Abstract
INTRODUCTION:
Both converted and difficult laparoscopic cholecystectomies (LC) have impact on operating time and training of juniors. The aim of this study is to evaluate parameters that predict difficult LC or conversion (C), and find predictive values for different cut-off points of C-reactive protein (CRP) for conversion.
MATERIALS AND METHODS:
A retrospective cohort study of cholecystectomies performed from January 2011 to December 2012 at NHS trust was undertaken. Association of intra-operative difficulties or conversion with the following factors was studied: Age, gender, CRP, white blood cell count (WBC), history of pancreatitis, and endoscopic retrograde cholangiopancreatography (ERCP).
RESULTS:
Two hundred and ninety one patients were analysed (222 laparoscopic, 45 difficult LC and 24 C). Only 141 patients had a recorded CRP. Median CRP was highest for patients who were converted (286.20) compared to those who had difficult LC (67.40) or LC (7.05). Those patients who did not have preoperative CRP (8/150, 5.3%) had less chance of conversion than those who had CRP (16/141, 11.34%) (P = 0.063). Patients with CRP of ≤220 (3/91, 3.2%) had significantly less chance of conversion than those with CRP >220 (13/21, 61.9%) (P < 0.001). High preoperative CRP, WBC count and ERCP, were predictors of conversion. These factors were only marginally better than CRP alone in predicting conversion.
CONCLUSION:
CRP can be a strong predictor of conversion of LC. Further validation of the results is needed.
Keywords: C-reactive protein, difficult dissection, laparoscopic cholecystectomy, predicting conversion
INTRODUCTION
Laparoscopic cholecystectomy (LC) can be the easiest or the most difficult laparoscopic operation. Conversion to open surgery has been a traditional marker of difficult LC and anticipation of conversion can help in consenting patients and preparing them for longer stay and complications. Though not appreciated widely, difficult LC can have similar implications, as conversion to open operation, in terms of operating time, expertise required for an operation and training of juniors.
In the early days of laparoscopic surgery conversion of LC was influenced by multiple factors like patient characteristics (high body mass index, previous abdominal surgery), anatomical variations of extra-hepatic biliary system and gallbladder (GB) pathology (severe inflammation of GB or common bile duct [CBD]). The studies from early 1990s found significant association of conversion with advancing age, male gender, obesity, previous abdominal surgery, previous endoscopic retrograde cholangiopancreatography (ERCP), and ultrasonogrphic findings (USS) like GB wall thickness etc.[1,2,3,4,5,6,7] With increasing experience in laparoscopic surgery and advancement of technology many of the difficulties due to anatomical and patient factors could be dealt with laparoscopically.[8] As a result LC was increasingly offered to patients with acute cholecystitis (AC). The subsequent studies showed that GB wall thickness on ultrasound scan was a strong predictor of conversion of LC for AC.[9,10,11,12] These conversions were related to the inflammation of the GB and were more relevant in terms of bile duct injury.
Meta-analysis comparing results of emergency and delayed LC[13] showed no difference in conversion rates[14] implying that once GB is significantly inflamed delaying the surgery doesn’t necessarily make the operation easier, or avoids conversion.
C-reactive protein (CRP) is an acute phase reactant protein secreted by the liver in response to interleukin-6 and other pro-inflammatory cytokines in the context in inflammation, infection, trauma, malignancy and tissue infarction.[15,16,17] Its circulating concentration is determined by its rate of synthesis reflecting the intensity of the pathological process, and hence it is a good indicator of severity of inflammation.[18]
In our practice it was observed that many of the patients who had their LC converted to open surgery (either emergency or delayed) had very high CRP at the time of their index admission for GB pathology. Even for those who were not converted, LC were difficult if their preoperative CRP levels were moderately raised.
We hypothesised that high preoperative CRP level due to GB pathology-either biliary colic or AC, is associated with intraoperative difficulties and conversion. Very few studies have looked at CRP as predictor of conversion of LC.[11,12]
The aim of this study is:
To separately examine CRP and other factors responsible for “difficult LC” and those responsible for “conversion.”
To assess the association between the highest recorded CRP at index admission for GB pathology and intraoperative difficulty/conversion irrespective of the timing of surgery-early or delayed.
To assess predictive value of different CRP cut-off points for conversion to open surgery.
