Abstract
Background:
Evidence proposes that maternal calcium (Ca) supplement during pregnancy may be inversely associated with the off spring's blood pressure (BP) level. It is suggested that increased maternal Ca intake during pregnancy may result in lower BP in the off spring. The reduction in the incidence of hypertension in mothers is documented but the effects on the off spring are uncertain.
Materials and Methods:
We conducted a systematic review of the literature to summarize the evidence supporting an association between maternal dietary Ca intake during pregnancy and the BP in the off spring. In this systematic review, relevant papers were selected in three phases. After quality assessment, a reviewer extracted the data while the other one checked the extracted data. We summarized the information regarding the association of maternal Ca intake either by food or supplements with BP in the off spring.
Results:
Four randomized trials and three observational studies were included in this review. The results were more consistent among the studies including older children (1-9 years) where a higher maternal Ca intake was associated with a reduction in the off spring's systolic BP. One large randomized trial found a clinically and statistically significant reduction in the incidence of elevated BP in 7-year-old children [relative risk (RR) = 0.59, 95% confidence interval (CI) 0.39-0.90].
Conclusion:
Overall, our findings confirm the beneficial effects of maternal Ca intake during pregnancy for the off spring's BP level.
Keywords: Blood pressure (BP), calcium (Ca), maternal, offspring, pregnancy, prevention
INTRODUCTION
Hypertension is considered as the first leading risk factor for the global burden of disease.[1] Epidemiological observations have led to the hypothesis that the risk of developing some chronic noncommunicable diseases (NCDs) in adulthood is influenced not only by genetic and adult lifestyle factors but also by environmental factors acting in early life. In addition to this “developmental origins of health and disease” concept, several factors determine the blood pressure (BP) level in childhood, which is associated with the adult BP levelrough the “tracking” phenomenon. Therefore, prevention of NCDs, namely, cardiovascular diseases in adulthood should begin from childhood.[2,3,4,5] In addition, hypertension in childhood may induce target organ damages such as left ventricular hypertrophy, thickening of the carotid vessel wall, retinal vascular changes, subtle cognitive changes,[6] and even premature development of atherosclerosis.[7]
The prevalence of hypertension is increasing in the pediatric population in line with the childhood obesity epidemic and lifestyle widespread changes.[6] Alarming data exist on the considerable prevalence of overweight children and its metabolic consequences not only in the industrialized countries but also in developing countries.[8] The strong relationship of even the early stages of hypertension with obesity and environmental factors such as air pollution, noise pollution, and passive smoking suggest that its prevalence will be escalating in the near future.[9]
There is a growing body of evidence, which shows that impaired maternal nutrition may negatively influence vascular health in later life.[10] More specifically, the dietary calcium (Ca) intake of pregnant women may be associated with the BP of their infants,[11] and Ca intake is inversely correlated to systolic BP in young children.[12] Some recent experimental and observational studies in humans and animals have reported an association between maternal Ca intake during pregnancy and BP in the offspring,[13,14] but others did not confirm it.[15,16] We conducted a systematic review of studies reporting the association of maternal Ca intake either by food or supplements with BP in the offspring.
MATERIALS AND METHODS
Search strategy
We searched PubMed and SCOPUS as the main international electronic data sources. The medical subject headings (MeSh) including entry terms of PubMed and Emtree of Scopus were used for most comprehensive and efficient searches. We searched the databases using the following strategy: For Scopus [title-ABS-KEY (maternal or mother) and title-ABS-KEY (calcium) and title-ABS-KEY (blood pressure)], and for PubMed [“others” (MeSH)) or maternal) and “blood pressure”(MeSH) and “dietary supplements”(MeSH)) or calcium].
Study selection and eligibility criteria
Duplicates were removed; the relevant papers were selected in three phases. In the first and second phases, titles and abstracts of the papers were screened and irrelevant papers were excluded. In the last phase, the full text of recruited papers was explored intensely to select only relevant papers. For any additional pertinent studies, the reference list of all reviews and relevant papers was screened as well. In the next step, the eligibility of relevant papers was checked. Discrepancies were resolved by consultation and consensus.
Quality assessment
Identification of main findings of the studies was conducted on a case-by-case basis and included consideration of any statistical analyses that might have been conducted and consistency of the general pattern across exposure groups.
Data extraction and abstraction
The required information that was extracted from all eligible papers were as follows:
General characteristics of the study (first author's name, publication year, study year, study design)
Participants
Supplement,
Age of the offspring,
Loss to follow-up, and
Outcomes.
