Abstract
This study evaluated the relationship between interpersonal communication about cigarette health warning labels (HWLs), psychological responses to HWLs, and smoking cessation attempts. Data were analyzed from online consumer panels of adult smokers in Australia, Canada and Mexico, during implementation of new pictorial health warning labels (HWLs) on cigarette packs. Approximately 1000 adult smokers were surveyed in each country every four months (September 2012, January 2013, May 2013, September 2013, January 2014). Only smokers followed for at least two waves were included in the analytic sample. Participants reported the frequency of talking about HWLs in the last month (in general, with family members, and with friends). For each country, poisson generalized estimating equation (GEE) models were estimated to assess the bivariate and adjusted correlates of talking about HWLs. Logistic GEE models regressed having attempted to quit by the subsequent wave on HWL talk, socio-demographics and psychological responses to HWLs. The frequency of HWL talk gradually decreased in Canada (48%–36%) after new HWLs were implemented; an increase (30%–58%) in Australia corresponded with implementation of new HWLs, after which talking stabilized; and the frequency of HWL talk in Mexico was stable over time, where new HWLs are implemented every six months. Talk about HWLs was an independent predictor of subsequent quit attempts in Canada (AOR = 1.50; 95% CI = 1.11 –2.02), Australia (AOR = 1.41; 95% CI = 1.05–1.89), and Mexico (AOR = 1.53; 95% CI = 1.11–2.10), as was cognitive responses to HWLs (Australia AOR = 1.66; 95% CI = 1.22–2.24; Canada AOR = 1.56; 95% CI = 1.15–2.11; Mexico AOR = 1.30; 95% CI = 0.91–1.85). No interaction between talk and cognitive reactions to HWLs were found. These results suggest that interpersonal communication about HWLs influences smoking cessation attempts independent of other established predictors of smoking cessation, including cessation-related HWL responses. Future research should determine ways to catalyze interpersonal communication about HWLs and thereby potentiate HWL effects.
Keywords: Canada, Australia, Mexico, Tobacco, Health warning labels, Communication, Policy, Smoking cessation
1. Introduction
The World Health Organization’s Framework Convention on Tobacco Control recommends prominent pictorial health warning labels (HWLs) on cigarette packs (WHO,2008), and by 201470 countries had adopted this policy (CCS, 2014). HWL effects have been studied primarily as individual-level psychosocial outcomes and intermediate changes in smoking-related intentions and behaviors (e.g., delaying smoking, motivation to quit, cessation attempts). However, HWLs may also work by promoting discussions about smoking within smokers’ social networks. No study of which we aware has assessed how interpersonal communication about HWLs changes over time or whether talk about HWLs predicts cessation-related behaviors among adults smokers. The current study examined these relationships among adult smokers in Australia, Canada and Mexico, after new pictorial HWLs were introduced.
1.1. Interpersonal communication about media campaigns
Communication campaigns can promote interpersonal communication, but this potential pathway to behavior change is less-widely studied than those involving individual psychosocial responses (Southwell and Yzer, 2007; Wakefield et al., 2010; Durkin et al., 2012). Campaigns may prompt network discussions about campaign messages (McAfee et al., 2013), even transmitting messages to people who are not directly exposed to the campaign (Putte et al., 2011). Some research from drug and tobacco prevention campaigns suggests that campaign effects mediated by interpersonal discussions are more powerful predictors of changes in attitudes, risk perceptions, intentions and behavior than direct effects from campaign exposure (Morton and Duck, 2006; Putte et al., 2011). These effects may be because interpersonal communication leads to greater message elaboration, stronger recall, and stronger attitudinal change (Southwell and Yzer, 2007).
Evaluations of anti-smoking campaigns have examined interpersonal communication as an outcome and mediator of campaign effects. Self-reported campaign exposure is associated with greater interpersonal discussion about smoking risks and quitting (Boyle et al., 2010; Perusco et al., 2010; Perl et al., 2011; Murukutla et al., 2012). After campaigns are aired, interpersonal discussions about smoking and cessation have been shown to increase in general (Grigg et al., 2008; McAfee et al., 2013) and as a function of self-reported campaign exposure (Halkjelsvik et al., 2013). Interpersonal discussions about anti-smoking campaigns are associated with greater cessation-related perceptions and behaviors (Hafstad and Aaro, 1997; Dunlop et al., 2008; Dunlop et al., 2014), including in longitudinal studies (Durkin and Wakefield, 2006; Putte et al., 2011). As a whole, these studies suggest that interpersonal discussion is an important pathway through which campaigns can influence cessation-related perceptions and behaviors.
