Abstract
Background
In 2010, Mexico was the most common (22.9%) country of origin for foreign-born persons with tuberculosis in the United States, and overall trends in tuberculosis morbidity are substantially influenced by the Mexico-born population.
Objectives
To determine the risk of tuberculosis disease among Mexico-born persons living in the United States.
Methods
Using data from the U.S. National Tuberculosis Surveillance System and the American Community Survey, we examined tuberculosis case counts and case rates stratified by years since entry into the United States and geographic proximity to the United States–Mexico border. We calculated trends in case rates over time measured by average annual percent change.
Results
The total tuberculosis case count (−14.5%) and annual tuberculosis case rate (average annual percent change −5.1%) declined among Mexico-born persons. Among those diagnosed with tuberculosis less than 1 year since entry into the United States (newly arrived persons), there was a decrease in tuberculosis cases (−60.4%), no change in tuberculosis case rate (average annual percent change of 0.0%), and a decrease in population (−60.7%). Among those living in the United States for more than 5 years (non-recently arrived persons), there was an increase in tuberculosis cases (+3.4%), a decrease in tuberculosis case rate (average annual percent change of −4.9%), and an increase in population (+62.7%). In 2010, 66.7% of Mexico-born cases were among non–recently arrived persons, compared with 51.1% in 2000. Although border states reported the highest proportions (>15%) of tuberculosis cases that were Mexico-born, the highest Mexico-born–specific tuberculosis case rates (>20/100,000 population) were in states in the eastern and southeastern regions of the United States.
Conclusions
The decline in tuberculosis morbidity among Mexico-born persons may be attributed to fewer newly arrived persons from Mexico and lower tuberculosis case rates among non–recently arrived Mexico-born persons. The extent of the decline was dampened by an unchanged tuberculosis case rate among newly arrived persons from Mexico and a large increase in the non–recently arrived Mexico-born population. If current trends continue, tuberculosis morbidity among Mexico-born persons will be increasingly driven by those who have been living in the United States for more than 5 years.
Keywords: tuberculosis, emigration, immigration, Hispanic Americans, Mexican Americans
Every year since 2004, over 50% of reported tuberculosis cases in the United States occurred among foreign-born persons (1). Mexico was the most common (22.9%) reported country of origin for foreign-born persons with tuberculosis in 2010 (2). An estimated 12 million Mexico-born persons lived in the United States in 2010, composing 28.2% of the foreign-born population (3).
Previous studies have characterized the challenges of tuberculosis prevention and care among Mexico-born persons, including repatriation before treatment completion (4) and barriers to accessing care associated with immigration status (5, 6). During 1993–2001, tuberculosis among Mexico-born persons in the United States occurred primarily in states along the United States–Mexico border, and approximately one-quarter of tuberculosis cases in border states occurred among Mexico-born persons (7). As a result, U.S. tuberculosis control policy surrounding Mexico-born persons has focused on interventions along the border between the United States and Mexico (8).
Beginning in 2007, the United States implemented enhanced preimmigration screening for tuberculosis disease among applicants for immigration from Mexico (and other countries) before arrival in the United States (9). In addition, U.S. tuberculosis control efforts extend beyond screening of immigrant applicants for disease; preventing tuberculosis in foreign-born persons with latent tuberculosis infection (through targeted testing and treatment) has become a high priority (10), given that three-quarters of all tuberculosis cases in foreign-born persons are thought to be from reactivation of latent tuberculosis infection (11). The potential impact of different targeted testing strategies among foreign-born persons has been debated extensively (10, 12–19), but an evidence-based approach specific to Mexico-born persons has not been previously studied. Some data included in this article have been presented previously in abstract form (20).
Methods
Study Population
Using data from the U.S. National Tuberculosis Surveillance System (2) and the U.S. National Tuberculosis Genotyping Service (21), we examined all verified cases of tuberculosis reported during 2000–2010. Cases were classified into three groups based on the reported country of birth: Mexico-born, United States-born (U.S.-born), and foreign-born from countries other than Mexico (foreign-born other). Cases missing data on country of birth or born as U.S. citizens outside of the United States were excluded from the analysis.
Data Analysis
Population estimates were derived from 1-year estimates from the American Community Survey, an ongoing statistical survey that samples approximately 1.9 million households over the course of each year (22). Persons are included in this survey regardless of immigration status. Population estimates are subdivided into public use microdata areas, which each contain a population of approximately 100,000 individuals. Tuberculosis case rates were calculated as the number of cases per 100,000 persons for each subpopulation. For example, the tuberculosis case rate among Mexico-born persons for each year was calculated using the number of tuberculosis cases among Mexico-born persons reported during that year and the estimated population of Mexico-born persons living in the United States during that same year. The 5- and 10-year case rates were calculated using aggregate case counts and aggregate population estimates for each time period.
We compared select demographic and clinical characteristics between U.S.-born, Mexico-born, and foreign-born other tuberculosis cases. The chi-square test was used to detect differences in proportions of individuals. We also examined tuberculosis case rates stratified by geographic proximity to the United States–Mexico border. Border states were defined as those that border with Mexico (i.e., California, Texas, New Mexico, and Arizona). Border areas were defined as public use microdata areas directly bordering Mexico and have been described elsewhere (23).
Joinpoint Regressional Software, version 3.5.2 (National Cancer Institute, Bethesda, MD), was used to calculate the average annual percent change of population estimates and tuberculosis case rates over the period of study (24). Standard errors for the population estimates and case rates were calculated using design factors (2000–2004) or replicate weights (2005–2010) per recommendations of the U.S. Census Bureau (22). In Joinpoint, P values for regression lines are calculated using a t test; if the P value was less than 0.05, then the slope was considered to be significantly different than zero.
The methods used to calculate tuberculosis case rates stratified by years since entry into the United States are described elsewhere (13). We stratified Mexico-born persons into three groups based upon years since U.S. entry: newly arrived (tuberculosis diagnosis <1 yr since U.S. entry), recently arrived (1–5 yr since U.S. entry), and non–recently arrived (>5 yr since U.S. entry). Mycobacterium bovis was identified using genotyping results of routinely collected isolates from reported tuberculosis cases (21, 25).
