Abstract
Background:
One of the most common and important diagnostic methods for the detection of heart diseases is coronary angiography. The aim of this study was to determine the optimum angle of the bed by using vital signals to optimize the patient's position after the angiography.
Materials and Methods:
This study was a randomized clinical trial (RCT) on participants after angiography who were divided into five groups. The first group was placed routinely in a supine position. In the other groups, all of the patients were placed in bed by angle 15°, 30°, 45°, and 60° upward. In each group, vital signals were measured that included blood pressure, percent of blood oxygen saturation, heart rate, respiratory rate, and temperature. All of measured data compared with the pain score has been achieved from numerical pain scale. The data were analyzed by descriptive statistics method, variance analysis, and post hoc tests in the Statistical Package for the Social Sciences (SPSS) software, version 16. Estimation of the relationship was done by MATLAB version 2011. The level of significance was considered to be 0.05.
Results:
In various groups, there was no significance difference in demographic variables such as gender, age, height, and weight. The mean of pain score, heart rate, systolic blood pressure, and respiratory rate changed significantly (P < 0.05) but the temperature variation, blood oxygen saturation, and diastolic blood pressure in subjects were not significant (P > 0.05). It showed linear changes between pain and systolic blood pressure, respiratory rate, and heart rate changes. A dramatic reduction was also seen in systolic blood pressure, respiratory rate, heart rate, and also pain at an angle of 45°.
Conclusion:
This study showed that, 45° was the best angle of the bed to optimize the patient's position after the procedure, based on his/her vital signs and pain score. Thus, in order to relive pain, this change in bed angle is advised to be planned by postangiography nurses in patients after coronary angiography.
Keywords: Coronary angiography, pain, pain score, bed position, vital signals
INTRODUCTION
Due to the increase in life expectancy and also the improvements in treating illnesses, chronic diseases are increasing.[1] Cardiovascular diseases (CVDs) are significant since they are the most common chronic diseases of the 21st century and are regarded as the main cause of disabilities and deaths all over the world.[2] By 2020, ischemic heart disease (IHD) will become the most usual cause of death; in Iran, it is considered as the first cause of mortality in people above 35 years of age up to 2008. Base on this data, CVD is the most dangerous and fatal disease. As coronary artery disease (CAD) accounts for a high percentage of CVD, early diagnosis and treatment will lead to fewer complications and deaths.[3,4] There are some experiments and diagnostic methods that are essential for the timely detection of heart diseases. One of the most common and important diagnostic methods is coronary angiography. This procedure is the gold standard for CAD diagnosis.[5] After angiography, vascular complications (such as bleeding, hematoma, and distal emboli due to trauma caused in the artery wall) are the most common complications of catheterization. One of the measures of care taken to reduce these complications is taking complete or relative rest for 10 h or 24 h without moving the legs.[6] Although it is accepted by a majority of specialists, unsuitable position and excessive immobility in the bed after angiography cause patients to experience pain in their lower back. Lunden et al. conducted a qualitative study and assessed the patient's responses after angiography; finally, they realized that the pain is frequently reported following cardiac catheterization.[7] Pain is an unpleasant sensory and emotional experience that is created by an annoying stimulation of sensory nerve terminals.[8] Some studies indicate that intramuscular pressure in the lumbar muscles has a direct relation to their positions. Rest in an unchanged position for a long period of time leads to increased tissue pressure and decreased blood supply in the bedridden patient.[9] In a parallel manner, activation of the sympathetic system and catecholamine release due to pain cause to increases blood pressure, heart rate, and respiratory rate, and decreases respiratory volume (with a greater impact on tidal volume) and finally myocardial infarction.[10,11,12,13,14,15]
Thus, given the possibility of cardiovascular system involvement in the patient who undergoes angiography, the necessity of prevention and control of pain is very important; there is no scientific support for any current method,[2] Therefore, changing the exhaustion intervention trial (EXIT) treatment method after angiography (which includes complete rest on the back and an unchanging position for a long period of time) and finding an optimal angle of bed to decrease the patient's backache and his/her dissatisfaction could lead to faster improvement and also decrease his/her period of hospitalization. The purpose of our investigation was to determine a suitable position for the patient during complete bed rest and for relieving his/her pain without increasing the probable coronary complications according to some vital signals that confirmed the best position.
