Abstract
Background/Objectives
Older adults commonly face difficult decisions regarding invasive medical treatments near the end of life, including surgical procedures. There is a need for interventions that help physicians, patients and caregivers deliberate about these difficult decisions and make informed choices that reflect patients’ values and goals.
Design
We designed a communication tool called “Best Case/Worst Case” (BC/WC) based on an established conceptual model of shared decision making. We evaluated the tool with focus groups of seniors (4 groups) and surgeons (2 groups) using modified questions from the Decision Aid Acceptability Scale and the Decisional Conflict Scale.
Setting and Participants
We recruited 37 adults over age 60 from senior centers and 17 surgeons from academic and private practices in Wisconsin to participate in the study.
Measurements
We used qualitative content analysis to explore themes and concepts identified by focus group respondents.
Results
Seniors and surgeons praised the tool for the unambiguous illustration of multiple treatment options, and the clarity gained from presentation of an array of treatment outcomes. Participants noted that the tool provides both an opportunity for in-the-moment, preference-based deliberation about options and a platform for further discussion with other clinicians and loved ones. Seniors worried that the format of the tool was not universally accessible for patients with different educational backgrounds, while surgeons had concerns that the tool was vulnerable to physicians’ subjective biases.
Conclusion
The BC/WC tool is a novel decision support intervention that may help facilitate difficult decision making for older adults and their physicians when considering invasive, acute medical treatments such as surgery.
Keywords: shared decision making, communication tool, acute care surgery, palliative care
INTRODUCTION
Many older Americans receive invasive treatments at the end of life,1–3 despite evidence that high intensity treatment may not be driven by patient preferences4 and is frequently inconsistent with patients’ treatment goals.5 Thirty-two percent of Americans 65 and older have surgery during their last year of life3 and these patients are more likely to spend time in the ICU and have prolonged hospitalization. Thus, many older adults will face a difficult surgical decision as they approach the end of life, and a choice to have surgery can initiate a cascade of invasive medical treatments that may be inconsistent with their goals.
Surgeons traditionally rely on the process of informed consent to help patients make decisions about whether to have surgery. This process emphasizes the objective quantification and disclosure of risk6. As such, surgeons commonly present a list of individual, discrete complications6 such as kidney failure or heart attack, and often do not describe the consequences of surgery in a way that helps patients recognize broader outcomes that might impact quality of life, including use of additional treatments or predictable changes in functional status.7 Although decision aids have been shown to improve decision making for a range of preference-sensitive surgical decisions, for example the choice between mastectomy of breast conserving surgery,8 existing aids are limited to a narrow range of clinical scenarios for which they have been specifically designed. Moreover, most decision aids have been designed for elective, outpatient decisions,8 require access to scales and pre-designed graphics9 and are thus difficult to use for in-the-moment decision making.
Because surgeons are often consulted to consider acute, invasive procedures that may impact the quality of life of frail older patients, they need tools to help patients evaluate high-risk operations and make choices that better reflect patients’ preferences, values and goals. We sought to design and evaluate an intervention to improve surgeon-patient communication for older patients near the end of life. In this study, we use qualitative analysis of focus groups with older adults and surgeons to evaluate and refine a novel decision support intervention.
METHODS
Intervention design
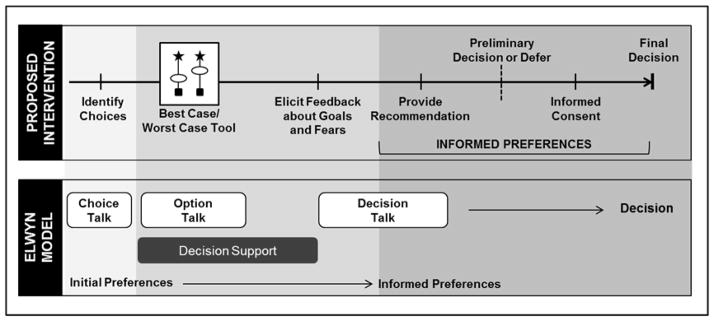
Our intervention (Figure 1) is designed to support in-the-moment decision making.10 It provides a framework to present options and express uncertainty to enable patients to express preferences for relevant outcomes. Building on the conceptual model proposed by Elwyn,11 we developed this tool to promote dialogue and deliberation in the context of life-threatening illness (Figure 2). The tool displays a confined range of possible outcomes, illustrates that some are more likely than others, and conveys a choice between two (or more) strategies. It uses narrative to explain the full treatment course, helping patients imagine downstream outcomes, including additional invasive treatments or changes in functional status.