Aside from average annual percent change calculations, analyses were conducted using SAS, version 9.3 (SAS Institute, Cary, NC), and, for all statistical tests, results were considered to be significant if P was less than 0.05.
Ethical Review
Data for the U.S. National Tuberculosis Surveillance System and National Tuberculosis Genotyping Service are collected as part of routine public health practice, and therefore this project was determined not to be human subject research requiring institutional review board approval.
Results
Tuberculosis Case Counts and Case Rates
During 2000–2010, there were 153,353 cases of tuberculosis reported in the United States; 539 cases with no reported information on birth country or born as U.S. citizens outside the United States were excluded from further analysis. The remaining 152,814 cases included 69,189 (45.3%) among U.S.-born persons, 20,254 (13.3%) among Mexico-born persons, and 63,371 (41.5%) among foreign-born other persons.
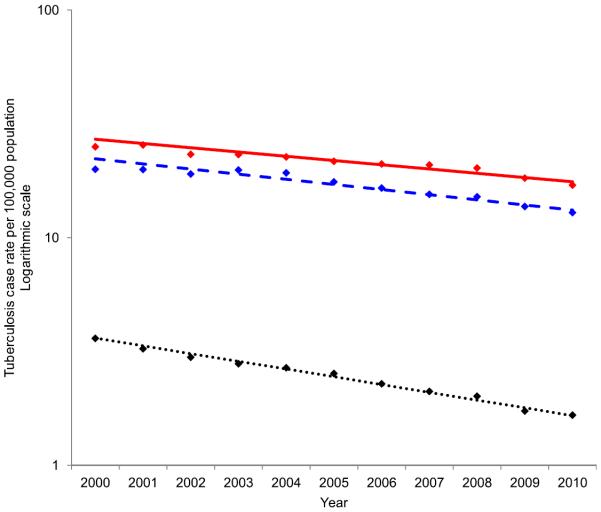
The number of tuberculosis cases among Mexico-born persons declined 14.5%, from 1,802 cases in 2000 to 1,541 cases in 2010, whereas tuberculosis among foreign-born other persons declined 11.0%. The overall tuberculosis case rate for the 10-year period was higher among the foreign-born other population (21.5/100,000 population) compared with the Mexico-born population (17.0/100,000 population). Annual tuberculosis case rates declined among both groups, with an average annual percent change of −4.2% among foreign-born other and −5.1% among Mexico-born persons (Figure 1).
Figure 1.
Annual tuberculosis case rate by origin, United States, 2000–2010. Solid line (red), annual tuberculosis case rate among foreign-born persons from countries other than Mexico (foreign-born other); dashed line (blue), annual tuberculosis case rate among Mexico-born persons; dotted line (black), annual tuberculosis case rate among U.S.-born persons.
Clinical and Demographic Characteristics
During 2000–2010, Mexico-born persons with tuberculosis were more frequently sputum smear–positive (54.1%) than foreign-born other (42.9%) and U.S.-born (45.0%) persons, and more frequently presented with cavitary disease (32.8 vs. 24.3 vs. 29.4%, respectively) (Table 1). Mexico-born persons had the lowest treatment completion rate (87.1 vs. 91.6 vs. 93.6%), and represented the highest proportion of persons with tuberculosis who moved or were lost to follow up (9.9 vs. 5.9 vs. 3.3%).
Table 1.
Select demographic and clinical characteristics of persons with tuberculosis by origin, United States, 2000–2010 (n = 152,814)*
| Characteristics | Mexico-Born (n = 20,254) n (%) | Foreign-Born Other (n = 63,371) n (%) | P Value† | U.S.-Born (n = 69,189) n (%) | P Value‡ |
|---|---|---|---|---|---|
| Any substance abuse | |||||
| Yes | 3,455 (17.1) | 3,345 (5.3) | <0.0001 | 17,916 (25.9) | <0.0001 |
| No | 16,006 (79.0) | 58,211 (91.9) | 48,389 (69.9) | ||
| Unknown | 793 (3.9) | 1,815 (2.9) | 2,884 (4.2) | ||
| Homelessness | |||||
| Yes | 1,014 (5.0) | 1,144 (1.8) | <0.0001 | 6,693 (9.7) | <0.0001 |
| No | 18,938 (93.5) | 61,409 (96.9) | 61,695 (89.2) | ||
| Unknown | 302 (1.5) | 818 (1.3) | 801 (1.2) | ||
| Correctional institution residence | |||||
| Yes | 1,326 (6.6) | 935 (1.5) | <0.0001 | 3,214 (4.7) | <0.0001 |
| No | 18,900 (93.3) | 62,267 (98.3) | 65,818 (95.1) | ||
| Unknown | 28 (0.1) | 169 (0.3) | 157 (0.2) | ||
| Disease site | |||||
| Pulmonary only | 14,462 (71.4) | 42,291 (66.7) | <0.0001 | 51,200 (74.0) | <0.0001 |
| Extrapulmonary only | 3,789 (18.7) | 15,723 (24.8) | 11,973 (17.3) | ||
| Both | 1,988 (9.8) | 5,307 (8.4) | 5,952 (8.6) | ||
| Unknown | 15 (0.1) | 50 (0.1) | 64 (0.1) | ||
| Chest radiograph results (n = 121,200)§ | |||||
| Cavitary | 5,393 (32.8) | 11,547 (24.3) | <0.0001 | 16,793 (29.4) | <0.0001 |
| Noncavitary | 10,757 (65.4) | 35,289 (74.1) | 39,064 (68.4) | ||
| Unknown/not done | 300 (1.8) | 762 (1.6) | 1,295 (2.3) | ||
| Sputum smear result (n = 121,200)§ | |||||
| Positive | 8,894 (54.1) | 20,438 (42.9) | <0.0001 | 25,719(45.0) | <0.0001 |