Two studies of HWLs suggest similar results. In a repeat cross-sectional study of adolescents in Australia, talk about HWLs increased after pictorial HWLs were first introduced (White et al., 2008); however, correlates or effects of this increase were not examined. Among adult smokers in Canada, an index that combined talking about HWLs with individual-level psychological responses to HWLs predicted subsequent cessation behavior (Hammond et al., 2003). However, any independent effects of talking about HWLs and its predictive power relative to other HWL responses were not analyzed. A better understanding of the role of interpersonal communication about anti-smoking media messages, including pictorial HWLs, requires research on the factors that influence interpersonal communication and its relationship with cessation-related perceptions and behaviors.
1.2. HWL policy context in Australia, Canada and Mexico
The current study examined data from three countries that had implemented new pictorial HWL content either immediately before or during the period of data collection (September 2012–January 2014). Canada first implemented pictorial HWLs in 2001 and introduced its second round of 16 warnings in 2012, when HWL size increased from 50% to 75% of the front and back of the package. Australia first adopted pictorial HWLs in 2006, and in December 2012, Australia became the first country in the world to implement ‘plain’ packaging (i.e., no brand logos, colors, typography), which was accompanied by seven new pictorial HWLs and an increase in HWL size from 30% to 75% of the pack front, while maintaining HWLs size on the back of the back (i.e., 90%). Finally, Mexico first implemented pictorial HWLs in 2010 and has the most rapid rotation of new HWL content in the world, introducing new content every 6 months. In Mexico, pictorial HWLs cover 30% of the front of the tobacco package and 100% of the back of the package includes a HWL with only textual content (Thrasher et al., 2012b).
1.3. Study aims
This study assesses changes in and effects of interpersonal communication about HWLs over a period when new pictorial HWLs were implemented in different ways. We hypothesized that interpersonal communication about HWLs will: 1a. increase after implementation of new HWLs (i.e., in Australia pre-to post-implementation of larger HWLs and plain packaging); 1b. decrease after implementation while HWL content remains unchanged (i.e., Australia after implementation; Canada across all waves); 1c. be stable where HWL content is regularly changed (i.e., Mexico across all waves); 2. Independently predict subsequent attempts to quit; and 3. moderate the relationship between individual-level, psychological responses to HWLs and subsequent cessation attempts, with stronger individual-level effects for people who more frequently engage in interpersonal communication about HWLs. These hypotheses mainly address associations or changes over time within countries rather than between countries due to differences in how samples were recruited and other potential confounding factors (e.g., culturally-shaped communication norms).
2. Methods
2.1. Sample
Data were collected from adult smokers who participate in online consumer panels in Australia, Canada, and Mexico; US data were excluded because of differences in study design (e.g., different baseline and followup periods) and confounding factors, such as the intermittent airing of its first nation-wide, smoking cessation media campaign (e.g., McAfee et al., 2013), which influence HWL responses (e.g., Thrasher et al., 2013). A rolling panel design was used, such that approximately 1000 adult smokers were surveyed in each country every four months (September 2012, January 2013, May 2013, September 2013, January 2014), with new participants recruited at each wave to replace smokers lost to follow-up. Eligibility criteria at study entry included being 18–64 years old, having smoked at least 100 cigarettes, and having smoked at least once in the prior month. After study entry, participants who quit smoking were surveyed. Because of our primary interest in examining predictors of cessation attempts, the analytic sample included data from 3201 individuals (Canada = 1096; Australia = 1082; Mexico = 1023) who were successfully followed up for at least one wave (i.e., range of follow up across waves: Canada = 54–55%; Australia = 62%–68%; Mexico = 46%–57%).
2.2. Measures
2.2.1. Interpersonal communication about HWLs
Three questions asked “In the last month, how often have: 1. you talked to others about the warning labels on cigarette packs?; 2 your family members spoken with you about the warning label son cigarette packs?; and other people besides your family spoken with you about the warning labels on cigarette packs?”, with responses on a 5-point scale (1 = “not at all”; 2 = “once”; 3 = “a few times”; 4 = “often”; 5 = “very often”) and good internal consistency (Australia, α= 0.87; Canada, α= 0.84; Mexico, α= 0.82). Because of skewed distributions, each original variable was recoded (i.e., never=0; once=1; a few times or more = 2) and summed (range = 0–6). When analyzing this measure as an independent variable, three categories were used (i.e., none=0; low=1–3; high=4–6), as cut points for these categories had the most uniform distribution across countries. Using the same cut points allowed qualitative comparison of the strength of associations across countries.
