Abstract
Background:
In India, only one woman is diagnosed with tuberculosis (TB) for every 2.4 men. Previous studies have indicated gender disparities in care-seeking behavior and TB diagnosis; however, little is known about the specific barriers women face.
Objectives:
This study aimed to characterize socio-cultural and knowledge-based barriers that affected TB diagnosis for women in Bhopal, India.
Materials and Methods:
In-depth interviews were conducted with 13 affected women and 6 health-care workers. The Bhopal Diagnostic Microscopy Laboratory Register (n = 121) and the Bhopal district report (n = 261) were examined for diagnostic and care-seeking trends.
Results:
Women, especially younger women, faced socio-cultural barriers and stigma, causing many to hide their symptoms. Older women had little awareness about TB. Women often sought treatment from private practitioners, resulting in delayed diagnosis.
Conclusions:
Understanding these diagnostic and help-seeking behaviors barriers for women is critical for development of a gender-sensitive TB control program.
Keywords: Age, Bhopal, gender, stigma, tuberculosis
Introduction
In 2012, there were 2.9 million women diagnosed with tuberculosis (TB) and 410,000 women killed by TB worldwide. This makes TB the third largest killer of women of reproductive age.(1) In India, one woman is diagnosed for every 2.4 men, one of the lowest female-to-male ratios worldwide.(1) This may reflect differences in biology, socio-economic roles, health-care access, educational levels, and decision-making power between men and women.(2) Studies have identified gender inequalities in care-seeking behavior, TB diagnosis, and TB treatment.(3,4,5,6) But little is known about barriers women face in India, a country accounting for 30% of the global TB burden.(1)
We investigated how socio-economic factors, access to care, and knowledge affect diagnosis of TB in women in Bhopal.
Materials and Methods
This study utilized a two-step, quantitative then qualitative, approach. First, quantitative analysis of Bhopal patient data was used to assess the male-to-female disparity of diagnosis. To do this, we reviewed the Bhopal Diagnostic Microscopy Laboratory Register (n = 121; February to November 2013) and the Bhopal district report (n = 261; July to September 2013) to determine the number of individuals evaluated by smear microscopy and new sputum-positive TB cases. We stratified the data by gender and age.
Second, qualitative semi-structured interviews were conducted to understand the reasons behind the diagnostic disparity. We interviewed the district TB officer, a physician, two TB nurses, two non-governmental organization staff members, and 13 women with TB at four Bhopal facilities. Women represented different ages (18 to 65 years), faiths, marital statuses, occupations, and socio-economic statuses. Interviews of participants were recorded after informed consent was received. Responses were coded manually for patients’ feelings of stigmatization, TB knowledge and information sources, traditional medicine usage, family support patterns, care seeking habits, and other barriers.
The Ethics Review Board of the School of International Training, Delhi, approved the study.
Results
The male-to-female ratio was 2.4:1 for those evaluated by sputum smear microscopy [Figure 1] and 1.7:1 for those diagnosed with TB. This indicates a higher smear positivity rate among women assessed for TB although males were proportionately more likely to be evaluated for TB. Male to female diagnosis ratio was lowest (0.6:1) among children (age 0-14 years) while highest (6.3:1) for age group 55-64 [Figure 2].
Figure 1.
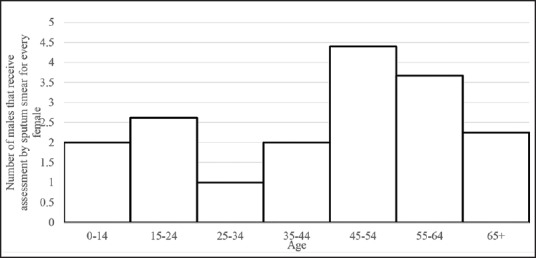
Male to female ratio of sputum smear assessment for different age ranges [original]
Figure 2.
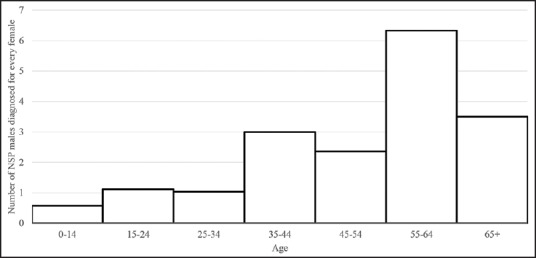
Male to female new spear positive pulmonary TB diagnosis ratio for different age ranges [original]
Of the women interviewed, perceived community stigma was the most reported barrier. Four women reported experiencing shame, discrimination, or stigmatization. In a society where arranged marriage is widely practiced, TB leads to rejection.(7) One young woman stated ‘I am not married’ as her biggest challenge post-TB. Many (6/13) women revealed their TB diagnosis to only family members. Especially, young women (<30 years of age) hid their diagnosis. One woman (age 20) hid her diagnosis from everyone, resulting in transmission to her grandmother.
“I walked two kilometers for my treatment. Some days I could not come, because my family could not know. . . I stayed away from them [family and friends]. I was scared they would see me in a bad manner.” (TB Patient.)
Health care workers confirmed that stigma is stronger for women and affects TB diagnoses and treatment:
“TB is harder for women. It's because India is male dominated. Society doesn’t accept women with TB. They are ashamed and stigmatized.” (TB Nurse.)
“It [stigma] makes women hesitate to come to the TB Center [for diagnosis], the DOTS [Directly Observed Treatment Short-Course] center [for treatment], and to disclose their complaints of cough and weight loss.” (District TB Officer.)