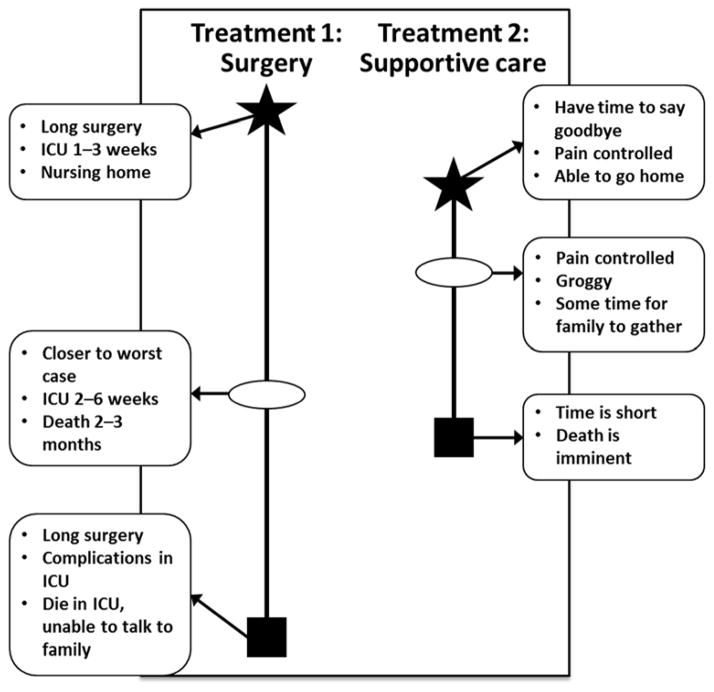
Figure 1.
The “best case/worst case” tool involves the drawing of a pen-and-paper diagram by the physician. Each treatment option is depicted by a vertical bar, and the length of the bar represents the range of possible outcomes. The “best case” is represented by a star, the “worst case” by a box, and the “most likely” outcome by an oval. The physician describes each “case” using narrative derived from clinical experience and relevant evidence, and writes key points on the diagram. Abbreviation: ICU, intensive care unit.
Figure 2.
A diagram of how the “best case/worst case” tool is used within in a complete clinical decision making process (top). The proposed use of “best case/worst case” builds on a conceptual model (bottom) described by Elwyn et al that promotes shared decision making and facilitates the development of informed preferences.12 The presentation of choices and options at the outset of the decision process using “best case/worst case” allows the patient to attach personal preferences to treatment options with the physician’s help, forming informed preferences.
This intervention, called “best case/worst case” (BC/WC), provides a structured framework that uses description and graphics to help patients organize information, visualize options and deliberate.12 It results in a diagram used by the surgeon, other physicians, patient and family as the basis for further dialogue (Figure 1). To start, the surgeon names each of the patient’s treatment options and describes, using his clinical judgment and best available evidence, the “best case” outcome, the “worst case” outcome, and what he believes is the “most likely” outcome for each treatment. “Most likely” is not a precise risk estimate; instead, it allows physicians and patients to begin to compare treatment options. The verbal description of each “case” incorporates rich narrative derived from clinical experience and relevant evidence, and focuses on the story of how the patient may experience an outcome, instead of quoting discrete statistical risks. In cases where accurate statistical data about outcomes and their relative frequencies exist, the physician can provide precise quantitative information after telling the story of each outcome. The surgeon simultaneously draws the pen-and-paper diagram, and under each treatment option he places a vertical bar. The bar length suggests a range of outcomes and the relative magnitude of difference between the “best case” (star), the “worst case” (box), and the physician’s estimate of the “most likely” (oval) outcome. After presenting the tool, the surgeon uses phrases to encourage deliberation13 such as, “what do you think about all of this?” to elicit the patient’s preferences and goals based on the outcomes described. The surgeon can then link these goals with the appropriate treatment choice (Figure 2).
Evaluation of Best Case/Worst Case
We conducted six professionally moderated, audio-recorded focus groups in Wisconsin. We held four focus groups of seniors (N = 37, Table 1), using purposive sampling of senior centers to capture study participants with a variety of socioeconomic backgrounds. We circulated an advertising flier at selected senior centers to recruit community-dwelling individuals who were English-speaking, 60 years of age or older and reported making a major medical decision for themselves or a family member in the last 10 years. We held two focus groups with surgeons (N = 17, Table 1) from private and academic medical practices in Wisconsin. The surgeons were recruited using snowball sampling and were sub-selected based on practice characteristics and clinical experience. The University of Wisconsin Social Sciences Institutional Review Board approved the study, and all individuals gave informed consent prior to participating and received cash honoraria upon completion.