RESULTS
Based on our search strategy, we found 636 records. After removing duplicates, during the three refine steps on the papers’ titles, abstracts, and full texts and considering the inclusion criteria, only seven articles were selected [Figure 1]. The extracted results of seven papers are reported in Table 1.
Figure 1.
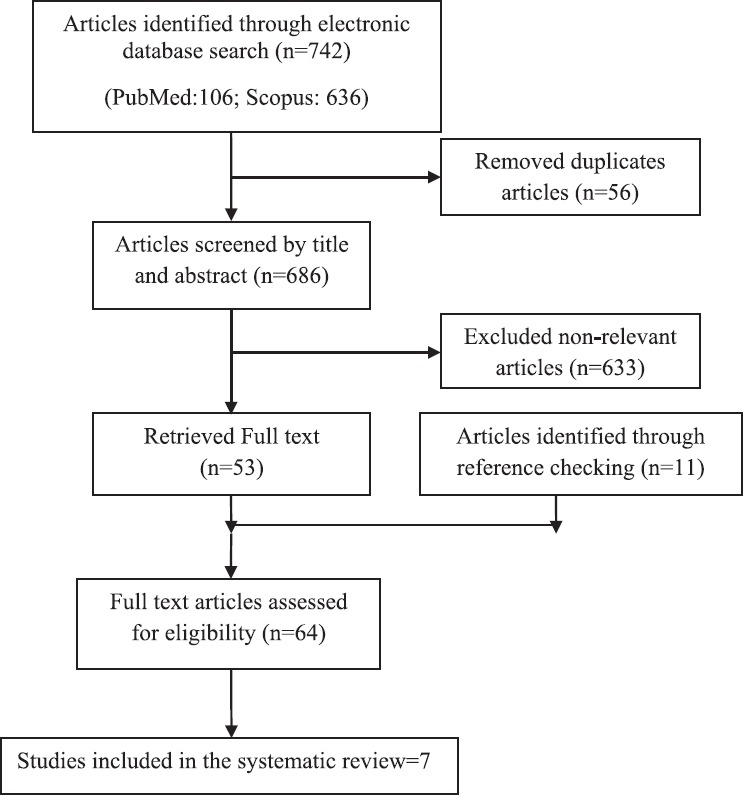
Flowchart of study selection
Table 1.
Summary of maternal calcium supplementation and offspring blood pressure
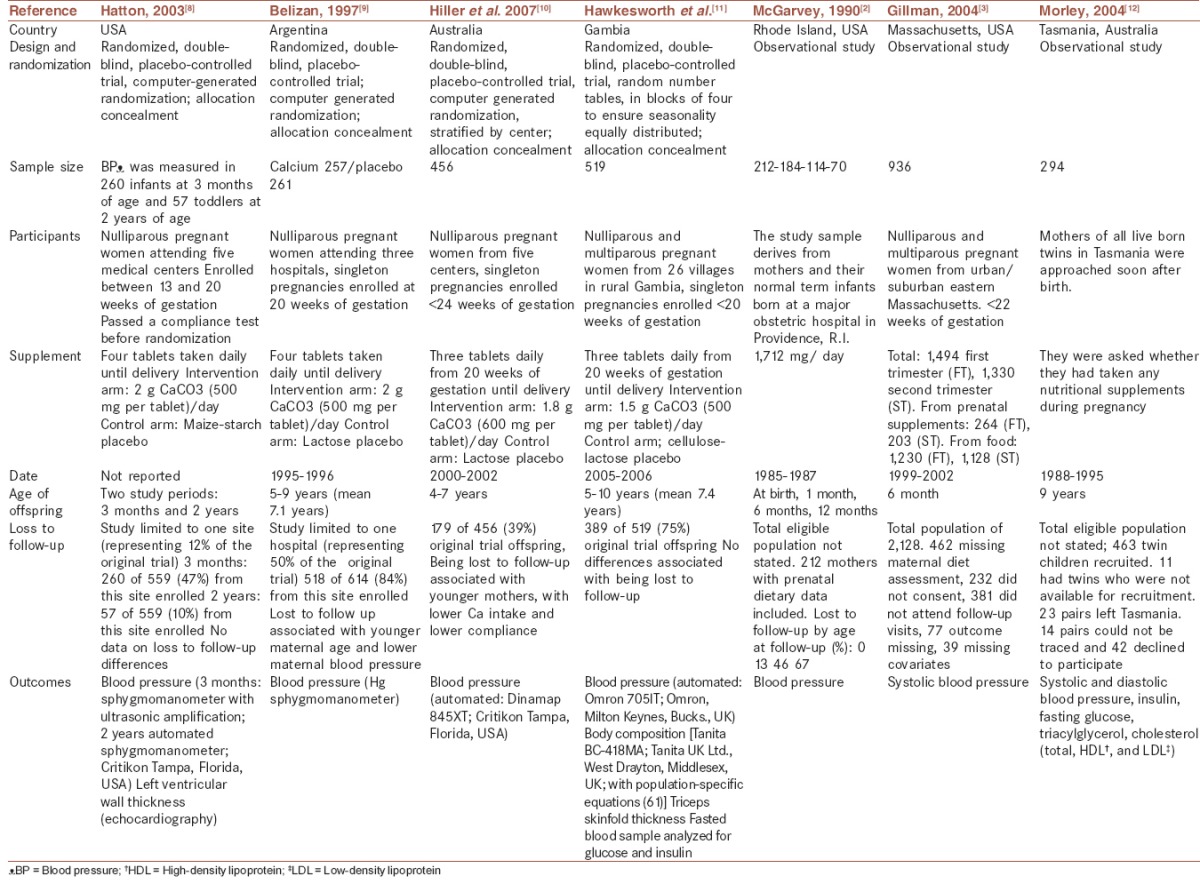
This systematic review of the literature identified four randomized trials and three observational studies. Three studies included infants less than 1 year of age[11,12,17] and seven included children between 1 year and 9 years of age.
A number of maternal Ca supplementation trials have been conducted on pregnant women in recent years, primarily to investigate the potential for reducing the risk of preeclampsia. All of the four trials have published follow-up data on the offspring, focusing on BP as an outcome.[17,18,19,20]
The study of Belizan et al. is a good quality randomized trial, which randomized 1,194 women during early pregnancy to either 2 g (four tablet of calcium carbonate of 500 mg) of oral Ca supplementation or placebo. Compliance with Ca supplementation was more than 80%. The follow-up only included the 614 participants from the private hospital (approximately 50% of the original sample). The proportion of children with high systolic BP was lower in the Ca group (11.4 %) than in the placebo group (19.3%) [relative risk (RR) 0.59; confidence interval (CI) 0.39-0.90]. The proportion of children with high diastolic BP was also lower in the Ca group [10.2% vs 12.7% (0.80; 0; 49-1.30)]. A large reduction in the incidence of hypertension in children at 7 years of age was found in this study.[18] There was a modest, statistically insignificant effect on systolic BP but a clinically and statistically significant effect on the incidence of high systolic BP at 7 years of age. This study also reported that the effect was stronger among overweight children; other studies did not observe this though the sample sizes were too small to exclude such a difference. For children under 12 months, the data were less consistent.