| Negative | 6,436 (39.1) | 23,308 (49.0) | 21,451 (37.5) | ||
| Unknown/not done | 1,120 (6.8) | 3,852 (8.1) | 9,982(17.5) | ||
| HIV status (n = 121,110)∥ | |||||
| Positive | 835 (6.6) | 3,185 (6.8) | <0.0001 | 7,001 (11.4) | <0.0001 |
| Negative | 9,201 (72.7) | 30,932 (65.9) | 36,237 (58.9) | ||
| Unknown/not done | 2,615 (20.7) | 12,816 (27.3) | 18,288 (29.7) | ||
| Previous tuberculosis | |||||
| Yes | 800 (4.0) | 3,359 (5.3) | <0.0001 | 3,296 (4.8) | <0.0001 |
| No | 19,270 (95.1) | 59,398 (93.7) | 65,345 (94.4) | ||
| Unknown | 184 (0.9) | 614 (1.0) | 548 (0.8) | ||
| Drug resistance | |||||
| Isoniazid-monoresistant¶ | 1,047 (5.2) | 4,715 (7.4) | <0.0001 | 2,111 (3.1) | <0.0001 |
| Multidrug-resistant** | 216 (1.1) | 887 (1.4) | 294 (0.4) | ||
| Other first line resistance | 118 (0.6) | 270 (0.4) | 298 (0.4) | ||
| Pyrazinamide-monoresistant†† | 823 (4.1) | 466 (0.7) | 552 (0.8) | ||
| Susceptible | 13,375 (66.0) | 42,936 (67.7) | 48,154 (69.6) | ||
| Unknown/not done | 4,675 (23.1) | 14,097 (22.3) | 17,780 (25.7) | ||
| Outcome (n = 118,381)‡‡ | |||||
| Completed therapy | 13,969 (87.1) | 45,862 (91.6) | <0.0001 | 48,954 (93.6) | <0.0001 |
| Moved/lost to follow-up | 1,593 (9.9) | 2,926 (5.9) | 1,707 (3.3) | ||
| Other/unknown | 473 (3.0) | 1,256 (2.5) | 1,647 (3.2) |
Foreign-born other indicates foreign-born from countries other than Mexico.
Excluding 539 cases with no reported information on birth country or born as U.S. citizens outside of the United States.
For Chi-square comparison between Mexico-born and foreign-born other.
For Chi-square comparison between Mexico-born and U.S.-born.
Among cases with pulmonary tuberculosis.
Excluding cases reported in California.
Isoniazid-monoresistant was defined as resistance to isoniazid, but susceptible to rifampin.
Multidrug-resistant was defined as resistance to at least isoniazid and rifampin.
Among cases with pyrazinamide-rnonoresistance and known genotyping results (2005–2010), 56.7% of isolates were Mycobacterium bovis (89.5% among Mexico-born, 12.2% among foreign-born other, and 51.8% among U.S.-born).
Data not available for cases reported in 2009 or 2010; does not include patients who died.
Among Mexico-born persons, 5.2% had isoniazid-monoresistant tuberculosis (resistant to isoniazid, but susceptible to rifampin) and 1.1% had multidrug-resistant tuberculosis (resistant to at least isoniazid and rifampin), lower than foreign-born other persons (7.4 and 1.4%), but greater than U.S.-born persons (3.1 and 0.4%). However, 4.1% of Mexico-born persons had pyrazinamide-monoresistant tuberculosis, compared with 0.7% among foreign-born other persons and 0.8% among U.S.-born persons. Among all cases with pyrazinamide-monoresistance and known genotyping results (2005–2010), 56.7% of isolates were M. bovis (89.5% among Mexico-born, 12.2% among foreign-born other, and 51.8% among U.S.-born persons).
Among Mexico-born persons with tuberculosis, 6.6% were incarcerated at diagnosis, a proportion higher than foreign-born other (1.5%) and U.S.-born (4.7%) persons. In 2010 only, 121 (9.7%) Mexico-born persons with tuberculosis were incarcerated at the time of diagnosis, (the highest percentage among any group during the period of study), with 33.1% diagnosed in jail, 24.1% in a state or federal prison, and 42.8% in “other” locations, including U.S. Immigration and Customs Enforcement facilities. Among Mexico-born persons who were incarcerated at tuberculosis diagnosis, approximately half (49.9%) completed treatment, lower than completion rates among foreign-born other (63.7%) and U.S.-born (83.5%) persons incarcerated at diagnosis.
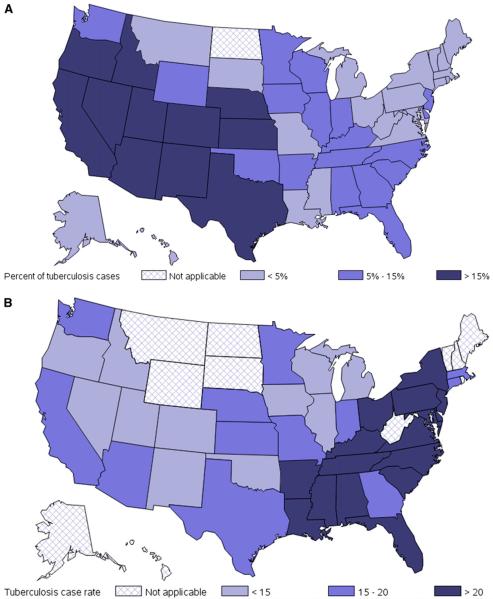
Proximity to the United States–Mexico Border
Western and southwestern states reported the highest proportions (>15%) of tuberculosis cases that were Mexico-born (Figure 2A). However, the highest Mexico-born–specific tuberculosis case rates (>20/100,000 population) were reported in states in the eastern and southeastern regions of the United States (Figure 2B).
Figure 2.