Table 1.
Characteristics of Senior and Focus Group Respondents
| Seniors, n = 37 | |
|---|---|
| Age | n (%) |
| 60–69 | 15 (41) |
| 70–79 | 10 (27) |
| > 80 | 12 (32) |
| Gender | |
| Female | 27 (73) |
| Race/Ethnicity+ | |
| White | 26 (70) |
| Black or African American | 3 (8) |
| Hispanic | 5 (13) |
| Other | 1 (3) |
| Education+ | |
| Some high school or less | 1 (3) |
| High school diploma or General Educational Development (GED) | 10 (27) |
| Occasional college or some college | 9 (24) |
| College degree | 9 (24) |
| Professional or graduate degree | 6 (16) |
| Some high school or less | 1 (3) |
| Surgeons, n = 17 | |
| Gender | |
| Male | 14 (82) |
| Female | 3 (18) |
| Surgical Specialty++ | |
| General Surgery | 10 (59) |
| Vascular | 4 (24) |
| Cardiothoracic | 4 (24) |
| Neurosurgery | 2 (12) |
Two seniors chose not to reply
Several surgeons selected more than one specialty
Data Collection
Each focus group began with questions to elicit participants’ experience with serious medical decisions and the concept of tradeoffs. Next, participants were shown a video of a 79 year-old patient with multiple medical comorbidities and a tender thoracoabdominal aneurysm. The video depicts a vascular surgeon using the BC/WC tool to present a choice between surgery and supportive care (a transcript of the video content is available at http://links.lww.com/SLA?A699). Accuracy of the clinical data presented was confirmed independently by 2 vascular surgeons. Study participants were given a paper copy of the graphic diagram used in this discussion. The diagram was iteratively revised between the second and third focus group based on input from the first two groups. Following the video, focus group participants were asked questions from the Decision Aid Acceptability Scale14 and the Decisional Conflict Scale15, modified to be open-ended and balanced for the focus group format (the senior focus group guide is available at http://links.lww.com/SLA/A698). All participants completed a demographic exit survey, and seniors were asked about their preferences for decision-making.16
Analysis
Audio recordings of each focus group were transcribed verbatim into text for analysis, which was facilitated by the use of NVIVO 10 software (QSR International). Seven investigators from diverse professional backgrounds (JK- internal medicine, MN- general surgery, NS- public health, KB- trauma surgery, critical care and palliative care, MG-law, TC- palliative care and oncology, MS- vascular surgery) independently reviewed each transcript generating codes for sections of text to classify observations, concepts and themes. We performed higher-level conventional content analysis during meetings of at least three investigators through exploration of codes, themes and trends. Consensus codes were collated and the collection was revised and applied to subsequent transcripts in an iterative process. We determined that we reached theoretical saturation when concepts and themes became redundant with previous observations.
RESULTS
Seniors: Praise for Best Case/Worst Case
Seniors appreciated how the BC/WC tool frames difficult medical decisions (Table 2). They praised the clear presentation of two distinct treatment options and the explicit illustration of a choice. One senior said, “it helped me to visualize those two different paths when I looked at this, rather than just trying to keep those two words, surgery or not surgery in my head. […] I appreciated this visualization to help me understand the two choices because they’re two different choices, very different.” Furthermore, seniors endorsed the tool as a way for the surgeon to describe “both sides of the story” rather than promote a singular agenda. Seniors believed the tool had the flexibility to provide information that was individualized and they approved of the tool’s capacity to incorporate knowledge about the patient’s underlying health state.
Table 2.