Hatton et al.[17] randomized 4,589 women during early pregnancy to receive either 2 g of oral Ca supplementation or placebo. Two follow-up studies were conducted at 3 months and 24 months postpartum. Patients from only one out of five medical centers were included in the follow-up (559 out of 4,589 subjects). Loss of follow-up was 53% at 3 months and 90% at 2 years. The authors acknowledged this to be a problem, adding that a large proportion of the cohort had not reached 2 years of age by the end of the study. This was the main methodological limitation of this study. The trial provided evidence that maternal Ca supplementation was associated with lower systolic BP in the offspring at 2 years. Systolic BP was 2.2 mmHg lower in the Ca-supplemented infants than in the placebo group (P > 0.05). At 2 years of age, systolic BP was 4.8 mm Hg lower in the Ca supplemented group (P < 0.05), whereas diastolic BP was lower by 3 mmHg.
McGarvey et al.[11] designed their study to explore the association between infant BP and maternal dietary intake of Ca, potassium, and magnesium. Data on maternal prenatal diet were obtained by conducting a quantitative food frequency questionnaire. The authors measured the offspring BP in hospital when the babies were 2-4 days old and at home at 1 month, 6 months, and 12 months. There were no significant associations between the mothers’ pregnancy intake of these cations and the newborns’ BP. However, at 1 month of age maternal prenatal Ca intake had a significant inverse association with systolic BP. At 6 months of age, maternal prenatal intakes of all three cations were significantly and inversely associated with diastolic BP. At 12 months of age, maternal prenatal potassium and intakes were significantly inversely related to diastolic BP.