MATERIALS AND METHODS
This is a retrospective cohort study of all the consecutive patients who had cholecystectomies performed by a single upper gastrointestinal surgeon or by his trainees under his direct supervision in a single NHS Trust in the UK from January 2011 to December 2012 [Figure 1].
Figure 1.
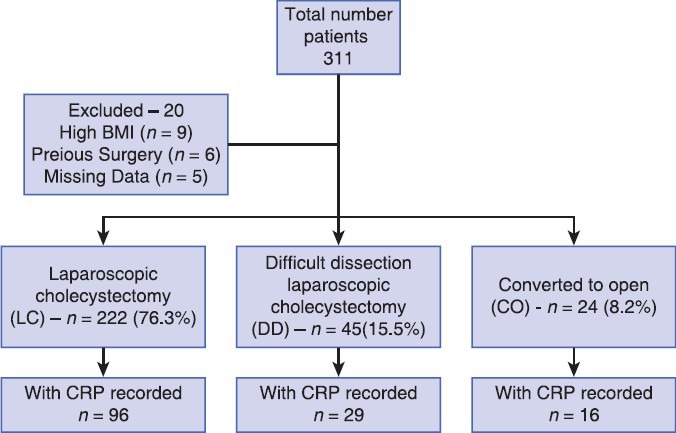
Flowchart showing patient distribution in three groups
Inclusion Criteria
All the patients 18 years and above who had cholecystectomy-either in emergency or delayed.
Exclusion Criteria
As the study aims to look at the association between CRP and difficult cholecystectomy/conversion due to GB pathology only, the following patients were excluded to avoid confounding effect of these factors on difficulty/conversion.
However separate account of these patients is given in results section.
High BMI (>35).
Previous abdominal surgery.
Those with incomplete data.
Highest recorded CRP (mg/L), and white blood cell count (WBC) (×109/L), on admission for gallstone related emergencies were recorded for all the patients.
Other parameters recorded include: Age, gender, presence/absence of CBD stones, ERCP and pancreatitis.
Intraoperative difficulty and its cause were identified by operative findings.
Statistical Analysis
Statistical analysis was performed using statistical packages Stata[19] (StataCorp. 2009. Stata Statistical Software: Release 11. College Station, TX) and StatsDirect.[20] Complete data were used for the statistical analysis.
The Shapiro-Wilk test was used to determine whether continuous variables could be assumed to have a normal distribution. The result of the normality test determined whether statistical analysis would be performed using a two sample t-test or Mann-Whitney U-test for continuous variables. A Chi-squared test or Fisher's exact test was used for categorical variables. These tests were used to compare laparoscopic with difficult dissection (DD) data and with conversion to open, respectively. These tests were also used to compare DD and conversion to open, in order to determine whether these two groups could be combined for analysis.
Univariate analysis and multiple logistic regression analysis were used to explore which variables were statistically significant in predicting a DD or conversion to open surgery respectively. Firstly, this analysis was performed on the overall complete data set, however CRP was not included in the modelling since CRP was recorded for a subset of the complete data. The diagnostic accuracy of CRP in predicting a DD or conversion to open surgery was investigated alone and in addition to other variables for the subset of patients who had a recorded preoperative CRP.
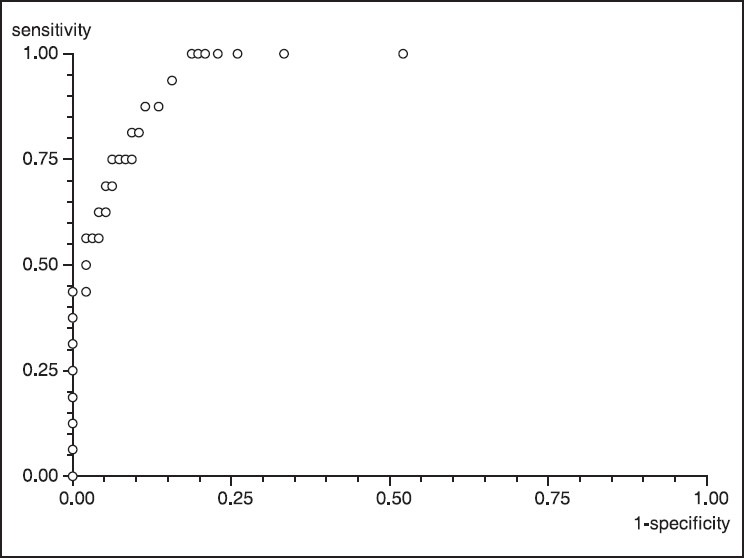
Receiver operating characteristic (ROC) curve analysis was used to identify a cut-off threshold to dichotomise CRP. ROC analysis was also used to investigate the diagnostic accuracy of significant variables in predicting a DD or conversion to open surgery respectively. An area under the ROC (AUROC) of 0.7-0.8 was regarded as acceptable, 0.8-0.9 was regarded as excellent, and >0.9 was regarded as outstanding.[21]
A P < 0.05 determined significance and a P < 0.1 was used to retain variables in a regression equation.