Seniors’ Praise of the BC/WC Tool
| Establishes a choice | “I like the idea that he gave the two choices. This is what’s going to happen if you have the surgery. This is what’s going to happen if you choose not to have the surgery.” |
| Comprehensive Provides clarity | “I thought it was all quite clear. I would have understood and deduced everything needed from what he said.” |
| Can be individualized to the patient’s medical history | “this is fairly personalized to the condition she is in, regardless of her aneurysm, because of the fact that the doctor indicated she has a lot of other health issues. […] these notes would be completely different if it was somebody coming in at age 55 with a husband, cognizant, couple of kids.” |
| Attends to range of preferences | “I think it’s providing all the options for her. And she’s going to look at it different than the next person. So I think by providing it, the bare bones like this, the person, each person can decide on their own based on their, what they need or don’t need.” |
| Encourages deliberation | “And I’m going to sit there by myself and think what does this mean for my life? What does this mean? And you look at it. What does this mean for my life, daughter?” “Well, like I said before, if it were written down, she could study it for a little bit, and she could decide what’s important to her after reading what she would have to go through.” “the doctor would say to the person […] I want you to take this form and list all the questions you have that need to be answered […]. And so he goes away, and now she can spend time with her daughter or the rest of the family too, and come up with a lot of questions, which could be answered within a few hours.” |
Seniors noted the BC/WC framework could account for a range of patient preferences. One senior reflected, “the scenario leaves room for both kinds of personalities. The ones that are fight, fight, fight everything and ones who lived all their lives that way and they want to take their very last chance, they have that opportunity here. And then the people who have been thinking about death maybe a long time and maybe have been ill and have had, they have an opportunity here. So is seems to me that it covers nicely both kinds of people.” Focus group participants recognized the tool encourages patient deliberation by allowing patients to imagine how they would value the consequences of different future health states. One senior noted that the framework can, “help organize each thing and then she can decide what is more important to her based on a visual rather than trying to sort it all out in…her brain.”
Seniors felt the tangible pen-and-paper diagram could be left with the patient and would provide a platform to deliberate about the choice with family. Furthermore, the patient could use the diagram to discuss options with other clinicians involved in the decision making. The first two focus groups received a handout that had only lines and symbols, which the seniors felt was inadequate. We refined the handout for the second two focus groups, adding short descriptions of each case, which was highly praised in subsequent groups.
Seniors: Critique of Best Case/Worst Case
Seniors worried the diagram might not be universally accessible, suggesting that some may prefer an audio-recorded format, a video, a larger picture or a color diagram. One senior recognized that the pictorial representation of lines and symbols could be difficult to interpret for, “[…] people that have very, very low education skills or if it’s a different culture.” Seniors also expressed concern that the diagram could introduce bias if the patient assumed that the first treatment option presented is favored over the second.
Seniors desired additional information about how the consequences of surgery would be experienced by the patient. They wanted more detail about how surgery would affect the ability to walk, be with family, bathe and go to the bathroom independently. One senior asked, “in the best case of the surgery, am I going to be able, can you [en]vision me getting up and being able to walk again? Am I, do you think I’d be in a wheelchair the rest of, do you think I’m going to be in pain the rest of my life?” Others wanted more information about the surgical procedure, including information about the incision, duration of surgery, and technical description about how the surgery would be done. Seniors also felt the physician should acknowledge hope by describing a chance for miraculous recovery, and some felt the prognostic information was too blunt and wanted the physician to suppress and soften information about death and dying.
Surgeons: Praise for Best Case/Worst Case
Surgeons felt the tool could prompt a physician to discuss the most salient points for decision making and noted that the structure clearly demonstrates the existence of two legitimate treatment choices (Table 3). One surgeon said, “I think it also kind of explains that supportive care means she’s still going to get treatment, meaning she’s going to be kept comfortable and things like that. I think a lot of times patients and families have this idea that either we operate or we do nothing, and we just say, nothing to do here.” They felt the tool was valuable in its ability to communicate the limitations of surgical treatment. By presenting the “best case scenario”, some patients may recognize that even the best possible outcome from surgery was not aligned with their goals. For example, “that’s the piece of information that then helps you allow the patient to say, that’s not the choice that I should make because the best I can get is something that I don’t want.” Furthermore, surgeons endorsed the tool’s ability to establish the patient’s goals within a context of the patient’s overall health: “Then they can make their goals and then you can kind of tie it all in. But I don’t think you can just say, well, [what] are [your] goals, because they say my goal might be to go to Starbucks tomorrow or, you know, versus whatever else. So it’s, they have to kind of get it within the same context of what you’re dealing with.”
Table 3.
