Abstract
Laparoscopic splenectomy is a gold standard for management of planned benign splenic pathologies. Spontaneous rupture of the spleen (SRS) leading to acute abdomen occurs in only 1% of all splenic ruptures. Laparoscopic splenectomy in traumatic and atraumatic rupture due to intra-splenic pathology is reported. We present the first reported case of laparoscopic splenectomy in a 23-year-old male who presented with hemoperitoneum due to idiopathic or SRS. The procedure was safely accomplished with slight modified technique and minimum usage of advanced gadgets.
Keywords: Acute abdomen, atraumatic splenic rupture, hemoperitoneum, laparoscopic splenectomy, spontaneous splenic rupture
INTRODUCTION
Abdominal trauma is the most common cause of splenic rupture. Spontaneous splenic rupture (SRS) is a life-threatening abdominal emergency, occurring in only 1% of all splenic ruptures.[1] Atraumatic splenic rupture usually occurs due to an underlying detectable disease process referred to as ‘pathological splenic rupture’. These are secondary to infectious, haematological, or malignant infiltration of spleen. These account for 93% of cases while the term ‘SRS’ refers to the idiopathic variety of atraumatic rupture and accounts for 7% of cases.[2] Strong index of suspicion is required to diagnose and manage it. Conservative approach for traumatic splenic rupture is well-established; however, mortality of conserved spleens in idiopathic splenic rupture at 30 days is 22%.[3] Moreover, pathological diagnosis of the cause of the rupture can be made only after surgical intervention. Lack of technical support and haemodynamic instability necessitates exploratory laparotomy in many patients. Laparoscopic splenectomy is a well-established surgical technique for elective splenectomy and was offered in this patient who presented with hemoperitoneum due to SRS. The surgery was accomplished within acceptable time span and minimum usage of advanced gadgets, emphasizing feasibility of laparoscopy in presence of haemorrhage.
CASE REPORT
A 23-year-old male was referred to our emergency department with acute onset abdominal pain of 12 h duration. Pain was associated with nausea and giddiness. Preliminary abdominal sonography done at the primary hospital showed presence of free fluid in the pelvis and left hypochondrium. The patient was shifted for computed tomography (CT) scan, where he collapsed, and test abandoned. He responded to fluid challenge and referred to higher centre for further management.
On admission, his pulse was 94/m with systolic blood pressure 90/60 mm, oxygen saturation of 90%. There was tenderness in left hypochondrium and periumbilical region but had no history or signs of external trauma. Intravenous fluids were given, and he was shifted for CT scan of the abdomen which revealed a 7 cm × 6 cm sub-capsular peri-splenic haematoma with moderate hemoperitoneum in peri-hepatic area, paracolic gutters and pelvis [Figure 1].
Figure 1.
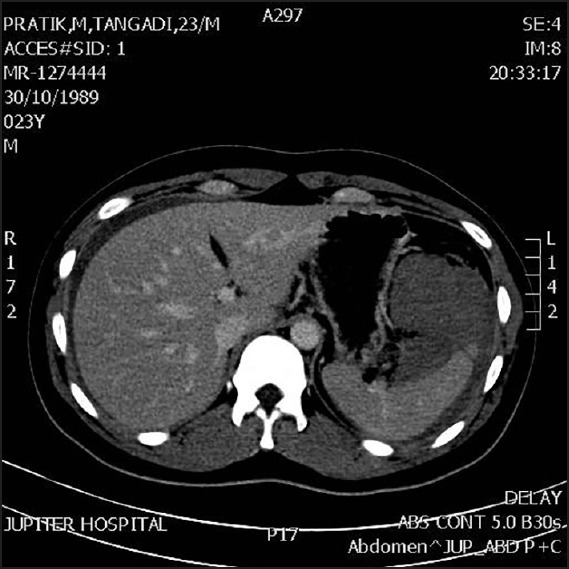
Computed tomography scan showing normal sized spleen with perisplenic haematoma
The patient was monitored in Intensive Care Unit, kept nil by mouth, started on intravenous antibiotics and analgesics. Blood investigations showed haemoglobin (Hb) of 14 g%, white blood cells of 15,400/cumm and platelet count of 280 × 1000/cumm with normal coagulation profile. Since there was no history of trauma, a detailed workup was done for the cause of splenic rupture, tests for typhoid, dengue, malaria, leptospirosis, infectious mononucleosis were negative.