2.2.2. Individual-level psychological responses to HWLs
Smoking-related risk beliefs were assessed as in prior research (Swayampakala et al., 2015), whereby participants were shown a randomized list of diseases and asked which, if any, were caused by smoking (“Yes” = 1; “No” = 0; “Don’t know” = 0). Smoking-related diseases on HWLs in at least one country (i.e., emphysema = all countries; heart attacks or strokes = all countries; gangrene = Australia and Mexico; blindness = Australia and Canada; bladder cancer =Australia and Canada) were combined into an index (range = 0–5). Questions on cognitive responses to HWLs that predict quitting behavior in prior studies (Borland et al., 2009) were adapted for the present study: “To what extent do the warning labels make you think about the health risks?”, “To what extent do the warning labels on cigarette packs make you more likely to quit?”, and “How much do the warning labels make you feel like you would be better off without smoking?”. Response options ranged from 1 to 9, with verbal anchors at regular intervals (i.e., 1 = “Not at all”; 3 = “A little”; 5 =“Moderately”; 7 =“Very much”; and 9 =“Extremely”). Reliability was high (i.e., Australia, α=0.93; Canada, α=0.92; Mexico, α=0.91), so items were summed. Tertile cut points were selected based on distributions within each country, because of likely linguistic and cultural variation in interpretation of response options.
2.2.3. Quit attempt at the subsequent wave
At each survey wave, participants were asked if they currently smoked cigarettes every day, some days, or had quit smoking. Another question asked about any quit attempt in the prior four months, with a four-month-ago anchor used. Report of being quit or of having attempted to quit at the follow-up survey (i.e., t + 1) was used to indicate a quit attempt at the subsequent wave. The small number of smokers who were quit for a month or longer at survey assessments did not permit analysis of sustained cessation.
2.2.4. Control variables
The Heaviness of Smoking Index (HSI) was used, combining information on the number of cigarettes per day with the time between waking and the first cigarette of the day (Heatherton et al., 1989). Smokers were asked their intention to quit, with responses dichotomized to indicate intention in the next six months (yes = 1 vs. no = 0). At each wave, participants were asked if they had attempted to stop smoking in the prior 4 months, with responses dichotomized (1 = “yes”; 0 = “no”; 0 = “don’t know”).
Socio-demographic control variables included age (i.e., 18–24; 25–34; 35–44; 45–54; 55–64), sex, education (i.e., high school or less; some college or university; complete university or higher), annual household income in Canada and Australia (i.e., low = $0 to $29,999; middle = $30,000 to $59,999; high = $60,000 or more) and monthly household income in Mexico (i.e., low = $0 to $5000; middle = $5001 to $10,000; high = $10,001 or more, in pesos). Living with children under 18 was assessed (yes = 1; no = 0) because smokers with young families may be more likely to discuss consequences of tobacco smoke exposure (Dunlop et al., 2014). To assess changes over time, wave of data collection for the observation was indicated. Finally, we adjusted for possible effects of participating in prior surveys (i.e., “time-in-sample”) by assessing the number of prior surveys participants had answered at each survey wave. Control variables were dummy coded, with the lowest value as the reference group.
2.3. Analysis
Stata version 13 (StataCorp LP, 2013) was used for all analyses. Within each country, chi-square tests were used to assess differences between the analytic sample and those who were excluded due to lack of follow-up. Within-country differences in the analytic sample across waves were assessed similarly. In each country for each wave, the percent of smokers who reported any talk about HWLs were estimated. For each country, poisson generalized estimating equation (GEE) models were estimated to assess bivariate and adjusted associations between the frequency of HWL talk (range = 0–6) and primary study variables and controls. Finally, we estimated a series of logistic GEE models to predict having attempted to quit by the subsequent wave (t + 1). These bivariate and adjusted models included the three-level HWL talk variable (i.e., no talk; low talk; high talk), the three-level HWL cognitive response variable, risk beliefs, and control variables. To assess interactions, HWL talk (range 0–6) was multiplied by HWL cognitive responses (range = 0–3) and, separately, by smoking-related risk beliefs (range = 0–5). Each multiplicative term was added separately to fully-adjusted models predicting quit attempts.
