Psychology. 1986;14:149–166. doi: 10.1007/BF00917230. [DOI] [PubMed] [Google Scholar]
- Browne MA, Joyce PR, Wells JC, Bushnell JA, Hornblow AR. Adverse parental behavior and other childhood experiences as risk factors for depression in women aged 18–44. Journal of Affective Disorders. 1995;34:13–23. doi: 10.1016/0165-0327(94)00099-u. [DOI] [PubMed] [Google Scholar]
- Burke L. The impact of maternal depression on family relationships. International Review of Psychiatry. 2003;15:243–255. doi: 10.1080/0954026031000136866. [DOI] [PubMed] [Google Scholar]
- Cerda M, Sagdeo A, Johnson G, Galea S. Genetic and environmental influences on psychiatric comorbidity: A systematic review. Journal of Affective Disorders. 2010;126:14–38. doi: 10.1016/j.jad.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coppens E, Van Audenhove C, Scheerder G, Arensman E, Coffey C, Costa S, Koburger N, Gottlebe K, Gusmao R, O’Connor R, Postuvan V, Sarchiapone N, Sisask M, Szekely A, van der Feltz-Cornelis C, Hegerl U. Public attitudes toward depression and help-seeking in four European countries baseline survey prior to the OSPI-Europe intervention. Journal of Affective Disorders. 2013;150:320–329. doi: 10.1016/j.jad.2013.04.013. [DOI] [PubMed] [Google Scholar]
- Culpin I, Heron J, Araya R, Melotti R, Joinson C. Father absence and depressive symptoms in adolescence: Findings from a UK cohort. Psychological Medicine. 2013;43:2615–2626. doi: 10.1017/S0033291713000603. [DOI] [PubMed] [Google Scholar]
- Dean K, Stevens H, Mortensen PB, Murray RM, Walsh E, Pedersen CB. Full spectrum of psychiatric outcomes among offspring with parental history of mental disorder. Archives of General Psychiatry. 2010;67:822–829. doi: 10.1001/archgenpsychiatry.2010.86. [DOI] [PubMed] [Google Scholar]
- Demirkan A, Penninx BW, Hek K, Wray NR, Amin N, Aulchenko YS, van Dyck R, de Geus EJ, Hofman A, Uitterlinden AG, Hottenga JJ, Noben WA, Oostra BA, Sullivan PF, Willemsen G, Zitman FB, Tiemeier H, Janssens AC, Boomsma DI, van Duijn CM, Middeldorp CM. Genetic risk profiles for depression and anxiety in adult and elderly cohorts. Molecular Psychiatry. 2011;16:773–783. doi: 10.1038/mp.2010.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donahue KL, D’Onofrio BM, Bates JE, Lansford JE, Dodge KA, Pettit GS. Early exposure to parents’ relationship instability: Implications for sexual behavior and depression in adolescence. Journal of Adolescent Health. 2010;47:547–554. doi: 10.1016/j.jadohealth.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfield AS, Cowley M, Smith FM, Moorwood K, Stewart-Cox JE, Gilroy K, Baker S, Xia J, Dalley JW, Hurst LD, Wilkinson LS, Isles AR, Ward A. Distinct physiological and behavioural functions for parental alleles of imprinted Grb10. Nature. 2011;469:534–538. doi: 10.1038/nature09651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershon ES, Hamovit J, Guroff JJ, Dibble E, Leckman JF, Sceery W, Targum SD, Nurberger JI, Jr, Goldin LR, Bunney WE., Jr A family study of schizoaffective, bipolar I, bipolar II, unipolar, and normal control probands. Archives of General Psychiatry. 1982;39:1157–1167. doi: 10.1001/archpsyc.1982.04290100031006. [DOI] [PubMed] [Google Scholar]
- Goodman SH. Depression in mothers. Annual Review of Clinical Psychology. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- Hammen C, Burge D, Burney E, Adrian C. Longitudinal study of diagnoses in children of women with unipolar and bipolar affective disorder. Archives of General Psychiatry. 1990;47:1112–1117. doi: 10.1001/archpsyc.1990.01810240032006. [DOI] [PubMed] [Google Scholar]
