Abstract
Background:
Infantile hemangioma (IH) is the most common tumor during infancy that usually appears as macular and gradually becomes a plaque or tumor. Approximately, 20% of all IH cases results in adverse effects and the Pulsed dye laser (PDL) 585 nm is a vascular laser leading to selective the micro vascular damage. Results of studies on non-selective B-blockers (e.g., timolol) indicate their effectiveness in preventing hemangioma growth. The aim of this study is a comparison of PDL plus timolol and PDL in the treatment of IH.
Materials and Methods:
This double-blind study was carried out on 30 infants (1-12 months old) and the patients were divided into two groups. Group A was treated with the four sessions PDL and the timolol gel 0.05% and Group B with PDL.
Results:
There were no differences in the mean age of patients for the diagnosis of hemangioma (Group A: 32.69 ± 24.64 days, Group B: 25.69 ± 21.16 days, P = 0.39) and the mean age at the start of the treatment (Group A: 148.125 ± 85.88 days, Group B: 146.25 ± 60.87 days, P = 0.94). There were a statistical difference in the mean of lesion size reduction (Group A: 17.62 ± 6.97 cm and Group B: 12 ± 5.71 cm, P = 0.018), mean percentage change in size mean (Group A: 71079 ± 23.41% and Group B: 54.59 ± 25.46%, P = 0.050) visual analog scale (Group A: 7.19 ± 1.51, Group B: 5.62 ± 1.78, P = 0.012) after treatment. There was no correlation between the time of beginning the treatment and the results (P = 0.857).
Conclusions:
Application of timolol with PDL is accompanied by the highest efficacy, cost benefits and the short time of treatment.
Keywords: Infantile hemangioma, Pulsed dye laser, timolol
INTRODUCTION
Infantile hemangioma (IH) is the most common tumor during infancy, affecting 10% of Caucasian children[1] and it is more frequent in females with a male to female ratio of 1:2.[2,3] Hemangioma is a benign proliferation of endothelial cells that usually appears as maculae and gradually enlarges and becomes a plaque or tumor. It may occur anywhere on the skin and mucosal surface, with approximately 50% of its occurrences being located on the head and neck. It typically arises sporadically, although, a 10% incidence of familial cases has been reported.[4] It is characterized by significant growth during the first several months of life, most growth occurring during the first 3 months.[5] It then progresses at a slower rate, and the plateau and involution slowly continues and by 5 years of age 50% and by 9 years of age 90% of the IH will have reached maximal regression. Maximal regression of IH does not define a return to normal skin.[6]
IH is present at birth in one-third of the cases. In the remaining cases, it appears shortly thereafter.[7] Approximately, 20% of IH results in pain bleeding, ulceration, infection, or functional impairment with the vision feeding or breathing.[8] There are many treatments for IHs. Most physicians believe that because of spontaneous resolution, treatment is not necessary unless the problem becomes complicated or impairs the function of vital organs.[9] Most therapeutic recommendations are intralesional corticosteroids, topical corticosteroids, topical imiquimod, systemic corticosteroids, systemic B-blockers.[9] Treatment of early hemangiomas with laser in the proliferative phase may induce involution and improve the rate of complete clinical clearance. This treatment is generally well-tolerated.[10] Pulsed dye laser (PDL) with the varying pulse duration and fluence has been used in the treatment of IH.[11] PDL with 585 wavelength is a vascular laser targeted at the oxyhemoglobin present in the red blood cells, which circulates in the blood vessels and after absorption of energy by these targets, thermal energy diffuses radially within the blood vessels leading to selective the microvascular damage, through the photocoagulation and the mechanical injury.[12] The new therapy that was first used for palpebral hemangioma is topical non-selective B-blocker, timolol, in treatment of superficial hemangioma.[13] Preliminary results of studies indicate the effectiveness in preventing hemangioma growth and decreasing tumor volume with more regularity than corticosteroid.[13] Therefore, we decided to test the two new treatments of IH and determine whether a combination of these two methods would have more effectiveness and lower adverse effects.