(A) Percent of tuberculosis cases born in Mexico, by state, United States, 2000–2010. Darkness of shading corresponds to the proportion of tuberculosis cases that occurred among Mexico-born persons. Dark blue–shaded states reported over 15% of tuberculosis cases among Mexico-born persons; medium blue–shaded states reported 5–15% of tuberculosis cases among Mexico-born persons; and light blue–shaded states reported less than 5% of tuberculosis cases among Mexico-born persons. States with cross-hatching reported insufficient numbers of cases among Mexico-born persons to report a proportion. (B) Tuberculosis case rates (per 100,000) among Mexico-born persons, by state, United States, 2000–2010. Darkness of shading corresponds to tuberculosis case rate among Mexico-born persons. Dark blue–shaded states had tuberculosis case rates of over 20 per 100,000 among Mexico-born persons; medium blue–shaded states had tuberculosis case rates between 15 and 20 per 100,000 among Mexico-born persons; and light blue–shaded states had tuberculosis case rates under 15 per 100,000 among Mexico-born persons. States with cross-hatching reported insufficient numbers of cases among Mexico-born persons to report a tuberculosis case rate.
Meanwhile, in border areas, all adult groups had higher tuberculosis case rates when compared with nonborder states (Table 2), with the greatest relative case rate increase among U.S.-born Hispanic adults (+95.9%), followed by foreign-born other (+77.7%), Mexico-born (+68.0%), and U.S.-born non-Hispanic adults (+17.7%). Both U.S.-born Hispanic and Mexico-born children in border areas had higher case rates (+72.9 and +60.9%, respectively) when compared with those populations in nonborder states.
Table 2.
Tuberculosis case counts and tuberculosis case rates by age group, origin, ethnicity, and proximity to the United States–Mexico border, 2005–2010*
| Nonborder States n (Rate) | Border States† |
||||
|---|---|---|---|---|---|
| Nonborder Areas |
Border Areas‡ |
||||
| n (Rate) | % Difference in Rate§ | n (Rate) | % Difference in Rate∥ | ||
| Children (<15 yr) | |||||
| Foreign-born other | 717 (9.4) | 150 (7.1) | −24.6 | 12 (6.9) | −27.2 |
| Mexico-born | 103 (5.5) | 121 (5.0) | −10.0 | 36 (8.9) | +60.9 |
| U.S.-born Hispanic | 812 (2.5) | 656 (1.9) | −25.3 | 256 (4.3) | +72.9 |
| U.S.-born non-Hispanic | 1,273 (0.5) | 343 (0.8) | +48.4 | 10 (0.3) | −36.6 |
| Adults (⩾15 yr) | |||||
| Foreign-born other | 22,025 (19.0) | 10,075 (23.6) | +24.6 | 879 (33.7) | +77.7 |
| Mexico-born | 3,818 (16.8) | 4,826 (13.2) | −21.0 | 1,734 (28.2) | +68.0 |
| U.S.-born Hispanic | 1,342 (4.0) | 1,668 (3.7) | −7.4 | 654 (7.9) | +95.9 |
| U.S.-born non-Hispanic | 19,568(2.1) | 4,944 (3.0) | +41.9 | 313 (2.4) | +17.7 |
Foreign-born other indicates foreign-born from countries other than Mexico.
Data for populations in border area public use microdata areas were not available before 2005.
States with a geopolitical border with Mexico (i.e., California, Texas, New Mexico, and Arizona).
Public use rnicrodata areas directly bordering Mexico.
Percent difference in tuberculosis case rate in nonborder areas of border states compared to nonborder states.
Percent difference in tuberculosis case rate in border areas of border states compared to nonborder states.
Years since Entry into the United States
Overall, newly arrived (<1 yr) foreign-born other persons had higher tuberculosis case rates when compared with newly arrived Mexico-born persons (112.4/100,000 population vs. 72.5/100,000 population; Figure 3). Although both groups experienced declines in case rate from 1 to 10 years after U.S. entry from 10 to 25 years there was a decreasing tuberculosis case rate among the foreign-born other population (from 19.5/100,000 population to 12.6/100,000 population), whereas the tuberculosis case rate among the Mexico-born population remained relatively constant (12.3/100,000 population to 12.5/100,000 population).
Figure 3.
Tuberculosis case rate among Mexico-born and foreign-born other persons, by years since entry into the United States, 2000–2010. Solid line (red), tuberculosis case rate among foreign-born persons from countries other than Mexico (foreign-born other); dashed line (blue), tuberculosis case rate among Mexico-born persons.
The difference between the two groups gradually diminished as years since U.S. entry increased. The tuberculosis case rate among the foreign-born other population further declined after 25 years, and reached a nadir of 5.8/100,000 population at 50 years since U.S. entry. The tuberculosis case rate among Mexico-born persons gradually increased from 25 to 50 years since U.S. entry, and reached 24.0/100,000 population after 50 years in the United States—4.1 times the case rate among foreign-born other persons for the same time since U.S. entry.
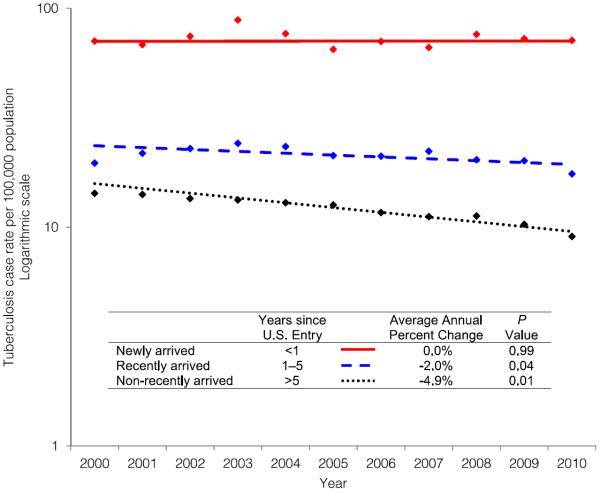
Trends in Tuberculosis Case Counts and Case Rates Stratified by Years since Entry into the United States
Comparing 2000 to 2010, the number of cases diagnosed among newly arrived (<1 yr) Mexico-born persons decreased by 60.4% (from 391 to 155 cases), and cases among recently arrived (1–5 yr) declined by 33.6% (from 452 to 300 cases). At the same time, the number of non-recently arrived (>5 yr) Mexico-born cases increased slightly, by 3.4% (from 880 to 910 cases).