MATERIALS AND METHODS
The present study was a clinical trial that was started in June 2013 and completed in December 2013. The sample of this study included all the patients who took to recourse to the angiography center of Imam Ali Hospital in Bojnurd, North Khorasan, Iran for whom nonemergency angiography was performed through the femoral artery based on specified indexes of angiography. The participants were randomly divided into five groups after considering the inclusion and exclusion criteria and obtaining the patients’ consents (which were approved by the ethics committee of the university). The first group was placed routinely in the supine position, quite straight and the head was not placed at any angle. In the second group, all the patients were placed in bed at a 15° upward angle; in the third group, all the patients were placed in bed at a 30° upward angle; in the fourth group, all the patients were placed in bed at a 45° upward angle; and in the fifth group, all the patients were placed in bed at a 60° upward angle. The mean of all mentioned angles is lumbosacral that performed for all patients. It was mentioned that the patients were in a supine position on bed and remained in the same position till the end. The sample study was determined 85 by considering means space and hypothesis of the same study (4) and mean deviations S1 = 1.67 and S2 = 1.22 and means X1 = 2.32 and X2 = 5.78 that in each group, was placed 17 persons. The method of block randomization was used. The exclusion criteria for this study included active bleeding caused by the cutter in the entrance area, existing coagulation disorders, relative time of thromboplastin more than 45 s, chronic back pain history, need for cardiopulmonary resuscitation (CPR) during angiography, existing chest pain with new changes of electrocardiogram (ECG), using warfarin or antipain before the procedure, systolic blood pressure of more than 180 mmHg or diastolic pressure more than 100 mmHg, motion artifact, and consciousness that the patient could not cooperate for change in position. In all the groups, sand bag was placed on the bandage after angiography. Angiocatheter size 16 (gray) [Haryana, India] was used to access the right femoral artery for cauterization. It used the same contrast agent (VISIPAQUE injection 270 mg/20 mL) in a different volume. The cutter was the same in all the patients and it was Judkins series right, left, and pigtail that was used at 3.5, 4, 5, and 6 mm curvatures; also, the guide wire was used in 0.035 and 0.038 cm diameters. The duration of angiography was recorded from the entrance of the cutter into the femoral artery to its exit with a time variation of ±30 s. In all the patients, vital signals were measured 30 min after completing the process that; the vital signs included blood pressure, percent of blood oxygen saturation, heart rate, respiratory rate, and temperature. The Timpani thermometer (Ontario L4Z. V4, Canada) was used for body temperature. The measurement of temperature was carried on only through one ear (right ear) for all of the patients. The other vital signals were measured by a monitoring device. The Numeric Rating Scale (NRS) was used to determine the pain intensity. This scale is a 10-cm horizontal line that is numbered from 0 to 10 (number 0 shows lack of pain and number 10 shows the severest possible pain). The patients were asked to determine the rate of the pain according to the line and numbers. The validity and reliability of this instrument has been evaluated in a similar study.[16] The demographic variables included were age, gender, height, and weight. The statistical analysis was done by Statistical Package for the Social Sciences (SPSS) software version 16. The data were analyzed by descriptive statistics method, variance analysis, and post hoc tests. Estimation of the relationship was done by MATLAB version 2011a. The level of significance was considered to be 0.05. The aim of the study was explained to the patients and their written informed consent was obtained according to the Declaration of Helsinki. Furthermore, it was explained that the patients could withdraw from the study at any time.
This study was approved by the ethics committee of North Khorasan University of Medical Sciences in June 2013 (No 9360542) and complies with the Declaration of Helsinki; informed consent has been obtained from the subjects.