MATERIALS AND METHODS
This double-blind randomized clinical trial was carried out on 30 infants with 32 hemangiomas (two patients had two lesions) in Alzahra hospital (Referral Center for Treatment of Skin Diseases) during January 2011 to January 2012. Before starting, the study was approved by The Ethics Committee of Isfahan University of Medical Sciences (Iran). Inclusion criteria were otherwise healthy infants between 1 month and 12 months old with superficial hemangioma ≤3 cm, and infants with a history of sensitivity to B-blockers or asthma, renal disease, heart disease, hypoglycemia, using of drugs that interact with B-blockers. The parents of all patients gave written informed consent for the study. On the first visit, all patients were examined by a dermatologist; then, questionnaires that included information about age, sex, past medical history, drug history, time of hemangioma appearance, size and location and history of pregnancy, and the age of the mother during pregnancy were completed. Before treatment and after every treatment session each patient underwent photography in the same physical condition with a digital camera (Canon Power Shot G12, Cannon Components Inc., Japan) carried out by one person. Then, patients were divided into two groups in double blind manner. Each group had 16 hemangiomas. Group A was treated with 585 PDL and timolol and Group B with 585 PDL plus lubricant gel as a placebo. Timolol gel and lubricant gel were used every 12 h. Timotol gel was prepared from its powder solved in a little ethanol and mixed with the lubricant gel up to 0.5% concentration. Laser therapy was carried out with 585 nm PDL manufactured by the Chromogenex (UK) company, without cooling, with spot size 5 mm, fluence 9 J/cm2, Pulse duration 450 ms and spot overlap 20%. Eutectic mixture of lidocaine and prilocaine was used on lesions 30 min prior to each laser therapy session. After laser therapy, ice pack and zinc oxide cream were used and use of zinc oxides continued until the petechia due to the laser had disappeared. Parents were asked to prevent the trauma and the sun exposure with regard to the treated areas and to contact the researcher if any side-effects (such as bleeding, ulceration) appeared. Laser therapy was carried out four sessions a month. The patients were followed-up for 6 months after the treatment. Since there is no standard objective method for assessing hemangioma improvement, for better comparison of the data and increase in accuracy, two forms of assessment were used: (1) clinical score for the overall change and (2) visual analog scale (VAS) similar to that employed in other objective studies.[14] The visual analog score consisted of grading each lesion based on three categories: Overall appearance, color and size. Each category was scored from − 3 to 3 (−3 = a lot worse: −2 = somewhat worse − 1= a little worse 0 = no change 1 = a little better 2 = somewhat better: 3 = a lot better).[14] The overall score was summed. The final range was from − 9 (worsening lesion) to +9 (considerable improvement). The clinical score was defined as the percentage of change in size and was calculated with the formula:[15]
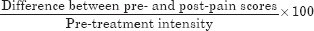
The statistical analysis of the results was performed using the paired t-test in the SPSS 20 for windows (SPSS Inc., Chicago, IL). In this study, the significance level was set at P values of equal and <0.05.
RESULTS
A total of 30 children with 32 hemangiamas (two patients had two hemangiomas), 24 girls and 8 boys were studied. The mean age of patients during diagnosis of hemongioma in the Group A was 32.69 ± 24.64 days and in Group B 25.69 ± 21.16 days (P = 0.39). The mean age at the start of treatment in the Group A was 148.125 ± 85.88 days and in Group B 146.25 ± 60.87 days (P = 0.94). 12.5% of the patients had a family history of IH. 56% of the children were born in the second and third delivery. Two children were born with birth weight less than 1500 g (6.25%) and six had a birth weight less than 2500 (18%); another 25% of the children had relatively low birth weight. In seven cases, the mother was older than 34 years at the time of pregnancy (21.8%). 13 lesions (40.65%) had appeared during the 1st weeks of life. The mean lesion size in the Group A was 25.31 ± 6.77 cm and in Group B 25 ± 6.55 cm (P = 0.895). The post-treatment mean lesion size was 7.68 ± 7.37 in Group A and 13 ± 7.02 in Group B (P = 0.046) [Table 1]. The mean percentage of change in lesion size was 71.79 ± 23.40% in Group A and 54.59 ± 25.46% in Group B (P = 0.056) and 7.01 ± 1.51 and 5.62 ± 1.78 for mean VAS change in each group respectively (P = 0.012). The mean of reduction in lesion size was 17.62 ± 6.97 cm and 12 ± 5.71 cm in the case [Figure 1] and control group [Figure 2] respectively (P = 0.018). Comparing the percentage of improvement in the lesion size and mean VAS change revealed a statistical difference between the two groups [Table 2]. Complete clearance was achieved in one patient in each group. This lesion was 16 mm and 7 mm in Group A and B, respectively. The treatments of both lesions were begun when the children were 60 day old; the lesions were on the lumbar and face in Group A and B, respectively. Because, the highest rate of progress in hemangioma (proliferation phase) is in the first 3 months of life,[5] the mean change in size in each group was divided into ≤3 months and > 3 months and then evaluated [Table 3]. There was no correlation between treatment initiation time and better results. None of the patients in Group B reported any systemic adverse effects such as hypotension, bradycardia, sleep disturbance or anxiety and hypoglycemia. In the Group A, two patients (12.5%) with hemangioma on the face and in Group B, five patients (31.25%) with hemangioma on the face and finger (four and one patients respectively) developed hypopigmentations (P = 0.27). In the Group A, two patients (12.5%) with hemangioma on the face and upper extremity and in Group B none of the patients developed change in texture (P = 0.16). No ulceration or hyperpigmentation occurred during treatment in either group.