Repeat Hb at 6 h showed a drop to 11 g%. Abdominal discomfort and pain persisted with features of localised guarding in the left hypochondrium. A repeat abdominal sonography showed an increase in the hemoperitoneum. Considering the persistent pain, drop in Hb and increasing hemoperitoneum, we subjected him for laparoscopic sos open surgical intervention. Supine with leg split and reverse Trendelenburg position was given. The camera port was trans-umbilical, and the port for liver retraction was also in the midline, at xiphisternum. Working ports were 5 mm midway between umbilicus and xiphisternum and 10 mm port in left periumbilical region, additional 5 mm in left anterior axillary line was made for splenic retraction. The operating surgeon stood between the legs, whereas camera surgeon on patient's right side and 2nd assistant on the left side. There was 1000cc of hemoperitoneum with clots in the perisplenic, perihepatic and pelvic region [Figure 2]. The spleen size and surface was normal except for a small capsular breach on the medial surface. There was no obvious parenchymal laceration or tear. The splenic vessels were normal. The liver and other abdominal organs were normal. After sucking out intraperitoneal blood and clots, continuous trickle of bright red ooze was evident from the medial surface of the splenic parenchyma. Hence, we proceeded for splenectomy. Ultrasonic scissors were used, and splenic hilum dissected. We continued in the same position since hilar anatomy was well-visualised. Splenic artery was ligated with 2/0 silk, clipped doubly and cut. Splenic vein too was tackled in similar manner and spleen was carefully dissected free off its attachments. Operation time was 90 min; umbilical port incision was extended and spleen delivered intact after placement in a retrieval bag. Drainage tube was placed in splenic fossa through 5 mm flank port, and umbilical incision was closed meticulously with non-absorbable sutures.
Figure 2.
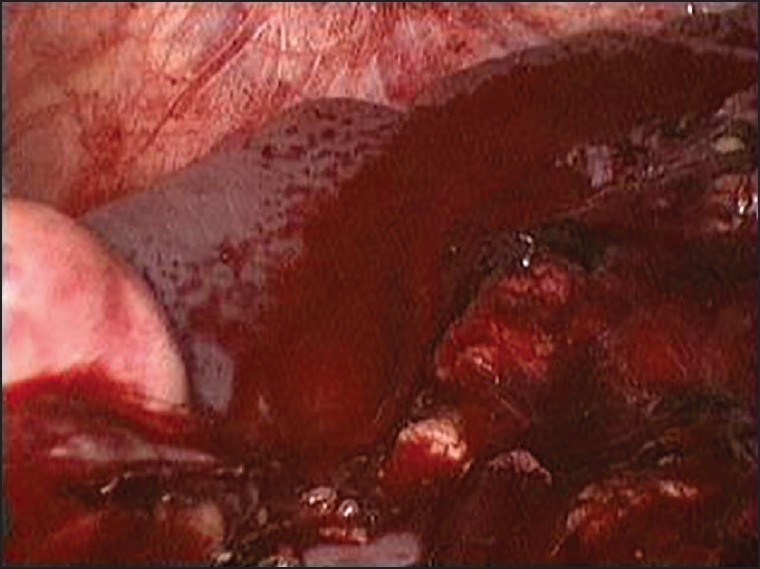
Intra-operative picture depicting hemoperitonuem with hilar ooze
Post-operative course was uneventful. His Hb was 9.9 g%, started on orals on day 1, drain removed and discharged on day 3 with a good cosmetic scar [Figure 3]. He was vaccinated against encapsulated bacterial organisms. Histopathology of the spleen did not reveal any abnormality except some congestion of hilar vessels. There was no evidence of vasculitis. There was no parasitic infiltration of spleen or any pathological cause of splenic rupture. Patient is stable at 24 months follow-up.
Figure 3.

Post-operative scar and port positions
DISCUSSION
Laparoscopic splenectomy in trauma was first reported by Basso et al. and Nasr et al., both these reports showed feasibility of the laparoscopic technique for delayed intervention in splenic trauma.[4,5] Since then, there have been case reports wherein laparoscopic splenectomy was safely accomplished immediately after trauma.[6]
Most reports on non-traumatic splenic rupture are due to pathological abnormality such as hamartoma, infectious mononucleosis, malaria, parasitic cyst rupture or iatrogenic rupture.
Conservative approach for traumatic splenic rupture is well-established; however mortality of conserved spleens in idiopathic splenic rupture at 30 days is 22%.[3]
The main issue in idiopathic cases is that the final diagnosis is post-surgical and only a working diagnosis can be formulated pre- or intra-operatively. This significantly affects the surgical decision making as seen in our case. Though the patient was haemodynamically stable with hemoperitoneum and perisplenic haematoma, drop in Hb by 3 g% with persistent pain and discomfort prodded us to do a laparoscopic evaluation. Intra-operatively the spleen appeared normal except the capsular breach on the medial surface with blood ooze. At this stage in an obvious case of traumatic rupture, splenorraphy would also be an option for management. However since the aetiology of the rupture was not confirmed we proceeded for splenic removal to assess histopathology and avoid delayed re-intervention.