RESULTS
During the study period, 311 patients underwent cholecystectomy [Table 2]. Those patients who were admitted through the clinic for cholecystectomy, usually referred by the general practitioner-did not have their CRP done (n = 150) and those who attended/admitted to hospital with severe biliary symptoms had their CRP done in hospital (n = 141). These 141 patients formed the study group: 96 (68.1%) L, 29 (20.6%) DD and 16 (11.3%) C [Figure 1]. All the difficulties/conversions in this study group refer to difficulty in getting satisfactory views of the Calot's triangle. The rate of conversion was higher in patients with preoperative CRP than those without (16/141, 11.34%, vs. 8/150, 5.3%, P = 0.063)
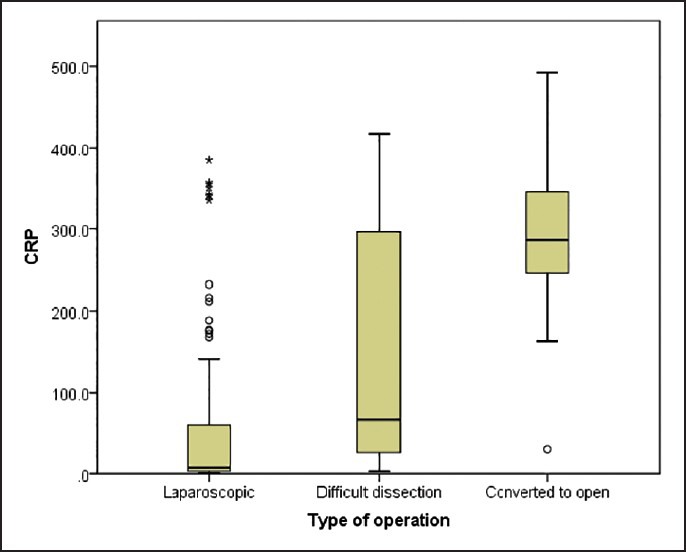
Table 2.
Distribution of difficult LC and converted patients in the cohort
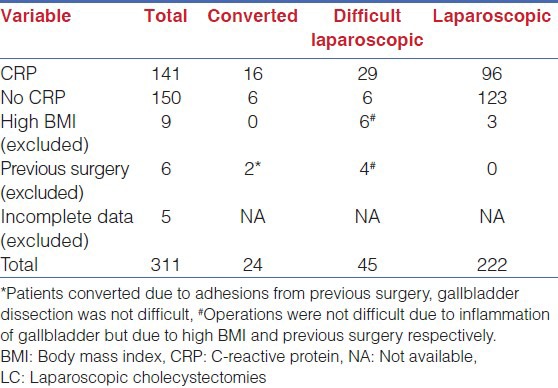
Median CRP was highest for patients who were converted to open surgery from laparoscopic [Figure 2].
Figure 2.
Box plot of C-reactive protein by type of operation (n = 141, laparoscopic = 96, difficult dissection = 29 and conversion = 16)
Comparison of the Three Surgical Groups
A higher percentage of the patients who were converted to open surgery had ERCP (P = 0.001) and CBD stones (P = 0.002) compared with patients who had a DD. Patients who were converted to open surgery also had a significantly higher CRP on average (P = 0.001) compared with patients who had DD. Since there were some significant differences between the two groups, it was decided that patients in the DD group would not be combined with patients who were converted (C) for analysis [Table 2].
