Abstract
The human tissue kallikrein and kallikrein-related peptidases (KLKs), encoded by the largest contiguous cluster of protease genes in the human genome, are secreted serine proteases with diverse expression patterns and physiological roles. Because of the broad spectrum of processes that are modulated by kallikreins, these proteases are the subject of extensive investigations. This review brings together basic information about the biochemical properties affecting enzymatic activity, with highlights on post-translational modifications, especially glycosylation. Additionally, we present the current state of knowledge regarding the physiological functions of KLKs in major human organs and outline recent discoveries pertinent to the involvement of kallikreins in cell signaling and in viral infections. Despite the current depth of knowledge of these enzymes, many questions regarding the roles of kallikreins in health and disease remain unanswered.
Keywords: kallikrein, PSA, EGF, serine proteases, enzymatic activity, glycosylation
1. General overview
Kallikreins are a family of proteases consisting of 15 closely related, secreted serine proteases with either trypsin-like or chymotrypsin-like specificity. The discovery of kallikreins in pancreatic extracts dates back to the 1930s, when a protease with the ability to release bradykinin and Lys-bradykinin from a Low Molecular Weight Kininogen (kininogenase) was described and shown to constitute an essential step in bradykinin B1 and B2 receptor signaling. Subsequently the term kallikreins was adapted to describe two isoforms of the kallikrein protease: plasma kallikrein (produced in the pancreas and circulating in the blood) and tissue kallikrein (expressed in various tissues). The tissue kallikreins consist of 15 proteases encoded by genes located on chromosome 19q13.4, which constitute the largest protease gene cluster in the human genome [1] (Fig.1A,B). All kallikreins are single polypeptides composed of 244–253 residues and share 40% identity with each other. The first described tissue kallikrein was named KLK1; the remaining 14 are called kallikrein-related proteases (KLK2–KLK15). Interestingly, plasma kallikrein, the first enzyme discovered to release kinins was found to be an unrelated protease, encoded by the KLKB1 gene, located on chromosome 4q34–35. Although the traditional name plasma kallikrein is still in use, the enzyme is not regarded as a member of the kallikrein family of peptidases.
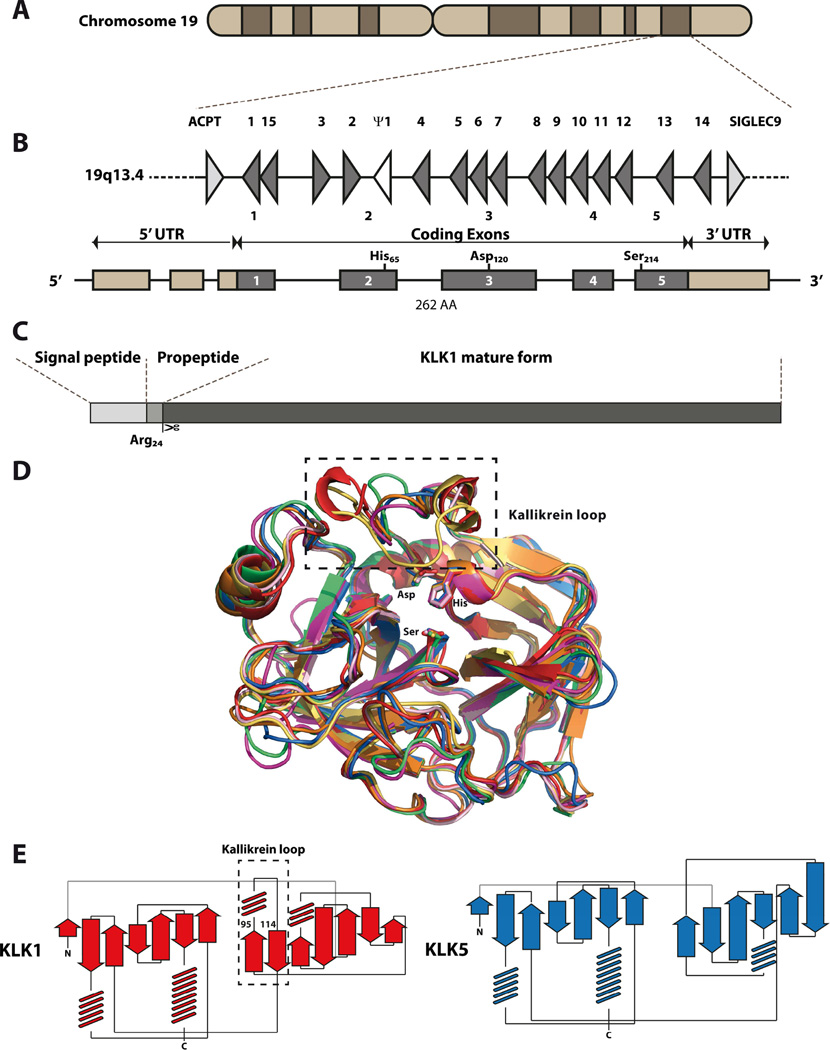
Figure 1. Gene, mRNA and protein structure of kallikreins.
(A) Kallikrein gene cluster 19q13.4 is located on the chromosome 19 and is flanked by testicular acid phosphatase (ACPT) and by sialic acid-binding Ig-like lectin 9 (SIGLEC9). It consists of 15 functional genes, represented by grey triangles and numbered 1–15 and single KLK1 pseudogene (Ψ1), represented by white triangle. (B) kallikreins are typically transcribed to the mRNA with 5 coding exons (dark grey boxes), where exon 2 carries catalytic His65, exon 3 Asp120 and exon 5 Ser214, as exemplified by KLK1 mRNA. The coding sequence is flanked by 5’ and 3’ regulatory UTR regions. (C) Kallikreins are produced as pre-pro-proteins, with N-terminal signal peptide, removed during secretion to extracellular milieu, followed by propeptide and mature, serine protease domain. Propeptide is removed extracellularly either by autocatalysis or by action of another protease (another KLK, MMP etc.). Typically, the activation requires proteolytic cleavage after basic residue, with exception of KLK4, which require hydrolysis after Gln30 for maturation.(D) Structural alignment of seven known kallikrein structures. Each kallikrein is represented as ribbon and colored accordingly, with RCSB accession codes as follows: KLK1 – red (1SPJ), KLK2 – pink (4NFE), KLK3/PSA – yellow (2ZCL), KLK4 – green (4KGA), KLK5 – blue (2PSX), KLK6 – violet (4D8N) and KLK7 – orange (3BSQ). Location of kallikrein loop in KLK1–3 is marked as frame at the top right and additional short loop can be seen in the same region in KLK4 structure. Catalytic triad is presented as sticks and its particular residues are labeled. Kallikrein share typical fold of the serine protease of S1 family. Two β-barrel- based lobes interact together to form active site and to create the substrate binding cleft. Kallikrein loop is located near the active site and partially occludes the S1 subsite. Due to its high mobility, the exact structure of the kallikrein loop is not determined in the deposited PDB files. (E) Schematic representation of the KLK1 and KLK5 secondary structure topology. The presence of kallikrein loop is marked in the black frame and residue locations of the start and the end of the whole loop structure are numbered. The presence of the kallikrein loop introduces the additional, short α-helical fragment and forces the change in the topology of the region. This figure is based on [2].
2. Kallikreins as proteases: basic information
Tissue KLKs belong to the chymotrypsin-like S1 family of serine endopeptidases (a sub-group of the PA clan of serine peptidases) that includes approximately 80% of the 178 known human serine proteases. This family includes major proteases such as thrombin, trypsin, chymotrypsin, elastase and matriptase (MEROPS Peptidases database). Thus, all the S1 proteases share similar features, including sequence similarities (e.g., human trypsin and KLK14 share 38.8% sequence identity), organization of the catalytic triad, structural organization, and a mechanism of activation involving the removal of a short N-terminal pro-fragment (Fig.1C).
2.1. Structure
Kallikreins, like other members of the S1 family, are classified based on sequence similarities, a conserved catalytic triad and general substrate specificity. The overlay of the seven available kallikrein structures confirms their typical chymotrypsin-like fold with two domains that form six-stranded beta barrels and three loops between the domains (Fig. 1D). The highly conserved active site triad of three amino acids—His57, Asp102, Ser195 (chymotrypsin numbering)—acts as a charge relay system for proteolytic catalysis, and is found at the interface of the two domains.
Kallikreins possess 10 highly conserved cysteine residues that form five disulfide bridges stabilizing the overall protein fold. An additional, sixth, disulfide bridge has been found in the majority of kallikreins, but is not present in KLK-1, -2, -3, and -13.
Moreover, KLK1, -2, and -3 contain a “kallikrein loop” – a special surface loop that is 11 residues longer then the corresponding loop of chymotrypsin (99-loop) (Fig. 1E). Because of the loop location close to Asp102 (chymotrypsin numbering), this fragment is postulated to be involved in interacting with substrates, as confirmed by structural and mutational studies of KLK2 [3]. The other six surface loops of kallikreins that surround the active site display high variability and may therefore contribute to differences in substrate specificities among kallikreins. Substrate preferences of kallikreins are determined mostly at the S1 subsite of a substrate-binding cleft (Schechter and Berger nomenclature). The classical paradigm for understanding specificity at this position is derived from early crystallographic studies of chymotrypsin, elastase, and trypsin [4] showing that amino acids immediately contacting a substrate at this site determine the observed selectivity for large hydrophobic, small hydrophobic, and basic residues [5]. In kallikreins, either Asp189 or Ser189 (chymotrypsin numbering) at the S1 pocket determine substrate cleavage specificity, with preference for basic or hydrophobic amino acids, respectively.
Apart from cleaving other proteins several kallikreins can undergo autocatalysis. Structural studies of proKLK6 revealed that the Arg80-Glu81 peptide bond (amino acid numbering of full-length pre-pro-kallikrein according to UniProt database, unless stated otherwise) is highly susceptible to autocatalytic cleavage, which leads to loss of enzyme activity [6]. Similarly, KLK13 undergoes inactivating autocatalytic cleavage at the Arg114 position (TK, unpublished observations). Both positions, although distant in the primary sequence, reside in the exposed loops, surrounding the substrate-binding cleft on the enzyme surface. This autocatalytic processing is believed to form an additional regulatory mechanism for modulating the protease activity of kallikreins.
2.2. Controlling protease activity
Dysfunctions in tissue-specific regulation of KLK activity has been linked to several pathologies, including respiratory diseases, neurodegeneration, anxiety, schizophrenia, skin-barrier dysfunction, pathological inflammation, and cancer. Endogenous KLK activity is controlled on multiple levels by different mechanisms and factors, including zymogen activation cascades, endogenous KLK inhibitors (circulatory molecules such as serpins, macroglobulins and tissue serine protease inhibitors from the lympho-epithelial Kazal-type-related inhibitor family, LEKTIs), and micro-environmental pH and single-metal-ion inhibitors of KLKs (such as Zn2+) [7]. Specific inhibitors of KLKs, given appropriate pharmacokinetic and pharmacodynamic properties, could potentially function as novel therapeutics for the above mentioned pathologies.
The activation of pro-KLKs is a key mechanism in regulating KLK activity in tissues [8]. The kallikreins are synthesized as inactive pre-pro-proteins that are secreted to the extracellular space. The zymogen form of pro-KLKs are activated extracellularly by the trypsin-like cleavage of their pro-peptide after either an arginine or lysine (Fig.2). The exception is pro-KLK4, which is activated by metalloproteinase-mediated cleavage after Gln30. The activating cleavage is performed either autocatalytically by the kallikrein itself (KLK2, KLK6 and KLK13) or by endogenous proteases that are yet unknown. In vitro studies have identified some proteases that activate kallikreins: trypsin activates KLK-1, -3, -5, - 6, -7, 15; thermolysin, plasma kallikrein, and plasmin cleave KLK1; and lysyl endopeptidase activates KLK6 [8]. Using a fusion construct approach and 12 mature KLKs, activation profiles for the 15 pro-KLKs were determined. The network of KLK interactions apparent from this study combined with previous data suggests that activation cascades exist in different tissues. Unfortunately, the emerging network of interactions is too complex to be accepted as the final activation scheme for pro-KLKs [9]. A detailed mechanism of maturation was proposed for pro-KLK6, based on structural studies of the pro-enzyme. After pro-fragment cleavage at the Lys21-Leu22 peptide bond, the N-terminal region (Leu22-Pro34) of the enzyme folds towards the protein surface. This movement induces several structural rearrangements that ultimately lead to formation of the salt bridge between Leu22 at the new N-terminus and Asp196 and correct positioning of the catalytic Ser197. Additionally, some surface loops are repositioned upon pro-enzyme activation [8].