Gillman et al.[12] used the data from a cohort study of pregnant women conducted in the United States. This study was designed to assess the effects of the mother's diet on the mother's and the offspring's health. It assessed maternal Ca intake during the first and second trimesters using a validated semi-quantitative food frequency questionnaire (FFQ), and measured offspring BP at birth and at 6 months. The authors reported figures for Ca from food sources and from prenatal supplements, and then performed two independent analyses accordingly. This seems to have been a non-prespecified analysis. After further adjustment for demographic, anthropometric, dietary, social, and economic variables, the decrease in 6-month systolic BP was −3.0 mmHg (95% CI, −4.9 to −1.1) for each 500 mg increment of maternal supplemental Ca intake during pregnancy.
Morley et al.[21] used the data from a population-based survey in Tasmania designed to investigate sudden infant death syndrome. Mothers of all live-born twins during the study period were approached after birth for data collection including nutritional supplement consumption during pregnancy. Data on Ca consumption from other sources (i.e., foods) were not available. Children were assessed at a mean age of 9 years and their BP was measured. The study found no significant association between maternal Ca supplementation and BP.
Hawkesworth et al.[20] conducted a study with 389 children from a rural area of Gambia whose mothers received Ca supplement (1,500 mg Ca/day from 20 weeks of gestation until delivery) or placebo in West Africa. The study was part of a European Union consortium investigation of the early life nutritional determinants of disease (Framework 6: “Early Nutrition Programming Project”). At the time of this follow-up study, the surviving offspring were aged between 5 years and 10 years (mean age: 7.4 years, standard deviation (SD) 6 1.2]. This study found no evidence that maternal calcium supplementation (1,500 mg Ca/day) of rural Gambian women during the second half of pregnancy was associated with the offspring's BP at 5-10 years of age.
Hiller et al.[19] followed up 414 participants with live-born infants who lived in South Australia. Mothers and their children attended the Women's and Children's Hospital for anthropomorphic examination. Information on lifestyle factors was collected by questionnaire. There was no indication that Ca supplementation during pregnancy had an impact on either systolic or diastolic BP at follow-up among women with preeclampsia, pregnancy-induced hypertension (PIH), or severe PIH. However, some evidence showed that their children tended to have lower BP at follow-up. This interaction between maternal Ca supplementation and the child's BP at follow-up was the strongest for women with more severe PIH and preeclampsia.
DISCUSSION
The evidence indicated by this body of research suggests a connection between dietary Ca intake during pregnancy and the offspring's BP. A good quality trial found a large reduction in the incidence of hypertension in children at 7 years of age.[18] For infants under 1 year of age, the evidence is discrepant and difficult to summarize. There are also large differences between studies in the infant's age at assessment. It is well-known that the determinant of BP varies with age, and it has been shown that the impact of factors affecting the fetal environment are seen particularly after adolescence.[22] This problem is magnified because of the difficulties in measuring BP accurately in early ages.[23]
The effect is observed mostly with systolic BP. It is unclear whether this is a true biological differential effect or a statistical artefact resulting from the greater variability within individuals of diastolic pressure compared with systolic pressure.[24]
Among the seven studies reported, we found four randomized trials. The validity of the evidence from observational studies for assessing the effect of interventions is controversial. Apart from the methodological problems of the original articles, other limitations of this analysis should be pointed out.
The heterogeneity between studies also created difficulties in explaining the results. The sources and dose of dietary CA vary widely among the observational studies, and so do the methods used to assess the amount consumed. There are also large differences between studies in the infant's age at assessment. It is well-known that the determinant of BP varies with age, and it has been shown that the impact of factors affecting the fetal environment are seen particularly after adolescence.[22] This problem is magnified because of the difficulties in measuring BP accurately at an early age.[25]
Six out of the seven studies included in the current review were conducted in developed countries, and on populations in which the maternal Ca intake was adequate or even higher than the recommended levels during pregnancy. This is clearly not the ideal target for a nutritional intervention. Given the evidence that the effect of Ca might be apparent only when there is a deficit, the external validity of these results might be compromised.[13] In Hawkesworth's[20] study from a region of habitually very low dietary calcium intake, there was no association between maternal calcium supplementation and offspring BP.