Patients in the DD group were significantly older, had significantly higher CRP and WBC, and a higher percentage of males compared with patients in the L group [Table 1].
Table 1.
The comparison of patients who had LC with difficult dissection and conversion to open surgery groups, respectively
Patients in the C group were significantly older, had significantly higher CRP and WBC, a higher percentage of males and a higher percentage of patients with ERCP and CBD stones present compared with patients in the L group [Table 2].
A significant high association was found between the presence of ERCP and the presence of CBD stones in all the three groups of patients, laparoscopic (L) (P < 0.001), DD (P = 0.001) and C (P < 0.001). Hence, it was decided that ERCP rather than CBD stones would be included as a covariate in the logistic regression models for predicting DD and conversion to open surgery.
Ninety six of the 112 patients did not have ERCP and 9 (9.4%) of these were converted to open surgery. Of the remaining 16 patients who had preoperative ERCP, 7 (43.7%) were converted.
Conversion to Open Surgery Compared to Laparoscopic
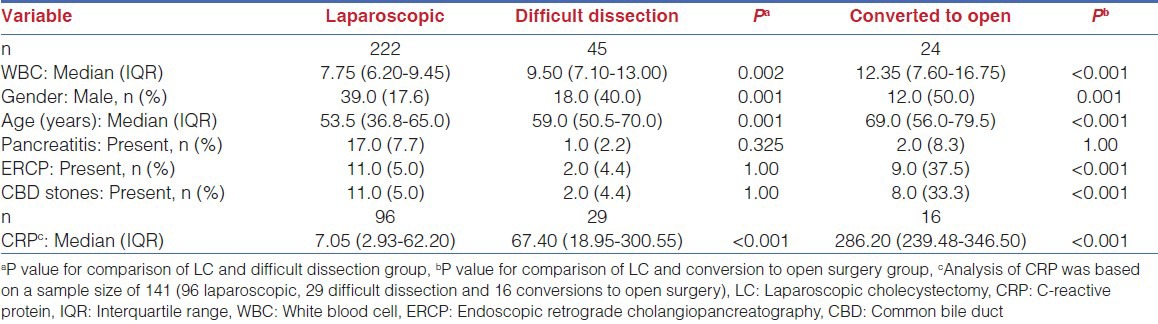
The diagnostic accuracy of CRP on its own in predicting a conversion to open surgery was modelled for the group of patients who had a recorded preoperative CRP (n = 112, C = 16). Univariate analysis showed that CRP was found to be significant in predicting whether a patient would be converted to open surgery (P < 0.001, odds ratios [OR] = 1.013, 95% confidence interval [CI] 1.008-1.019).
The AUROC was 0.925, with a 95% CI 0.873-0.977 [Figure 3]. This showed that CRP alone was “outstanding” at separating patients who are likely to have a conversion to open surgery from laparoscopic patients. Sensitivity of CRP as a continuous measure was 43.75% with a 95% CI 19.75-70.12, specificity was 92.71% (85.55-97.02), positive predictive value (PPV) was 50.0% (23.04-76.96) and negative predictive value (NPV) was 90.82% (83.28-95.71).
Figure 3.