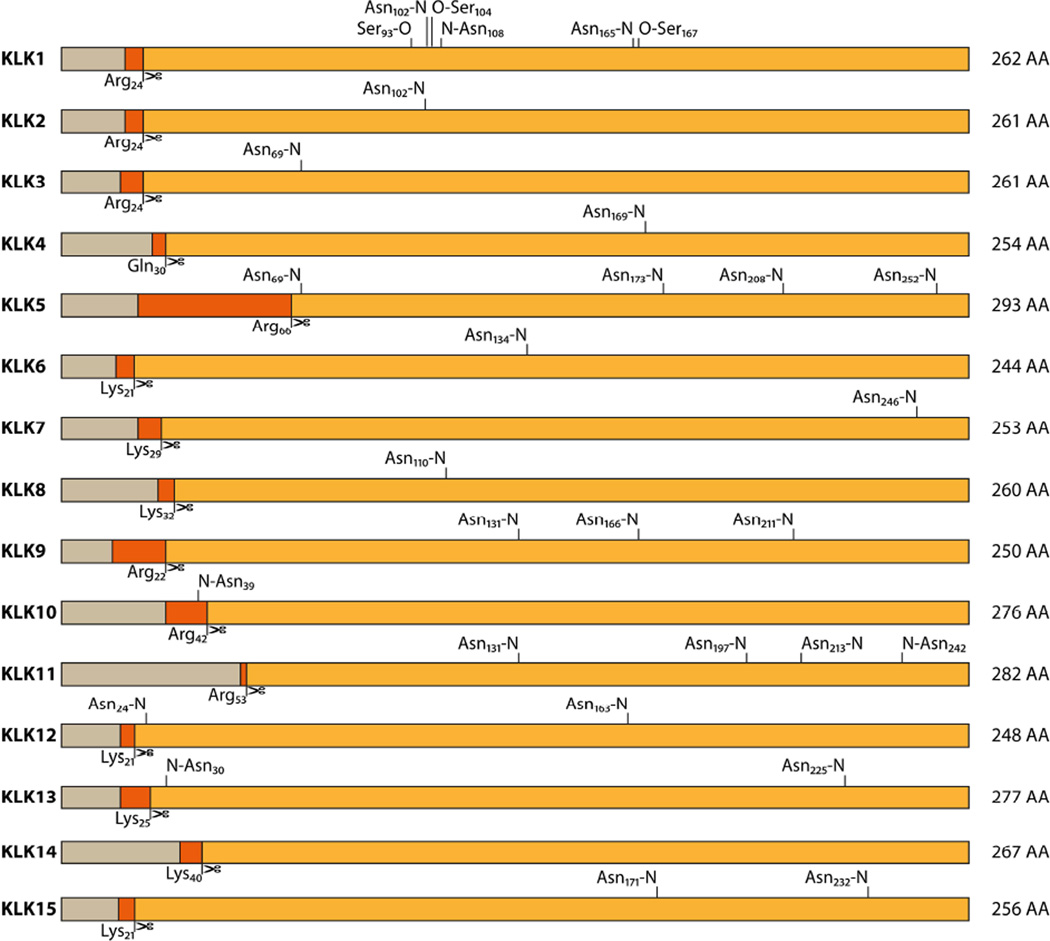
Figure 2. Schematic presentation of kallikrein post-translational modifications.
Sequences are presented according to the UniProt system. Signal peptides are presented in gray; propeptides are shown in dark orange. Pale orange boxes represent the full-length mature kallikreins. Activation cleavage sites, marked with scissors are denoted below each kallikrein, while glycosylation locations are described above, with the respective residue and O- or N-glycosylation type noted. All distances are presented in proportion to the full-length preproprotein. Residue numbering is consistent with the UniProt database. All kallikreins are activated by Lys- or Arg-specific (tryptic-like) cleavage, with exception of KLK4, which requires hydrolysis after Gln30. Glycosylation in the KLK1 and KLK2 is located in the region of the “kallikrein loop” (residues 102–118 in KLK1). In KLK5, KLK12 and KLK13 glycans are added at the region proximal to the activation site or within the propeptide itself (KLK10), possibly affecting the activation of these proteases. For more details see text.
2.2.1. Inhibitors
Once released into the extracellular matrix, endogenous proteins, including protein tissue and plasma protease inhibitors, as well as simple cations such as Zn2+, can inhibit kallikreins. The zinc cation interacts with salt bridges formed in active sites of KLK4 [10], KLK5 [11], and KLK7 [12], or modifies the kallikrein loop in KLK2 [3].
Endogenous inhibitors, present in the blood plasma and to some extent penetrating into tissues, include proteins of the serpin family [13]. Serpins target almost exclusively proteases of the S1 family and are certainly involved in control of kallikrein activity [14]. Although serpins, as exemplified by α1-antitrypsin [15], have a long history of therapeutic use and are the best studied inhibitors for kallikreins [16–18], it is unlikely that they can be used in therapies targeting single kallikreins. Interestingly, α2-macroglobulin (α2M), a serum derived pan-proteinase inhibitor that clears proteases destined for degradation from the blood, can control the activity of only KLK1, KLK2, and KLK3. Despite the α2M trapping mechanism of inhibition, the remaining kallikreins are not inhibited by this high molecular weight protein [7].
With different members of the kallikrein family expressed in various tissues, tissue-specific inhibitors are the main attenuators of kallikrein activity. The main group of kallikrein inhibitors includes the canonical Kazal-type inhibitors from the SPINK/LEKTI family (Serine Proteinase INhibitor Kazal-type/Lympho-Epithelial Kazal-Type Inhibitor). This emerging group of inhibitors was initially described based on the discovery of LEKTI/SPINK5 [19, 20], a large, 15-domain protein in which each domain has the Kazal-type fold and is presumed to be a proteinase inhibitor. Indeed, this protein is processed into smaller units and the individual fragments inhibit KLK5 and KLK7 [21–23]. Interestingly, SPINK5 gene dysfunctions were quickly correlated with the development of Netherton syndrome and atopic dermatitis [20]. Additional members of the SPINK/LEKTI family are currently being described, including SPINK6 [24] and SPINK9 [25, 26]. Nanomolar levels of SPINK6 inhibit KLK4, KLK5, KLK12, KLK13, and KLK14 [27], and SPINK6 activity is further modulated by crosslinking it to the extracellular matrix [28]. By contrast, SPINK9 inhibition seems to be limited to KLK5, while other kallikreins expressed in the skin, KLK4 and KLK14, are unaffected [25].
In addition to the natural, circulating or tissue-specific inhibitors, attempts to engineer specific kallikreins inhibitors have been reported. Specific antibodies reduced the activity of plasma kallikrein that is involved in hereditary angioedema and other disorders [29]. Similarly, a KLK13 specific mAb inhibited the activity of this kallikrein, suggesting that it might have therapeutic application in the treatment of ovarian cancer patients [30]. The overall stability, good tolerance, and long-term inhibitory activity encourage further investigations into the development of specific antibodies as potential therapeutic agents in the treatment of pathologies related to excessive kallikrein activity [31].
Alternatively, a number of synthetic inhibitory compounds were designed (based on the properties of natural endogenous protease inhibitors) and synthesized [32–34] and some have been tested in clinical trials for kallikrein-related diseases [35]. Caution is needed in the implementation of new therapeutic agents since all aspects of their biological activity must be taken into consideration. First, determination of an actual therapeutic target is a challenging task when the interaction network of a kallikrein and its protein partners is considered. Secondly, the selectivity of a reactive inhibitory compound needs to be well defined, as the structural configuration of the active site is very similar among kallikreins. Therefore, the inhibitor design requires detailed structural investigations of the enzyme fold and extended mapping of the specificity of substrate-binding subsites and surface exosites. Thirdly, the toxicity, pharmacokinetics, and biochemical stability of the compound in human biological fluids need to be considered. Likely, kallikreins can perform similar biological activities, being regulated not exclusively by their substrate specificity, but rather by the expression pattern in various tissues and, therefore, will display similar substrate and inhibitory patterns. These factors highlight the need for optimal inhibitor design and careful verification of side effects, metabolism, and distribution of the inhibitor in various tissues.
2.2.2 Activity control by glycosylation
According to structural data, molecular weight, and sequence analysis of KLKs, all members possess at least one potential glycosylation site (Fig.2). Although most sites are N-glycosylation sites (sequence motif: Asn-Xaa-Ser/Thr), O-glycosylation sites have also been found, but less frequently. Not every potential glycosylation site is occupied in vivo, as exemplified by KLK14, which, regardless of the expression system (yeast, insect, primate and human cells), is not glycosylated on its Asn-Ile-Ser sequence motif. Glycosylation influences not only protein folding and stability, but also impacts activity.
The importance of glycosylation is apparent in the activation of pro-KLK13. The recombinant kallikrein expressed in yeast cells possesses two sites of activation, Lys25 and Phe35, and one glycosylation site located between these two residues at Asn30. Depending on the glycosylation pattern, the activation cleavage results in release of two different active variants of KLK13. The presence of a glycan attached to Asn30 prevents cleavage after Phe35 [36]. The presence of glycans affects the activity of most kallikreins, including KLK-3, -4, -8, and -13. The exceptions are KLK-1, -2, and -15 [36]. However, research to date on kallikrein glycosylation has been conducted using proteins expressed either in bacterial or yeast expression systems, resulting in no glycosylation or non-homogeneous glycosylation. Therefore, until such analyses are performed on KLKs expressed in mammalian cells, conclusions regarding the presence and role of glycosylation should be considered preliminary.
Glycosylation of KLK3, the main biomarker of prostate cancer, has a significant effect on protease activity against small synthetic substrates [37], and the differences between non-glycosylated and glycosylated forms are mostly attributed to substrate-binding preferences at the P1 position [38–40]. The activity differences can be explained at the structural level as glycosylated KLK3 has a large glycan linked to Asn69, which resides near the substrate-binding cleft close to the primed-site of the active site [41, 42].
Therefore, differences in the glycosylation of KLK3, often observed in prostate cancer development, are linked to enzymatic dysfunction [43–45]. Moreover, variations in the glycosylation pattern of KLK3 are correlated with metastasis of this cancer [46] and seem to possess diagnostic value; however, this correlation will require further validation before it can serve as the basis for the development of a diagnostic tool. KLK6, the kallikrein that exhibits hyperactivity in ovarian cancer, exhibits sialylation and glycosylation patterns that are more heterogeneous in cancer cells than in normal cells (from cerebrospinal fluid) [47, 48]. Such differences may also have applications in the detection and prognosis of ovarian cancer.
Another aspect of the effect of glycans on kallikrein activity is their interaction with glycosaminoglycans (GAGs) in the extracellular matrix. Hyaluronic acid is involved in innate immunity at the apical pole of epithelial cells lining air ways of the lung and can spatially limit the proteolytic activity of KLK1 through immobilization of the protease [49]. However, depolymerization and breakdown of hyaluronic acid upon exposure to reactive oxygen species derived from tobacco smoke or endogenous sources can result in the release of KLK1 and loss of the spatial constraints on activity [50].
Detailed studies on GAG (heparin, heparan sulfate, dermatan sulfate, and chondroitin sulfate) activation of kallikreins have been performed on KLK-6, -7, and -13. KLK6 activity was increased by these GAGs in a concentration-dependent manner, but with distinctly different profiles at pH 7.5 vs. pH 9.0 [51]. At pH 7.5, KLK13 activity was rapidly activated by heparin, whereas chondroitin and dermatan sulfate only moderately activated KLK13 [52]. This activation was described for insect-cell-derived, non-natively-glycosylated KLK13 and, therefore, these results must be treated with caution. Recently, KLK7 showed increased activity when it was incubated with GAGs [53]. Heparan sulfate also facilitates interactions between kallikreins and their substrates. This phenomenon is exemplified by KLK8-mediated cleavage of the major capsid protein L1 of human papillomaviruses. L1 is required for infection and cleavage is enabled by prior interaction of viral particles with heparan sulfate proteoglycans [54].
KLKs may also be effectively modulated in the in vivo microenvironment by ion concentrations. The hydrolytic activity of KLK13 is substantially activated by kosmotropic salts, including sodium citrate and sodium sulfate [52]. Sodium citrate is present in normal prostate tissue and in seminal fluid at high concentrations [55] and can be a potential physiological modulator of KLK13 activity, since it is present in the prostate and testis, as well as in female reproductive organs [56]. KLK6 exhibited the highest activity in buffers containing sodium citrate (in a concentration-dependent manner) and sodium sulfate at pH 7.5, whereas these same salts inhibited the enzyme at pH 9.0 [51]. The anion-dependent activation of KLK6 followed the Hofmeister series, citrate > sulfate > acetate > chloride, but only at pH 7.5. In contrast to the observed activating effects of the kosmotropic salts sodium citrate and sodium sulfate on KLK-3, -6 and -13, these salts reduced KLK7 and KLK1 activity at concentrations up to approximately 250 mM [53]. The activity of KLK7 returned to its initial level at concentrations close to 1.2 M for both salts, but KLK1 recovered only half of the initial activity at this high salt concentration. In contrast to the kosmotropic salts, NaCl reduced the activity of KLK7 and KLK1 in all assayed ranges of salt concentration.
2.3. Substrate specificity
The trypsin-like KLKs (KLK2, KLK4–KLK6, KLK-8, -10, -12, -13, and -15) have a strict preference for a positively-charged residue (arginine or lysine) at the P1 position, while the chymotrypsin-like kallikreins (KLK-3, -7, and -9) cleave peptide bonds with tyrosine, tryptophan or phenylalanine at the P1 position. Interestingly, three kallikreins (KLK-1, -11, and -14) exhibit dual specificity, exhibiting both trypsin-like and chymotrypsin-like cleavages. The P1 amino acid preferences can be explained by structure analysis, consistent with the classical trypsin and chymotrypsin overall fold and topology of the primary subsite (S1) of the substrate-binding cleft [57]. In the trypsin-like proteases, the carboxylate group of Asp189 (chymotrypsin numbering) forms a strong ionic bond either with the positively-charged guanidine moiety of the P1 arginine or the alkyl amine moiety of the lysine side chain. By contrast, the amino acid in the corresponding position in chymotrypsin-like KLKs is Ser207 (in KLK3), Asn199 (in KLK7), or Gly198 (in KLK9). Interestingly, the dual specificity can be explained by interaction with the well-organized solvent network in the S1 pocket, which either forms a hydrogen-bond network with positively-charged side chains or is displaced by large hydrophobic residues such as Met. Additionally, substrate binding induces the correct orientation of the catalytic triad residues in the active site of the enzyme as exemplified by KLK1 [58].
Multiple approaches have been applied to reveal subtle differences in specificity exerted by different kallikreins [40, 59, 60] (summarized in Table 1). Unfortunately, application of different methods with variable sensitivities has generated inconsistent conclusions. Each applied method has limitations and disadvantages, even though each individually is helpful in determining protease cleavage site consensus motifs [61]. Despite continuous improvement of high-throughput synthetic and proteomic methods in determining substrate specificity [62], these methods may fail to yield compelling explanations if enzymatic specificity is influenced by exosite interactions and structural adaptations upon substrate binding [63].