Examining population trends alone, the estimate of non-recently arrived (>5 yr) Mexico-born persons increased 62.7%, from 6.2 million in 2000 to 10.0 million in 2010 (average annual percent change, +4.4%; P < 0.05). At the same time, the estimated population of recently arrived (1–5 yr) Mexico-born persons decreased 25.7%, from 2.3 million to 1.7 million (average annual percent change, −4.4%; P < 0.05), and the estimated population of newly arrived (<1 yr) Mexico-born persons decreased 60.7%, from 0.6 million to 0.2 million (average annual percent change, −9.3%; P < 0.05).
During the study period, the annual tuberculosis case rate among Mexico-born persons remained relatively constant among newly arrived persons (average annual percent change, 0.0%; P = 0.99), declined slightly among recently arrived persons (average annual percent change, −2.0%; P = 0.04), and experienced a significant decline among non-recently arrived (>5 yr) persons (average annual percent change, −4.9%; P < 0.01) (Figure 4).
Figure 4.
Annual tuberculosis case rates among Mexico-born persons by years since entry into the United States, 2000–2010. Solid line (red), tuberculosis case rate among newly arrived Mexico-born persons (<1 yr since U.S. entry); dashed line (blue), tuberculosis case rate among recently arrived Mexico-born persons (1–5 yr since U.S. entry), dotted line (black), tuberculosis case rate among non–recently arrived Mexico-born persons (> 5 yr since U.S. entry). If the P value is 0.05 or less, then slope is considered significantly different than zero.
Discussion
Several demographic and clinical characteristics distinguish Mexico-born persons with tuberculosis from those born in the United States and countries other than Mexico. High proportions of sputum smear–positive (54.1%) and cavitary disease (32.8%) among Mexico-born persons suggest greater severity of disease, potentially due to delayed diagnosis and initiation of treatment (26). Several factors may contribute to this phenomenon; a large number of Mexico-born persons living in the United States are undocumented (6.6 million in 2010) (27), and undocumented persons with tuberculosis may have poor access to care (5, 6, 28). In addition, compared with foreign-born persons from countries other than Mexico, Mexico-born persons tend to be less educated and less likely to be fluent in English (29), making medical services particularly difficult for this population to reach.
Among Mexico-born persons, we found high rates of incarceration at the time of diagnosis (9.7% in 2010) and low rates of reported treatment completion among those incarcerated (49.9%). The incarceration facility type for a large proportion (42.8%) of Mexico-born persons was categorized as “other,” including Immigration and Customs Enforcement facilities. The U.S. National Tuberculosis Surveillance System recently began recording information specifically regarding persons diagnosed in Immigration and Customs Enforcement custody; future analyses may help identify any potential association between incarceration facility type and rates of treatment completion.
High rates of incarceration, combined with low rates of treatment completion among incarcerated Mexico-born persons (49.9%), are concerning, as persons who fail to complete treatment are more likely to have recurrent disease (30). An unknown proportion of Mexico-born persons diagnosed with tuberculosis at the time of incarceration move back to Mexico (either by choice after release from custody, or by repatriation), and, therefore, definitive data on completion rates are unavailable at this time.
Although the largest proportion of Mexico-born tuberculosis cases are diagnosed in border states (Figure 2A), the highest Mexico-born–specific tuberculosis case rates are not found in border states, but rather states in the eastern and southeastern regions of the United States (Figure 2B). Given these findings, future tuberculosis prevention, diagnosis, and care activities aimed at Mexico-born persons should not focus on border states to the exclusion of nonborder states. Possible activities focused on these areas with high Mexico-born-specific tuberculosis case rates could include improving access to medical care for Mexico-born persons, providing culturally sensitive education regarding the signs and symptoms of tuberculosis disease to immigrant communities, encouraging local providers serving these communities to consider tuberculosis disease in Mexico-born persons with appropriate clinical presentations, and increasing routine targeted testing and treatment for latent tuberculosis infection.
Despite the lower tuberculosis case rates in border states compared with some nonborder states, tuberculosis cases rates were highest in border areas, with the largest relative case rate increase among the U.S.-born Hispanic population (Table 2). A recent analysis suggested that tuberculosis transmission commonly occurs among U.S.-born and Mexico-born persons, particularly along the United States–Mexico border (23). This phenomenon requires further study to explore the potential relationship between U.S.-born and Mexico-born cases along the border, such as transmission within families with Mexico-born adults and U.S.-born Hispanic children.
When examining tuberculosis case rates by years since U.S. entry we found that the case rate among newly (<1 yr) or recently arrived (1–5 yr) Mexico-born persons is more than twice that of nonrecent arrivers (>5 yr) (29.2/100,000 population vs. 12.0/100,000 population) (Figure 3). However, we also found that the tuberculosis case rate among Mexico-born persons who have been in the United States for more than 10 years remained elevated decades after U.S. entry, supporting recent studies demonstrating the persistent risk of reactivation among foreign-born persons with latent tuberculosis infection (14, 18). In addition, there is an increased tuberculosis case rate in Mexico-born persons in the United States for more than 25 years; the reasons for this delayed increase in rate among Mexico-born persons (but not among foreign-born other persons) are not clear, but this finding might be partly due to recent transmission via return visits to Mexico, exposure to cases with infectious tuberculosis visiting from outside the United States (e.g., friends or relatives), or a higher prevalence of medical conditions that increase the risk of progression from latent tuberculosis infection to tuberculosis disease.
During 2000–2010, the Mexico-born population experienced an overall 14.5% decline in tuberculosis case count. Stratified analysis by years since U.S. entry provides some insight into the driving forces behind the declining incidence of tuberculosis among Mexico-born persons. Specifically, the overall decline in tuberculosis morbidity among Mexico-born persons was not due to a change in tuberculosis case rate among newly arrived (<1 yr) persons, as this rate remained relatively constant during the study period. Rather, the change in trend may be attributed to changing demographics of the underlying population (i.e., fewer newly arrived persons), and lower tuberculosis rates among non–recently arrived (>5 yr) Mexico-born persons. At the same time, the extent of the decline was dampened by a large increase in the size of the non–recently arrived Mexico-born population.