RESULTS
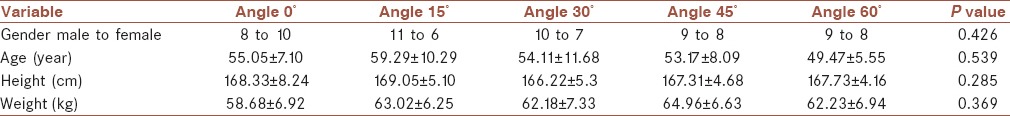
In this study, 86 patients participated. Of these patients, 37 (43%) were males and 49 (57%) were females. For all of the subjects, the mean age was 54.34 ± 7.67 years, mean height 167.42 ± 5.49 cm, and the average weight 61.66 ± 6.25 kg. Each group (proportional to each bed angle) comprised 17 persons and only one group comprised 18 persons with respect by way of random selection. Among the various groups, there was no significance difference in the demographic variables such as gender, age, height, and weight. Table 1 shows the results of change in position and the mean demographic variables, along with standard deviation.
Table 1.
Distribution of the patients in different positions of the bed based on demographic variables (there was no significant difference in any case)
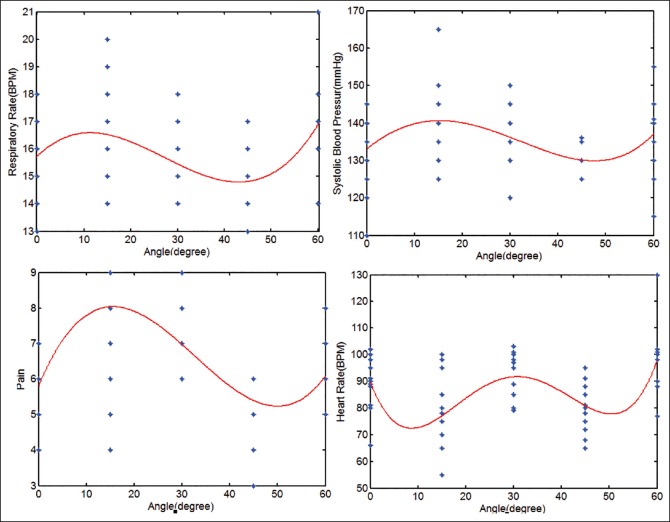
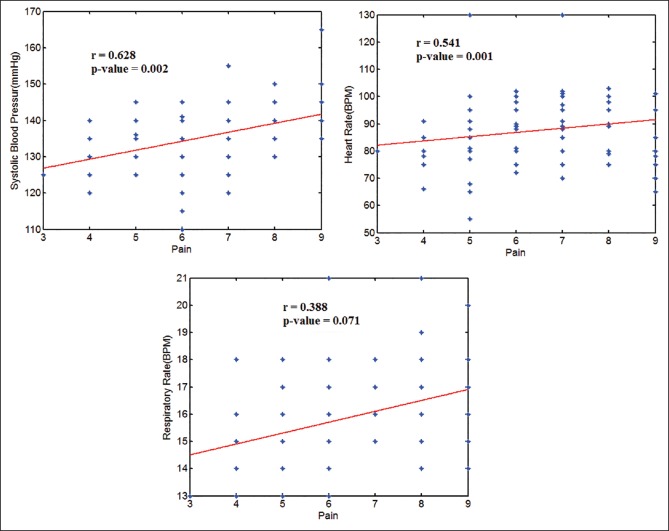
Also, among of the various groups, the pain variables, ambient temperature, percent of blood oxygen saturation, blood pressure, respiratory rate, and heart rate were evaluated. Table 2 shows the mean and standard deviation of the variables in five angles of the bed. By changing the angle of the bed, the mean pain, heart rate, systolic blood pressure, and respiratory rate changed significantly (P < 0.05) but the temperature variation, blood oxygen saturation, and diastolic blood pressure in subjects were not significant (P > 0.05). Figure 1 shows the recording of signal for a subject in 45° angle. Figure 2 shows the relationship between pain, heart rate, systolic blood pressure, and respiratory rate with the angle of the bed. The relationship between the variables and angle changed nonlinearly. A significant reduction was observed in pain, respiratory rate, heart rate, and systolic blood pressure in a 45° angle of the bed. Figure 3 shows the relationship between pain and vital signals. Accordingly, the changes of systolic blood pressure, respiratory rate, and heart rate with pain changed linearly and significantly. The highest correlation was observed between systolic blood pressure and pain (r = 0.62, P value = 0.002). Heart rate changes at 0° angle showed a significant level of difference in comparison to the 15° and 45° angles. Systolic blood pressure and respiratory rate also showed considerable changes in 0° to 15° and 15° to 45°, respectively. Systolic blood pressure and respiratory rate at 15° angle were significantly changed only with 45°. The heart rate also showed changes at 15°, 45°, and 60° angles. The pain changes, respiratory rate, heart rate, and systolic blood pressure were significant in 30° and 45° angles. The pain score also significantly changed at 30° angle compared to 60° angle. A significant correlation was observed between pain and all vital signals in 45° (P < 0.05).