Table. 1.
Summary of major methods applied in kallikrein substrate specificity profiling [9, 40, 51, 52, 59, 60, 64–76]
| Protease | Specificity | PS-SCL | Phage | Peptides |
|---|---|---|---|---|
| KLK1 | mix | X | X | |
| KLK2 | tryptic | X | X | |
| KLK3 | chymo | X | X | X |
| KLK4 | tryptic | X | ||
| KLK5 | tryptic | X | ||
| KLK6 | tryptic | X | X | X |
| KLK7 | chymo | X | ||
| KLK8 | tryptic | X | ||
| KLK9 | chymo | X | ||
| KLK10 | typtic | X | X | |
| KLK11 | mix | X | ||
| KLK12 | tryptic | X | ||
| KLK13 | tryptic | X | X | |
| KLK14 | mix | X | X | X |
| KLK15 | tryptic | X |
3. Physiological function of KLKs
One or more KLK genes are expressed in nearly all tissues and the enzyme(s) are found in the majority of physiological fluids in the human body. The majority of KLKs, however, have a more restricted distribution. Over a century of basic research has contributed to the elucidation of the putative functions of each kallikrein and their protein interaction networks within the human proteome [77]. Nevertheless, ongoing research continues to reveal novel functions for each kallikrein. These numerous studies have characterized KLKs as regulatory proteases with key signaling and innate immunity-related properties. The KLK proteases are now known to be involved in mechanistic pathways that regulate skin desquamation, tooth enamel formation, kidney function, seminal liquefaction, synaptic neural plasticity, and brain function.
3.1. KLKs within the skin
One of the most intensively studied organs for KLK function is the skin. Here, the pioneering work of Torbjörn Egelrud and colleagues identified proteases in the uppermost part of the skin, the stratum corneum, which are involved in keratinocyte detachment (desquamation) and inflammatory processes of the skin. This research led to the discovery of KLK5 (formerly known as “stratum corneum tryptic enzyme”) [78] and KLK7 (described as “stratum corneum chymotryptic enzyme”) [79], which were purified from stratum corneum extracts and shown to be involved in desquamation [80]. Eight KLKs (KLK-5, -6, -7, -8, -11, -12, -13, and -14) have currently been detected in healthy skin (reviewed in [81]); however, their exact mode of action is being studied in detail. In addition to being involved in desquamation, KLK7 activates interleukin-1beta (IL-1F2) in human skin [82]. Since the classical IL-1 converting enzyme, caspase-1, is produced by keratinocytes at very low levels, KLK7 may be crucial for activation of IL-1F2 in human epidermis. Mouse KLK13 activates IL-1F2 in the submandibular gland [83], suggesting that more KLKs than KLK7 alone may be involved in IL-1 processing. KLK5 processes the pro-inflammatory antimicrobial peptide human cathelicidin [84]. This event is thought to play a major role in the pathophysiology of the inflammatory skin disease rosacea [85, 86]. The importance of KLKs in skin homeostasis is clearly seen in Netherton syndrome, a severe skin disease in which the KLK inhibitor LEKTI is absent, as discussed earlier (see paragraph 2.2.1). Transgenic KLK-5 and -7 mice reproduce the major cutaneous and systemic hallmarks of the Netherton syndrome, including epidermal thickness, hyperkeratosis, dermal inflammation, and severe pruritus [87, 88]. Also KLK8 has been described as kallikrein expressed by keratinocytes, with potential function in skin barrier proteolytic function [89]. More detailed study indicate the C-terminal fragment of KLK8 as one of the peptides involved in skin innate immunity [90].
3.2. KLKs within tooth enamel
Formation of tooth enamel is a multistep process dependent on the cooperation of various proteins and proteases, which include KLK4 (known as enamel-matrix protease 1). KLK4 is involved in the final stages of this process, the transition and formation steps (described in detail in [91]), as it degrades enamel-matrix proteins (including enamelin and ameloblastin) and facilitates the lateral expansion of the hydroxyapatite crystal of the tooth via a transforming growth factor-β (TGF-β)-associated mechanism [91–93]. Mutations in the KLK4 gene resulting in the dysfunction of this protease lead to the autosomal recessive condition known as hypomaturation amelogenesis imperfecta, which leads to defective tooth mineralization and crystal formation [94, 95]. Moreover, KLK4 is involved in degradation of amelogenin, remodeling of the organic matrix, and disruption of the intercellular junctions in tooth development. KLK4 overexpression and hyperactivity has been associated with oral squamous cell carcinoma metastasis [96].
3.3. KLKs within the reproductive system
The majority of studies on kallikreins and their physiological functions have focused on KLK3, also known as Prostate Specific Antigen (PSA). Since its identification and characterization in the 1970s, KLK3 has been investigated extensively with respect to its biochemical and cellular functions as an enzyme and prostate cancer biomarker. Investigations into KLK3 as a prostate cancer marker, performed mostly by pharmaceutical companies, were fueled by its tissue specificity and incredibly high expression in prostate cancer [97]. These studies eventually led to development of diagnostic kits for the detection of the prostate cancer. However, KLK3 elevation needs to be considered in a broader biological context since it leads to frequent false-positive diagnoses followed by unnecessary treatments that have resulted in some instances in treatment-associated health problems [44, 98].
Originally, the physiological activity of KLK3 was associated with its ability to perform semen liquefaction and enhance sperm motility, which it achieves by cleaving fibronectin and seminal-gel-forming proteins semenogelin 1 and semenogelin 2 [99]. Recent reports, however, highlight the expression and mechanisms of action of other kallikreins in semen liquefaction, including proKLK3 (pro-PSA) activation by KLK-4, -5, -14, and -15, as well as the direct proteolytic activity of KLK-14 and -5 [100]. Following its activation, KLK3 degrades numerous proteins [extracellular matrix proteins, insulin-like growth factor (IGF)-binding proteins 3 and 5, and parathyroid-hormone-related protein (PTHRP)] facilitating metastasis of prostate cancer cells [65].
KLK2 is the second-best-characterized kallikrein biomarker used in prostate cancer diagnosis [101]. Despite its relatively low expression compared with PSA, utilization of KLK2 as a secondary biomarker increases the specificity and sensitivity of cancer detection [102]. To date, the only known protein substrate of KLK2 is the ARA70 - the androgen receptor coregulator [103], suggesting that KLK2 has potential function in maintaining tissue balance in the testis.
Another kallikrein highly expressed in prostate cancer is KLK4, an androgen regulated enzyme [104]. Along with PSA, KLK4 facilitates metastasis of prostate cancer to the bone because it facilitates the degradation of extracellular matrix proteins [105, 106].
Synergistic hormonal regulation of transcription of KLK genes is well documented as the underlying cause of pathological dysregulation of KLK gene expression. In a subset of tissues, KLK expression is strictly regulated by steroid hormones, including androgens, estrogens, progestins, mineralocorticoids, and glucocorticoids [107]. Accumulating evidence indicates that KLKs are coordinately up- or down-regulated at both the transcriptional and translational levels in several neoplastic diseases, including adenocarcinomas derived from steroid-hormone-regulated tissues, suggesting the existence of common regulatory pathways [108–112]. The most striking example is overexpression of KLK2–10, KLK11, and KLK13–15 transcripts and/or proteins in ovarian carcinoma tissues, cell lines and/or serum and tumor ascites fluid, which has been confirmed by several experimental approaches [113–127]. Thus, kallikreins may be coordinately expressed in a steroid hormone-dependent manner via a hormone-dependent cassette preceding kallikrein genes [128].
3.4. KLKs within the respiratory and renal systems
Despite the broad distribution of KLK12 in tissues of adult humans, the highest levels of KLK12 are found in the lungs [56]. The detailed functions of KLK12 in the lungs are largely unknown. A single report showing that KLK 12 degrades several members of the CCN family (acronym derived from the names of first three members of the family: Cysteine-rich angiogenic protein 61/CCN1, Connective tissue growth factor/CCN2 and Nephroblastoma overexpressed/CCN3) has suggested that KLK12 has an angiogenic function. CCN substrates are extracellular matrix associated signaling proteins with multiple domains interacting with various growth factors. Thus, their degradation by KLK12 may modulate the bioavailability and/or activity of growth factors, such as vascular endothelial growth factor [64]. KLK12 is dysregulated in systemic sclerosis, a disorder characterized by defective angiogenesis, and antibodies inhibiting KLK12 in human skin endothelial cells result in reduced endothelial cell growth, migration, and tubule-like formation [129]. In human lung cell lines, the proangiogenic activity of KLK12 did not correlate with kinin-dependent activation of the bradykinin B2 receptor (B2R), and a detailed mode of action awaits elucidation [130]. Recently, an effector pathway that includes degradation of PDGF-B, which induces the recruitment and proliferation of mural cells, probably through a short-range paracrine action, has implicated PDGFR in stabilizing new vessels [131].
Depending on the specific tissue, KLK1 (initially described as tissue kallikrein) expression correlates with adverse effects on tissue homeostasis. In airway diseases, KLK1 is consistently elevated in the bronchial alveolar lavage fluid of individuals with asthma or chronic bronchitis, where it is responsible for releasing kinins from a high molecular weight kininogen (HMWK) [132], resulting in hyperactivation of the bradykinin B2 receptor (B2R), which, in turn, induces bronchoconstriction and hypersecretion of mucus. KLK1 activity is also up-regulated by the presence of reactive oxygen species that cause the degradation of the hyaluronic acid present on epithelial cells lining lung airways [50]. Uncontrolled activity of KLK1 results in direct proteolytic cleavage of pro-EGF, the release of mature EGF, and subsequent activation of EGFR. Thus, KLK1 may contribute to metaplasia and mucus hypersecretion in diseases such as asthma and chronic bronchitis [133]. Moreover, such EGFR activation is also correlated with the pathological phenotypes of epithelial cells of smokers [134].
In contrast to the adverse effects of KLK1 described above, KLK1 activity in the renal and cardiovascular systems exerts multiple effects, especially at the intersection of these two systems. Released into renal tubules, KLK1 modulates the activity of epithelial sodium channels, inhibits cortical collecting duct H+, K+-ATPase activity, and activates TRPV (Transient Receptor Potential Vanilloid) channels. Moreover, due to proteolytic activity of KLK-1 on HMWK and bradykinin release, the activated bradykinin-B2 receptor (B2R) mediates beneficial effects on the progression of type 2 diabetes and hypertension and ischemic renal injury in rodents [135].
The renin-angiotensin-aldosterone system (RAAS) controls blood pressure and fluid balance and influences cardiovascular remodeling [136]. Therefore, dysregulation of RAAS by KLK1 contributes to cardiovascular and renal morbidity [137, 138]. Recent studies indicate contradictory effects of elevated levels of KLK1 expression on diabetic nephropathy. KLK1 exhibits renoprotective effects [139], but can also mediate a pro-inflammatory pathway via Proteinase Activated Receptor (PAR) activation [140]. Despite extensive research aimed at better understanding the molecular basics of renal and cardiovascular diseases, the overall view of interplay between kallikreins and other functional proteins still is unclear.
3.5. KLKs within neural system
Neural plasticity requires permanent protein modifications, which includes proteolytic cleavage. The presence of active proteases within the small synaptic space suggests their activity is strictly regulated, as any 'misbehavior' would result in neural disorders [141].
The kallikrein predominantly expressed in brain is KLK6, expressed primarily in oligodendrocytes, pyramidal cells, astrocytes, and glial cells. KLK6 may be involved in the pathogenesis of neurodegenerative disorders, including Alzheimer's disease, Parkinson's disease, and multiple sclerosis [142, 143]. KLK6 (zyme/protease M/neurosin) appears to be down-regulated in serum and tissues of Alzheimer's disease patients and may be involved in amyloid metabolism [143, 144]. Moreover, recent studies also correlate lower expression of KLK6 with increased glioma growth [145]. Whereas in case of glioblastoma, a highly malignant type of glioma tumor with different physiology then glioma, KLK6 is responsible for reduction in cell sensitivity to cytotoxic agents, including staurosporine and cisplatin, and current standard treatments of radiotherapy, or temozolomide, alone or in combination. The ability of KLK6 to promote resistance of glioblastoma cells to apoptosis depends on activation of the PAR1 receptor [146]. A similar mode of action mediates development of astrogliosis, where KLK6 functions as a trigger of selected physiological processes [147].
Another central nervous system (CNS) disease where KLK6 activity seems to be essential is Parkinson’s disease. In vitro cell-based studies show that KLK6 can extracellularly degrade an unphosphorylated form of α-synuclein, an aggregate-forming protein important in the progression of the disease; phosphorylation prevents α-synuclein polymerization. Interestingly, phosphorylation of α-synuclein decreases the ability of KLK6 to hydrolyze the protein, yet more detailed structural studies are needed to elucidate this phenomenon.
KLK6 is involved in the process of demyelination in the CNS through degradation of myelin basic protein and a rat myelin oligodendrocyte glycoprotein [148]. Elevated levels of KLK6 are detected in active multiple sclerosis lesions and patient sera [149]. In addition to cleaving myelin proteins such as the myelin basic protein, KLK6 can cleave components of the blood–brain barrier, such as laminin, fibronectin and collagens, and can induce inflammation via the activation of cell-surface PARs [150]. Studies show that PAR2 modulates neuro-inflammation by enhancing demyelination and that application of KLK6-inactivating antibodies can reduce the pathobiological role of KLK6 [151, 152].