These findings have important implications regarding the close relationship between population shifts and tuberculosis morbidity among Mexico-born persons living in the United States. As immigration from Mexico has declined, the proportion of Mexico-born cases that are newly arrived (<1 yr) has become a smaller fraction of all Mexico-born tuberculosis cases diagnosed in the United States (only 11.4% in 2010). Given this trend, public health authorities must be mindful not to devote resources solely focused on the newly arrived to the exclusion of Mexico-born persons that have been in the United States for longer periods of time, as this latter group has become the main driver of tuberculosis morbidity among the Mexico-born population. Moreover, these findings demonstrate how variable patterns of immigration among Mexico-born persons have impacted (and will likely continue to impact) tuberculosis morbidity, suggesting that years since U.S. entry may be an unreliable measure to guide tuberculosis prevention and control strategies.
The past several years have seen an emphasis on preimmigration screening as a mechanism to reduce the burden of tuberculosis among foreign-born persons living in the United States. Previous studies have demonstrated the effectiveness of this intervention for foreign-born persons from countries other than Mexico (18, 31, 32), and every case of tuberculosis diagnosed and treated overseas directly decreases tuberculosis morbidity in the United States. However, results of our analysis suggest that, among the Mexico-born population, preimmigration screening should not be the only strategy pursued.
First, the proportion of Mexico-born persons with tuberculosis who are diagnosed with tuberculosis within 1 year of arrival is decreasing every year, and this decline began before the new preimmigration screening instructions were implemented (22.7% in 2000 compared with 13.7% of all Mexico-born cases in 2007). Thus, strategies focusing on the newly arrived (<1 yr) are not sufficient to address the large contribution of reactivation tuberculosis to the total morbidity among Mexico-born persons.
Second, in contrast to other foreign-born populations, only a small proportion of Mexico-born persons (<3%) pass through preimmigration screening (33); instead, many enter the United States as a visitor, temporary resident, or without a visa altogether (34). A recent study in California found that, among Mexico-born persons undergoing preimmigration screening, only two cases were diagnosed within 6 months after arrival from October 2006 to September 2007 (before the new preimmigration screening instructions were implemented) (32). During the same time period, 52 cases were diagnosed within 6 months after arrival in California among Mexico-born persons without preimmigration screening (U.S. Centers for Disease Control and Prevention, National Tuberculosis Surveillance System, unpublished data). Thus, even if preimmigration screening were 100% sensitive, it would not address the large number of persons from Mexico who enter into the United States without screening.
Traditionally, targeted testing for latent tuberculosis infection has focused almost exclusively on persons who have newly (<1 yr) or recently (1–5 yr) arrived in the United States (12), due to elevated tuberculosis case rates among these populations (16, 35). Our findings support this approach—we found that the case rate among newly or recently arrived Mexico-born persons is more than twice that of nonrecent arrivers. A recent study concluded that elevated tuberculosis case rates among newly arrived persons might be primarily due to prevalent tuberculosis rather than a higher risk of reactivation (18). This finding further supports the focus of targeted testing on newly arrived Mexico-born persons, (most of whom have not passed through preimmigration screening), as targeted testing might also detect prevalent tuberculosis disease (36).
In addition to the traditional focus on newly (<1 yr) and recently (1–5 yr) arrived Mexico-born persons, our findings also support extending targeted testing and treatment to non–recently arrived (>5 yr) Mexico-born persons. Others have suggested that targeted testing of foreign-born persons, regardless of time living in the United States, could aid progress toward tuberculosis elimination (10, 15, 17, 18). Tuberculosis genotyping studies have estimated that only 25% of Mexico-born cases in the United States are due to recent transmission, meaning that the vast majority are likely due to reactivation of latent tuberculosis infection (11, 37).
However, addressing the burden of latent tuberculosis infection among this population can be daunting; an estimated 2.3 million Mexico-born persons living in the United States are latently infected with tuberculosis (38). Strategies such as targeted testing for latent tuberculosis infection among subgroups of non–recently arrived Mexico-born persons with higher risk for progression to tuberculosis disease (e.g., diabetes mellitus) might be more feasible and cost effective (10, 12, 39, 40). In addition, new tools against latent tuberculosis infection, including more specific diagnostics (36, 41) and shorter courses of therapy (42), could help alleviate the workload of treatment for this population.
Overall, the unique epidemiology and demographics of the Mexico-born population dictate a tailored approach to tuberculosis prevention and control. Most jurisdictions will continue to justly prioritize their resources on newly (<1 yr) and recently (1–5 yr) arrived Mexico-born persons. However, although this approach targets the Mexico-born population with the highest tuberculosis case rate and is cost effective (10), it does not address the large and growing pool of latent tuberculosis infection among non–recently arrived Mexico-born persons, and therefore will not be sufficient to achieve substantial future reductions in tuberculosis in this population. As a result, future trends in tuberculosis morbidity among Mexico-born persons will likely continue to be driven by the non–recently arrived population.
This study had several limitations. First, the foreign-born other population is not homogenous, and while useful as a referent to compare with the Mexico-born population, we are limited in our ability to interpret trends among the foreign-born population from countries other than Mexico. Second, persons from other Latin American countries may be misclassified as Mexico-born in the U.S. National Tuberculosis Surveillance System, particularly if they passed through Mexico en route to entering the United States. Third, reports of years since U.S. entry rely on self-report and can be complicated by multiple entries for a given individual. Fourth, American Community Survey population data are estimates, and not census counts of the population at risk; however, the U.S. Census does not record country of birth.
We found the overall decline in tuberculosis morbidity among Mexico-born persons may be attributed to two factors: (1) fewer newly arrived (<1 yr) persons; and (2) lower tuberculosis case rates among non–recently arrived (>5 yr) persons. At the same time, the extent of the decline was dampened by an unchanged tuberculosis case rate among newly arrived persons from Mexico and a large increase in the non–recently arrived Mexico-born population. If current trends continue, tuberculosis morbidity among Mexico-born persons will continue to be driven by the non–recently arrived population. To achieve substantial reductions in tuberculosis among Mexico-born persons living in the United States, more effective prevention and control measures (e.g., improved testing for and treatment of latent tuberculosis infection) are needed, particularly in those who have been living in the United States for more than 5 years.