As a whole, all seven studies seem to have been well-conducted. The main limitation in all the observational studies was loss to follow-up. For two of these studies, a small sample size was also a problem. Higher maternal calcium intake during pregnancy was associated with lower offspring systolic BP in all studies but the effect was statistically significant in only three of them.[11,12,17]
The Argentinean[18] follow-up reported an interaction between the intervention and childhood BMI; for individuals with a BMI above the mean (15.7), maternal calcium supplementation was associated with lower systolic BP. In contrast to these findings, in the Gambian[20] and Gillman study.[12] These studies did not observe an increase in effect estimates as the body mass index increased. Gillman's study suggested that the BP-lowering effect of Ca might be limited to the three quartiles of the offspring's body mass index.[12]
Most of the protective effect of Ca supplementation during pregnancy is concentrated in children with high body mass index; if this finding is confirmed, it might have important preventive implications because this subgroup is at higher risk of elevated BP and adult hypertension.[26,27]
High maternal Ca intake with lower maternal BP could reduce fetal exposure to maternal hormones or substances related to elevated BP.
The observed effect could reflect a long-term programming of elevated BP in utero by Ca supplementation in the mother. This is consistent with the results obtained from observational studies that an early fetal exposure to calcium reduces BP during childhood.[11,12]
CONCLUSION
In general, our findings confirm the association of maternal Ca intake during pregnancy and offspring BP. However, more research is needed to confirm these findings, given the small sample sizes and the methodological problems in many of the studies conducted so far. More studies on populations with low Ca intake are also needed. If confirmed, these findings could have important public health implications. Ca supplementation during pregnancy is simple and inexpensive and may be a way to reduce the risk of elevated BP and its sequels in the next generation.
Financial support and sponsorship
The study was funded as a thesis of Isfahan University of Medical Sciences, Isfahan, Iran.
Conflicts of interest
There are no conflicts of interest.
AUTHOR'S CONTRIBUTION
All authors contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
Acknowledgments
This study was conducted as the project number 393599 of Isfahan University of Medical Sciences, Isfahan, Iran.
REFERENCES
- 1.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miersch A, Vogel M, Gausche R, Siekmeyer W, Pfäffle R, Dittrich K, et al. Blood pressure tracking in children and adolescents. Pediatr Nephrol. 2013;28:2351–9. doi: 10.1007/s00467-013-2596-3. [DOI] [PubMed] [Google Scholar]
- 3.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: A systematic review and meta-regression analysis. Circulation. 2008;117:3171–80. doi: 10.1161/CIRCULATIONAHA.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Juhola J, Magnussen CG, Viikari JS, Kähönen M, Hutri-Kähönen N, Jula A, et al. Tracking of serum lipid levels, blood pressure, and body mass index from childhood to adulthood: The cardiovascular risk in young finns study. J Pediatr. 2011;159:584–90. doi: 10.1016/j.jpeds.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 5.Virdis A, Ghiadoni L, Masi S, Versari D, Daghini E, Giannarelli C, et al. Obesity in the childhood: A link to adult hypertension. Curr Pharm Des. 2009;15:1063–71. doi: 10.2174/138161209787846900. [DOI] [PubMed] [Google Scholar]
- 6.Falkner B. Hypertension in children and adolescents: Epidemiology and natural history. Pediatr Nephrol. 2010;25:1219–24. doi: 10.1007/s00467-009-1200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luma GB, Spiotta RT. Hypertension in children and adolescents. Am Fam Physician. 2006;73:1558–68. [PubMed] [Google Scholar]
- 8.Kelishadi R. Childhood overweight, obesity, and the metabolic syndrome in developing countries. Epidemiol Rev. 2007;29:62–76. doi: 10.1093/epirev/mxm003. [DOI] [PubMed] [Google Scholar]
- 9.Kelishadi R, Poursafa P, Keramatian K. Overweight, air and noise pollution: Universal risk factors for pediatric pre-hypertension. J Res Med Sci. 2011;16:1234–50. [PMC free article] [PubMed] [Google Scholar]