Another kallikrein expressed in the CNS is KLK8, whose localization is limited to the hippocampus, the lateral nucleus of the amygdala, and other areas of the limbic system, all of which are involved in learning and memory [153]. Mice with impaired KLK8 activity exhibit diminished early-phase, long-term potentiation (LTP) in the Schaffer collateral pathway and in the hippocampus-dependent memory [154]. A postulated mode of action involves transient activation of pro-KLK8 in an NMDA receptor-dependent manner. The activated KLK8 immediately cleaves Synaptic Adhesion Molecule in the presynaptic site and releases the effector, a neuropsin-specific extracellular 180-kDa fragment [155]. The association of KLK8 activity with learning was highlighted by the observation that KLK8 deficiency completely impaired the early phase of LTP, leading to the absence of late associativity. Associations between early and persistent-LTP synapses may be related to mammalian working memory and, consequently, to integration in learning and memory [156]. Moreover, KLK8 proteolytic activity is correlated with the development of schizophrenia, where neuregulin 1 (NRG1) is expressed as dysfunctional isoforms. KLK8-mediated cleavage of NRG1 results in the release of the NRG1 EGF-like domain, which, in turn, activates ErbB4 receptors and leads to an impairment of γ-aminobutyric acid (GABA)-ergic inhibitory transmission and excessive postsynaptic excitation [157].
3.6. Kallikreins as EGF-signaling modulators
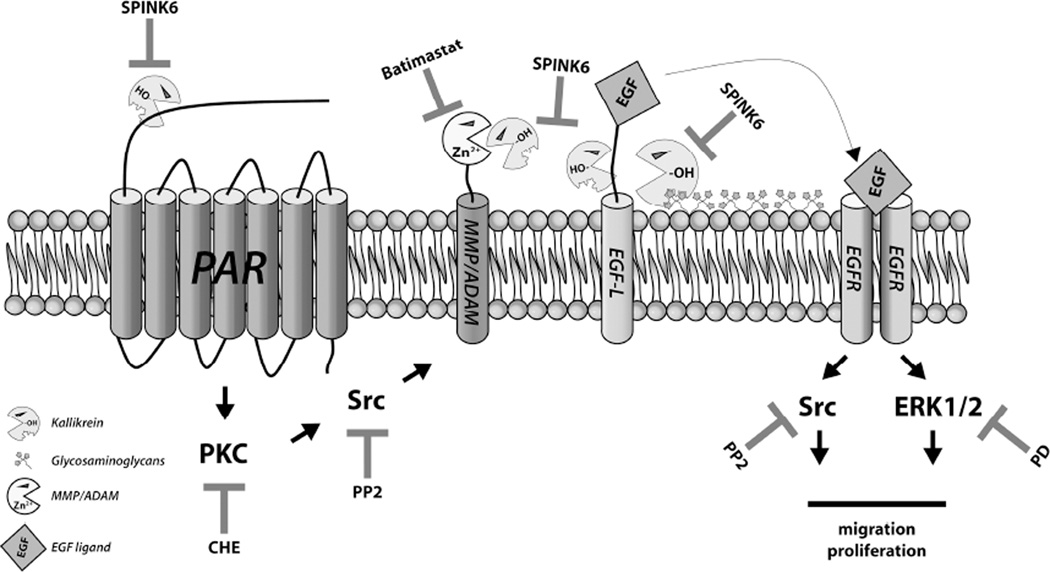
The role of kallikreins as EGF processing enzymes in cell signaling networks described in reports from the mid-90s in mice and rats became grossly underappreciated after the discovery of ADAMs and their role in EGF-mediated signaling activation [158] (Fig. 3). Kallikreins appear to be ADAM activators that result in release of endogenous ADAM substrates such as EGF or TNF-α [159].
Figure 3.
Schematic representation of the role of kallikreins in EGF signaling. Kallikreins may interact with PAR receptors, leading to the activation of Protein Kinase C and signal propagation, which promotes the activation of cell-surface ADAMs/MMPs. Activated metallopeptidases shed the EGF receptor ligands and consequently activate EGFR. Alternatively, kallikreins may directly activate cell-surface MMPs/ADAMs, or directly shed EGF ligands, possibly docking to the cell surface via glycosaminoglycan interactions. Signal transduction may be blocked by application of specific inhibitors: chelerythrine (PKC inhibitor), PP2 (Src kinase inhibitor), Batimastat (metalloprotease inhibitor), PD58059 (ERK1/2 kinase inhibitor) and SPINK6 (kallikrein family inhibitor).
Recent investigations have correlated EGF release and EGFR activation with KLK1 activity in airway epithelial cells (as mentioned in 2.4.3 [158]). The effect of kallikreins on EGFR-related signaling is very important because the basal layer of various epithelial tissues are enriched in EGFR [160, 161], and EGFR signaling has been implicated in the regulation of epithelial homeostasis and tissue repair, the release of host defense mediators, and the production of mucin [162]. KLK1 can increase the level of the active form of EGF and thus activate EGFR on basal cells (BCs) [134]. Exposure of BCs to EGF shifted the BC differentiation program toward squamous and epithelial–mesenchymal transition-like phenotypes with down-regulation of genes related to ciliogenesis and secretory differentiation, and markedly reduced junctional barrier integrity, mimicking the abnormalities present in the airways of smokers in vivo [134, 163]. This persistent BC activation via the EGF-EGFR pathway may be responsible for the progressive alteration of the airway architecture and subsequent development of tissue pathology [163]. As discussed above (see part 3.4), hyaluronic acid plays an essential role in regulating KLK1 activity, while kallikrein-mediated release of active EGF leads to tracheal submucosal gland cell hypertrophy and hyperplasia, as well as mucus hypersecretion with subsequent airflow obstruction [50]. Selective targeting of the EGF-EGFR pathway in airway BCs may be a useful strategy for preventing the development of smoking-induced lung disorders, including lung cancer [164, 165].
An alternative mechanism for the role of KLK1 in EGF signaling has been proposed by cell migration and proliferation models, using keratinocytes or prostate cancer cell lines (Fig. 3). KLK1 treatment enhances would healing in rats by inducing cell migration via direct PAR1 activation and subsequent EGFR transactivation [166, 167]. Similarly, KLK1 promoted the migration and invasion of prostate cancer cells via PAR1-dependent EGFR activation, whereas cell proliferation was stimulated via the kinin B2 receptor. These findings indicate that KLK1 stimulates signaling pathways during physiological proliferation that are different from those stimulated during cancer cell migration/invasion [166].
Analysis of urine from psoriatic patients revealed decreased levels of EGF and kallikrein in human urine [168]. This observation was confirmed by urine analysis of patients with immunoglobulin A nephropathy (IgAN), where EGF excretion is a potential predictive marker and consecutive measurements of EGF levels may provide information about disease outcome and the effect of treatment [169]. Moreover, detailed analysis of rat urine indicates that rKLK1, rKLK7 and rKLK10 (“r” denotes enzyme isoform from rat) are involved in processing of the EGF precursor in the rat submandibular gland [170].
As described previously (see chapter 2.4.5), KLK8 activity is involved in schizophrenia development possibly via proteolytic degradation of neuregulin-1, a member of the large family of EGF-like signaling molecules involved in cell–cell communication during development and disease in brain tissue (reviewed in [171]). Neuregulins transmit their signals to target cells by interacting with transmembrane tyrosine kinase receptors of the ErbB family [172]. Direct proteolysis of mature NRG-1 by KLK8 leads to co-localization of the processed NRG-1 with ErbB4 in parvalbumin-positive hippocampal interneurons and subsequent tyrosine phosphorylation of proteins in the cells [157].
3.7. Kallikreins in viral infections
Kallikreins take part in multiple physiological processes. Viral infections take advantage of the host cell machinery during multiplication and propagation of viral particles. Recent studies reveal hijacking of KLK-5, -8 and -12 in viral infections. During influenza virus replication, the critical step is proteolytic modification of the HA protein, which is responsible for fusion with the host endosome, allowing for release of the viral genome into the host cell. Kallikreins secreted in the respiratory tract are among the host proteases that support viral replication. KLK-5 and -12 exhibit HA subtype specificity, with KLK5 cleaving the H1 and H3 subtypes of influenza virus most efficiently and KLK12 preferring the H1 and H2 subtypes [173].
KLK8 is implicated in human papillomavirus turnover [54], where the major capsid protein L1 undergoes proteolytic degradation upon entry of the virus into a host cell. In addition to a dispensable cathepsin-mediated proteolysis that likely occurs after removal of capsomers from the subviral complex in endosomes, at least two further proteolytic cleavages of L1 are observed, one of which is attributed to KLK8 activity. Such an activation pattern appears to be conserved among the papillomaviruses and may aid development of novel anti-viral treatments.
4.0. Conclusion
In general, the functions of the kallikrein family of peptidases are broad. Dysregulation of KLK gene expression in malignant tissues provides insight into the importance of kallikreins in maintaining homeostasis in the human body. More problematic is the pathophysiological relevance of studies on KLKs performed at the protein level. In the vast majority of these studies, recombinant forms of KLKs with different glycosylation patterns and/or variations within the N-terminal pro-fragment were used, which may have resulted in contradictory descriptions of the enzymatic properties of individual KLKs. Despite the application of multiple high-throughput methods for the determination of the physiological targets of kallikreins, we are still far from understanding the pathophysiological functions of each kallikrein. KLKs not only seem to engage with each other within certain tissue or physiological fluids, but also seem to interact with a large variety of cell signaling factors and structural proteins. In fact, it is now well-known that dysregulation of KLK activity can lead to certain pathophysiological conditions. Consequently, inhibition of the excessive proteolytic activity of KLKs by small synthetic inhibitory compounds as well as by natural polypeptidic exogenous inhibitors might constitute a novel, challenging road under construction in cancer therapeutics. Due to structural homology of kallikreins development of highly specific inhibitory compounds targeting selected kallikrein is very difficult. Nevertheless picture emerging from results from structural modeling, biochemical assays and cell assays encourage for further investigations on compounds targeting chosen kallikrein. To date, only well-studied kallikreins, such as PSA/KLK3, have been successfully targeted for pharmacological applications such as diagnostic kits and KLK-targeting drugs [34]. Nevertheless, it is clear that KLKs are attractive and promising therapeutic targets and pharmacological effort to develop KLK-specific compounds has begun.
HIGHLIGHTS.
Kallikreins modulate broad spectrum of physiological processes.
This review describes biochemical properties of kallikreins with emphasis on post-translational modifications, such as glycosylation.
Besides physiological functions of kallikreins in human organs, we describe recent discoveries pertinent to the involvement of kallikreins in cell signaling and in viral infections.