Surgeons’ Praise for the BC/WC Tool
| Establishes a choice | “I think what I saw is the tool is that you paint the two options, where they are, and you paint a best and worst scenario of those two options as best you can I think, you know, I think it’s true that we often don’t have that structure in a conversation with patients when they make decisions” |
| Provides structure for physician | “I mean, having a structured sort of overview of what you should try to present, and we can all present it in our own ways, I think makes a lot of sense.” |
| Shows range of possible outcomes | “And I think the diagram gives, in a sense, gives a range of the possible outcomes and the constraints. So, you know, not on this is you go back to your independent living. That’s not a possibility here. So it’s a way of framing what are the constraints of your future” |
| Tangible visual framework | “I think the tool gives a visual and it can help, for her, help organize each thing and then she can decide what is more important to her based on a visual rather than trying to sort it all out in the, her brain.” “if you have something that they can hold and write down, and maybe they can write in their own goal so they invest in the process rather than, you know, however you decide to do it.” |
| Durable, can be used for future reference | “So I think the second trip back. Okay, now that, you know, ten minutes ago we discussed this, do you have questions? What didn’t you understand, and is there stuff I can help sort out, you know? So that you sort of let them expand on what they heard and what they didn’t hear.” |
| Can be used for other decisions | “I would say that not only is this valuable in conversation before surgery. I’m often having this conversation with families after surgery because there was no one to make a decision, they were taken emergently to the operating room by default, and then this is the conversation that we’re having with a patient critically ill in the ICU with an open abdomen. “ |
Abbreviation: ICU, intensive care unit.
Surgeons approved of the visual aid for organizing information, because it could allow patients to participate more fully in the conversation. Furthermore, they saw the tool as an iterative way to transmit information, check for understanding and help patients remember more of the conversation. Surgeons thought it was valuable to leave the pen-and-paper diagram with patients and their families so they could digest the information and discuss it amongst themselves and with other clinicians. This would allow for a more productive conversation when the surgeon returned. Finally, they thought the tool would be useful for other types of decisions, including discussions about postoperative life supporting interventions.
Surgeons: Critique of Best Case/Worst Case
Surgeons voiced concerns that the tool both presents too much information and that several important details are missing, including information about the gravity of the procedure and quantitative information. Surgeons were unsure how to accurately position the “most likely” outcome on the graphic aid. They also thought the diagram might be too complex for some patients and noted that finding paper to create the graphic aid may be difficult given computer-based workflows.
Surgeons worried that the content of the tool was subjective. They recognized that the best, worst and most likely cases might vary by practitioner or be influenced by biases of the individual surgeon who had his own opinion about the value of surgery. As one surgeon said, “surgeons can be very aggressive in recommending surgery, or they could be conservative, or they could be in the middle. So again, that introduces an element of subjectivity.” Some thought the information was too blunt; the bad news was more than some patients and families could handle at once, and it didn’t leave open the possibility that the patient would do better than expected, “it caught me when he said, you will never go home again. I’m thinking, you never know. You know, there’s old people who will surprise you.”
Criticism of the video
Although focus group participants were told that the physician actor in the video was explicitly instructed to “speak plainly and without emotion” and that the tool was a small portion of a larger discussion, seniors and surgeons found the video presentation of the tool distracting because it lacked emotion, empathy and failed to present an active give-and-take conversation. One senior said, “I think if the emotion was different, if he showed more compassion, I think she might have been able to relax more and come up with questions. She would feel like she’s talking to a friend or someone she knows. […] So I think there’s a lot of things left open that she might have, or her daughter might have thought to ask if he had been more compassionate or more caring […].”
Biased or Neutral?
All participants were asked to respond individually to the question, “Do you think the surgeon in the video wanted [the patient] to choose one course of action over the other or do you think the surgeon was neutral about [her] choice?” Although all were shown the same video, surgeons and seniors perceived the presentation of options differently. Seniors were mixed about whether the surgeon favored surgery or palliative care and many felt that the surgeon was neutral about the options (15 thought the surgeon was neutral while 9 thought the surgeon favored surgery and 9 thought he favored palliative care, 5 were undecided/unclear). In contrast, the vast majority of surgeons believed the surgeon in the video favored palliative care (15 palliative care, 1 neutral, 1 undecided).
DISCUSSION
The purpose of this study was to evaluate and refine a novel decision support intervention, the “best case/worst case” communication tool. Seniors and surgeons noted several important benefits of using the BC/WC tool to help older patients with multiple comorbidities in the event of acute surgical illness. They praised the structure of this tool for its clarity in choice presentation, its demonstration of the limits of potential outcomes, and its ability to help patients make choices that are consistent with their values. Both groups felt the tool would facilitate deliberation with family and other clinicians and found the use of narrative to explain outcomes both relatable and flexible in its accounting for a variety of health states and preferences.