Acknowledgment
The authors gratefully acknowledge the staffs of the U.S. National Tuberculosis Genotyping Service contract laboratories, local and state public health laboratories, and local and state health departments, which collected the data included in these analyses. They also acknowledge Steve Kammerer, Dr. Michael Chen, and Jim Tobias for their contributions to this work, and Dr. Tom Navin and Dr. Phil LoBue for their critical revision of the manuscript.
Supported by the Division of Tuberculosis Elimination, Centers for Disease Control and Prevention.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.CDC . Reported tuberculosis in the United States, 2011. U.S. Department of Health and Human Services, CDC; Atlanta: 2012. [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Trends in tuberculosis—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61:181–185. [PubMed] [Google Scholar]
- 3.US Census Bureau [accessed 2013 Jul 1];American Community Survey. Available from: http://www.census.gov/acs/www/
- 4.Schneider DL, Lobato MN. Tuberculosis control among people in U.S. Immigration and Customs Enforcement custody. Am J Prev Med. 2007;33:9–14. doi: 10.1016/j.amepre.2007.02.044. [DOI] [PubMed] [Google Scholar]
- 5.Asch S, Leake B, Gelberg L. Does fear of immigration authorities deter tuberculosis patients from seeking care? West J Med. 1994;161:373–376. [PMC free article] [PubMed] [Google Scholar]
- 6.Vargas Bustamante A, Fang H, Garza J, Carter-Pokras O, Wallace SP, Rizzo JA, Ortega AN. Variations in healthcare access and utilization among Mexican immigrants: the role of documentation status. J Immigr Minor Health. 2012;14:146–155. doi: 10.1007/s10903-010-9406-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schneider E, Laserson KF, Wells CD, Moore M. Tuberculosis along the United States–Mexico border, 1993–2001. Rev Panam Salud Publica. 2004;16:23–34. doi: 10.1590/s1020-49892004000700004. [DOI] [PubMed] [Google Scholar]
- 8.Tuberculosis Along the US-Mexico Border Work Group. Centers for Disease Control and Prevention Preventing and controlling tuberculosis along the U.S.–Mexico border. MMWR Recomm Rep. 2001;50:1–27. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevetion [accessed 2014 Apr 18];CDC immigration requirements: technical instructions for tuberculosis screening and treatment using cultures and directly observed therapy. 2009 Available from: http://www.cdc.gov/immigrantrefugeehealth/pdf/tuberculosis-ti-2009.pdf.
- 10.Linas BP, Wong AY, Freedberg KA, Horsburgh CR., Jr Priorities for screening and treatment of latent tuberculosis infection in the United States. Am J Respir Crit Care Med. 2011;184:590–601. doi: 10.1164/rccm.201101-0181OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ricks PM, Cain KP, Oeltmann JE, Kammerer JS, Moonan PK. Estimating the burden of tuberculosis among foreign-born persons acquired prior to entering the U.S., 2005–2009. PLoS One. 2011;6:e27405. doi: 10.1371/journal.pone.0027405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Thoracic Society Targeted tuberculin testing and treatment of latent tuberculosis infection. MMWR Recomm Rep. 2000;49:1–51. [PubMed] [Google Scholar]
- 13.Cain KP, Haley CA, Armstrong LR, Garman KN, Wells CD, Iademarco MF, Castro KG, Laserson KF. Tuberculosis among foreign-born persons in the United States: achieving tuberculosis elimination. Am J Respir Crit Care Med. 2007;175:75–79. doi: 10.1164/rccm.200608-1178OC. [DOI] [PubMed] [Google Scholar]
- 14.Patel S, Parsyan AE, Gunn J, Barry MA, Reed C, Sharnprapai S, Horsburgh CR., Jr Risk of progression to active tuberculosis among foreign-born persons with latent tuberculosis. Chest. 2007;131:1811–1816. doi: 10.1378/chest.06-2601. [DOI] [PubMed] [Google Scholar]
- 15.Cain KP, Mac Kenzie WR. Editorial commentary: overcoming the limits of tuberculosis prevention among foreign-born individuals: next steps toward eliminating tuberculosis. Clin Infect Dis. 2008;46:107–109. doi: 10.1086/523732. [DOI] [PubMed] [Google Scholar]
- 16.Cain KP, Benoit SR, Winston CA, Mac Kenzie WR. Tuberculosis among foreign-born persons in the United States. JAMA. 2008;300:405–412. doi: 10.1001/jama.300.4.405. [DOI] [PubMed] [Google Scholar]
- 17.Hill AN, Becerra J, Castro KG. Modelling tuberculosis trends in the USA. Epidemiol Infect. 2012;140:1862–1872. doi: 10.1017/S095026881100286X. [DOI] [PubMed] [Google Scholar]
- 18.Walter ND, Painter J, Parker M, Lowenthal P, Flood J, Fu Y, Asis R, Reves R, Tuberculosis Epidemiologic Studies Consortium Persistent latent tuberculosis reactivation risk in United States immigrants. Am J Respir Crit Care Med. 2014;189:88–95. doi: 10.1164/rccm.201308-1480OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shea KM, Kammerer JS, Winston CA, Navin TR, Horsburgh CR., Jr Estimated rate of reactivation of latent tuberculosis infection in the United States, overall and by population subgroup. Am J Epidemiol. 2014;179:216–225. doi: 10.1093/aje/kwt246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker BJ, Jeffries CD, Moonan PK. Tuberculosis in Mexico-Born persons in the United States—1993–2010. American Thoracic Society International Conference; San Francisco, CA. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ghosh S, Moonan PK, Cowan L, Grant J, Kammerer S, Navin TR. Tuberculosis genotyping information management system: enhancing tuberculosis surveillance in the United States. Infect Genet Evol. 2012;12:782–788. doi: 10.1016/j.meegid.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 22.US Census Bureau . Design and methodology: American Community Survey. U.S. Government Printing Office; Washington, DC: [accessed 2013 Jul 1]. 2009. Available from: http://www.census.gov/acs/www/downloads/survey_methodology/acs_design_methodology.pdf. [Google Scholar]
- 23.Baker BJ, Moonan PK. Characterizing tuberculosis genotype clusters along the United States–Mexico border. Int J Tuberc Lung Dis. 2014;18:289–291. doi: 10.5588/ijtld.13.0684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28:3670–3682. doi: 10.1002/sim.3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hlavsa MC, Moonan PK, Cowan LS, Navin TR, Kammerer JS, Morlock GP, Crawford JT, Lobue PA. Human tuberculosis due to Mycobacterium bovis in the United States, 1995–2005. Clin Infect Dis. 2008;47:168–175. doi: 10.1086/589240. [DOI] [PubMed] [Google Scholar]
- 26.Wallace RM, Kammerer JS, Iademarco MF, Althomsons SP, Winston CA, Navin TR. Increasing proportions of advanced pulmonary tuberculosis reported in the United States: are delays in diagnosis on the rise? Am J Respir Crit Care Med. 2009;180:1016–1022. doi: 10.1164/rccm.200901-0059OC. [DOI] [PubMed] [Google Scholar]
- 27.Hoefer M, Rytina N, Baker BC. [accessed 2013 Jul 1];Estimates of the unauthorized immigrant population residing in the United States: January 2010, Office of Immigration Statistics, Policy Directorate, U.S. Department of Homeland Security. 2011 Available from: http://www.dhs.gov/xlibrary/assets/statistics/publications/ois_ill_pe_2010.pdf.