Table 2.
The mean and standard deviation of variables in five angles of the bed
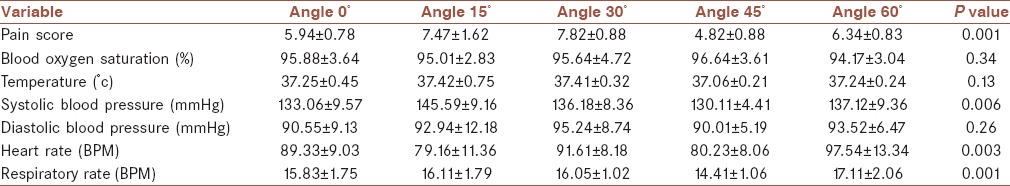
Figure 1.

Recording the signal in 45°
Figure 2.
The relationship between pain and heart rate, systolic blood pressure, and respiratory rate with the angle of the bed
Figure 3.
The relationship between pain and vital signals (systolic blood pressure, heart rate, and respiratory rate)
DISCUSSION
The aim of this study was to determine the optimum angle of the bed by using vital signals to reduce pain after angiography. The results showed a significant correlation between pain levels at different angles. The minimum pain was obtained at an angle of 45° and also vital signals such as heart rate, systolic blood pressure, and respiratory rate were significantly changed at different angles. It showed linear changes between pain and systolic blood pressure, respiratory rate and heart rate changes; also, a dramatic reduction was seen in these parameters at an angle of 45°. This study showed that 45° angle was the best position for the bed in order to reduce the patient's pain after the procedure based on his/her vital signals.
This finding indicates that the patient's recovery after coronary angiography in a flat position causes the experiencing of severe pain. Notably, after the procedure all patients remained in a fixed position of predetermined randomization till the end. Hence, time — a likely cause of reducing the level of pain in various situations during successive survey — in this study was under control. Another strong point of this study was the assessment of vital signals to confirm hemodynamic changes, which are related to the patient's pain. In various researches, the effect of changed position was investigated as a pain-reducing factor.[2,16,17,18,19,20] In these studies, it was shown that change in position caused a significant reduction in pain intensity at different times after the procedure. Also, no significant difference was seen in the blood pressure and heart rate among the participants. This finding was not consistent with our results. However, the study by Adaryani et al.[6] showed that blood pressure and heart rate in the control group were dramatically higher than the intervention group 6-8 h after catheterization. Increase in the pain level leads to increases in blood pressure, heart rate, and respiratory rate.[10,12,13,21] This finding confirms the effect of catecholamine releasing and its positive impact on the quality of pain such as inotropic, chronotropic, and dromotropic effects on the heart rate and respiratory rate. Systolic blood pressure subsequently increased. In the present study, the most changing was happened between systolic blood pressure and pain. In our study, nonadherence pain increased by increasing the angle of the bed; as flat angle increased to 45°, the heart rate and breathing rate increased but at position of 45°, the vital signals showed significant change (P < 0.05). They were decreased along with of pain intensity. Also, at 60° angle, it was found that the vital signals, which confirmed the increasing levels of pain severity increased significantly (P < 0.05). These findings did not match with the results of similar studies.[2,17] In the aforementioned study, no association found between a bed angle of 0° and 30° and then 45°, also, no relation was shown between decreasing of pain base on hemodynamic signals. After the procedure, the position was changed from supine to left or right lateral so as to reduce or alleviate pain and it was bed rest that likely caused the sandbag to move and then bleeding at the catheter (catheter entrance).[5,22] Providing an optimal position without creating risks for patients for the relieving of pain will increase patient satisfaction and reduce risks in the catheterization procedure. This study had some limitations such as a variable pain threshold among patients, probability variable race in the population study, and the fact that any stage of this study was not blinded. Other studies would be helpful to resolve the limitations of this study so as to obtain better guidelines for managing a patient's pain and discomfort after cardiac catheterization.