Some seniors wanted more information about technical aspects of surgery and description about quality of life while others felt the information presented was too explicit and lacked the chance for a miracle. Surgeons also worried the information might be too overwhelming for some patients and that the tool was vulnerable to the biases of the individual surgeon. After iterative revision of the graphic aid to include a brief written description of each “best”, “worst”, and “most likely” case, respondents in the remaining groups found it useful for organizing information for decision making. These findings are important because they suggest that the BC/WC tool may be used as an intervention to improve in-the-moment decision making about invasive procedures for older patients with multi-morbidity. Understanding seniors’ and surgeons’ reactions to a tool designed to improve shared decision making for older patients with an acute surgical illness has important implications for surgeons, patients and geriatricians.
For surgeons, use of BC/WC may prevent patients from over-attributing unspoken benefits to surgical treatments. Our surgeon participants noted that framing choices using BC/WC may help patients recognize the limitations of surgery. This finding is important, as standard disclosure of surgical risk does little to illuminate how patients may experience surgical survival; it is not surprising that frail older patients who are quoted 50% surgical mortality would assume they have a 50% chance of being exactly as they were before surgery. The surgical literature focuses much attention on precise risk prediction17–19 with little regard to how these risks are understood and used by patients to form expectations. Anthropologist Sharon Kaufman notes that patients and families do not need more information but rather more interpretation20 about how treatments impact outcomes within the context of the patient’s overall health. Using the BC/WC tool, surgeons can provide a more realistic and relatable description of potential surgical outcomes while communicating the boundaries of what is possible. This framing may help patients better formulate preferences for treatments based on clinically relevant expectations.
Our findings are also important for geriatricians, primary care physicians and other specialists who care for older adults. Without prompting, seniors suggested the graphic aid could be used as a platform to consider options with family and, if possible, their primary doctor. Because the tool is nimble and the diagram is constructed with simple pen and paper, the focus group participants valued the portability of the completed tool. Primary care providers and other specialists caring for older adults could use BC/WC with its graphic aid—both before and after surgical consultation—to inform patients about multiple treatment options, including palliative care, in order to help patients visualize and compare potential outcomes.
For patients, focus group participants appreciated how the framework of BC/WC can help organize complex information so patients can make decisions based on their personal preferences. This tool expands the medical context of the decision beyond a commonly portrayed, narrow construct of an isolated surgical problem that needs to be fixed.21–24 While seniors in our focus groups found the graphic aid particularly helpful for sorting this information, they raised an important consideration for patients with low health literacy. If the BC/WC tool is ultimately found effective for improving decision making for high-stakes surgical decisions, additional study will be required to examine its utility with different patient populations.
Unlike other decision aids designed for one decision and pre-populated with relevant statistical details, BC/WC relies on the physician to provide the clinical context and relevant evidence so that it can be flexible for complex decision making. Thus, as the respondents noted, the tool content is vulnerable to biases inherent in clinical judgment and sacrifices information standardization for flexibility and use in multiple settings. Furthermore, determining the position of the elements (star/box/oval) on the graphic aid could, in some settings, be challenging. This in an important issue for broader tool dissemination and will need careful attention during surgeon training for use of the tool to insure both accuracy and relevance to patients. Nonetheless, BC/WC contextualizes the decision in a way that attends to a wide array of in-the-moment clinical possibilities particularly common in older patients with multiple comorbidities.
Both seniors and surgeons were upset by the lack of emotion displayed in the focus group video. We purposely asked the actor (a palliative care physician) to avoid demonstrating empathy as we worried this would confound our ability to study the transmission of information with the tool. Instead, we learned that difficult decisions require more than simple provision of information and this cannot be isolated from its emotional context. This finding leads to the important conclusion that BC/WC, or similar tools, cannot be evaluated, disseminated, or taught without specific attention to the communication skills of the physician. Our study has several limitations. All focus groups took place in Wisconsin, a state with a national reputation for a high penetrance of advance care planning.25 Although we were able to enroll seniors with diverse educational and racial backgrounds, seniors and surgeons in other locales may have differing reactions to the BC/WC tool. Furthermore, given the time constraints of a 90 minute focus group we were unable to present more of the conversation between surgeon and patient which might have better illustrated how the BC/WC tool works within the overall decision making process. Finally, all senior participants were community dwelling, and the tool might prompt different reactions in people who are hospitalized with acute illnesses.