We also conducted a range of sensitivity analyses. Bivariate and adjusted logistic GEE models regressed quit attempts on each of the three original HWL talk variables, analyzed separately. To address potential issues with attrition, we used two approaches: 1) propensity scores were developed using a variety of indicators not used in our models (e.g., frequency of consumer surveys) to predict likelihood of dropping out of the study, and models were adjusted using these scores; 2) multiple imputation was used to replace missing data for observations eliminated due to list wise deletion (Canada n = 202–205 observations across adjusted models; Australia n = 284–288; Mexico n = 183–187); 3) observations were integrated that had been excluded because of participation in only one wave (Canada n = 1235; Australia n = 950; Mexico n = 1482; see Table 1) or because, except for information on quit attempts, our analyses excluded information from the final survey for participants who dropped out before wave 5 (Canada n = 541; Australia n = 490; Mexico n = 565); these observations were integrated into the analytic sample, missing data were imputed, and GEE models regressing HWL talk on study variables were reestimated. Results were consistent with the reported results in terms of direction, magnitude, and, in the vast majority of cases, for statistical significance. Because differences in statistical significance were marginal, did not pertain to the primary study variables, and would not change our interpretations, we do not provide results from these analyses (available on request).
Table 1.
Characteristics of the analytic and excluded samples* for each country.
| Characteristics | Canada
|
Australia
|
Mexico
|
|||
|---|---|---|---|---|---|---|
| Excluded sample
|
Analytic sample*
|
Excluded sample
|
Analytic sample*
|
Excluded sample
|
Analytic sample*
|
|
| n = 1235 | n = 1122 | n = 950 | n = 1113 | n = 1481 | n = 1059 | |
| Age | ||||||
| 18–24 | 21% | 10%c | 21% | 6%c | 25% | 19%c |
| 25–34 | 26% | 22% | 29% | 22% | 31% | 30% |
| 35–44 | 23% | 21% | 21% | 24% | 18% | 20% |
| 45–54 | 16% | 22% | 17% | 24% | 14% | 15% |
| 55–64 | 14% | 24% | 12% | 23% | 12% | 16% |
| Gender | ||||||
| Male | 38% | 46%c | 36% | 46%c | 54% | 55% |
| Female | 62% | 54% | 64% | 54% | 46% | 45% |
| Education | ||||||
| High school or less | 40% | 30%c | 41% | 32%c | 42% | 32%c |
| Some College or Uni | 46% | 45% | 42% | 41% | 22% | 20% |
| Complete College or Uni | 14% | 25% | 17% | 27% | 36% | 48% |
| Income | ||||||
| Low | 33% | 25%c | 25% | 22%a | 54% | 39%c |
| Medium | 34% | 32% | 31% | 28% | 28% | 31% |
| High | 33% | 43% | 44% | 50% | 18% | 28% |
| HSI (mean) | 2.35 | 2.44 | 2.44 | 2.65b | 0.76 | 0.77 |
| Daily smoker | ||||||
| No | 21% | 21% | 23% | 16%c | 53% | 51% |
| Yes | 79% | 79% | 77% | 84% | 47% | 49% |
| Quit Intentions | ||||||
| No | 51% | 58%c | 52% | 57%a | 56% | 55% |
| Yes | 49% | 42% | 48% | 43% | 44% | 45% |
| Recent quit attempt | ||||||
| No | 57% | 62%a | 58% | 63%a | 49% | 48% |
| Yes | 43% | 38% | 42% | 37% | 51% | 52% |
| Children at home | ||||||
| No | 63% | 70%c | 57% | 67%c | 39% | 37% |
| Yes | 37% | 30% | 43% | 33% | 61% | 63% |
Data on the analytic sample are from initial enrollment into the study; each individual contributed up to four observations (i.e., Canada n = 2226 observations; Australia n = 2566 observations; Mexico n = 1960 observations), as well as data only on quit attempts from the final survey to which the participant responded.
p-value <0.05.
p-value<0.01.
p-value <0.001 for within-country differences between excluded sample vs. analytical subsample (Omnibus X2; F-test).
3. Results
3.1. Sample characteristics
In all three countries, comparison of the analytic sample with the sample that was excluded due to attrition (Table 1) indicated that the excluded sample was younger and more likely to report living with a child. In Australia, females, those with lower educational attainment, lower income, lower HSI, a recent quit attempt and higher quit intentions were also more likely to be lost to follow-up and thus excluded. In Canada, excluded participants were more likely to be female, intend to quit, and to have recently attempted to quit. Mexican participants who had lower education and income were more likely to be excluded. When comparing the analytic sample across waves within each country, no characteristics were significantly different except educational attainment: in all three countries, participants with higher educational attainment were less likely to participate in the second and third surveys.