CONCLUSION
Change in the patient's bed angles after coronary angiography was associated with relief of pain. Our study showed that the optimal angle for patients was 45° bed angle and confidence about this result comes from observing the vital signals. So, it is advisable that postangiography nurses plan the application of this optimal position in order to relieve pain in patients after coronary angiography.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This work was supported by North Khorasan University of Medical Sciences of Iran under Grant 9360542.
Conflicts of interest
There are no conflicts of interest.
AUTHOR'S CONTRIBUTION
MAYH contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, analysis and interpretation of data for the work, and agreed for all aspects of the work. MY contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. SJ contributed in the Drafting of manuscript.
Acknowledgments
The authors would like to thank all the patients who participated in this study. We would also like to thank the directors of Imam Ali and Imam Reza hospitals, nurses of the cardiac catheterization, and postangiography wards of Imam Ali Hospital, and coronary care unit (CCU) wards of Imam Reza Hospital in Bojnurd, North Khorasan, Iran.
REFERENCES
- 1.Smeltzer SC, Bare B, Hinkle J L, Cheever KH. Brunner and Suddarth's Text book of Medical- Surgical Nursing. 12th ed. New York: Lippincott Williams & Wilkins; 2010. p. 145. [Google Scholar]
- 2.Farmanbar R, Mohammadiyan MA, Moghaddamniya MT, Kazemnejad E, Salari A. The effect of position change and bed-rest duration after coronary angiography on vascular complications. IJCCN. 2012;4:177–82. [Google Scholar]
- 3.Astin F, Closs SJ, McLenachan J, Hunter S, Priestley C. The information needs of patients treated with primary angioplasty for heart attack: An exploratory study. Patient Educ Couns. 2008;73:325–32. doi: 10.1016/j.pec.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 4.Antman EM, Selwyn AP, Braunwald E, Loscalzo J. Ischemic heart disease. In: Khodaee M, Zinsaz Boroujerdi H, editors. Harrison's Principles of Internal Medicine: Disorders of the Cardiovascular System. 17th ed. Tehran: Arjmand Publications; 2008. p. 390. [Google Scholar]
- 5.Kalyani MN, Jamshidi N. Risk factors of Iranian patients with three vessels disease candidate for coronary artery bypass graft surgery (CABG) Pak J Med Sci. 2010;26:837–41. [Google Scholar]
- 6.Rezaei-Adaryani M, Ahmadi F, Mohamadi E, Asghari-Jafarabadi M. The effect of three positioning methods on patient outcomes after cardiac catheterization. J Adv Nurs. 2008;65:417–24. doi: 10.1111/j.1365-2648.2008.04889.x. [DOI] [PubMed] [Google Scholar]
- 7.Lundén MH, Bengtson A, Lundgren SM. Hours during and after coronary intervention and angiography. Clin Nurs Res. 2006;15:274–89. doi: 10.1177/1054773806291855. [DOI] [PubMed] [Google Scholar]
- 8.Smeltzer SC. Chronic illness and disability. In: Smeltzer SC, Bare B, Hinkle JL, Cheever KH, editors. Brunner and Suddarth's Text book of Medical-Surgical Nursing. 12th ed. New York: Lippincott Williams & Wilkins; 2010. p. 217. [Google Scholar]
- 9.Akbari H, Younessi Heravi MA, Yaghubi M. Designing and constructing an optical monitoring system of blood supply to tissues under pressure. Journal of Medical Signals and Sensors. 2012;2:114–9. [PMC free article] [PubMed] [Google Scholar]