Table 1.
Demographic data and IH anatomical location

Figure 1a.

Two months old boy with a perioral infantile hemangioma treated with Pulsed dye laser and timolol gel at the start of treatment (c)
Figure 2a.

Nine months old girl with a perioral infantile hemangioma treated with Pulsed dye laser at the start of treatment (a)
Table 2.
Mean percentage change and mean VAS change in the case and control group
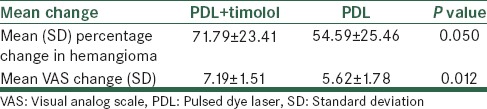
Table 3.
Correlation between the time of beginning treatment and results
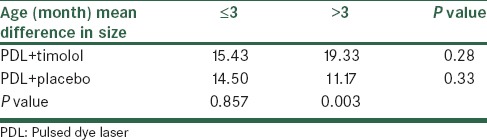
Figure 1b.

Two months old boy with a perioral infantile hemangioma treated with Pulsed dye laser and timolol gel 4months later (d)
Figure 2b.

Nine months old girl with a perioral infantile hemangioma treated with Pulsed dye laser 4 months later (b)
DISCUSSION
IH is a vascular tumor that is the most common soft-tissue tumor in infants less than 1 year old.[1] Infants with hemangiomas were more likely to be Caucasian, have low birth weight, pre-mature, the product of multiple gestation pregnancies and born to older mothers.[2] There is no consensus about its pathogenesis. Several mechanisms have focused on different theories such as endothelial progenitor cell origin, somatic mutations in genes related to the vascular endothelial growth factor signaling.[16,17,18] In most studies, the hemangiomas are more common in females and the infant is a product of the multiple gestations such as those in our study. In the study of Haggstrom et al., male to female ratio was 1-3. Most hemangiomas appear during the first few weeks of life as in our study.[2] In Waner et al.’ study 15-60% hemangiomas were congenital, the percentage of which was 40.65% in this study.[19] There has been the idea that “active non-intervention” is a better way to approach babies with hemangioma unless it becomes complicated.[20] However, parent anxiety and the effect of the impairment on the growing baby such as psychosocial effects and its physical scar has forced researchers to find a treatment.[20] Many treatments are available such as topical corticosteroids, imiquimod, intralesional corticosteroids, oral corticosteroids, and beta blockers.[9] Two new treatments that are supposed to be effective are topical timolol a non-selective beta blocker and PDL585 nm.[21,22] In the multicenter study done by Chakkittakandiyil et al. from 2011 to 2012 in the US it became clear that topical timolol was safe and effective for small and superficial hemangiomas.[23] This study showed the safety of using the timolol gel, which was without any systemic adverse effects.[23] In the case series that was carried out by Moehrle an et al. one the treatment of 11 IH s with topical tiomolol 0.5% gel was associated with the growth arrest, reduction in redness, thickness; complete resolution was achieved in seven patients, and its regression occurred earlier than spontaneous regression.[22] The first published randomized controlled trial that compared no intervention or early treatment of IH with 585 nm PDL without epidermal cooling for superficial hemangioma, showed that early intervention was significantly more likely to result in complete clearance of hemangioma in 1 year olds (30% of those treated with early PDL versus. Only 5% of the control group P > 0.001).[24] However, in this study the adverse effects were high (45% case group, 15% control group). In our study, the adverse effect rate was 25% and this may be due to concomitant use of timolol gel and laser or using the different pulse durations. In Rizzo et al.’ study, 595-nm PDL with dynamic cooling for 105 hemangiomas was used; according to this study, near-complete or complete clearance in color was achieved for 81% and thickness for 64% of cases and there was no scarring or atrophy. Ulceration occurred in one case and hyper and hypo pigmentation occurred in 4% and14% of the hemangiomas respectively.[8]