Acknowledgements
This work was supported by funds from the Ministry of Science and Higher Education -0221/IP1/2011/71 (TK) and from the National Science Center - 2013/08/W/NZ1/00696 (JP).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Yousef GM, Diamandis EP. The new human tissue kallikrein gene family: structure, function, and association to disease. Endocr. Rev. 2001;22:184–204. doi: 10.1210/edrv.22.2.0424. [DOI] [PubMed] [Google Scholar]
- 2.Borgono CA, Diamandis EP. The emerging roles of human tissue kallikreins in cancer, Nature reviews. Cancer. 2004;4:876–890. doi: 10.1038/nrc1474. [DOI] [PubMed] [Google Scholar]
- 3.Skala W, Utzschneider DT, Magdolen V, Debela M, Guo S, Craik CS, Brandstetter H, Goettig P. Structure-function analyses of human kallikrein-related peptidase 2 establish the 99-loop as master regulator of activity. The Journal of biological chemistry. 2014;289:34267–34283. doi: 10.1074/jbc.M114.598201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Steitz TA, Shulman RG. Crystallographic and NMR studies of the serine proteases. Annual review of biophysics and bioengineering. 1982;11:419–444. doi: 10.1146/annurev.bb.11.060182.002223. [DOI] [PubMed] [Google Scholar]
- 5.Perona JJ, Craik CS. Structural basis of substrate specificity in the serine proteases. Protein science : a publication of the Protein Society. 1995;4:337–360. doi: 10.1002/pro.5560040301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gomis-Ruth FX, Bayes A, Sotiropoulou G, Pampalakis G, Tsetsenis T, Villegas V, Aviles FX, Coll M. The structure of human prokallikrein 6 reveals a novel activation mechanism for the kallikrein family. The Journal of biological chemistry. 2002;277:27273–27281. doi: 10.1074/jbc.M201534200. [DOI] [PubMed] [Google Scholar]
- 7.Goettig P, Magdolen V, Brandstetter H. Natural and synthetic inhibitors of kallikrein-related peptidases (KLKs) Biochimie. 2010;92:1546–1567. doi: 10.1016/j.biochi.2010.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yousef GM, Diamandis EP. Human tissue kallikreins: a new enzymatic cascade pathway? Biological chemistry. 2002;383:1045–1057. doi: 10.1515/BC.2002.113. [DOI] [PubMed] [Google Scholar]
- 9.Yoon H, Laxmikanthan G, Lee J, Blaber SI, Rodriguez A, Kogot JM, Scarisbrick IA, Blaber M. Activation profiles and regulatory cascades of the human kallikrein-related peptidases. The Journal of biological chemistry. 2007;282:31852–31864. doi: 10.1074/jbc.M705190200. [DOI] [PubMed] [Google Scholar]
- 10.Debela M, Magdolen V, Grimminger V, Sommerhoff C, Messerschmidt A, Huber R, Friedrich R, Bode W, Goettig P. Crystal structures of human tissue kallikrein 4: activity modulation by a specific zinc binding site. Journal of molecular biology. 2006;362:1094–1107. doi: 10.1016/j.jmb.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Debela M, Goettig P, Magdolen V, Huber R, Schechter NM, Bode W. Structural basis of the zinc inhibition of human tissue kallikrein 5. Journal of molecular biology. 2007;373:1017–1031. doi: 10.1016/j.jmb.2007.08.042. [DOI] [PubMed] [Google Scholar]
- 12.Debela M, Hess P, Magdolen V, Schechter NM, Steiner T, Huber R, Bode W, Goettig P. Chymotryptic specificity determinants in the 1.0 A structure of the zinc-inhibited human tissue kallikrein 7. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:16086–16091. doi: 10.1073/pnas.0707811104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silverman GA, Bird PI, Carrell RW, Church FC, Coughlin PB, Gettins PG, Irving JA, Lomas DA, Luke CJ, Moyer RW, Pemberton PA, Remold-O'Donnell E, Salvesen GS, Travis J, Whisstock JC. The serpins are an expanding superfamily of structurally similar but functionally diverse proteins. Evolution, mechanism of inhibition, novel functions, and a revised nomenclature. The Journal of biological chemistry. 2001;276:33293–33296. doi: 10.1074/jbc.R100016200. [DOI] [PubMed] [Google Scholar]
- 14.Luo LY, Jiang W. Inhibition profiles of human tissue kallikreins by serine protease inhibitors. Biological chemistry. 2006;387:813–816. doi: 10.1515/BC.2006.103. [DOI] [PubMed] [Google Scholar]
- 15.Schmidt EW, Rasche B, Ulmer WT, Konietzko N, Becker M, Fallise JP, Lorenz J, Ferlinz R. Replacement therapy for alpha-1-protease inhibitor deficiency in PiZ subjects with chronic obstructive lung disease. The American journal of medicine. 1988;84:63–69. doi: 10.1016/0002-9343(88)90160-x. [DOI] [PubMed] [Google Scholar]
- 16.Fischer J, Meyer-Hoffert U. Regulation of kallikrein-related peptidases in the skin - from physiology to diseases to therapeutic options. Thrombosis and haemostasis. 2013;110:442–449. doi: 10.1160/TH12-11-0836. [DOI] [PubMed] [Google Scholar]
- 17.Heiker JT, Kloting N, Kovacs P, Kuettner EB, Strater N, Schultz S, Kern M, Stumvoll M, Bluher M, Beck-Sickinger AG. Vaspin inhibits kallikrein 7 by serpin mechanism. Cellular and molecular life sciences : CMLS. 2013;70:2569–2583. doi: 10.1007/s00018-013-1258-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mavridis K, Avgeris M, Scorilas A. Targeting kallikrein-related peptidases in prostate cancer. Expert opinion on therapeutic targets. 2014;18:365–383. doi: 10.1517/14728222.2014.880693. [DOI] [PubMed] [Google Scholar]
- 19.Magert HJ, Standker L, Kreutzmann P, Zucht HD, Reinecke M, Sommerhoff CP, Fritz H, Forssmann WG. LEKTI, a novel 15-domain type of human serine proteinase inhibitor. The Journal of biological chemistry. 1999;274:21499–21502. doi: 10.1074/jbc.274.31.21499. [DOI] [PubMed] [Google Scholar]
- 20.Walley AJ, Chavanas S, Moffatt MF, Esnouf RM, Ubhi B, Lawrence R, Wong K, Abecasis GR, Jones EY, Harper JI, Hovnanian A, Cookson WO. Gene polymorphism in Netherton and common atopic disease. Nature genetics. 2001;29:175–178. doi: 10.1038/ng728. [DOI] [PubMed] [Google Scholar]
- 21.Schechter NM, Choi EJ, Wang ZM, Hanakawa Y, Stanley JR, Kang Y, Clayman GL, Jayakumar A. Inhibition of human kallikreins 5 and 7 by the serine protease inhibitor lympho-epithelial Kazal-type inhibitor (LEKTI) Biological chemistry. 2005;386:1173–1184. doi: 10.1515/BC.2005.134. [DOI] [PubMed] [Google Scholar]
- 22.Egelrud T, Brattsand M, Kreutzmann P, Walden M, Vitzithum K, Marx UC, Forssmann WG, Magert HJ. hK5 and hK7, two serine proteinases abundant in human skin, are inhibited by LEKTI domain 6. The British journal of dermatology. 2005;153:1200–1203. doi: 10.1111/j.1365-2133.2005.06834.x. [DOI] [PubMed] [Google Scholar]
- 23.Miyai M, Matsumoto Y, Yamanishi H, Yamamoto-Tanaka M, Tsuboi R, Hibino T. Keratinocyte-specific mesotrypsin contributes to the desquamation process via kallikrein activation and LEKTI degradation. The Journal of investigative dermatology. 2014;134:1665–1674. doi: 10.1038/jid.2014.3. [DOI] [PubMed] [Google Scholar]
- 24.Meyer-Hoffert U, Wu Z, Kantyka T, Fischer J, Latendorf T, Hansmann B, Bartels J, He Y, Glaser R, Schroder JM. Isolation of SPINK6 in human skin: selective inhibitor of kallikrein-related peptidases. The Journal of biological chemistry. 2010;285:32174–32181. doi: 10.1074/jbc.M109.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brattsand M, Stefansson K, Hubiche T, Nilsson SK, Egelrud T. SPINK9: a selective, skin-specific Kazal-type serine protease inhibitor. The Journal of investigative dermatology. 2009;129:1656–1665. doi: 10.1038/jid.2008.448. [DOI] [PubMed] [Google Scholar]
- 26.Sperrhacke M, Fischer J, Wu Z, Klunder S, Sedlacek R, Schroeder JM, Meyer-Hoffert U, Reiss K. SPINK9 stimulates metalloprotease/EGFR-dependent keratinocyte migration via purinergic receptor activation. The Journal of investigative dermatology. 2014;134:1645–1654. doi: 10.1038/jid.2014.23. [DOI] [PubMed] [Google Scholar]
- 27.Kantyka T, Fischer J, Wu Z, Declercq W, Reiss K, Schroder JM, Meyer-Hoffert U. Inhibition of kallikrein-related peptidases by the serine protease inhibitor of Kazal-type 6. Peptides. 2011;32:1187–1192. doi: 10.1016/j.peptides.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 28.Fischer J, Koblyakova Y, Latendorf T, Wu Z, Meyer-Hoffert U. Cross-linking of SPINK6 by transglutaminases protects from epidermal proteases. The Journal of investigative dermatology. 2013;133:1170–1177. doi: 10.1038/jid.2012.482. [DOI] [PubMed] [Google Scholar]
- 29.Kenniston JA, Faucette RR, Martik D, Comeau SR, Lindberg AP, Kopacz KJ, Conley GP, Chen J, Viswanathan M, Kastrapeli N, Cosic J, Mason S, DiLeo M, Abendroth J, Kuzmic P, Ladner RC, Edwards TE, TenHoor C, Adelman BA, Nixon AE, Sexton DJ. Inhibition of plasma kallikrein by a highly specific active site blocking antibody. The Journal of biological chemistry. 2014;289:23596–23608. doi: 10.1074/jbc.M114.569061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kapadia C, Chang A, Sotiropoulou G, Yousef GM, Grass L, Soosaipillai A, Xing X, Howarth DH, Diamandis EP. Human kallikrein 13: production and purification of recombinant protein and monoclonal and polyclonal antibodies, and development of a sensitive and specific immunofluorometric assay. Clinical chemistry. 2003;49:77–86. doi: 10.1373/49.1.77. [DOI] [PubMed] [Google Scholar]
- 31.Cereda V, Formica V, Menghi A, Pellicori S, Roselli M. Kallikrein-related peptidases targeted therapies in prostate cancer: perspectives and challenges. Expert opinion on investigational drugs. 2015;24:929–947. doi: 10.1517/13543784.2015.1035708. [DOI] [PubMed] [Google Scholar]
- 32.Arama DP, Soualmia F, Lisowski V, Longevial JF, Bosc E, Maillard LT, Martinez J, Masurier N, El Amri C. Pyrido-imidazodiazepinones as a new class of reversible inhibitors of human kallikrein 7. European journal of medicinal chemistry. 2015;93:202–213. doi: 10.1016/j.ejmech.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 33.Tan X, Soualmia F, Furio L, Renard JF, Kempen I, Qin L, Pagano M, Pirotte B, El Amri C, Hovnanian A, Reboud-Ravaux M. Toward the first class of suicide inhibitors of kallikreins involved in skin diseases. Journal of medicinal chemistry. 2015;58:598–612. doi: 10.1021/jm500988d. [DOI] [PubMed] [Google Scholar]
- 34.Prassas I, Eissa A, Poda G, Diamandis EP. Unleashing the therapeutic potential of human kallikrein-related serine proteases, Nature reviews. Drug discovery. 2015;14:183–202. doi: 10.1038/nrd4534. [DOI] [PubMed] [Google Scholar]
- 35.Marques RB, Aghai A, de Ridder CM, Stuurman D, Hoeben S, Boer A, Ellston RP, Barry ST, Davies BR, Trapman J, van Weerden WM. High Efficacy of Combination Therapy Using PI3K/AKT Inhibitors with Androgen Deprivation in Prostate Cancer Preclinical Models. European urology. 2015;67:1177–1185. doi: 10.1016/j.eururo.2014.08.053. [DOI] [PubMed] [Google Scholar]
- 36.Guo S, Skala W, Magdolen V, Brandstetter H, Goettig P. Sweetened kallikrein-related peptidases (KLKs): glycan trees as potential regulators of activation and activity. Biological chemistry. 2014;395:959–976. doi: 10.1515/hsz-2014-0140. [DOI] [PubMed] [Google Scholar]
- 37.Shibata K, Kajihara J, Kato K, Hirano K. Purification and characterization of prostate specific antigen from human urine. Biochimica et biophysica acta. 1997;1336:425–433. doi: 10.1016/s0304-4165(97)00055-x. [DOI] [PubMed] [Google Scholar]
- 38.Takayama TK, Fujikawa K, Davie EW. Characterization of the precursor of prostate-specific antigen. Activation by trypsin and by human glandular kallikrein. J. Biol. Chem. 1997;272:21582–21588. doi: 10.1074/jbc.272.34.21582. [DOI] [PubMed] [Google Scholar]
- 39.Coombs GS. Substrate specificity of prostate-specific antigen (PSA) Chem. Biol. 1998;5:475–488. doi: 10.1016/s1074-5521(98)90004-7. [DOI] [PubMed] [Google Scholar]
- 40.Debela M, Magdolen V, Schechter N, Valachova M, Lottspeich F, Craik CS, Choe Y, Bode W, Goettig P. Specificity profiling of seven human tissue kallikreins reveals individual subsite preferences. The Journal of biological chemistry. 2006;281:25678–25688. doi: 10.1074/jbc.M602372200. [DOI] [PubMed] [Google Scholar]
- 41.Menez R, Michel S, Muller BH, Bossus M, Ducancel F, Jolivet-Reynaud C, Stura EA. Crystal structure of a ternary complex between human prostate-specific antigen, its substrate acyl intermediate and an activating antibody. Journal of molecular biology. 2008;376:1021–1033. doi: 10.1016/j.jmb.2007.11.052. [DOI] [PubMed] [Google Scholar]
- 42.Stura EA, Muller BH, Bossus M, Michel S, Jolivet-Reynaud C, Ducancel F. Crystal structure of human prostate-specific antigen in a sandwich antibody complex. Journal of molecular biology. 2011;414:530–544. doi: 10.1016/j.jmb.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 43.Vermassen T, Speeckaert MM, Lumen N, Rottey S, Delanghe JR. Glycosylation of prostate specific antigen and its potential diagnostic applications. Clinica chimica acta; international journal of clinical chemistry. 2012;413:1500–1505. doi: 10.1016/j.cca.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 44.Gilgunn S, Conroy PJ, Saldova R, Rudd PM, O'Kennedy RJ. Aberrant PSA glycosylation--a sweet predictor of prostate cancer, Nature reviews. Urology. 2013;10:99–107. doi: 10.1038/nrurol.2012.258. [DOI] [PubMed] [Google Scholar]