- 10.Ledowski T, Reimer M, Chavez V, Kapoor V, Wenk M. Effects of acute postoperative pain on catecholamine plasma levels, hemodynamic parameters, and cardiac autonomic control. Pain. 2012;153:759–64. doi: 10.1016/j.pain.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Koenig J, Jarczok MN, Ellis RJ, Warth M, Hillecke TK, Thayer JF. Lowered parasympathetic activity in apparently healthy subjects with self-reported symptoms of pain: Preliminary results from a pilot study. Pain Pract. 2015:314–8. doi: 10.1111/papr.12177. [DOI] [PubMed] [Google Scholar]
- 12.Sesay M, Robin G, Tauzin-Fin P, Sacko O, Gimbert E, Vignes JR, et al. Responses of heart rate variability to acute pain after minor spinal surgery: Optimal thresholds and correlation with the numeric rating scale. J Neurosurg Anesthesiol. 2015;27:148–54. doi: 10.1097/ANA.0000000000000102. [DOI] [PubMed] [Google Scholar]
- 13.Vyas HP, Shah S, Vyas N. Cardiovascular responses to lumbar core muscle stability exercise in young adults having postural low back pain. Natl J Physiol Pharm Pharmacol. 2015;5:98–100. [Google Scholar]
- 14.Hochstenbach LM, Courtens AM, Zwakhalen SM, van Kleef M, de Witte LP. Self-management support intervention to control cancer pain in the outpatient setting: A randomized controlled trial study protocol. BMC Cancer. 2015;15:416. doi: 10.1186/s12885-015-1428-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodriguez CS, McMillan S, Yarandi H. Pain measurement in older adults with head and neck cancer and communication impairments. Cancer Nurs. 2004;27:425–33. doi: 10.1097/00002820-200411000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Chair SY, Taylor-Piliae RE, Lam G, Chan S. Effect of positioning on back pain after coronary angiography. J Adv nurs. 2003;42:470–8. doi: 10.1046/j.1365-2648.2003.02646.x. [DOI] [PubMed] [Google Scholar]
- 17.Haghshenas H, Mansoori P, Najafi S, Nikoo MH, Zare N, Jonoobi M. The effect of changes in patients’ body position on the back pain intensity and hemodynamic status during and after radiofrequency catheter ablation of cardiac dysrhythmias. Iran J Nurs Midwifery Res. 2013;18:89–93. [PMC free article] [PubMed] [Google Scholar]
- 18.Chair SY, Thompson DR, Li SK. Effect of ambulation after cardiac catheterization on patient outcomes. J Clin Nurs. 2007;16:212–4. doi: 10.1111/j.1365-2702.2006.01599.x. [DOI] [PubMed] [Google Scholar]
- 19.Benson G. Changing patients’ position in bed after non-emergency coronary angiography reduced back pain. Evid Based Nurs. 2004;7:19. doi: 10.1136/ebn.7.1.19. [DOI] [PubMed] [Google Scholar]
- 20.Coyne C, Baier W, Perra B, Sherer BK. Controlled trial of backrest elevation after coronary angiography. Am J Crit Care. 1994;3:282–8. [PubMed] [Google Scholar]
- 21.Pickering TG. Effects of stress and behavioral interventions in hypertension. Pain and blood pressure. J Clin Hypertens (Greenwich) 2003;5:359–61. doi: 10.1111/j.1524-6175.2003.02830.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalyani MN, Sharif F, Ahmadi F, Iman MT. Iranian patient's expectations about coronary angiography: A qualitative study. Iran J Nurs Midwifery Res. 2013;18:180–5. [PMC free article] [PubMed] [Google Scholar]