3.2. Correlates and changes over time in talking about HWLs
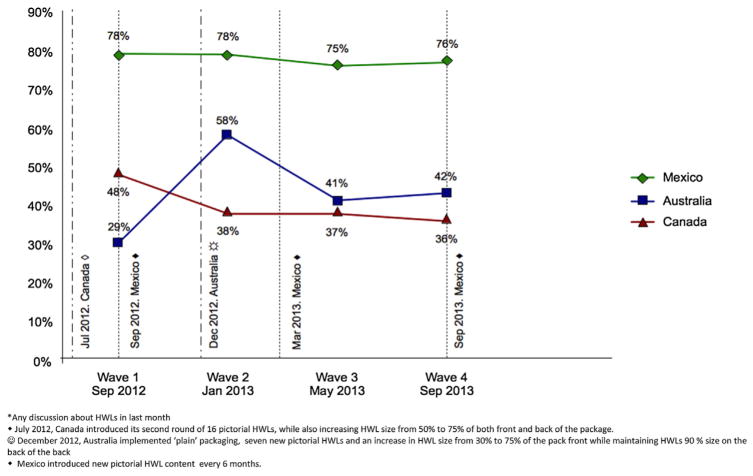
The prevalence of talking about HWLs showed a different pattern across all three countries (see Fig. 1). The prevalence of any talk was highest in Mexico, where it was stable over time (range = 78%–76%; mean range = 3.01–3.24). At the beginning of the study, Canada had the second highest prevalence (48%; mean = 1.52), which decreased over time (36% at wave 4; mean = 1.25). Australia started with the lowest prevalence (29%; mean = 1.06), with a substantial increase by wave 2 (58%; mean = 2.14), followed by a decrease and stability after the initial implementation period (range 41%–42%; mean 1.42–1.53).
Fig. 1.
Interpersonal communication* about health warning labels (HWLs) on cigarette packages, by country, September 2012–January 2014.
Results from poisson GEE models to assess correlates of talking about HWLs (See Table 2) were consistent with the time-related changes shown in Fig. 1. No statistically significant time-related associations with talking about HWLs were found for Mexico. For Canada, HWL talk significantly decreased after the initial survey wave (AORwave2 v wave 1 = 0.77, 95% CI = 0.65, 0.92), and then remained relatively stable. The statistically significant increase in talk about HWLs from baseline to immediate post-implementation in Australia (AORwave2 v wave 1 = 2.26, 95% CI = 1.90, 2.68) was followed by a significant decrease (AORwave3 v wave 1 = 1.46, 95% CI = 1.20, 1.76) and leveling off. Results from both bivariate and adjusted models in all three countries indicated an inverse relationship between age and HWL talk, whereas having made a recent quit attempt and reporting relatively stronger cognitive responses to HWLs were positively associated with HWL talk. Participants in all three countries who lived with children were more likely to talk about HWLs than those who did not, although this association remained statistically significant in adjusted models only in Canada. In Canada and Australia, participants with the highest educational attainment were more likely to talk about HWLs than those in the lowest groups (Canada AORhigh v low = 1.30, 95% CI = 1.07, 1.56; Australia AORhigh v low = 1.31, 95% CI = 1.11, 1.55).
Table 2.
Correlates of more frequent talking about health warning labels (HWLs) in the prior month, by country.
| Sample characteristics | Canada
|
Australia
|
Mexico
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IRR* | (SE) | AIRR* | (SE) | IRR* | (SE) | AIRR* | (SE) | IRR* | (SE) | AIRR* | (SE) | |
| Age | ||||||||||||
| 18–24 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 25–34 | 0.96 | (0.11) | 0.87 | (0.09) | 1.00 | (0.12) | 0.87 | (0.10) | 0.87 | (0.05) | 0.92 | (0.04) |
| 35–44 | 0.67b | (0.09) | 0.61c | (0.07) | 0.79b | (0.10) | 0.73b | (0.08) | 1.02 | (0.06) | 0.99 | (0.05) |
| 45–54 | 0.57c | (0.08) | 0.62c | (0.08) | 0.46c | (0.06) | 0.56c | (0.07) | 0.76c | (0.05) | 0.77c | (0.05) |
| 55–64 | 0.47c | (0.07) | 0.55c | (0.07) | 0.41c | (0.06) | 0.55c | (0.07) | 0.74c | (0.06) | 0.79c | (0.06) |
| Sex | ||||||||||||
| Male | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Female | 0.93 | (0.08) | 0.91 | (0.07) | 0.90 | (0.07) | 0.94 | (0.06) | 1.06 | (0.04) | 1.05 | (0.04) |
| Education | ||||||||||||
| High school or less | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Some College or Uni | 1.02 | (0.10) | 1.02 | (0.09) | 1.18 | (0.11) | 1.10 | (0.09) | 1.00 | (0.05) | 0.96 | (0.04) |
| Completed college or Uni | 1.51c | (0.16) | 1.30b | (0.12) | 1.69c | (0.16) | 1.31c | (0.11) | 1.02 | (0.04) | 1.02 | (0.04) |
| Income | ||||||||||||
