Abstract
Sclerotic bone dysplasias are diagnosed based on clinical and radiological features; however, in some instances pose a dilemma. We herewith report a case of a 38-year-old female who presented with right lower extremity pain, and was detected to have sclerotic diaphyseal lesion on X-ray. Triphasic 99mTc methylene diphosphonate (MDP) Bone scan helped in confirming the diagnosis of intramedullary osteosclerosis, a dysplastic bone disorder.
Keywords: Bone scan, intramedullary: Diaphysis, methylene diphosphonate, Single photon emission computed tomography/computed tomography
INTRODUCTION
Sclerotic focal diaphyseal lesions in patients with painful lower limb are routinely evaluated using conventional X-ray imaging. However, radiological features pose a diagnostic dilemma. Triphasic bone scan in our case ruled out common clinical scenarios narrowing the diagnosis to sclerotic dysplasia. This helped in arriving at the diagnosis of intramedullary osteosclerosis (IMOS), with further correlation of clinical and pathological findings.
CASE REPORT
A 38-year-old female presented with complaints of pain in right thigh since 3 months, which gradually increased in intensity. Patient was on anti-inflammatory medications that provided transient pain relief with on and off bouts of pain and difficulty in walking. There was no history of trauma or family history of skeletal disorders. The patient was asymptomatic otherwise. Leukocyte count (5400/mm3), erythrocyte sedimentation rate (15 mm/h), and alkaline phosphatase levels (61 IU/L) were within normal limits. Radiograph (X-ray) of right thigh [Figure 1a and b, arrows], arrows showed diffuse diaphyseal sclerosis with widening of bone and endosteal hyperostosis. The patient was referred for whole body 99mTc-methylene diphosphonate (MDP) bone scan. Triphasic study was performed. Initial vascular phase and blood pool images at 2 min showed no evidence of increased vascularity or soft tissue tracer pooling [Figure 2a–d]. Delayed anterior and posterior planar images showed fusiform-shaped intense area of tracer uptake in the diaphysis of right femur [Figure 3a–d, arrows], corresponding to the site of pain; with similar pattern of tracer localization of lesser intensity in left proximal femoral shaft [Figure 3c and d, arrowheads]. No abnormal tracer uptake was seen in rest of the skeletal system. Fused single photon emission computed tomography/computed tomography (SPECT/CT) images showed tracer localized to intense sclerosis in the intra-medullary region with associated overlying cortical thickening in bilateral femoral diaphysis [Figure 4a–c, right – triangulate, left – arrow], visualized more prominently on right side. CT-guided biopsy was performed. Pathological findings of replacement of normal spongiosa by sclerotic trabeculae devoid of osteocytes with associated degeneration were seen. Since there was no similar family history, correlation of clinical, imaging, and pathological findings yielded the diagnosis of intra-medullary osteosclerosis. The patient was referred for medullary reaming, since pain was not relived by analgesics, and follow-up is awaited.
Figure 1.

Anterior (a) and lateral (b) view radiographs of right femur showing intense intramedullary diaphyseal sclerosis (arrow) with bone widening and endosteal thickening (arrowhead) in the proximal femoral shaft
Figure 2.
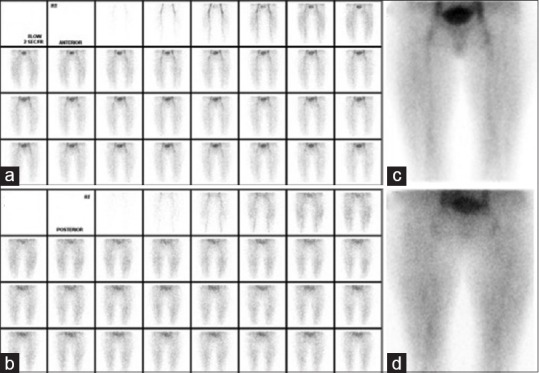
Anterior (a) and posterior flow (b) images obtained by injection of 20 mCi of 99mTc methylene diphosphonate show no evidence of increased vascularity in the region of both femorii. Furthermore, there is no increased pooling of tracer in the region of both femorii on anterior (c) and posterior (d) blood pool images
Figure 3.
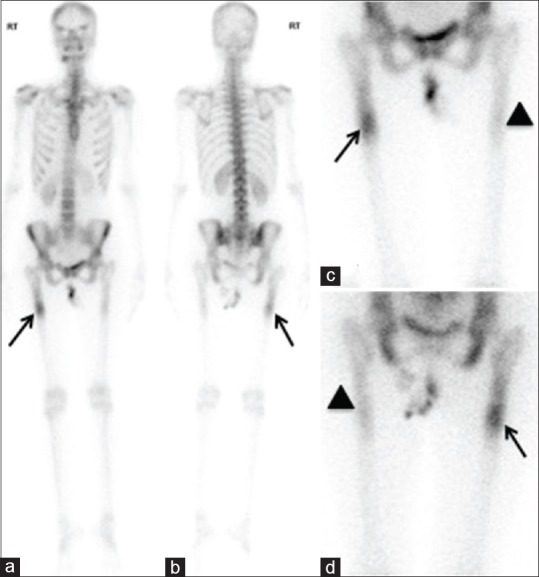
Anterior and posterior whole body planar images acquired at 3 h show focal intense tracer uptake in right proximal femoral shaft (a and b, arrow), with no increased tracer uptake in the rest of the skeletal system. Faint uptake in the left proximal femoral shaft, appreciated better on planar anterior and posterior images of both femorii (c and d, arrowhead)
Figure 4.