Some authors believe that PDL is a good method in ages below 6 months when its cosmetic effects are relevant and after this age laser therapy should be used for residual lesions.[1] Based on our study there is no differ between the two groups when treatment begins before 3 months of age, but PDL plus timolol is more effective than PDL alone when the beginning of treatment is after the age of 3 months. Furthermore, the beginning time of treatment (before 3 months or after) had no effects on treatment results. However, Rizzo et al. reported a retrospective study with excellent clearance rate and only few adverse effect in the early treatment of superficial hemangiomas using 595 nm PDL and Kessels et al. reported in their prospective study that treatment of IH with PDL595 nm had a significant effect on the proliferative phase but also had effects on reducing proliferation sometimes beyond the age of 6 months.[1] In our prospective cohort study, the results showed that adverse effects were the same in both groups and most of them were change in texture or hypo pigmentation. Both methods discussed in our article were effective in size reduction and the improvement of the visual score of hemangiomas; however, the effectiveness of PDL plus timolol in mean size change or mean VAS improvement was statistically more effective than PDL alone. However, significant clearance was not achieved possibly because of the short duration of treatment (four sessions). In the study of Christopher et al., on average five sessions of treatment were performed and complete clearance was achieved in 36.4%, and excellent improvement was achieved in 77.3% of the cases.[25] Our study showed that the location of lesions did not have any effect on the result of treatment. According to the results, it seems that PDL plus timolol is more effective than PDL alone and if the physician decides to use PDL for the treatment of hemangima, it is better to combine it with topical timolol especially when the infant's age is more than 3 months.
The limitations of our study were short duration of treatment and the lack of objective methods for result assessment.
ACKNOWLEDGMENTS
We thank all the patients who participated in this study and Dr. Fariba Iraji for her presentation of patients and kind cooperation and Dr. Hosseini for his cooperation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kessels JP, Hamers ET, Ostertag JU. Superficial Hemangioma: Pulsed Dye Laser Versus Wait- and-See. Dermatol Surg. 2012;26:12081. doi: 10.1111/dsu.12081. [DOI] [PubMed] [Google Scholar]
- 2.Haggstrom AN, Drolet BA, Baselga E, Chamlin SL, Garzon MC, et al. Hemangioma Investigator Group. Prospective study of infantile hemangiomas: Demographic, prenatal, and perinatal characteristics. J Pediatr. 2007;150:291–4. doi: 10.1016/j.jpeds.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Hoornweg MJ, Smeulders MJ, Ubbink DT, van der Horst CM. The prevalence and risk factors of infantile haemangiomas: A case-control study in the Dutch population. Paediatr Perinat Epidemiol. 2012;26:156–62. doi: 10.1111/j.1365-3016.2011.01214.x. [DOI] [PubMed] [Google Scholar]
- 4.Margileth AM, Museles M. Cutaneous hemangiomas in children. Diagnosis and conservative management. JAMA. 1965;194:523–6. [PubMed] [Google Scholar]
- 5.Chang LC, Haggstrom AN, Drolet BA, Baselga E, Chamlin SL, Garzon MC, et al. Growth characteristics of infantile hemangiomas: Implications for management. Pediatrics. 2008;122:360–7. doi: 10.1542/peds.2007-2767. [DOI] [PubMed] [Google Scholar]
- 6.Miller T, Frieden IJ. Hemangiomas: New insights and classification. Pediatr Ann. 2005;34:179–87. doi: 10.3928/0090-4481-20050301-07. [DOI] [PubMed] [Google Scholar]
- 7.Barry RB, Hughes BR, Cook LJ. Involution of infantile haemangiomas after imiquimod 5% cream. Clin Exp Dermatol. 2008;33:446–9. doi: 10.1111/j.1365-2230.2007.02676.x. [DOI] [PubMed] [Google Scholar]
- 8.Rizzo C, Brightman L, Chapas AM, Hale EK, Cantatore-Francis JL, Bernstein LJ, et al. Outcomes of childhood hemangiomas treated with the pulsed-dye laser with dynamic cooling: A retrospective chart analysis. Dermatol Surg. 2009;35:1947–54. doi: 10.1111/j.1524-4725.2009.01356.x. [DOI] [PubMed] [Google Scholar]