- 45.Behnken HN, Ruthenbeck A, Schulz JM, Meyer B. Glycan analysis of Prostate Specific Antigen (PSA) directly from the intact glycoprotein by HR-ESI/TOF-MS. Journal of proteome research. 2014;13:997–1001. doi: 10.1021/pr400999y. [DOI] [PubMed] [Google Scholar]
- 46.Barak M, Mecz Y, Lurie A, Gruener N. Evaluation of prostate-specific antigen as a marker for adenocarcinoma of the prostate. The Journal of laboratory and clinical medicine. 1989;113:598–603. [PubMed] [Google Scholar]
- 47.Kuzmanov U, Jiang N, Smith CR, Soosaipillai A, Diamandis EP. Differential N-glycosylation of kallikrein 6 derived from ovarian cancer cells or the central nervous system. Molecular & cellular proteomics : MCP. 2009;8:791–798. doi: 10.1074/mcp.M800516-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kuzmanov U, Smith CR, Batruch I, Soosaipillai A, Diamandis A, Diamandis EP. Separation of kallikrein 6 glycoprotein subpopulations in biological fluids by anion-exchange chromatography coupled to ELISA and identification by mass spectrometry. Proteomics. 2012;12:799–809. doi: 10.1002/pmic.201100371. [DOI] [PubMed] [Google Scholar]
- 49.Forteza R, Casalino-Matsuda SM, Monzon ME, Fries E, Rugg MS, Milner CM, Day AJ. TSG-6 potentiates the antitissue kallikrein activity of inter-alpha-inhibitor through bikunin release. American journal of respiratory cell and molecular biology. 2007;36:20–31. doi: 10.1165/rcmb.2006-0018OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Casalino-Matsuda SM, Monzon ME, Conner GE, Salathe M, Forteza RM. Role of hyaluronan and reactive oxygen species in tissue kallikrein-mediated epidermal growth factor receptor activation in human airways. The Journal of biological chemistry. 2004;279:21606–21616. doi: 10.1074/jbc.M309950200. [DOI] [PubMed] [Google Scholar]
- 51.Angelo PF, Lima AR, Alves FM, Blaber SI, Scarisbrick IA, Blaber M, Juliano L, Juliano MA. Substrate specificity of human kallikrein 6: salt and glycosaminoglycan activation effects. The Journal of biological chemistry. 2006;281:3116–3126. doi: 10.1074/jbc.M510096200. [DOI] [PubMed] [Google Scholar]
- 52.Andrade D, Assis DM, Santos JA, Alves FM, Hirata IY, Araujo MS, Blaber SI, Blaber M, Juliano MA, Juliano L. Substrate specificity of kallikrein-related peptidase 13 activated by salts or glycosaminoglycans and a search for natural substrate candidates. Biochimie. 2011;93:1701–1709. doi: 10.1016/j.biochi.2011.05.037. [DOI] [PubMed] [Google Scholar]
- 53.Oliveira JR, Bertolin TC, Andrade D, Oliveira LC, Kondo MY, Santos JA, Blaber M, Juliano L, Severino B, Caliendo G, Santagada V, Juliano MA. Specificity studies on Kallikrein-related peptidase 7 (KLK7) and effects of osmolytes and glycosaminoglycans on its peptidase activity. Biochimica et biophysica acta. 2015;1854:73–83. doi: 10.1016/j.bbapap.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 54.Cerqueira C, Samperio Ventayol P, Vogeley C, Schelhaas M. Kallikrein-8 Proteolytically Processes Human Papillomaviruses in the Extracellular Space To Facilitate Entry into Host Cells. Journal of virology. 2015;89:7038–7052. doi: 10.1128/JVI.00234-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mycielska ME, Patel A, Rizaner N, Mazurek MP, Keun H, Patel A, Ganapathy V, Djamgoz MB. Citrate transport and metabolism in mammalian cells: prostate epithelial cells and prostate cancer. BioEssays : news and reviews in molecular, cellular and developmental biology. 2009;31:10–20. doi: 10.1002/bies.080137. [DOI] [PubMed] [Google Scholar]
- 56.Shaw JL, Diamandis EP. Distribution of 15 human kallikreins in tissues and biological fluids. Clinical chemistry. 2007;53:1423–1432. doi: 10.1373/clinchem.2007.088104. [DOI] [PubMed] [Google Scholar]
- 57.Perona JJ, Craik CS. Evolutionary divergence of substrate specificity within the chymotrypsin-like serine protease fold. The Journal of biological chemistry. 1997;272:29987–29990. doi: 10.1074/jbc.272.48.29987. [DOI] [PubMed] [Google Scholar]
- 58.Laxmikanthan G, Blaber SI, Bernett MJ, Scarisbrick IA, Juliano MA, Blaber M. 1.70 A X-ray structure of human apo kallikrein 1: structural changes upon peptide inhibitor/substrate binding. Proteins. 2005;58:802–814. doi: 10.1002/prot.20368. [DOI] [PubMed] [Google Scholar]
- 59.Magklara A, Mellati AA, Wasney GA, Little SP, Sotiropoulou G, Becker GW, Diamandis EP. Characterization of the enzymatic activity of human kallikrein 6: Autoactivation, substrate specificity, and regulation by inhibitors. Biochemical and biophysical research communications. 2003;307:948–955. doi: 10.1016/s0006-291x(03)01271-3. [DOI] [PubMed] [Google Scholar]
- 60.Debela M, Beaufort N, Magdolen V, Schechter NM, Craik CS, Schmitt M, Bode W, Goettig P. Structures and specificity of the human kallikrein-related peptidases KLK 4, 5, 6, and 7. Biological chemistry. 2008;389:623–632. doi: 10.1515/BC.2008.075. [DOI] [PubMed] [Google Scholar]
- 61.Yu Y, Prassas I, Diamandis EP. Putative kallikrein substrates and their (patho)biological functions. Biological chemistry. 2014;395:931–943. doi: 10.1515/hsz-2014-0129. [DOI] [PubMed] [Google Scholar]
- 62.Doucet A, Overall CM. Protease proteomics: revealing protease in vivo functions using systems biology approaches. Molecular aspects of medicine. 2008;29:339–358. doi: 10.1016/j.mam.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 63.Krishnaswamy S. Exosite-driven substrate specificity and function in coagulation. Journal of thrombosis and haemostasis : JTH. 2005;3:54–67. doi: 10.1111/j.1538-7836.2004.01021.x. [DOI] [PubMed] [Google Scholar]
- 64.Guillon-Munos A, Oikonomopoulou K, Michel N, Smith CR, Petit-Courty A, Canepa S, Reverdiau P, Heuze-Vourc'h N, Diamandis EP, Courty Y. Kallikrein-related peptidase 12 hydrolyzes matricellular proteins of the CCN family and modifies interactions of CCN1 and CCN5 with growth factors. The Journal of biological chemistry. 2011;286:25505–25518. doi: 10.1074/jbc.M110.213231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mattsson JM, Ravela S, Hekim C, Jonsson M, Malm J, Narvanen A, Stenman UH, Koistinen H. Proteolytic activity of prostate-specific antigen (PSA) towards protein substrates and effect of peptides stimulating PSA activity. PloS one. 2014;9:e107819. doi: 10.1371/journal.pone.0107819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yu Y, Prassas I, Dimitromanolakis A, Diamandis EP. Novel Biological Substrates of Human Kallikrein 7 Identified Through Degradomics. The Journal of biological chemistry. 2015 doi: 10.1074/jbc.M115.643551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cloutier SM. Substrate specificity of human kallikrein 2 (hK2) as determined by phage display technology. Eur. J. Biochem. 2002;269:2747–2754. doi: 10.1046/j.1432-1033.2002.02960.x. [DOI] [PubMed] [Google Scholar]
- 68.Denmeade SR. Specific and efficient peptide substrates for assaying the proteolytic activity of prostate-specific antigen. Cancer Res. 1997;57:4924–4930. [PMC free article] [PubMed] [Google Scholar]
- 69.Malm J, Hellman J, Hogg P, Lilja H. Enzymatic action of prostate-specific antigen (PSA or hK3): substrate specificity and regulation by Zn2+, a tight-binding inhibitor. The Prostate. 2000;45:132–139. doi: 10.1002/1097-0045(20001001)45:2<132::aid-pros7>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 70.Matsumura M, Bhatt AS, Andress D, Clegg N, Takayama TK, Craik CS, Nelson PS. Substrates of the prostate-specific serine protease prostase/KLK4 defined by positional-scanning peptide libraries. The Prostate. 2005;62:1–13. doi: 10.1002/pros.20101. [DOI] [PubMed] [Google Scholar]
- 71.Shimizu C, Yoshida S, Shibata M, Kato K, Momota Y, Matsumoto K, Shiosaka T, Midorikawa R, Kamachi T, Kawabe A, Shiosaka S. Characterization of recombinant and brain neuropsin, a plasticity-related serine protease. The Journal of biological chemistry. 1998;273:11189–11196. doi: 10.1074/jbc.273.18.11189. [DOI] [PubMed] [Google Scholar]
- 72.Yamada A, Nakamura Y, Sugita D, Shirosaki S, Ohkuri T, Katsukawa H, Nonaka K, Imoto T, Ninomiya Y. Induction of salivary kallikreins by the diet containing a sweet-suppressive peptide, gurmarin, in the rat. Biochemical and biophysical research communications. 2006;346:386–392. doi: 10.1016/j.bbrc.2006.05.154. [DOI] [PubMed] [Google Scholar]
- 73.Luo LY, Shan SJ, Elliott MB, Soosaipillai A, Diamandis EP. Purification and characterization of human kallikrein 11, a candidate prostate and ovarian cancer biomarker, from seminal plasma. Clinical cancer research : an official journal of the American Association for Cancer Research. 2006;12:742–750. doi: 10.1158/1078-0432.CCR-05-1696. [DOI] [PubMed] [Google Scholar]
- 74.Borgono CA, Gavigan JA, Alves J, Bowles B, Harris JL, Sotiropoulou G, Diamandis EP. Defining the extended substrate specificity of kallikrein 1-related peptidases. Biological chemistry. 2007;388:1215–1225. doi: 10.1515/BC.2007.124. [DOI] [PubMed] [Google Scholar]
- 75.Borgono CA, Michael IP, Shaw JL, Luo LY, Ghosh MC, Soosaipillai A, Grass L, Katsaros D, Diamandis EP. Expression and functional characterization of the cancer-related serine protease, human tissue kallikrein 14. The Journal of biological chemistry. 2007;282:2405–2422. doi: 10.1074/jbc.M608348200. [DOI] [PubMed] [Google Scholar]
- 76.Takayama TK, Carter CA, Deng T. Activation of prostate-specific antigen precursor (pro-PSA) by prostin, a novel human prostatic serine protease identified by degenerate PCR. Biochemistry. 2001;40:1679–1687. doi: 10.1021/bi002129r. [DOI] [PubMed] [Google Scholar]
- 77.Emami N, Diamandis EP. New insights into the functional mechanisms and clinical applications of the kallikrein-related peptidase family. Molecular oncology. 2007;1:269–287. doi: 10.1016/j.molonc.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ekholm IE, Brattsand M, Egelrud T. Stratum corneum tryptic enzyme in normal epidermis: a missing link in the desquamation process? The Journal of investigative dermatology. 2000;114:56–63. doi: 10.1046/j.1523-1747.2000.00820.x. [DOI] [PubMed] [Google Scholar]
- 79.Lundstrom A, Egelrud T. Stratum corneum chymotryptic enzyme: a proteinase which may be generally present in the stratum corneum and with a possible involvement in desquamation. Acta dermato-venereologica. 1991;71:471–474. [PubMed] [Google Scholar]
- 80.Egelrud T. Desquamation in the stratum corneum, Acta dermato-venereologica. Supplementum. 2000;208:44–45. doi: 10.1080/000155500750012513. [DOI] [PubMed] [Google Scholar]
- 81.Lundwall A, Brattsand M. Kallikrein-related peptidases. Cellular and molecular life sciences : CMLS. 2008;65:2019–2038. doi: 10.1007/s00018-008-8024-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nylander-Lundqvist E, Back O, Egelrud T. IL-1 beta activation in human epidermis. Journal of immunology. 1996;157:1699–1704. [PubMed] [Google Scholar]
- 83.Yao C, Karabasil MR, Purwanti N, Li X, Akamatsu T, Kanamori N, Hosoi K. Tissue kallikrein mK13 is a candidate processing enzyme for the precursor of interleukin-1beta in the submandibular gland of mice. The Journal of biological chemistry. 2006;281:7968–7976. doi: 10.1074/jbc.M507705200. [DOI] [PubMed] [Google Scholar]
- 84.Yamasaki K, Schauber J, Coda A, Lin H, Dorschner RA, Schechter NM, Bonnart C, Descargues P, Hovnanian A, Gallo RL. Kallikrein-mediated proteolysis regulates the antimicrobial effects of cathelicidins in skin. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2006;20:2068–2080. doi: 10.1096/fj.06-6075com. [DOI] [PubMed] [Google Scholar]
- 85.Yamasaki K, Di Nardo A, Bardan A, Murakami M, Ohtake T, Coda A, Dorschner RA, Bonnart C, Descargues P, Hovnanian A, Morhenn VB, Gallo RL. Increased serine protease activity and cathelicidin promotes skin inflammation in rosacea. Nature medicine. 2007;13:975–980. doi: 10.1038/nm1616. [DOI] [PubMed] [Google Scholar]
- 86.Meyer-Hoffert U, Schroder JM. Epidermal proteases in the pathogenesis of rosacea. The journal of investigative dermatology. Symposium proceedings / the Society for Investigative Dermatology, Inc. [and] European Society for Dermatological Research. 2011;15:16–23. doi: 10.1038/jidsymp.2011.2. [DOI] [PubMed] [Google Scholar]
- 87.Furio L, de Veer S, Jaillet M, Briot A, Robin A, Deraison C, Hovnanian A. Transgenic kallikrein 5 mice reproduce major cutaneous and systemic hallmarks of Netherton syndrome. The Journal of experimental medicine. 2014;211:499–513. doi: 10.1084/jem.20131797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hansson L, Backman A, Ny A, Edlund M, Ekholm E, Ekstrand Hammarstrom B, Tornell J, Wallbrandt P, Wennbo H, Egelrud T. Epidermal overexpression of stratum corneum chymotryptic enzyme in mice: a model for chronic itchy dermatitis. The Journal of investigative dermatology. 2002;118:444–449. doi: 10.1046/j.0022-202x.2001.01684.x. [DOI] [PubMed] [Google Scholar]