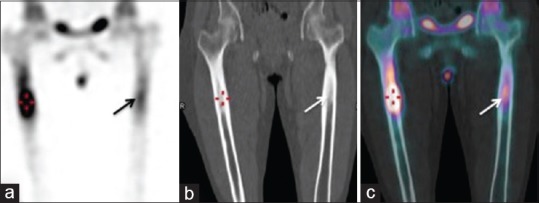
Coronal single photon emission computed tomography image (a) increased focal intense tracer uptake involving diaphysis of both femorii (triangulate – right; arrow – left) proximally, more on the right side, showing intramedullary sclerosis on corresponding low dose coronal CT (b), which is confirmed on fused SPECT/CT images (c)
DISCUSSION
Sclerotic intramedullary lesions on radiographs in patients with painful long bones have a number of differentials such as malignancy (osteosarcoma, lymphoma), infections (osteomyelitis), trauma (stress fracture), or bone dysplasias. Absence of increased vascularity on initial flow images of triphasic bone scan was suggestive of low probability for malignancy, infection and stress fracture. Furthermore, findings of increased tracer uptake predominantly in the medullary cavity and in the thickened cortex, confined to both femoral diaphysis, raised a high possibility of dysplastic bone disorder. Comprehensive analysis of clinical, pathological, and imaging findings helped us confirming the diagnosis of IMOS. IMOS was first described by Abdul-Karim et al[1] in 1988, as an unusual pathological condition characterized by endosteal new bone formation and sclerosis in diaphysis of long bones in adults. It has a higher predominance in women, especially affecting at middle age.[2] Clinically IMOS involves lower extremities, commonly tibia followed by femur, and presents as chronic severe pain unrelieved by non-steroidal anti-inflammatory drugs. Few cases have been reported in literature so far;[3,4,5] with the last one highlighting the role of bone scan. Isolated radiological findings are not diagnostic; hence, the role of triphasic bone scan in ruling out other differentials is valuable. Even then, similar pattern on radiograph and bone scan has been observed in other congenital developmental skeletal dysplasias such as Ribbing disease[6] or Camurati–Engelmann disease.[7] Histologically, Camurati–Engelmann disease demonstrates both osteoclastic and blastic activity, unlike IMOS.[8] However, Ribbing disease and IMOS share the same histological features, hence were close differentials.[9] As in our patient, there was no positive family history, hence Ribbing disease, which is an autosomal recessive inherited disorder, was ruled out. Radiological features in skeletal dysplasias are not pathognomonic of this condition, and triphasic bone scan helps narrow down the differentials. Thus, this case highlights the role of bone scan and demonstrates its imaging features in IMOS. It also underlines the importance of correlating clinical and histological features with imaging findings for accurate diagnosis in bone dysplasias like IMOS, which thereby impacts further management.[10]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Abdul-Karim FW, Carter JR, Makley JT, Morrison SC, Helper SD, Joyce MJ, et al. Intramedullary osteosclerosis. A report of the clinicopathologic features of five cases. Orthopedics. 1988;11:1667–75. doi: 10.3928/0147-7447-19881201-08. [DOI] [PubMed] [Google Scholar]
- 2.Horwitz T. Monomelic medullary osteosclerosis of unknown etiology. Radiology. 1941;36:343–51. [Google Scholar]
- 3.Chanchairujira K, Chung CB, Lai YM, Haghighi P, Resnick D. Intramedullary osteosclerosis: Imaging features in nine patients. Radiology. 2001;220:225–30. doi: 10.1148/radiology.220.1.r01jl24225. [DOI] [PubMed] [Google Scholar]
- 4.Balkissoon AR, Hayes CW. Case 14: Intramedullary osteosclerosis. Radiology. 1999;212:708–10. doi: 10.1148/radiology.212.3.r99se39708. [DOI] [PubMed] [Google Scholar]
- 5.de Vernejoul MC. Sclerosing bone disorders. Best Pract Res Clin Rheumatol. 2008;22:71–83. doi: 10.1016/j.berh.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 6.Seeger LL, Hewel KC, Yao L, Gold RH, Mirra JM, Chandnani VP, et al. Ribbing disease (multiple diaphyseal sclerosis): Imaging and differential diagnosis. AJR Am J Roentgenol. 1996;167:689–94. doi: 10.2214/ajr.167.3.8751682. [DOI] [PubMed] [Google Scholar]
- 7.Bartuseviciene A, Samuilis A, Skucas J. Camurati-Engelmann disease: Imaging, clinical features and differential diagnosis. Skeletal Radiol. 2009;38:1037–43. doi: 10.1007/s00256-008-0642-1. [DOI] [PubMed] [Google Scholar]
- 8.Janssens K, Vanhoenacker F, Bonduelle M, Verbruggen L, Van Maldergem L, Ralston S, et al. Camurati-Engelmann disease: Review of the clinical, radiological, and molecular data of 24 families and implications for diagnosis and treatment. J Med Genet. 2006;43:1–11. doi: 10.1136/jmg.2005.033522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacobson HG. Dense bone – Too much bone: Radiological considerations and differential diagnosis. Part I. Skeletal Radiol. 1985;13:1–20. doi: 10.1007/BF00349088. [DOI] [PubMed] [Google Scholar]
- 10.Noain-Sanz E, Martínez de Morentin-Garraza J, Eslava-Gurrea E. Intramedullary reaming in Ribbing disease. Rev Esp Cir Ortop Traumatol. 2013;57:231–4. doi: 10.1016/j.recot.2013.02.004. [DOI] [PubMed] [Google Scholar]