| Low | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Middle | 1.05 | (0.10) | 1.02 | (0.09) | 1.20 | (0.12) | 1.16 | (0.11) | 1.03 | (0.04) | 1.04 | (0.04) |
| High | 1.33c | 0.12 | 1.12 | (0.10) | 1.33b | (0.13) | 1.20a | (0.11) | 0.99 | (0.04) | 1.04 | (0.04) |
| Children at home | ||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Yes | 1.48c | (0.11) | 1.19a | (0.09) | 1.44c | (0.11) | 1.12 | (0.08) | 1.16c | (0.05) | 1.02 | (0.04) |
| Heaviness Smoking Index | 0.99 | (0.02) | 1.09c | (0.03) | 0.98 | (0.02) | 1.07c | (0.02) | 1.01 | (0.02) | 1.04c | (0.02) |
| Daily smoker | ||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Yes | 0.82a | (0.07) | 0.89 | (0.08) | 0.93 | (0.08) | 0.98 | (0.08) | 0.93a | (0.03) | 0.99 | (0.04) |
| Quit Intentions | ||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Yes | 1.44c | (0.09) | 1.10 | (0.07) | 1.39c | (0.08) | 1.14a | (0.07) | 1.16c | (0.04) | 1.04 | (0.03) |
| Recent quit attempt | ||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Yes | 1.59c | (0.10) | 1.23c | (0.08) | 1.45c | (0.08) | 1.18b | (0.07) | 1.22c | (0.05) | 1.07 | (0.04) |
| Smoking-related risk beliefs | 1.03 | (0.02) | 0.99 | (0.02) | 1.01 | (0.02) | 0.98 | (0.02) | 1.05c | (0.01) | 1.04b | (0.01) |
| Cognitive HWL responses | ||||||||||||
| Low | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Mid | 2.58c | (0.24) | 2.41c | (0.22) | 2.41c | (0.20) | 2.09c | (0.17) | 1.94c | (0.15) | 1.88c | (0.15) |
| High | 4.22c | (0.36) | 3.71c | (0.33) | 3.61c | (0.29) | 2.84c | (0.25) | 2.53c | (0.19) | 2.42c | (0.19) |
| Wave | ||||||||||||
| 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| 2 | 0.86a | (0.06) | 0.77b | (0.07) | 1.90c | (0.12) | 2.26c | (0.20) | 1.05 | (0.04) | 1.02 | (0.04) |
| 3 | 0.89 | (0.06) | 0.86 | (0.07) | 1.25c | (0.08) | 1.46c | (0.14) | 0.99 | (0.04) | 1.05 | (0.05) |
| 4 | 0.86a | (0.06) | 0.80a | (0.08) | 1.32c | (0.08) | 1.54c | (0.15) | 1.00 | (0.04) | 1.09 | (0.05) |
IRR: unadjusted bivariate association; AIRR: adjusted model includes all variables in the table and time-in-sample. Adjusted models include 2024 observations from 1065 individuals in Canada, 2282 observations from 1062 individuals in Australia, and 1777 observations from 990 individuals in Mexico. All models estimated using poisson GEE.
p < 0.05.
p < 0.01.
p < 0.001.
3.3. Predictors of quit attempts
The study results showed a clear dose–response relationship between talk about HWLs and subsequent quit attempts, with more quit attempts for greater frequency of talk in Canada (32%, 42%, 61%), Australia (26%, 36%, 53%), and Mexico (41%, 55%, 65%). Greater frequency of HWL talk was significantly associated with quit attempts in bivariate models (see Table 3), although this relationship remained statistically significant in adjusted models only when comparing the group that most frequently talked about HWLs with those who did not talk about them (Canada, AORhigh v none = 1.50 95% CI = 1.11, 2.02; Australia, AORhigh v none = 1.41, 95% CI = 1.05, 1.89; Mexico, AORhigh v none = 1.53, 95% CI = 1.13, 2.13). A similar pattern of results was found when examining individual-level cognitive responses to HWLs, except that results for Mexico were no longer statistically significant in adjusted models. Other predictors of quit attempts at follow-up in both bivariate and adjusted models included greater education in Canada and Australia, intending to quit in all three countries, and recent quit attempts in all three countries. Interactions between HWL talk and cognitive responses to HWLs as well as between HWL talk and smoking-related risk beliefs were not statistically significant in either Canada (p = 0.92 & p = 0.42, respectively), Australia (p = 0.71 & p = 0.34 respectively), or Mexico (p = 0.31 & p = 43).
Table 3.