- Henin A, Biederman J, Mick E, Sachs GS, Hirshfeld-Becker D, Siegel RS, McMurrich S, Grandin L, Nierenberg AA. Psychopathology in the offspring of parents with bipolar disorder: A controlled study. Biological Psychiatry. 2005;58:554–561. doi: 10.1016/j.biopsych.2005.06.010. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Smailes E, Brook JS. Association of maladaptive parental behavior with psychiatric disorder among parents and their offspring. Archives of General Psyciatry. 2001;58:453–460. doi: 10.1001/archpsyc.58.5.453. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Brook JS. A multiwave multi-informant study of the specificity of the association between parental and offspring psychiatric disorders. Comprehensive Psychiatry. 2006;47:169–177. doi: 10.1016/j.comppsych.2005.05.005. [DOI] [PubMed] [Google Scholar]
- Kendler KS. Is seeking treatment for depression predicted by a history of depression in relatives? Implications for family studies of affective disorder. Psychological Medicine. 1995;25:807–814. doi: 10.1017/s0033291700035054. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Davis CG, Kessler RC. The familial aggregation of common psychiatric and substance use disorders in the national comorbidity survey: A family history study. The British Journal of Psychiatry. 1997;170:541–548. doi: 10.1192/bjp.170.6.541. [DOI] [PubMed] [Google Scholar]
- Kessing LV. Diagnostic stability in depressive disorder as according to ICD-10 in clinical practice. Psychopathology. 2005;38:32–37. doi: 10.1159/000083968. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Klein DN, Lewinsohn PM, Rohde P, Seeley JR, Olino TM. Psychopathology in the adolescent and young adult offspring of a community sample of mothers and fathers with major depression. Psychological Medicine. 2005;35:353–365. doi: 10.1017/s0033291704003587. [DOI] [PubMed] [Google Scholar]
- Klein DN, Clark DC, Dansky L, Margolis ET. Dysthymia in the offspring of parents with primary unipolar affective disorder. Journal of Abnormal Psychology. 1988;97:265–274. doi: 10.1037//0021-843x.97.3.265. [DOI] [PubMed] [Google Scholar]
- Klein DN, Lewinsohn PM, Seeley JR, Rohde P. A family study of major depressive disorder in a community sample of adolescents. Archives of General Psychiatry. 2001;58:13–21. doi: 10.1001/archpsyc.58.1.13. [DOI] [PubMed] [Google Scholar]
- Laird N, Olivier D. Covariance analysis of censored survival data using log-linear analysis techniques. Journal of the American Statistical Association. 1981;76:231–240. [Google Scholar]
- Landman-Peeters KM, Ormel J, Van Sonderen EL, Den Boer JA, Minderaa RB, Hartman CA. Risk of emotional disorder in offspring of depressed parents: Gender differences in the effect of a second emotionally affected parent. Depression and Anxiety. 2008;25:653–650. doi: 10.1002/da.20350. [DOI] [PubMed] [Google Scholar]
- Lee SH Cross Disorder Group of the Psychiatric Genomics Consortium. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nature Genetics. 2013;45:984–995. doi: 10.1038/ng.2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieb R, Isensee B, Hofler M, Pfister H, Wittchen HU. Parental major depression and the risk of depression and other mental disorders in offspring. Archives of General Psychiatry. 2002;59:365–374. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Low NC, Dugas E, Constantin E, Karp I, Rodriguez D, O’Loughlin J. The association between parental history of diagnosed mood/anxiety disorders and psychiatric symptoms and disorders in young adult offspring. BMC Psychiatry. 2012;12 doi: 10.1186/1471-244X-12-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuffin P, Rijsdijk F, Andrew M, Shan P, Katz R, Cardno A. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Archives of General Psychiatry. 2003;60:497–502. doi: 10.1001/archpsyc.60.5.497. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Risch NJ, Weissman MM. Comorbidity and co-transmission of alcoholism, anxiety and depression. Psychological Medicine. 1994;24:69–80. doi: 10.1017/s0033291700026842. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Prusoff BA, Weissman MM. Parental concordance for affective disorders: Psychopathology in offspring. Journal of Affective Disorders. 1988;15:279–290. doi: 10.1016/0165-0327(88)90025-0. [DOI] [PubMed] [Google Scholar]