CONCLUSIONS
Our novel, adaptable communication tool is designed for in-the-moment difficult treatment decisions for frail older patients, including decisions about acute surgical intervention. Our tool may help patients understand options, compare and ask questions about relevant outcomes, and formulate value-sensitive treatment preferences. Further study is required to determine whether the BC/WC tool can effectively improve clinical decision making and align treatment choices with patient goals.
Acknowledgments
Financial Support: Dr. Schwarze is supported by a training award (KL2TR000428) from the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant (UL1 TR000427) and the Greenwall Foundation (Greenwall Faculty Scholars Program.) The project described was also supported by the National Institute for Minority Health and Health Disparities Center of Excellence program, through the UW Collaborative Center for Health Equity (CCHE) grant (5P60MD003428.) These funding sources had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; and preparation, review, or approval of the manuscript for publication. No other financial support was declared for the remaining authors.
The authors would like to thank Ken Croes, PhD from the UW Survey Center for his moderation of the focus groups, Layton “Bing” Rikkers, MD, the Collaborative Center for Health Equity (ICTR CCHE), and the Community-Academic Aging Research Network (CAARN) for their help with focus group participant recruitment, the Qualitative Research Group (ICTR QRG) and Nora Jacobson for assistance with study design and presentation of results and Bob Arnold, MD for his comments on an earlier version of this manuscript.
Sponsor’s Role: Dr. Schwarze is supported by a training award (KL2TR000428) from the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant (UL1 TR000427) and the Greenwall Foundation (Greenwall Faculty Scholars Program.) The project described was also supported by the National Institute for Minority Health and Health Disparities Center of Excellence program, through the UW Collaborative Center for Health Equity (CCHE) grant (5P60MD003428.) These funding sources had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; and preparation, review, or approval of the manuscript for publication. No other financial support was declared for the remaining authors.
Footnotes
Reprints will not be available from the authors.
| Elements of Financial/Personal Conflicts | J Kruser | M Nabozny | N Steffens | K Brasel | T Campbell | M Gaines | M Schwarze | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | X | X | X | X | X | |||||||
| Grants/Funds | X | X | X | X | X | X | X | |||||||
| Honoraria | X | X | X | X | X | X | X | |||||||
| Speaker Forum | X | X | X | X | X | X | X | |||||||
| Consultant | X | X | X | X | X | X | X | |||||||
| Stocks | X | X | X | X | X | X | X | |||||||
| Royalties | X | X | X | X | X | X | X | |||||||
| Expert Testimony | X | X | X | X | X | X | X | |||||||
| Board Member | X | X | X | X | X | X | X | |||||||
| Patents | X | X | X | X | X | X | X | |||||||
| Personal Relationship | X | X | X | X | X | X | X | |||||||
*Authors can be listed by abbreviations of their names.
For “yes” x mark(s): give brief explanation below:
Author Contributions: All authors listed have contributed sufficiently to the project to be included as authors. All authors meet the criteria for authorship stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals
References
- 1.Riley GF, Lubitz JD. Long-Term Trends in Medicare Payments in the Last Year of Life. Health Serv Res. 2010;45:565–76. doi: 10.1111/j.1475-6773.2010.01082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Teno JM, Gozalo PL, Bynum JPW, et al. Change in End-of-Life Care for Medicare Beneficiaries: Site of Death, Place of Care, and Health Care Transitions in 2000, 2005, and 2009. JAMA. 2013;309:470–7. doi: 10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwok AC, Semel ME, Lipsitz SR, et al. The intensity and variation of surgical care at the end of life: a retrospective cohort study. Lancet. 2011;378:1408–13. doi: 10.1016/S0140-6736(11)61268-3. [DOI] [PubMed] [Google Scholar]
- 4.Barnato AE, Herndon MB, Anthony DL, et al. Are Regional Variations in End-of-Life Care Intensity Explained by Patient Preferences? Med Care. 2007;45:386–93. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teno JM, Fisher ES, Hamel MB, et al. Medical care inconsistent with patients’ treatment goals: association with 1-year Medicare resource use and survival. J Am Geriatr Soc. 2002;50:496–500. doi: 10.1046/j.1532-5415.2002.50116.x. [DOI] [PubMed] [Google Scholar]