Crude and adjusted odds of trying to quit by follow-up, by country.
| Canada
|
Australia
|
Mexico
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | OR | 95% CI | AOR* | 95% CI | % | OR | 95% CI | AOR* | 95% CI | % | OR | 95% CI | AOR* | 95% CI | |
| Age | |||||||||||||||
| 18–24 | 53 | ||||||||||||||
| 25–34 | 53 | 1.01 | [0.70–1.46] | 1.04 | [0.66–1.65] | 49 | 1.16 | [0.71–1.89] | 1.67 | [0.87–3.2] | 63 | 1.23 | [0.89–1.72] | 1.03 | [0.71–1.48] |
| 35–44 | 41 | 0.67a | [0.45–1.00] | 0.79 | [0.49–1.27] | 39 | 0.81 | [0.49–1.33] | 1.23 | [0.64–2.36] | 64 | 1.31 | [0.93–1.88] | 1.10 | [0.75–1.61] |
| 45–54 | 35 | 0.53b | [0.36–0.79] | 0.72 | [0.45–1.15] | 27 | 0.49b | [0.30–0.81] | 1.04 | [0.54–2.01] | 53 | 0.77 | [0.53–1.14] | 0.79 | [0.53–1.20] |
| 55–64 | 33 | 0.48c | [0.33–0.72] | 0.69 | [0.43–1.1] | 30 | 0.53a | [0.32–0.88] | 1.26 | [0.66–2.43] | 46 | 0.59b | [0.41–0.86] | 0.89 | [0.59–1.35] |
| Sex | |||||||||||||||
| Male | 42 | 37 | 58 | ||||||||||||
| Female | 40 | 0.87 | [0.70–1.09] | 0.88 | [0.71–1.1] | 34 | 0.88 | [0.71–1.10] | 0.88 | [0.71–1.1] | 59 | 1.05 | [0.84–1.31] | 1.09 | [0.88–1.36] |
| Education | |||||||||||||||
| High school or less | 37 | 29 | 60 | ||||||||||||
| Some College or Uni | 37 | 1.10 | [0.87–1.39] | 1.01 | [0.77–1.31] | 33 | 1.19 | [0.93–1.53] | 1.22 | [0.95–1.57] | 57 | 0.83 | [0.63–1.13] | 0.93 | [0.67–1.30] |
| Completed college o Uni | 52 | 1.76c | [1.32–2.35] | 1.47a | [1.07–2.01] | 49 | 2.13c | [1.62–2.80] | 1.64c | [1.22–2.2] | 57 | 0.83 | [0.65–1.05] | 0.97 | [0.74–1.28] |
| Income | |||||||||||||||
| Low | 36 | 1 | 1 | 33 | 1 | 1 | 69 | 1 | 1 | ||||||
| Middle | 41 | 1.11 | [0.85–1.45] | 1.06 | [0.80–1.41] | 32 | 0.89 | [0.69–1.17] | 0.65b | [0.48–0.89] | 59 | 0.81 | [0.65–1.09] | 0.81 | [0.61–1.07] |
| High | 43 | 1.21 | [0.94–1.56] | 0.88 | [0.67–1.17] | 39 | 1.18 | [0.93–1.51] | 0.77 | [0.59–1.02] | 58 | 0.72a | [0.56–0.93] | 0.78 | [0.57–1.07] |
| Children at home | |||||||||||||||
| No | 39 | 1 | 1 | 33 | 1 | 1 | 51 | 1 | 1 | ||||||
| Yes | 47 | 1.32c | [1.05–1.66] | 1.04 | [0.80–1.35] | 41 | 1.49c | [1.20–1.84] | 1.06 | [0.83–1.35] | 62 | 1.43c | [1.17–1.75] | 1.18 | [0.92–1.51] |
| Heaviness Smoking Index | 0.84c | [0.79–0.89] | 0.96 | [0.89–1.05] | 0.87c | [0.80–0.95] | 0.93 | [0.86–1.01] | 0.88c | [0.81–0.96] | 0.93 | [0.84–1.03] | |||
| Daily smoker | |||||||||||||||
| No | 67 | 1 | 1 | 60 | 1 | 1 | 66 | 1 | 1 | ||||||
| Yes | 35 0.c | 43 | [0.35–0.53] | 0.55c | [0.39–0.77] | 31 | 0.46c | [0.37–0.59] | 0.72 | [0.50–1.02] | 50 | 0.63c | [0.51–0.76] | 0.78 | [0.6–1.02] |
| Quit Intentions | |||||||||||||||
| No | 24 | 1 | 1 | 18 | 1 | 1 | 41 | 1 | 1 | ||||||
| Yes | 61 | 2.94c | [2.41–3.59] | 2.28c | [1.80–2.88] | 60 | 3.85c | [3.17–4.68] | 2.66c | [2.11–3.36] | 75 | 2.84c | [2.30–3.51] | 1.75c | [1.33–2.32] |
| Recent quit attempt | |||||||||||||||
| no | 20 | 1 | 1 | 17 | 1 | 1 | 33 | 1 | 1 | ||||||
| yes | 72 | 7.74c | [6.18–9.69] | 4.91c | [3.78–6.38] | 69 | 11.4c | [9.12–14.23] | 6.42c | [4.98–8.28] | 79 | 8.19c | [6.56–10.22] | 6.27c | [4.78–8.23] |
| Smoking-related risk beliefs | 61 | 1.03 | [0.98–1.09] | 1.02 | [0.94–1.11] | 53 | 1.02 | [0.97–1.07] | 1.04 | [0.97–1.12] | 65 | 1.09a | [1.02–1.17] | 1.08 | [0.97–1.20] |
| Cognitive HWL responses | |||||||||||||||
| Low | 28 | 1 | 1 | 21 | 1 | 1 | 37 | 1 | 1 | ||||||