- 28.Achkar JM, Sherpa T, Cohen HW, Holzman RS. Differences in clinical presentation among persons with pulmonary tuberculosis: a comparison of documented and undocumented foreign-born versus US-born persons. Clin Infect Dis. 2008;47:1277–1283. doi: 10.1086/592572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Passel JS, Cohn D, Gonzalez-Barrera A. Net migration from Mexico falls to zero—and perhaps less. Pew Hispanic Center; Washington, DC: 2012. [Google Scholar]
- 30.Pascopella L, Deriemer K, Watt JP, Flood JM. When tuberculosis comes back: who develops recurrent tuberculosis in California? PLoS ONE. 2011;6:e26541. doi: 10.1371/journal.pone.0026541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu Y, Weinberg MS, Ortega LS, Painter JA, Maloney SA. Overseas screening for tuberculosis in U.S.-bound immigrants and refugees. N Engl J Med. 2009;360:2406–2415. doi: 10.1056/NEJMoa0809497. [DOI] [PubMed] [Google Scholar]
- 32.Lowenthal P, Westenhouse J, Moore M, Posey DL, Watt JP, Flood J. Reduced importation of tuberculosis after the implementation of an enhanced pre-immigration screening protocol. Int J Tuberc Lung Dis. 2011;15:761–766. doi: 10.5588/ijtld.10.0370. [DOI] [PubMed] [Google Scholar]
- 33.US Department of Homeland Security. Office of Immigration Statistics [accessed 2013 Jul 1];Yearbook of immigration statistics. 2009 Available from: http://www.dhs.gov/xlibrary/assets/statistics/yearbook/2009/ois_yb_2009.pdf.
- 34.Passel JS, Cohn D. Unauthorized immigrant population: national and state trends, 2010. Pew Hispanic Center; Washington, DC: 2011. [Google Scholar]
- 35.Zuber PLF, McKenna MT, Binkin NJ, Onorato IM, Castro KG. Long-term risk of tuberculosis among foreign-born persons in the United States. JAMA. 1997;278:304–307. [PubMed] [Google Scholar]
- 36.Painter JA, Graviss EA, Hai HH, Nhung DT, Nga TT, Ha NP, Wall K, Loan TH, Parker M, Manangan L, et al. Tuberculosis screening by tuberculosis skin test or QuantiFERON-TB Gold In-Tube Assay among an immigrant population with a high prevalence of tuberculosis and BCG vaccination. PLoS One. 2013;8:e82727. doi: 10.1371/journal.pone.0082727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moonan PK, Ghosh S, Oeltmann JE, Kammerer JS, Cowan LS, Navin TR. Using genotyping and geospatial scanning to estimate recent mycobacterium tuberculosis transmission, United States. Emerg Infect Dis. 2012;18:458–465. doi: 10.3201/eid1803.111107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bennett DE, Courval JM, Onorato I, Agerton T, Gibson JD, Lambert L, McQuillan GM, Lewis B, Navin TR, Castro KG. Prevalence of tuberculosis infection in the United States population: the National Health and Nutrition Examination Survey, 1999–2000. Am J Respir Crit Care Med. 2008;177:348–355. doi: 10.1164/rccm.200701-057OC. [DOI] [PubMed] [Google Scholar]
- 39.Menzies D, Gardiner G, Farhat M, Greenaway C, Pai M. Thinking in three dimensions: a web-based algorithm to aid the interpretation of tuberculin skin test results. Int J Tuberc Lung Dis. 2008;12:498–505. [PubMed] [Google Scholar]
- 40.Horsburgh CR, Jr, Rubin EJ. Clinical practice: latent tuberculosis infection in the United States. N Engl J Med. 2011;364:1441–1448. doi: 10.1056/NEJMcp1005750. [DOI] [PubMed] [Google Scholar]
- 41.Mazurek GH, Jereb J, Vernon A, LoBue P, Goldberg S, Castro K, IGRA Expert Committee. Centers for Disease Control and Prevention (CDC) Updated guidelines for using interferon gamma release assays to detect Mycobacterium tuberculosis infection—United States, 2010. MMWR Recomm Rep. 2010;59:1–25. [PubMed] [Google Scholar]
- 42.Sterling TR, Villarino ME, Borisov AS, Shang N, Gordin F, Bliven-Sizemore E, Hackman J, Hamilton CD, Menzies D, Kerrigan A, et al. TB Trials Consortium PREVENT TB Study Team Three months of rifapentine and isoniazid for latent tuberculosis infection. N Engl J Med. 2011;365:2155–2166. doi: 10.1056/NEJMoa1104875. [DOI] [PubMed] [Google Scholar]