- 6.Neuman M, Bosk C. What We Talk about When We Talk about Risk: Refining Surgery’s Hazards in Medical Thought. Milbank Q. 2012;90:135–59. doi: 10.1111/j.1468-0009.2011.00657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pecanac KE, Kehler JM, Brasel KJ, et al. It’s big surgery: preoperative expressions of risk, responsibility, and commitment to treatment after high-risk operations. Ann Surg. 2014;259:458–63. doi: 10.1097/SLA.0000000000000314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stacey D, Legare F, Col NF, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2014;10 doi: 10.1002/14651858.CD001431.pub4. [DOI] [PubMed] [Google Scholar]
- 9.Weymiller AJ, Montori VM, Jones LA, et al. Helping patients with Type 2 Diabetes Mellitus make treatment decisions: Statin choice randomized trial. Arch Int Med. 2007;167:1076–1082. doi: 10.1001/archinte.167.10.1076. [DOI] [PubMed] [Google Scholar]
- 10.Schwarze ML, Kehler JM, Campbell TC. Navigating High Risk Procedures with More Than Just a Street Map. J Palliat Med. 2013;10:1169–71. doi: 10.1089/jpm.2013.0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elwyn G, Frosch D, Volandes AE, et al. Investing in deliberation: a definition and classification of decision support interventions for people facing difficult health decisions. Med Decis Making. 2010;30:701–11. doi: 10.1177/0272989X10386231. [DOI] [PubMed] [Google Scholar]
- 12.Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–7. doi: 10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stiggelbout AM, Weijden TVD, De Wit MPTD, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ. 2012;344:e256. doi: 10.1136/bmj.e256. [DOI] [PubMed] [Google Scholar]
- 14.O’Connor A, Cranney A. [Accessed July 7, 2013];User Manual - Acceptability [document on the Internet] 1996 Available at: http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Acceptability.pdf.
- 15.O’Connor AM. [Accessed January 23, 2014];Decisional Conflict Scale. 1993 [updated 2005]. Available at: www.ohri.ca/decisionaid.
- 16.Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Can J Nurs Res. 1997;29:21–43. [PubMed] [Google Scholar]
- 17.Robinson TN, Wu DS, Sauaia A, et al. Slower Walking Speed Forecasts Increased Postoperative Morbidity and 1-Year Mortality across Surgical Specialties. Ann Surg. 2013;258:582–590. doi: 10.1097/SLA.0b013e3182a4e96c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Osnabrugge RLJ, Speir AM, Head SJ, et al. Costs for Surgical Aortic Valve Replacement According to Preoperative Risk Categories. Ann Thorac Surg. 2013;96:500–506. doi: 10.1016/j.athoracsur.2013.04.038. [DOI] [PubMed] [Google Scholar]
- 19.Powell HA, Tata LJ, Baldwin DR, et al. Early mortality after surgical resection for lung cancer: an analysis of the English National Lung cancer audit. Thorax. 2013;68:826–834. doi: 10.1136/thoraxjnl-2012-203123. [DOI] [PubMed] [Google Scholar]
- 20.Russ AJ, Kaufman SR. Family perceptions of prognosis, silence, and the “suddenness” of death. Cult Med Psychiatry. 2005;29:103–123. doi: 10.1007/s11013-005-4625-6. [DOI] [PubMed] [Google Scholar]
- 21.Towle A, Godolphin W, Grams G, et al. Putting informed and shared decision making into practice. Health Expect. 2006;9:321–32. doi: 10.1111/j.1369-7625.2006.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lynn J, DeGrazia D. An outcomes model of medical decision making. Theor Med. 1991;12:325–43. doi: 10.1007/BF00489892. [DOI] [PubMed] [Google Scholar]
- 23.Kruser JM, Pecanac KE, Brasel KJ, et al. “And I Think That We Can Fix It” Mental Models Used in High-Risk Surgical Decision Making. Ann Surg. 2014 doi: 10.1097/SLA.0000000000000714. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neuman M. Surgeons’ decisions and the financial and human costs of medical care. N Engl J Med. 2010;363:2382–3. doi: 10.1056/NEJMp1009621. [DOI] [PubMed] [Google Scholar]
- 25.Hammes BJ, Rooney BL, Gundrum JD. A Comparative, Retrospective, Observational Study of the Prevalence, Availability, and Specificity of Advance Care Plans in a County that Implemented an Advance Care Planning Microsystem. J Am Geriatr Soc. 2010;58:1249–55. doi: 10.1111/j.1532-5415.2010.02956.x. [DOI] [PubMed] [Google Scholar]