- 89.Eissa A, Amodeo V, Smith CR, Diamandis EP. Kallikrein-related peptidase-8 (KLK8) is an active serine protease in human epidermis and sweat and is involved in a skin barrier proteolytic cascade. The Journal of biological chemistry. 2011;286:687–706. doi: 10.1074/jbc.M110.125310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kasetty G, Papareddy P, Kalle M, Rydengard V, Walse B, Svensson B, Morgelin M, Malmsten M, Schmidtchen A. The C-terminal sequence of several human serine proteases encodes host defense functions. Journal of innate immunity. 2011;3:471–482. doi: 10.1159/000327016. [DOI] [PubMed] [Google Scholar]
- 91.Bartlett JD. Dental enamel development: proteinases and their enamel matrix substrates. ISRN dentistry. 2013;2013:684607. doi: 10.1155/2013/684607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Simmer JP, Fukae M, Tanabe T, Yamakoshi Y, Uchida T, Xue J, Margolis HC, Shimizu M, DeHart BC, Hu CC, Bartlett JD. Purification, characterization, and cloning of enamel matrix serine proteinase 1. Journal of dental research. 1998;77:377–386. doi: 10.1177/00220345980770020601. [DOI] [PubMed] [Google Scholar]
- 93.Cho A, Haruyama N, Hall B, Danton MJ, Zhang L, Arany P, Mooney DJ, Harichane Y, Goldberg M, Gibson CW, Kulkarni AB. TGF-ss regulates enamel mineralization and maturation through KLK4 expression. PloS one. 2013;8:e82267. doi: 10.1371/journal.pone.0082267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hart PS, Hart TC, Michalec MD, Ryu OH, Simmons D, Hong S, Wright JT. Mutation in kallikrein 4 causes autosomal recessive hypomaturation amelogenesis imperfecta. Journal of medical genetics. 2004;41:545–549. doi: 10.1136/jmg.2003.017657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wang SK, Hu Y, Simmer JP, Seymen F, Estrella NM, Pal S, Reid BM, Yildirim M, Bayram M, Bartlett JD, Hu JC. Novel KLK4 and MMP20 mutations discovered by whole-exome sequencing. Journal of dental research. 2013;92:266–271. doi: 10.1177/0022034513475626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Papagerakis P, Pannone G, Zheng LI, Athanassiou-Papaefthymiou M, Yamakoshi Y, McGuff HS, Shkeir O, Ghirtis K, Papagerakis S. Clinical significance of kallikrein-related peptidase-4 in oral cancer. Anticancer research. 2015;35:1861–1866. [PMC free article] [PubMed] [Google Scholar]
- 97.Becker C, Noldus J, Diamandis E, Lilja H. The role of molecular forms of prostate-specific antigen (PSA or hK3) and of human glandular kallikrein 2 (hK2) in the diagnosis and monitoring of prostate cancer and in extra-prostatic disease. Critical reviews in clinical laboratory sciences. 2001;38:357–399. doi: 10.1080/20014091084236. [DOI] [PubMed] [Google Scholar]
- 98.Ilic D, Neuberger MM, Djulbegovic M, Dahm P. Screening for prostate cancer. The Cochrane database of systematic reviews. 2013;1:CD004720. doi: 10.1002/14651858.CD004720.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Pampalakis G, Sotiropoulou G. Tissue kallikrein proteolytic cascade pathways in normal physiology and cancer. Biochimica et biophysica acta. 2007;1776:22–31. doi: 10.1016/j.bbcan.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 100.Laflamme BA, Wolfner MF. Identification and function of proteolysis regulators in seminal fluid. Molecular reproduction and development. 2013;80:80–101. doi: 10.1002/mrd.22130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Partin AW, Catalona WJ, Finlay JA, Darte C, Tindall DJ, Young CY, Klee GG, Chan DW, Rittenhouse HG, Wolfert RL, Woodrum DL. Use of human glandular kallikrein 2 for the detection of prostate cancer: preliminary analysis. Urology. 1999;54:839–845. doi: 10.1016/s0090-4295(99)00270-8. [DOI] [PubMed] [Google Scholar]
- 102.Nam RK, Diamandis EP, Toi A, Trachtenberg J, Magklara A, Scorilas A, Papnastasiou PA, Jewett MA, Narod SA. Serum human glandular kallikrein-2 protease levels predict the presence of prostate cancer among men with elevated prostate-specific antigen. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2000;18:1036–1042. doi: 10.1200/JCO.2000.18.5.1036. [DOI] [PubMed] [Google Scholar]
- 103.Shang Z, Niu Y, Cai Q, Chen J, Tian J, Yeh S, Lai KP, Chang C. Human kallikrein 2 (KLK2) promotes prostate cancer cell growth via function as a modulator to promote the ARA70-enhanced androgen receptor transactivation. Tumour biology : the journal of the International Society for Oncodevelopmental Biology and Medicine. 2014;35:1881–1890. doi: 10.1007/s13277-013-1253-6. [DOI] [PubMed] [Google Scholar]
- 104.Avgeris M, Stravodimos K, Scorilas A. Kallikrein-related peptidase 4 gene (KLK4) in prostate tumors: quantitative expression analysis and evaluation of its clinical significance. The Prostate. 2011;71:1780–1789. doi: 10.1002/pros.21395. [DOI] [PubMed] [Google Scholar]
- 105.Logothetis CJ, Lin SH. Osteoblasts in prostate cancer metastasis to bone, Nature reviews. Cancer. 2005;5:21–28. doi: 10.1038/nrc1528. [DOI] [PubMed] [Google Scholar]
- 106.Gao J, Collard RL, Bui L, Herington AC, Nicol DL, Clements JA. Kallikrein 4 is a potential mediator of cellular interactions between cancer cells and osteoblasts in metastatic prostate cancer. The Prostate. 2007;67:348–360. doi: 10.1002/pros.20465. [DOI] [PubMed] [Google Scholar]
- 107.Lawrence MG, Lai J, Clements JA. Kallikreins on steroids: structure, function, and hormonal regulation of prostate-specific antigen and the extended kallikrein locus. Endocrine reviews. 2010;31:407–446. doi: 10.1210/er.2009-0034. [DOI] [PubMed] [Google Scholar]
- 108.Hakalahti L, Vihko P, Henttu P, Autio-Harmainen H, Soini Y, Vihko R. Evaluation of PAP and PSA gene expression in prostatic hyperplasia and prostatic carcinoma using northern-blot analyses, in situ hybridization and immunohistochemical stainings with monoclonal and bispecific antibodies. International journal of cancer. Journal international du cancer. 1993;55:590–597. doi: 10.1002/ijc.2910550413. [DOI] [PubMed] [Google Scholar]
- 109.Luo LY, Rajpert-De Meyts ER, Jung K, Diamandis EP. Expression of the normal epithelial cell-specific 1 (NES1; KLK10) candidate tumour suppressor gene in normal and malignant testicular tissue. British journal of cancer. 2001;85:220–224. doi: 10.1054/bjoc.2001.1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Pretlow TG, Pretlow TP, Yang B, Kaetzel CS, Delmoro CM, Kamis SM, Bodner DR, Kursh E, Resnick MI, Bradley EL., Jr Tissue concentrations of prostate-specific antigen in prostatic carcinoma and benign prostatic hyperplasia. International journal of cancer. Journal international du cancer. 1991;49:645–649. doi: 10.1002/ijc.2910490503. [DOI] [PubMed] [Google Scholar]
- 111.Yousef GM, Yacoub GM, Polymeris ME, Popalis C, Soosaipillai A, Diamandis EP. Kallikrein gene downregulation in breast cancer. British journal of cancer. 2004;90:167–172. doi: 10.1038/sj.bjc.6601451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yu H, Diamandis EP, Levesque M, Giai M, Roagna R, Ponzone R, Sismondi P, Monne M, Croce CM. Prostate specific antigen in breast cancer, benign breast disease and normal breast tissue. Breast cancer research and treatment. 1996;40:171–178. doi: 10.1007/BF01806212. [DOI] [PubMed] [Google Scholar]
- 113.Borgono CA, Grass L, Soosaipillai A, Yousef GM, Petraki CD, Howarth DH, Fracchioli S, Katsaros D, Diamandis EP. Human kallikrein 14: a new potential biomarker for ovarian and breast cancer. Cancer research. 2003;63:9032–9041. [PubMed] [Google Scholar]
- 114.Diamandis EP, Okui A, Mitsui S, Luo LY, Soosaipillai A, Grass L, Nakamura T, Howarth DJ, Yamaguchi N. Human kallikrein 11: a new biomarker of prostate and ovarian carcinoma. Cancer research. 2002;62:295–300. [PubMed] [Google Scholar]
- 115.Dong Y, Kaushal A, Bui L, Chu S, Fuller PJ, Nicklin J, Samaratunga H, Clements JA. Human kallikrein 4 (KLK4) is highly expressed in serous ovarian carcinomas. Clinical cancer research : an official journal of the American Association for Cancer Research. 2001;7:2363–2371. [PubMed] [Google Scholar]
- 116.Kim H, Scorilas A, Katsaros D, Yousef GM, Massobrio M, Fracchioli S, Piccinno R, Gordini G, Diamandis EP. Human kallikrein gene 5 (KLK5) expression is an indicator of poor prognosis in ovarian cancer. British journal of cancer. 2001;84:643–650. doi: 10.1054/bjoc.2000.1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kishi T, Grass L, Soosaipillai A, Scorilas A, Harbeck N, Schmalfeldt B, Dorn J, Mysliwiec M, Schmitt M, Diamandis EP. Human kallikrein 8, a novel biomarker for ovarian carcinoma. Cancer research. 2003;63:2771–2774. [PubMed] [Google Scholar]
- 118.Luo LY, Bunting P, Scorilas A, Diamandis EP. Human kallikrein 10: a novel tumor marker for ovarian carcinoma? Clinica chimica acta; international journal of clinical chemistry. 2001;306:111–118. doi: 10.1016/s0009-8981(01)00401-6. [DOI] [PubMed] [Google Scholar]
- 119.Luo LY, Katsaros D, Scorilas A, Fracchioli S, Bellino R, van Gramberen M, de Bruijn H, Henrik A, Stenman UH, Massobrio M, van der Zee AG, Vergote I, Diamandis EP. The serum concentration of human kallikrein 10 represents a novel biomarker for ovarian cancer diagnosis and prognosis. Cancer research. 2003;63:807–811. [PubMed] [Google Scholar]
- 120.Magklara A, Scorilas A, Katsaros D, Massobrio M, Yousef GM, Fracchioli S, Danese S, Diamandis EP. The human KLK8 (neuropsin/ovasin) gene: identification of two novel splice variants and its prognostic value in ovarian cancer. Clinical cancer research : an official journal of the American Association for Cancer Research. 2001;7:806–811. [PubMed] [Google Scholar]
- 121.Obiezu CV, Soosaipillai A, Jung K, Stephan C, Scorilas A, Howarth DH, Diamandis EP. Detection of human kallikrein 4 in healthy and cancerous prostatic tissues by immunofluorometry and immunohistochemistry. Clinical chemistry. 2002;48:1232–1240. [PubMed] [Google Scholar]
- 122.Tanimoto H, Underwood LJ, Shigemasa K, Yan Yan MS, Clarke J, Parmley TH, O'Brien TJ. The stratum corneum chymotryptic enzyme that mediates shedding and desquamation of skin cells is highly overexpressed in ovarian tumor cells. Cancer. 1999;86:2074–2082. [PubMed] [Google Scholar]
- 123.Underwood LJ, Tanimoto H, Wang Y, Shigemasa K, Parmley TH, O'Brien TJ, et al. Cloning of tumor-associated differentially expressed gene-14, a novel serine protease overexpressed by ovarian carcinoma. Cancer research. 1999;59:4435–4439. [PubMed] [Google Scholar]
- 124.Welsh JB, Sapinoso LM, Kern SG, Brown DA, Liu T, Bauskin AR, Ward RL, Hawkins NJ, Quinn DI, Russell PJ, Sutherland RL, Breit SN, Moskaluk CA, Frierson HF, Jr, Hampton GM. Large-scale delineation of secreted protein biomarkers overexpressed in cancer tissue and serum. Proceedings of the National Academy of Sciences of the United States of America. 2003;100:3410–3415. doi: 10.1073/pnas.0530278100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Yousef GM, Polymeris ME, Grass L, Soosaipillai A, Chan PC, Scorilas A, Borgono C, Harbeck N, Schmalfeldt B, Dorn J, Schmitt M, Diamandis EP. Human kallikrein 5: a potential novel serum biomarker for breast and ovarian cancer. Cancer research. 2003;63:3958–3965. [PubMed] [Google Scholar]
- 126.Yousef GM, Polymeris ME, Yacoub GM, Scorilas A, Soosaipillai A, Popalis C, Fracchioli S, Katsaros D, Diamandis EP. Parallel overexpression of seven kallikrein genes in ovarian cancer. Cancer research. 2003;63:2223–2227. [PubMed] [Google Scholar]
- 127.Yousef GM, Scorilas A, Katsaros D, Fracchioli S, Iskander L, Borgono C, Rigault de la Longrais IA, Puopolo M, Massobrio M, Diamandis EP. Prognostic value of the human kallikrein gene 15 expression in ovarian cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2003;21:3119–3126. doi: 10.1200/JCO.2003.09.111. [DOI] [PubMed] [Google Scholar]
- 128.Paliouras M, Diamandis EP. Coordinated steroid hormone-dependent and independent expression of multiple kallikreins in breast cancer cell lines. Breast cancer research and treatment. 2007;102:7–18. doi: 10.1007/s10549-006-9312-y. [DOI] [PubMed] [Google Scholar]
- 129.Giusti B, Serrati S, Margheri F, Papucci L, Rossi L, Poggi F, Magi A, Del Rosso A, Cinelli M, Guiducci S, Kahaleh B, Matucci-Cerinic M, Abbate R, Fibbi G, Del Rosso M. The antiangiogenic tissue kallikrein pattern of endothelial cells in systemic sclerosis. Arthritis and rheumatism. 2005;52:3618–3628. doi: 10.1002/art.21383. [DOI] [PubMed] [Google Scholar]
- 130.Kryza T, Lalmanach G, Lavergne M, Lecaille F, Reverdiau P, Courty Y, Heuze-Vourc'h N. Pro-angiogenic effect of human kallikrein-related peptidase 12 (KLK12) in lung endothelial cells does not depend on kinin-mediated activation of B2 receptor. Biological chemistry. 2013;394:385–391. doi: 10.1515/hsz-2012-0291. [DOI] [PubMed] [Google Scholar]
- 131.Betsholtz C, Lindblom P, Bjarnegard M, Enge M, Gerhardt H, Lindahl P. Role of platelet-derived growth factor in mesangium development and vasculopathies: lessons from platelet-derived growth factor and platelet-derived growth factor receptor mutations in mice. Current opinion in nephrology and hypertension. 2004;13:45–52. doi: 10.1097/00041552-200401000-00007. [DOI] [PubMed] [Google Scholar]