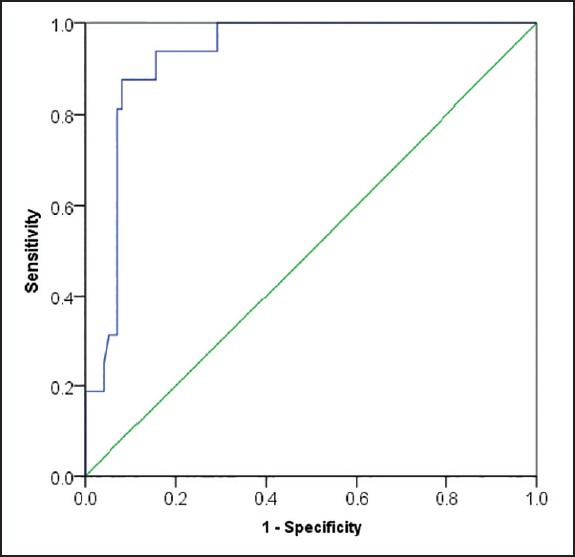
Receiver operating characteristic curve for C-reactive protein (n = 112)
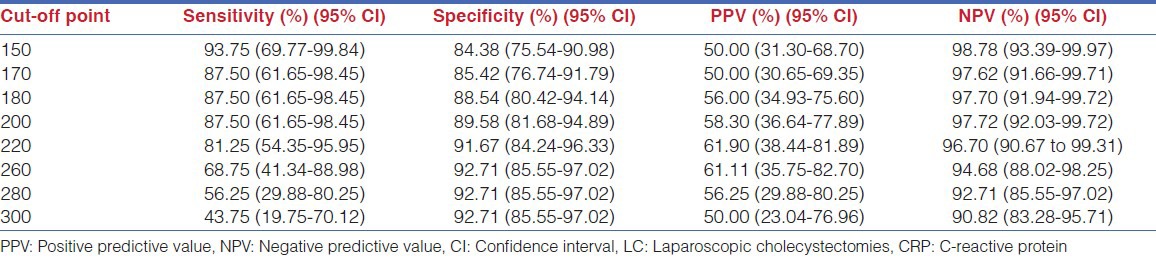
The diagnostic accuracy for different cut-off points of CRP was calculated. Table 3 shows that 220 was the best cut-off point for CRP, in terms of sensitivity/(1-specificity), when predicting conversion of LC to open surgery. Of the laparoscopic and converted patients, 112 patients had a preoperative CRP recorded. Ninety-one patients were coded as having low (0-220) CRP, of these 3 (3.2%) were converted; and of twenty one patients coded as having high (>220) CRP, 13 (61.9%) were converted to open (P < 0.001).
Table 3.
Sensitivity, specificity, PPV and NPV for different cut-off points for CRP when predicting conversion of LC to open surgery (n = 112, conversion = 16)
Univariate analyses showed that in addition to CRP (P < 0.001); WBC (P < 0.001), ERCP (P = 0.001) and age (P = 0.025) were also significant in predicting whether a patient would have a conversion of LC [Table 4].
Table 4.
Unadjusted and adjusted OR from univariate analyses and multiple logistic regression analysis, respectively for laparoscopic versus conversion to open for all patients (n = 112)
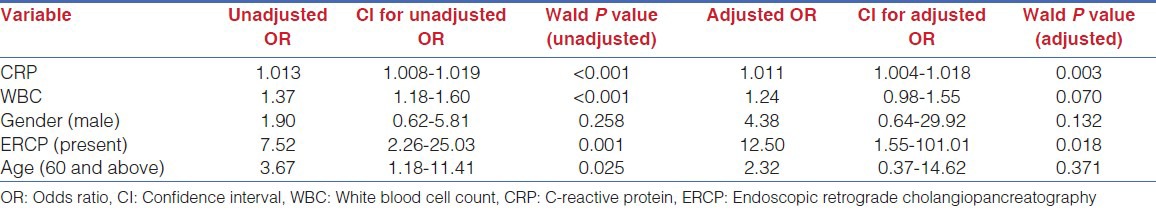
When multiple logistic regression analysis was performed, the variables CRP, WBC and ERCP were still found to be significant in predicting conversion, even after adjusting for the other variables. The model was refitted retaining only CRP, WBC and ERCP [Table 5].
Table 5.
Unadjusted and adjusted OR from univariate analyses and multiple logistic regression analysis, respectively for laparoscopic versus conversion to open for patients who had preoperative CRP (n = 112, conversion = 16)
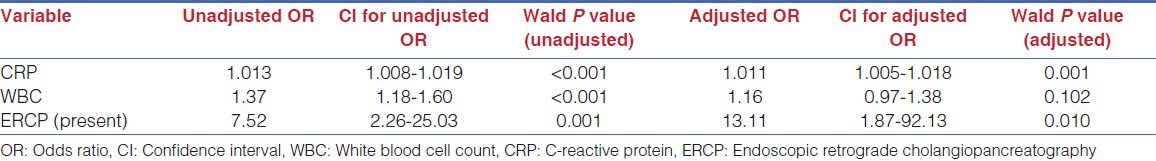
The AUROC for this model was 0.956, with a 95% CI (0.919-0.992) [Figure 4]. This shows that looking at a patients CRP, WBC and whether they had ERCP present would be considered to be “outstanding” at separating converted from laparoscopic patients. Sensitivity of this model was 56.25% with a 95% CI (29.88-80.25), specificity was 95.83% (38.57-90.91), PPV was 69.23% (38.57-90.91) and NPV was 92.93% (85.97-97.11).