- Middeldorp CM, Cath DC, van Dyck R, Boomsma DI. The co-morbidity of anxiety and depression in the perspectives of genetic epidemiology: A review of twin and family studies. Psychological Medicine. 2005;35:611–624. doi: 10.1017/s003329170400412x. [DOI] [PubMed] [Google Scholar]
- Mitchell J, McCauley E, Burke P, Calderon R, Schloredt K. Psychopathology in parents of depressed children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1989;28:352–357. doi: 10.1097/00004583-198905000-00008. [DOI] [PubMed] [Google Scholar]
- Morris BH, McGrath AC, Goldman MS, Rottenberg J. Parental depression confers greater prospective depression risk to females than males in emerging adulthood. Child Psychiatry and Human Development. 2014;45:78–89. doi: 10.1007/s10578-013-0379-5. [DOI] [PubMed] [Google Scholar]
- Mors O, Perto GP, Mortensen PB. The danish psychiatric central research register. Scandinavian Journal of Public Health. 2011;39:54–57. doi: 10.1177/1403494810395825. [DOI] [PubMed] [Google Scholar]
- Orvaschel H, Walsh-Allis G, Ye WJ. Psychopathology in children of parents with recurrent depression. Journal of Abnormal Child Psychology. 1988;16:17–28. doi: 10.1007/BF00910497. [DOI] [PubMed] [Google Scholar]
- Pedersen CB. The danish civil registration system. Scandinavian Journal of Public Health. 2011;39:22–25. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- Pedersen CB, Gøtzsche H, Møller JO, Mortensen PB. The Danish civil registration system: A cohort of eight million persons. Danish Medical Bulletin. 2006;53:441–449. [PubMed] [Google Scholar]
- Puig-Antich J, Goetz D, Davies M, Kaplan T, Davies S, Ostrow L, Asnis L, Twomey J, Lyengar S, Ryan ND. A controlled family history study of prepubertal major depressive disorder. Archives of General Psychiatry. 1989;46:406–418. doi: 10.1001/archpsyc.1989.01810050020005. [DOI] [PubMed] [Google Scholar]
- Radke-Yarrow M, Nottelmann E, Martinez P, Fox MB. Young children of affectively ill parents: A longitudinal study of psychosocial development. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:68–77. doi: 10.1097/00004583-199201000-00011. [DOI] [PubMed] [Google Scholar]
- Roy A. Early parental separation and adult depression. Archives of General Psychiatry. 1985;42:987–991. doi: 10.1001/archpsyc.1985.01790330067008. [DOI] [PubMed] [Google Scholar]
- Steegenga WT, Boekschoten MV, Lute C, Hooiveld GJ, de Groot PJ, Morris TJ, Teschendorff AE, Butcher LM, Beck S, Müller M. Genome-wide age-related changes in DNA methylation and gene expression in human PBMCs. Age. 2014;36:1523–1540. doi: 10.1007/s11357-014-9648-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinhausen HC, Foldager L, Perto G, Munk-Jørgensen P. Family aggregation of mental disorders in the nationwide Danish three generation study. European Archives of Clinical Neuroscience. 2009;259:270–277. doi: 10.1007/s00406-008-0865-0. [DOI] [PubMed] [Google Scholar]
- Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: Review and meta-analysis. The American Journal of Psychiatry. 2000;157:1552–1562. doi: 10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- Thygesen LC, Daasnes C, Thaulow I, Bronnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: Structure, access, legislation and archiving. Scandinavian Journal of Public Health. 2011;39(Suppl 7):12–16. doi: 10.1177/1403494811399956. [DOI] [PubMed] [Google Scholar]