- 132.Christiansen SC, Proud D, Cochrane CG. Detection of tissue kallikrein in the bronchoalveolar lavage fluid of asthmatic subjects. The Journal of clinical investigation. 1987;79:188–197. doi: 10.1172/JCI112782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Casalino-Matsuda SM, Monzon ME, Forteza RM. Epidermal growth factor receptor activation by epidermal growth factor mediates oxidant-induced goblet cell metaplasia in human airway epithelium. American journal of respiratory cell and molecular biology. 2006;34:581–591. doi: 10.1165/rcmb.2005-0386OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Shaykhiev R, Zuo WL, Chao I, Fukui T, Witover B, Brekman A, Crystal RG. EGF shifts human airway basal cell fate toward a smoking-associated airway epithelial phenotype. Proceedings of the National Academy of Sciences of the United States of America. 2013;110:12102–12107. doi: 10.1073/pnas.1303058110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Charest-Morin X, Raghavan A, Charles ML, Kolodka T, Bouthillier J, Jean M, Robbins MS, Marceau F. Pharmacological effects of recombinant human tissue kallikrein on bradykinin B2 receptors. Pharmacology research & perspectives. 2015;3:e00119. doi: 10.1002/prp2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Igic R, Skrbic R. The renin-angiotensin system and its blockers. Srpski arhiv za celokupno lekarstvo. 2014;142:756–763. doi: 10.2298/sarh1412756i. [DOI] [PubMed] [Google Scholar]
- 137.Sharma JN, Narayanan P. The kallikrein-kinin pathways in hypertension and diabetes, Progress in drug research. Fortschritte der Arzneimittelforschung. Progres des recherches pharmaceutiques. 2014;69:15–36. [PubMed] [Google Scholar]
- 138.Lieb W, Chen MH, Teumer A, de Boer RA, Lin H, Fox ER, Musani SK, Wilson JG, Wang TJ, Volzke H, Petersen AK, Meisinger C, Nauck M, Schlesinger S, Li Y, Menard J, Hercberg S, Wichmann HE, Volker U, Rawal R, Bidlingmaier M, Hannemann A, Dorr M, Rettig R, van Gilst WH, van Veldhuisen DJ, Bakker SJ, Navis G, Wallaschofski H, Meneton P, van der Harst P, Reincke M, Vasan RS, Consortium CK, Icbp. EchoGen C. Genome-wide meta-analyses of plasma renin activity and concentration reveal association with the kininogen 1 and prekallikrein genes, Circulation. Cardiovascular genetics. 2015;8:131–140. doi: 10.1161/CIRCGENETICS.114.000613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Zou X, Zhang XX, Liu XY, Li R, Wang M, Wu WJ, Sui Y, Zhao HL. Renal kallikrein activation and renoprotection after dual blockade of renin-angiotensin system in diet-induced diabetic nephropathy. Journal of diabetes research. 2015;2015:310645. doi: 10.1155/2015/310645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yiu WH, Wong DW, Chan LY, Leung JC, Chan KW, Lan HY, Lai KN, Tang SC. Tissue kallikrein mediates pro-inflammatory pathways and activation of protease-activated receptor-4 in proximal tubular epithelial cells. PloS one. 2014;9:e88894. doi: 10.1371/journal.pone.0088894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wang Y, Luo W, Reiser G. Trypsin and trypsin-like proteases in the brain: proteolysis and cellular functions. Cellular and molecular life sciences : CMLS. 2008;65:237–252. doi: 10.1007/s00018-007-7288-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ashby EL, Kehoe PG, Love S. Kallikrein-related peptidase 6 in Alzheimer's disease and vascular dementia. Brain research. 2010;1363:1–10. doi: 10.1016/j.brainres.2010.09.017. [DOI] [PubMed] [Google Scholar]
- 143.Ogawa K, Yamada T, Tsujioka Y, Taguchi J, Takahashi M, Tsuboi Y, Fujino Y, Nakajima M, Yamamoto T, Akatsu H, Mitsui S, Yamaguchi N. Localization of a novel type trypsin-like serine protease, neurosin, in brain tissues of Alzheimer's disease and Parkinson's disease. Psychiatry and clinical neurosciences. 2000;54:419–426. doi: 10.1046/j.1440-1819.2000.00731.x. [DOI] [PubMed] [Google Scholar]
- 144.Zarghooni M, Soosaipillai A, Grass L, Scorilas A, Mirazimi N, Diamandis EP. Decreased concentration of human kallikrein 6 in brain extracts of Alzheimer's disease patients. Clinical biochemistry. 2002;35:225–231. doi: 10.1016/s0009-9120(02)00292-8. [DOI] [PubMed] [Google Scholar]
- 145.Lou J, Si H, Chen Y, Sun X, Zhang H, Niu A, Hu C. Correlation between KLK6 expression and the clinicopathological features of glioma. Contemporary oncology. 2014;18:246–251. doi: 10.5114/wo.2014.44628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Drucker KL, Paulsen AR, Giannini C, Decker PA, Blaber SI, Blaber M, Uhm JH, O'Neill BP, Jenkins RB, Scarisbrick IA. Clinical significance and novel mechanism of action of kallikrein 6 in glioblastoma. Neuro-oncology. 2013;15:305–318. doi: 10.1093/neuonc/nos313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Scarisbrick IA, Radulovic M, Burda JE, Larson N, Blaber SI, Giannini C, Blaber M, Vandell AG. Kallikrein 6 is a novel molecular trigger of reactive astrogliosis. Biological chemistry. 2012;393:355–367. doi: 10.1515/hsz-2011-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Scarisbrick IA, Blaber SI, Lucchinetti CF, Genain CP, Blaber M, Rodriguez M. Activity of a newly identified serine protease in CNS demyelination. Brain : a journal of neurology. 2002;125:1283–1296. doi: 10.1093/brain/awf142. [DOI] [PubMed] [Google Scholar]
- 149.Hebb AL, Bhan V, Wishart AD, Moore CS, Robertson GS. Human kallikrein 6 cerebrospinal levels are elevated in multiple sclerosis. Current drug discovery technologies. 2010;7:137–140. doi: 10.2174/157016310793180611. [DOI] [PubMed] [Google Scholar]
- 150.Burda JE, Radulovic M, Yoon H, Scarisbrick IA. Critical role for PAR1 in kallikrein 6-mediated oligodendrogliopathy. Glia. 2013;61:1456–1470. doi: 10.1002/glia.22534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Sotiropoulou G, Pampalakis G, Prosnikli E, Evangelatos GP, Livaniou E. Development and immunochemical evaluation of a novel chicken IgY antibody specific for KLK6. Chemistry Central journal. 2012;6:148. doi: 10.1186/1752-153X-6-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Panos M, Christophi GP, Rodriguez M, Scarisbrick IA. Differential expression of multiple kallikreins in a viral model of multiple sclerosis points to unique roles in the innate and adaptive immune response. Biological chemistry. 2014;395:1063–1073. doi: 10.1515/hsz-2014-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Mitsui S, Tsuruoka N, Yamashiro K, Nakazato H, Yamaguchi N. A novel form of human neuropsin, a brain-related serine protease, is generated by alternative splicing and is expressed preferentially in human adult brain. European journal of biochemistry / FEBS. 1999;260:627–634. doi: 10.1046/j.1432-1327.1999.00213.x. [DOI] [PubMed] [Google Scholar]
- 154.Oka T, Akisada M, Okabe A, Sakurai K, Shiosaka S, Kato K. Extracellular serine protease neuropsin (KLK8) modulates neurite outgrowth and fasciculation of mouse hippocampal neurons in culture. Neuroscience letters. 2002;321:141–144. doi: 10.1016/s0304-3940(01)02470-3. [DOI] [PubMed] [Google Scholar]
- 155.Matsumoto-Miyai K, Ninomiya A, Yamasaki H, Tamura H, Nakamura Y, Shiosaka S. NMDA-dependent proteolysis of presynaptic adhesion molecule L1 in the hippocampus by neuropsin. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2003;23:7727–7736. doi: 10.1523/JNEUROSCI.23-21-07727.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Shiosaka S, Ishikawa Y. Neuropsin--a possible modulator of synaptic plasticity. Journal of chemical neuroanatomy. 2011;42:24–29. doi: 10.1016/j.jchemneu.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 157.Tamura H, Kawata M, Hamaguchi S, Ishikawa Y, Shiosaka S. Processing of neuregulin-1 by neuropsin regulates GABAergic neuron to control neural plasticity of the mouse hippocampus. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2012;32:12657–12672. doi: 10.1523/JNEUROSCI.2542-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Sahin U, Weskamp G, Kelly K, Zhou HM, Higashiyama S, Peschon J, Hartmann D, Saftig P, Blobel CP. Distinct roles for ADAM10 and ADAM17 in ectodomain shedding of six EGFR ligands. The Journal of cell biology. 2004;164:769–779. doi: 10.1083/jcb.200307137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Abdallah RT, Keum JS, El-Shewy HM, Lee MH, Wang B, Gooz M, Luttrell DK, Luttrell LM, Jaffa AA. Plasma kallikrein promotes epidermal growth factor receptor transactivation and signaling in vascular smooth muscle through direct activation of protease-activated receptors. The Journal of biological chemistry. 2010;285:35206–35215. doi: 10.1074/jbc.M110.171769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Voynow JA, Fischer BM, Roberts BC, Proia AD. Basal-like cells constitute the proliferating cell population in cystic fibrosis airways. American journal of respiratory and critical care medicine. 2005;172:1013–1018. doi: 10.1164/rccm.200410-1398OC. [DOI] [PubMed] [Google Scholar]
- 161.Hackett NR, Shaykhiev R, Walters MS, Wang R, Zwick RK, Ferris B, Witover B, Salit J, Crystal RG. The human airway epithelial basal cell transcriptome. PloS one. 2011;6:e18378. doi: 10.1371/journal.pone.0018378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Takeyama K, Dabbagh K, Lee HM, Agusti C, Lausier JA, Ueki IF, Grattan KM, Nadel JA. Epidermal growth factor system regulates mucin production in airways. Proceedings of the National Academy of Sciences of the United States of America. 1999;96:3081–3086. doi: 10.1073/pnas.96.6.3081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Takeyama K, Jung B, Shim JJ, Burgel PR, Dao-Pick T, Ueki IF, Protin U, Kroschel P, Nadel JA. Activation of epidermal growth factor receptors is responsible for mucin synthesis induced by cigarette smoke. American journal of physiology. Lung cellular and molecular physiology. 2001;280:L165–L172. doi: 10.1152/ajplung.2001.280.1.L165. [DOI] [PubMed] [Google Scholar]
- 164.Hirsch FR, Scagliotti GV, Langer CJ, Varella-Garcia M, Franklin WA. Epidermal growth factor family of receptors in preneoplasia and lung cancer: perspectives for targeted therapies. Lung cancer. 2003;41(Suppl 1):S29–S42. doi: 10.1016/s0169-5002(03)00137-5. [DOI] [PubMed] [Google Scholar]
- 165.Vallath S, Hynds RE, Succony L, Janes SM, Giangreco A. Targeting EGFR signalling in chronic lung disease: therapeutic challenges and opportunities. The European respiratory journal. 2014;44:513–522. doi: 10.1183/09031936.00146413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Gao L, Chao L, Chao J. A novel signaling pathway of tissue kallikrein in promoting keratinocyte migration: activation of proteinase-activated receptor 1 and epidermal growth factor receptor. Experimental cell research. 2010;316:376–389. doi: 10.1016/j.yexcr.2009.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Oikonomopoulou K, Hansen KK, Saifeddine M, Vergnolle N, Tea I, Diamandis EP, Hollenberg MD. Proteinase-mediated cell signalling: targeting proteinase-activated receptors (PARs) by kallikreins and more. Biological chemistry. 2006;387:677–685. doi: 10.1515/BC.2006.086. [DOI] [PubMed] [Google Scholar]
- 168.Madeddu P, Ena P, Parpaglia PP, Patteri G, Bacciu S, Maioli M, Glorioso N. Depressed urinary excretion of epidermal growth factor in psoriasis. American journal of nephrology. 1991;11:313–317. doi: 10.1159/000168329. [DOI] [PubMed] [Google Scholar]
- 169.Stangou M, Alexopoulos E, Papagianni A, Pantzaki A, Bantis C, Dovas S, Economidou D, Leontsini M, Memmos D. Urinary levels of epidermal growth factor, interleukin-6 and monocyte chemoattractant protein-1 may act as predictor markers of renal function outcome in immunoglobulin A nephropathy. Nephrology. 2009;14:613–620. doi: 10.1111/j.1440-1797.2008.01051.x. [DOI] [PubMed] [Google Scholar]
- 170.Jorgensen PE, Nexo E, Poulsen SS, Almendingen M, Berg T. Processing of epidermal growth factor in the rat submandibular gland by Kallikrein-like enzymes. Growth factors. 1994;11:113–123. doi: 10.3109/08977199409001053. [DOI] [PubMed] [Google Scholar]
- 171.Britsch S. The neuregulin-I/ErbB signaling system in development and disease. Advances in anatomy, embryology, and cell biology. 2007;190:1–65. [PubMed] [Google Scholar]
- 172.Ieguchi K, Fujita M, Ma Z, Davari P, Taniguchi Y, Sekiguchi K, Wang B, Takada YK, Takada Y. Direct binding of the EGF-like domain of neuregulin-1 to integrins ({alpha}v{beta}3 and {alpha}6{beta}4) is involved in neuregulin-1/ErbB signaling. The Journal of biological chemistry. 2010;285:31388–31398. doi: 10.1074/jbc.M110.113878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Hamilton BS, Whittaker GR. Cleavage activation of human-adapted influenza virus subtypes by kallikrein-related peptidases 5 and 12. The Journal of biological chemistry. 2013;288:17399–17407. doi: 10.1074/jbc.M112.440362. [DOI] [PMC free article] [PubMed] [Google Scholar]