- 9.Awadein A, Fakhry MA. Evaluation of intralesional propranolol for periocular capillary hemangioma. Clin Ophthalmol. 2011;5:1135–40. doi: 10.2147/OPTH.S22909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ashinoff R, Geronemus RG. Failure of the flashlamp-pumped pulsed dye laser to prevent progression to deep hemangioma. Pediatr Dermatol. 1993;10:77–80. doi: 10.1111/j.1525-1470.1993.tb00021.x. [DOI] [PubMed] [Google Scholar]
- 11.Tay YK, Tan SK. Treatment of infantile hemangiomas with the 595-nm pulsed dye laser using different pulse widths in an Asian population. Lasers Surg Med. 2012;44:93–6. doi: 10.1002/lsm.21159. [DOI] [PubMed] [Google Scholar]
- 12.Srinivas CR, Kumaresan M. Lasers for vascular lesions: Standard guidelines of care. Indian J Dermatol Venereol Leprol. 2011;77:349–68. doi: 10.4103/0378-6323.79728. [DOI] [PubMed] [Google Scholar]
- 13.Weissenstein A, Straeter A, Villalon G, Bittmann S. Topical timolol for small infantile hemangioma: A new therapy option. Turk J Pediatr. 2012;54:156–8. [PubMed] [Google Scholar]
- 14.Ho NT, Lansang P, Pope E. Topical imiquimod in the treatment of infantile hemangiomas: A retrospective study. J Am Acad Dermatol. 2007;56:63–8. doi: 10.1016/j.jaad.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 15.Williamson A, Hoggart B. Pain: A review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798–804. doi: 10.1111/j.1365-2702.2005.01121.x. [DOI] [PubMed] [Google Scholar]
- 16.Yu Y, Flint AF, Mulliken JB, Wu JK, Bischoff J. Endothelial progenitor cells in infantile hemangioma. Blood. 2004;103:1373–5. doi: 10.1182/blood-2003-08-2859. [DOI] [PubMed] [Google Scholar]
- 17.Frieden IJ, Haggstrom AN, Drolet BA, Mancini AJ, Friedlander SF, Boon L, et al. Infantile hemangiomas: Current knowledge, future directions. Proceedings of a research workshop on infantile hemangiomas, April 7-9, 2005, Bethesda, Maryland, USA. Pediatr Dermatol. 2005;22:383–406. doi: 10.1111/j.1525-1470.2005.00102.x. [DOI] [PubMed] [Google Scholar]
- 18.Khan ZA, Boscolo E, Picard A, Psutka S, Melero-Martin JM, Bartch TC, et al. Multipotential stem cells recapitulate human infantile hemangioma in immunodeficient mice. J Clin Invest. 2008;118:2592–9. doi: 10.1172/JCI33493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.North PE, Waner M, James CA, Mizeracki A, Frieden IJ, Mihm MC. Congenital clinicopathologic infantile hemangioma. Arch Dermatol. 2002;137:1607–20. doi: 10.1001/archderm.137.12.1607. [DOI] [PubMed] [Google Scholar]
- 20.Frieden IJ, Eichenfield LF, Esterly NB, Geronemus R, Mallory SB. Guidelines of care for hemangiomas of infancy. American Academy of Dermatology Guidelines/Outcomes Committee. J Am Acad Dermatol. 1997;37:631–7. doi: 10.1016/s0190-9622(97)70183-x. [DOI] [PubMed] [Google Scholar]
- 21.Mariwalla K, Dover JS. The use of lasers in the pediatric population. Skin Therapy Lett. 2005;10:7–9. [PubMed] [Google Scholar]
- 22.Moehrle M, Léauté-Labrèze C, Schmidt V, Röcken M, Poets CF, Goelz R. Topical timolol for small hemangiomas of infancy. Pediatr Dermatol. 2013;30:245–9. doi: 10.1111/j.1525-1470.2012.01723.x. [DOI] [PubMed] [Google Scholar]
- 23.Chakkittakandiyil A, Phillips R, Frieden IJ, Siegfried E, Lara-Corrales I, Lam J, et al. Timolol maleate 0.5% or 0.1% gel-forming solution for infantile hemangiomas: A retrospective, multicenter, cohort study. Pediatr Dermatol. 2012;29:28–31. doi: 10.1111/j.1525-1470.2011.01664.x. [DOI] [PubMed] [Google Scholar]
- 24.Batta K, Goodyear HM, Moss C, Williams HC, Hiller L, Waters R. Randomised controlled study of early pulsed dye laser treatment of uncomplicated childhood haemangiomas: Results of a 1-year analysis. Lancet. 2002;360:521–7. doi: 10.1016/S0140-6736(02)09741-6. [DOI] [PubMed] [Google Scholar]
- 25.Hunzeker M C, Geronemuf G R. Treatment of infantile hemangioma of the eyelid using the 595 nm pulsed dye laser. J Dermato surg. 2010;36:590–7. doi: 10.1111/j.1524-4725.2010.01511.x. [DOI] [PubMed] [Google Scholar]