Because of stigma, TB is rarely discussed in community or family settings.
“Awareness is a problem because they have to come to us at 2 weeks [of being symptomatic], but many times they come after 1, 2 or 4 months, 1, 2, or 3 years. They go to quacks, talk to unqualified practitioners, take home remedies, a few medicines from a chemist's shop. Very few populations know [about TB]. There is a lack of awareness in the mass. Most who are educated are aware, but not everybody is [educated]. Especially in India, education status is less in women so they are much less aware. Increasing awareness and education for women is the next step.” (District TB Officer.)
Few (2/13) women (both age <25 years) had heard of TB before their diagnosis. Five women reported that their community does not know about TB even after their diagnosis. Before diagnosis, none knew what causes TB, what treatment consists of, or how severe TB is.
There is also a lack of awareness about free governmental services. Most women were symptomatic for one to five months due to care by unqualified practitioners and ignoring or self-treating symptoms. Delay was longer for older women, reflecting greater lack of TB knowledge. Eight women sought help from a practitioner, mostly private physicians, who did not diagnose their TB before they ultimately received a proper diagnosis. Health care providers confirmed this is a major problem.
“90 percent of the patients are below the poverty line yet they rely on the private sector. The Indian government is giving full support to eradicate TB, yet they [patients] prefer to first spend money in the private sector. But the private doctors just want more money; they diagnose wrongly and give another treatment. Then when the patient is conditioned to die, when money is over and gone, they refer to the TB Hospital.” (TB Nurse.)
Discussion
India's current TB treatment initiative, the Revised National Tuberculosis Control Program (RNTCP) which utilizes the directly observed treatment-short course (DOTS), has shown to be standard and effective. However, it assumes that women can recognize TB symptoms and feel confident to seek treatment. While women face complex and diverse obstacles to TB diagnosis, this small-scale study has suggested that the most prominent barriers are likely different given their ages. Younger women more greatly face socio-cultural barriers and stigma, while older women face knowledge-based barriers to diagnosis. These distinctions and nuances are important to further investigate as they are necessary for the development of an equitable TB control program.(8)
Sharma et al. identified that the gender gap in the prevalence of TB has widened which they attributed to higher underreporting due to social stigma and lack of health seeking behavior.(9) Our study supports their finding; however, we also found that even when women exhibited health seeking behavior they received delayed care because of their lack of knowledge regarding TB and lack of awareness in free government services. Concurrent with previous studies, many patients first sought care from private practices, most of which have no access to TB training programs.(10)
Not only are women less likely to seek a diagnosis, but Dhuria et al. found that women with TB have a quantitatively lower quality of life than men.(11) By decreasing stigma surrounding TB and by increasing access to information regarding TB, the two greatest barriers to diagnosis found in this study, treatment is more likely to succeed. Continuing research and implementation of gender-sensitive approaches are needed to supplement the current approach to TB control to reduce the barriers women face and the diagnostive disparity between women and men.(8)
Footnotes
Source of Support: Nil
Conflicts of interest: None declared.
References
- 1.Geneva, Switzerland: WHO; 2013. World Health Organization. Global Tuberculosis Report 2013. WHO/HTM/TB/2013.11; pp. 12–13. [Google Scholar]
- 2.Buckshee K. Impact of roles of women on health in India. Int J Gynecol Obstet. 1997;58:35–42. doi: 10.1016/s0020-7292(97)02887-7. [DOI] [PubMed] [Google Scholar]
- 3.Uplekar MW, Rangan S, Weiss MG, Ogden J, Borgdorff MW, Hudelson P. Attention to gender issues in tuberculosis control. Int J Tuberc Lung Dis. 2001;5:220–4. [PubMed] [Google Scholar]
- 4.Borgdorff MW, Hagelkerke NJ, Dye C, Nunn P. Gender and tuberculosis: A comparison of prevalence surveys with notification data to explore sex differences in case detection. Int J Tuberc Lung Dis. 2000;4:123–32. [PubMed] [Google Scholar]
- 5.Hudelson P. Gender differentials in tuberculosis: The role of socio-economic and cultural factors. Tuber Lung Dis. 1996;77:391–400. doi: 10.1016/s0962-8479(96)90110-0. [DOI] [PubMed] [Google Scholar]
- 6.Thorson A, Hoa NP, Long NH. Health-seeking behaviour of individuals with a cough of more than 3 weeks. Lancet. 2000;356:1823–4. doi: 10.1016/s0140-6736(00)03241-4. [DOI] [PubMed] [Google Scholar]
- 7.Mehta PC. New Delhi, India: Discovery Pub House; 2005. Marriages in Indian Society. [Google Scholar]
- 8.Courtwright A, Turner AN. Tuberculosis and stigmatization: Pathways and interventions. Public Health Rep. 2010;125(Suppl 4):34–42. doi: 10.1177/00333549101250S407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma PP, Kumar A, Singh P. A study of gender differentials in the prevalence of tuberculosis based on NFHS-2 and NFHS-3 data. Indian J Community Med. 2010;35:230–7. doi: 10.4103/0970-0218.66869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verma R, Khanna P, Mehta B. Revised national tuberculosis control program in India: The need to strengthen. Int J Prev Med. 2013;4:1–5. [PMC free article] [PubMed] [Google Scholar]
- 11.Dhuria M, Sharma N, Ingle GK. Impact of tuberculosis on the quality of life. Indian J Community Med. 2008;33:58–9. doi: 10.4103/0970-0218.39249. [DOI] [PMC free article] [PubMed] [Google Scholar]