- 10.Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 2008;359:61–73. doi: 10.1056/NEJMra0708473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McGarvey ST, Zinner SH, Willett WC, Rosner B. Maternal prenatal dietary potassium, calcium, magnesium, and infant blood pressure. Hypertension. 1991;17:218–24. doi: 10.1161/01.hyp.17.2.218. [DOI] [PubMed] [Google Scholar]
- 12.Gillman MW, Rifas-Shiman SL, Kleinman KP, Rich-Edwards JW, Lipshultz SE. Maternal calcium intake and offspring blood pressure. Circulation. 2004;110:1990–5. doi: 10.1161/01.CIR.0000143199.93495.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hofmeyr GJ, Lawrie TA, Tallah A, Duley L. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2010:CD001059. doi: 10.1002/14651858.CD001059.pub3. [DOI] [PubMed] [Google Scholar]
- 14.Dwyer JH, Dwyer KM, Scribner RA, Sun P, Li L, Nicholson LM, et al. Dietary calcium, calcium supplementation, and blood pressure in African American adolescents. Am J Clin Nutr. 1998;68:648–55. doi: 10.1093/ajcn/68.3.648. [DOI] [PubMed] [Google Scholar]
- 15.van Mierlo LA, Arends LR, Streppel MT, Zeegers MP, Kok FJ, Grobbee DE, et al. Blood pressure response to calcium supplementation: A meta-analysis of randomized controlled trials. J Hum Hypertens. 2006;20:571–80. doi: 10.1038/sj.jhh.1002038. [DOI] [PubMed] [Google Scholar]
- 16.Stary HC. Lipid and macrophage accumulations in arteries of children and the development of atherosclerosis. Am J Clin Nutr. 2000;72(Suppl):1297–306S. doi: 10.1093/ajcn/72.5.1297s. [DOI] [PubMed] [Google Scholar]
- 17.Hatton DC, Harrison-Hohner J, Coste S, Reller M, McCarron D. Gestational calcium supplementation and blood pressure in the offspring. Am J Hypertens. 2003;16:801–5. doi: 10.1016/s0895-7061(03)01027-6. [DOI] [PubMed] [Google Scholar]
- 18.Belizán JM, Villar J, Bergel E, del Pino A, Di Fulvio S, Galliano SV, et al. Long-term effect of calcium supplementation during pregnancy on the blood pressure of offspring: Follow up of a randomised controlled trial. BMJ. 1997;315:281–5. doi: 10.1136/bmj.315.7103.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hiller JE, Crowther CA, Moore VA, Willson K, Robinson JS. Calcium supplementation in pregnancy and its impact on blood pressure in children and women: Follow up of a randomised controlled trial. Aust N Z J Obstet Gynaecol. 2007;47:115–21. doi: 10.1111/j.1479-828X.2007.00696.x. [DOI] [PubMed] [Google Scholar]
- 20.Hawkesworth S, Sawo Y, Fulford AJ, Goldberg GR, Jarjou LM, Prentice A, et al. Effect of maternal calcium supplementation on offspring blood pressure in 5- to 10-y-old rural Gambian children. Am J Clin Nutr. 2010;92:741–7. doi: 10.3945/ajcn.2010.29475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morley R, Carlin JB, Dwyer T. Maternal calcium supplementation and cardiovascular risk factors in twin offspring. Int J Epidemiol. 2004;33:1304–9. doi: 10.1093/ije/dyh284. [DOI] [PubMed] [Google Scholar]
- 22.Huxley RR, Shiell AW, Law CM. The role of size at birth and postnatal catch-up growth in determining systolic blood pressure: A systematic review of the literature. J Hypertens. 2000;18:815–31. doi: 10.1097/00004872-200018070-00002. [DOI] [PubMed] [Google Scholar]
- 23.O’Brien E, Beevers G, Lip GY. ABC of hypertension. Blood pressure measurement. Part III-automated sphygmomanometry: Ambulatory blood pressure measurement. BMJ. 2001;322:1110–4. doi: 10.1136/bmj.322.7294.1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosner B, Cook NR, Evans DA, Keough ME, Taylor JO, Polk BF, et al. Reproducibility and predictive values of routine blood pressure measurements in children. Comparison with adult values and implications for screening children for elevated blood pressure. Am J Epidemiol. 1987;126:1115–25. doi: 10.1093/oxfordjournals.aje.a114750. [DOI] [PubMed] [Google Scholar]
- 25.O’Brien E. Ambulatory blood pressure measurement is indispensable to good clinical practice. J Hypertens Suppl. 2003;21:S11–8. doi: 10.1097/00004872-200305002-00003. [DOI] [PubMed] [Google Scholar]
- 26.de Swiet M, Fayers P, Shinebourne EA. Blood pressure in first 10 years of life: The Brompton study. BMJ. 1992;304:23–6. doi: 10.1136/bmj.304.6818.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Higgins M, Keller J, Moore F, Ostrander L, Metzner H, Stock L. Studies of blood pressure in Tecumseh, Michigan I. Blood pressure in young people and its relationship to personal and familial characteristics and complications of pregnancy in mothers. Am J Epidemiol. 1980;111:142–55. doi: 10.1093/oxfordjournals.aje.a112882. [DOI] [PubMed] [Google Scholar]