Literature review on technical aspects of laparosocopic splenectomy in traumatic as well as atraumatic rupture has mentioned standard right lateral decubitus position. Suction of hemoperitoneum, clearance of haematoma from lesser sac, followed by hilar dissection are the basic steps. Quick control of haemorrhage being of prime importance, all have used vascular staplers for hilar control.[4,5,6]
In the present case, since the cause of hemoperitoneum was uncertain due to the absence of trauma; whole abdomen evaluation was contemplated. Hence instead of routine right decubitus position for ‘hanging spleen technique’, we preferred anterior approach. The port placements were slightly altered so that ports could be joined to perform a mid-line laparotomy if the need arose. Lesser sac was opened using harmonic shears; clot evacuated, and spleen assessed. Once we decided to proceed with organ removal, splenic artery was identified, dissected and ligated. Vein was tackled in a similar fashion. Experience in elective laparoscopic splenectomies using conventional instruments, helped in quick and safe hilar dissection, without usage of vascular stapler.[7] Maintenance of stable haemodynamics, good team work helped in safe and quick completion of surgery in 90 min without any major blood loss. Intact spleen retrieval is of utmost importance. Since the patient was thin built and umbilical port was used as camera port, trans-umbilical extension enabled intact delivery and good cosmetic scar.
There is a lack of data on optimal treatment protocols for cases of SRS as they are a rarity, more so the idiopathic variety. SRS was first reported by Rokintnsy in 1861.[1,2] However the term SRS is often misused to include all atraumatic splenic rupture which includes pathological spleen.
Orloff and Peskin in 1958 laid down a four point criteria for diagnosis of SRS consisting of no history of trauma, no perisplenic adhesions indicating previous trauma, no disease process involving spleen and presence of micro and macroscopic normal spleen.[8] History of pertinent viral infection and absence of viral antibody titters is an additional fifth criteria recommended by Crate and Payne in 1991.[9] The present case matched all the five criteria and was labelled as spontaneous non-traumatic, non-pathological splenic rupture causing hemoperitoneum. Thorough PubMed search did not reveal any reported case of laparosocopic spelnectomy in hemeoperitioneum due to SRS.
The patient recovered well post-operatively and was discharged in 72 h. Less pain, faster recovery, and shorter hospital stay are a proven advantage of the laparoscopic approach.[10]
CONCLUSION
Laparoscopic splenectomy can be considered as an option in splenic rupture in a patient with stable haemodynamics without any compromise on patient safety. SRS is an uncommon but important life-threatening clinical entity. Unfortunately, the diagnosis is often missed or delayed due to the absence of any history of trauma. Increased awareness of this condition would enhance early diagnosis and effective treatment by minimal invasive technique.
ACKNOWLEDGEMENT
We thank Dr. Ajay Thakker CEO of Jupiter Hospital for permitting us to publish hospital data for academic purposes.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
REFERENCES
- 1.Acar YA, Dedouglu E, Cevik E, Cinar O, Arslan D, Kesim E, et al. Spontaneous rupture of spleen as a rare cause of abdominal pain. Eur J Surg Sci. 2010;1:27–9. [Google Scholar]
- 2.Renzulli P, Hostettler A, Schoepfer AM, Gloor B, Candinas D. Systematic review of atraumatic splenic rupture. Br J Surg. 2009;96:1114–21. doi: 10.1002/bjs.6737. [DOI] [PubMed] [Google Scholar]
- 3.Görg C, Cölle J, Görg K, Prinz H, Zugmaier G. Spontaneous rupture of the spleen: Ultrasound patterns, diagnosis and follow-up. Br J Radiol. 2003;76:704–11. doi: 10.1259/bjr/69247894. [DOI] [PubMed] [Google Scholar]
- 4.Basso N, Silecchia G, Raparelli L, Pizzuto G, Picconi T. Laparoscopic splenectomy for ruptured spleen: Lessons learned from a case. J Laparoendosc Adv Surg Tech A. 2003;13:109–12. doi: 10.1089/109264203764654740. [DOI] [PubMed] [Google Scholar]
- 5.Nasr WI, Collins CL, Kelly JJ. Feasibility of laparoscopic splenectomy in stable blunt trauma: A case series. J Trauma. 2004;57:887–9. doi: 10.1097/01.ta.0000057962.07187.56. [DOI] [PubMed] [Google Scholar]
- 6.Dissanaike S, Frezza EE. Laparoscopic splenectomy in blunt trauma. JSLS. 2006;10:499–503. [PMC free article] [PubMed] [Google Scholar]
- 7.Dalvi AN, Thapar PM, Deshpande AA, Rege SA, Prabhu RY, Supe AN, et al. Laparoscopic splenectomy using conventional instruments. J Minim Access Surg. 2005;1:63–9. doi: 10.4103/0972-9941.16529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orloff MJ, Peskin GW. Spontaneous rupture of the normal spleen; a surgical enigma. Int Abstr Surg. 1958;106:1–11. [PubMed] [Google Scholar]
- 9.Crate ID, Payne MJ. Is the diagnosis of spontaneous rupture of a normal spleen valid? J R Army Med Corps. 1991;137:50–1. doi: 10.1136/jramc-137-01-12. [DOI] [PubMed] [Google Scholar]
- 10.Habermalz B, Sauerland S, Decker G, Delaitre B, Gigot JF, Leandros E, et al. Laparoscopic splenectomy: The clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) Surg Endosc. 2008;22:821–48. doi: 10.1007/s00464-007-9735-5. [DOI] [PubMed] [Google Scholar]