Figure 4.
Receiver operating characteristic curve for model produced in Table 5
The AUROC, sensitivity, specificity, PPV and NPV increased when variables WBC and ERCP were also included as predictive variables in the model compared to CRP alone.
Difficult Dissection Compared to Laparoscopic
The diagnostic accuracy of CRP in predicting a DD from L was modelled for patients who had a recorded preoperative CRP (n = 125, DD = 29). Univariate analysis showed that CRP was significant in predicting whether a patient would have a DD (P = 0.003, OR = 1.005, 95% CI 1.002-1.008).
The AUROC for continuous CRP was 0.731, with a 95% CI 0.632-0.830.
This showed that CRP was “acceptable” at separating DD from laparoscopic patients. Sensitivity for CRP as a continuous measure was 13.79% with a 95% CI 3.89-31.66, specificity was 92.71% (85.55-97.02).
Positive predictive value was 36.36% (10.93-69.21) and NPV was 78.07% (69.35-85.28).
Univariate analyses showed that in addition to CRP (P = 0.003), WBC (P = 0.001), gender (P = 0.033) and pancreatitis (P = 0.088) were significant in predicting whether a patient would have a DD.
With multiple logistic regression analysis, CRP, WBC and pancreatitis were still significant in predicting whether a patient would have a DD, even when adjusted for the other variables. Gender was no longer significant. The adjusted OR produced from the refitted model were CRP (P = 0.012, OR = 1.007, 95% CI [1.001-1.012]), WBC (P = 0.049, OR = 1.12 [1.00-1.26]) and pancreatitis (P = 0.007, OR = 0.03 [0.003-0.38]).
The AUROC for this model was 0.782, with a 95% CI 0.678-0.886. This showed that CRP, WBC and presence of pancreatitis was “acceptable” at separating DD from laparoscopic patients. Sensitivity of this model was 31.03% with a 95% CI 15.28-50.83, specificity was 97.92% (92.68-99.75), PPV was 81.82% (48.22-97.72) and NPV was 82.46% (74.21-88.94).
DISCUSSION
In this study, the median CRP was significantly higher in the patients converted to open operation (286.2) compared to those with difficult LC (67.4) and laparoscopic group (7.05) [Figure 2].
Patients admitted through the clinic (who did not have preoperative CRP) had less chance of conversion to open than those who attended hospital for biliary symptoms (and had CRP done) (8/150 vs. 16/141, P = 0.063). High CRP of >220 increased the possibility of conversion even further (13/21 vs. 3/91, P < 0.001).
This is the first study to assess value of CRP as a sole predictor of conversion. Two other studies have evaluated predictive value of CRP along with other parameters.[11,12] In a study for AC by Schäfer et al., CRP level on admission along with American Society of Anaesthesiology grade, duration of symptoms, age and WBC count on admission were found to be determinants of surgical approach-laparoscopic or open.[11] Another recent study for AC found that CRP level at admission (≥3.6 mg/dL) and male gender were strongly related to conversion of emergency LC.[12] Our study looked at peak CRP level during acute admission and showed that, 61.9% patients who had CRP >220 mg/L during their index admission were converted irrespective of timing of operation-emergency or delayed.
This finding highlights the fact that once severe inflammation sets in, delaying surgery in these patients does not make the operation easier or prevents conversion. A recent meta-analysis of using CRP to predict anastomotic leak after colorectal surgery has shown the value of CRP as a negative predictor. The same may be true for predicting conversion of LC, as suggested in this study (3.2% conversion if CRP ≤220).
Factors other than GB pathology leading to conversion, though important, are not specific for cholecystectomy (e.g., previous surgery, high BMI), can sometimes be unpredictable (e.g., adhesions due to previous surgery), and do not have direct impact on complication specific to cholecystectomy like bile duct injury. For this reason we feel that difficult LC and conversions specifically due to GB pathology are clinically more relevant and are addressed in this study.