- Todd RD, Geller B, Neuman R, Fox LW, Hickok J. Increased prevalence of alcoholism in relatives of depressed and bipolar children. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:716–724. doi: 10.1097/00004583-199606000-00011. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Kidd KK, Prusoff BA. Variability in rates of affective disorders in relatives of depressed and normal probands. Archives of General Psychiatry. 1982;39:1397–1403. doi: 10.1001/archpsyc.1982.04290120033006. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Gershon ES, Kidd KK, Prusoff BA, Leckman JF, Dibble E, Hamovit J, Thompson D, Pauls DL, Guroff JJ. Psychiatric disorders in the relatives of probands with affective disorders. the yale university--national institute of mental health collaborative study. Archives of General Psychiatry. 1984a;41:13–21. doi: 10.1001/archpsyc.1984.01790120015003. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Prusoff BA, Gammon GD, Merikangas KR, Leckman JF, Kidd KK. Psychopathology in the children (ages 6–18) of depressed and normal parents. Journal of the American Academy of Child Psychiatry. 1984b;23:78–84. doi: 10.1097/00004583-198401000-00011. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Leckman JF, Merikangas KR, Gammon GD, Prusoff BA. Depression and anxiety disorders in parents and children. results from the yale family study. Archives of General Psychiatry. 1984c;41:845–852. doi: 10.1001/archpsyc.1984.01790200027004. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Merikangas KR, Leckman JF, Prusoff BA, Caruso KA, Kidd KK, Gammon GD. Onset of major depression in early adulthood. increased familial loading and specificity. Archives of General Psychiatry. 1984d;41:1136–1143. doi: 10.1001/archpsyc.1984.01790230022003. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Gammon GD, John K, Merikangas KR, Warner V, Prusoff BA, Sholomskas D. Children of depressed parents. increased psychopathology and early onset of major depression. Archives of General Psychiatry. 1987;44:847–853. doi: 10.1001/archpsyc.1987.01800220009002. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Fendrich M, Warner V, Wickramaratne P. Incidence of psychiatric disorder in offspring at high and low risk for depression. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:640–648. doi: 10.1097/00004583-199207000-00010. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Warner V, Wickramaratne P, Moreau D, Olfson M. Offspring of depressed parents. 10 years later. Archives of General Psychiatry. 1997;54:932–940. doi: 10.1001/archpsyc.1997.01830220054009. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. The American Journal of Psychiatry. 2006;163:1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]
- Weller RA, Kapadia P, Weller EB, Fristad M, Lazaroff LB, Preskorn SH. Psychopathology in families of children with major depressive disorders. Journal of Affective Disorders. 1994;31:247–252. doi: 10.1016/0165-0327(94)90100-7. [DOI] [PubMed] [Google Scholar]
- Welner Z, Rice J. School-aged children of depressed parents: A blind and controlled study. Journal of Affective Disorders. 1988;15:291–302. doi: 10.1016/0165-0327(88)90026-2. [DOI] [PubMed] [Google Scholar]
- Wickramaratne PJ, Weissman MM. Onset of psychopathology in offspring by developmental phase and parental depression. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:933–942. doi: 10.1097/00004583-199809000-00013. [DOI] [PubMed] [Google Scholar]
- Wilson S, Durbin CE. Effects of paternal depression on fathers’ parenting behaviors: A meta-analytic review. Clinical Psychology Review. 2010;30:167–180. doi: 10.1016/j.cpr.2009.10.007. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Classification of diseases: Extended danish-latin version of the world health organization international classification of diseases, 8th revision, 1965. Copenhagen: Danish National Board of Health; 1971. [Google Scholar]
- World Health Organization. WHO ICD-10: Mental and behavioural disorders, classification and diagnostic criteria. Copenhagen: Munksgaard Danmark; 1994. [Google Scholar]