As far as we are aware this is the first study to use “difficult LC” and “conversion” as two separate markers of difficulties related to GB pathology. Two studies have been done previously to predict difficult LC rather than predicting conversion.[22,23] Randhawa and Pujahari looked at 15 factors that make the operation difficult, but not necessarily requiring conversion.[22] The other study by Sakuramoto et al. is the only study that looked at “difficult LC due to GB pathology” — a concept similar to ours, but required 41 factors to predict intraoperative difficulties. Authors have graded inflammation of GB in four categories based on histopathological findings and correlated these grades with intraoperative difficulties.[23] These difficulties in turn correlated well with “time taken for GB dissection” than with total operating time and could be predicted preoperatively.
It was previously thought that LC has less morbidity than open cholecystectomy even if it takes longer time.[24] However, Giger et al. in their analysis of 22,953 patients from Swiss database have shown that risk of complications of LC is increased with conversion as well as with longer operating time (for, e.g., difficult LC).[1] The authors claim that addition of each 30 min duration increases chances of both local and systemic postoperative complications. This finding demonstrates why predicting difficult LC is as important as predicting conversion. This study and another one by Alponat et al. have shown experience of surgeon as predictor of conversion.[8] It is possible that total number of difficult LC and conversions may be constant for given population and proportion of conversions may reduce with increasing experience of a surgeon.
Due to retrospective nature of this study the investigated variables have been limited to objective measures such as laboratory results, radiological findings and preoperative complication of gallstone disease (pancreatitis and CBD stones). We have not incorporated other important variables like physical examination due to subjective nature. In previous studies, USS diagnosed wall thickness is shown to be an important predictor of conversion particularly for emergency cholecystectomy. In our hospital this is not routinely measured and hence could not be included in the study.
Other limitations of the study is the small numbers and lack of grading of intraoperative difficulties. If grading was available conversion would have been highest grade of difficulty. The study also lacks the data for preoperative admissions to the nearby trusts.
SUMMARY
Our study shows a strong association between peak preoperative CRP levels and GB pathology related conversions. At a cut-off point of 220, CRP has high positive as well as NPV. CRP on its own appears to be a good independent predictor of conversion.
Considering strong correlation of CRP and ERCP with conversion it may be possible to develop a simple scoring system. Prospective validation of these findings is necessary and is underway in our institution.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
REFERENCES
- 1.Giger UF, Michel JM, Opitz I, Th Inderbitzin D, Kocher T, Krähenbühl L, et al. Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: Analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J Am Coll Surg. 2006;203:723–8. doi: 10.1016/j.jamcollsurg.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 2.Sharma SK, Thapa PB, Pandey A, Kayastha B, Poudyal S, Uprety KR, et al. Predicting difficulties during laparoscopic cholecystectomy by preoperative ultrasound. Kathmandu Univ Med J (KUMJ) 2007;5:8–11. [PubMed] [Google Scholar]
- 3.Târcoveanu E, Niculescu D, Georgescu S, Epure O, Bradea C. Conversion in laparoscopic cholecystectomy. Chirurgia (Bucur) 2005;100:437–44. [PubMed] [Google Scholar]
- 4.Tayeb M, Raza SA, Khan MR, Azami R. Conversion from laparoscopic to open cholecystectomy: Multivariate analysis of preoperative risk factors. J Postgrad Med. 2005;51:17–20. [PubMed] [Google Scholar]
- 5.Ilie AC, Nica C, Szucsik IA, Motoc A, Sava A, Grosu S. Preoperative ultrasonography as a mean of predicting the conversion of mini cholecystectomy into classic cholecystectomy. Rev Med Chir Soc Med Nat Iasi. 2009;113:1136–40. [PubMed] [Google Scholar]
- 6.Rosen M, Brody F, Ponsky J. Predictive factors for conversion of laparoscopic cholecystectomy. Am J Surg. 2002;184:254–8. doi: 10.1016/s0002-9610(02)00934-0. [DOI] [PubMed] [Google Scholar]
- 7.Takegami K, Kawaguchi Y, Nakayama H, Kubota Y, Nagawa H. Preoperative grading system for predicting operative conditions in laparoscopic cholecystectomy. Surg Today. 2004;34:331–6. doi: 10.1007/s00595-003-2714-0. [DOI] [PubMed] [Google Scholar]
- 8.Alponat A, Kum CK, Koh BC, Rajnakova A, Goh PM. Predictive factors for conversion of laparoscopic cholecystectomy. World J Surg. 1997;21:629–33. doi: 10.1007/pl00012288. [DOI] [PubMed] [Google Scholar]
- 9.Cwik G, Skoczylas T, Wyroslak-Najs J, Wallner G. The value of percutaneous ultrasound in predicting conversion from laparoscopic to open cholecystectomy due to acute cholecystitis. Surg Endosc. 2013;27:2561–8. doi: 10.1007/s00464-013-2787-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Halachmi S, DiCastro N, Matter I, Cohen A, Sabo E, Mogilner JG, et al. Laparoscopic cholecystectomy for acute cholecystitis: How do fever and leucocytosis relate to conversion and complications? Eur J Surg. 2000;166:136–40. doi: 10.1080/110241500750009483. [DOI] [PubMed] [Google Scholar]
- 11.Schäfer M, Krähenbühl L, Büchler MW. Predictive factors for the type of surgery in acute cholecystitis. Am J Surg. 2001;182:291–7. doi: 10.1016/s0002-9610(01)00702-4. [DOI] [PubMed] [Google Scholar]
- 12.Teckchandani N, Garg PK, Hadke NS, Jain SK, Kant R, Mandal AK, et al. Predictive factors for successful early laparoscopic cholecystectomy in acute cholecystitis: A prospective study. Int J Surg. 2010;8:623–7. doi: 10.1016/j.ijsu.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 13.Ercan M, Bostanci EB, Teke Z, Karaman K, Dalgic T, Ulas M, et al. Predictive factors for conversion to open surgery in patients undergoing elective laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2010;20:427–34. doi: 10.1089/lap.2009.0457. [DOI] [PubMed] [Google Scholar]
- 14.Lau H, Lo CY, Patil NG, Yuen WK. Early versus delayed-interval laparoscopic cholecystectomy for acute cholecystitis: A metaanalysis. Surg Endosc. 2006;20:82–7. doi: 10.1007/s00464-005-0100-2. [DOI] [PubMed] [Google Scholar]
- 15.Black S, Kushner I, Samols D. C-reactive protein. J Biol Chem. 2004;279:48487–90. doi: 10.1074/jbc.R400025200. [DOI] [PubMed] [Google Scholar]
- 16.Cole DS, Watts A, Scott-Coombes D, Avades T. Clinical utility of peri-operative C-reactive protein testing in general surgery. Ann R Coll Surg Engl. 2008;90:317–21. doi: 10.1308/003588408X285865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vigushin DM, Pepys MB, Hawkins PN. Metabolic and scintigraphic studies of radioiodinated human C-reactive protein in health and disease. J Clin Invest. 1993;91:1351–7. doi: 10.1172/JCI116336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pepys MB, Hirschfield GM. C-reactive protein: A critical update. J Clin Invest. 2003;111:1805–12. doi: 10.1172/JCI18921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.StataCorp. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- 20.England: StatsDirect Ltd; 2013. StatsDirect Ltd. StatsDirect statistical software. http://www.statsdirect.com . [Google Scholar]
- 21.Hosmer DW, Jr, Lemeshow S, Sturdivant RX. Applied Logistic Regression. 3rd ed. Hoboken, New Jersey: John Wiley & Sons; 2013. [Google Scholar]
- 22.Randhawa JS, Pujahari AK. Preoperative prediction of difficult lap chole: A scoring method. Indian J Surg. 2009;71:198–201. doi: 10.1007/s12262-009-0055-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakuramoto S, Sato S, Okuri T, Sato K, Hiki Y, Kakita A. Preoperative evaluation to predict technical difficulties of laparoscopic cholecystectomy on the basis of histological inflammation findings on resected gallbladder. Am J Surg. 2000;179:114–21. doi: 10.1016/s0002-9610(00)00248-8. [DOI] [PubMed] [Google Scholar]
- 24.Habib FA, Kolachalam RB, Khilnani R, Preventza O, Mittal VK. Role of laparoscopic cholecystectomy in the management of gangrenous cholecystitis. Am J Surg. 2001;181:71–5. doi: 10.1016/s0002-9610(00)00525-0. [DOI] [PubMed] [Google Scholar]