| Mid | 38 | 1.22 | [0.99–1.52] | 0.97 | [0.74–1.27] | 37 | 1.45c | [1.21–1.73] | 1.08 | [0.84–1.41] | 52 | 1.22 | [0.95–1.56] | 1.08 | [0.77–1.52] |
| High | 60 | 2.15c | [1.70–2.72] | 1.56b | [1.15–2.11] | 55 | 2.22c | [1.79–2.75] | 1.66c | [1.22–2.24] | 67 | 1.79c | [1.40–2.29] | 1.30 | [0.91–1.85] |
| Interpersonal communication | |||||||||||||||
| None | 32 | 1 | 1 | 26 | 1 | 1 | 41 | 1 | 1 | ||||||
| Low | 42 | 1.27a | [1.03–1.57] | 0.99 | [0.74–1.32] | 36 | 1.24a | [1.00–1.53] | 1.09 | [0.81–1.46] | 55 | 1.43b | [1.11–1.85] | 1.29 | [0.93–1.80] |
| High | 61 | 2.17c | [1.72–2.73] | 1.50b | [1.11–2.02] | 53 | 1.98c | [1.60–2.44] | 1.41a | [1.05–1.89] | 65 | 2.15c | [1.68–2.75] | 1.53b | [1.11–2.10] |
OR = Crude Odds Ratio for bivariate association. AOR = Adjusted model includes all variables in the table, as well as survey wave and time-in-sample. Adjusted models include 2021 observations from 1065 individuals in Canada, 2278 observations from 1025 individuals in Australia and 1773 observations from 988 individuals in Mexico.
p < 0.05.
p < 0.01.
p < 0.001.
4. Discussion
The current study suggests that interpersonal communication about HWLs is an independent predictor of attempting to quit in Canada, Australia, and Mexico, above and beyond other established predictors, including individual-level cognitive responses to HWLs (Borland et al., 2009). This is consistent with studies of mass media campaigns (Hafstad and Aaro, 1997; Dunlop et al., 2008; Dunlop et al., 2014; Durkin and Wakefield, 2006; Putte et al., 2011), providing further support for the importance of this pathway of influence on behavior. Talking may not only embed the issue of smoking-related harms within social networks, but strengthen memories and evaluative associations by means of the elaborated thinking that accompanies a conversation. Encouraging greater talk about smoking-related harms might be done through mass media and social media campaigns that link with and compliment HWL content (Brennan et al., 2011; Thrasher et al., 2013), making HWLs more meaningful by increasing the frequency and depth of interpersonal communication about HWL topics (Wakefield et al., 2010). Indeed, minimum thresholds for effective media buys (Durkin et al., 2012) may be lower when messaging compliments pictorial HWLs because smokers’ are repeatedly exposed to HWLs (Thrasher et al., 2013). Future research should determine optimal media mixes for cessation campaigns that work in synergy with HWLs, perhaps considering strategies that promote and capitalize on interpersonal communication.
Changes in interpersonal communication about HWLs generally corresponded with hypothesized expectations related to the implementation of new HWL content in each country. Soon after new HWLs were implemented in Canada (i.e., July 2012), the baseline survey (i.e., September 2012) indicated a relatively high percentage of smokers who talked about HWLs (50%), with a decrease over subsequent waves, as found for cognitive responses to pictorial HWLs over longer periods of time (Hitchman et al., 2014; Borland et al., 2009b; Hammond et al., 2007). In Australia, a new HWL policy that included plain packaging was implemented after the baseline survey, doubling the smokers who talked about HWLs (from 29% to 58%), followed by a rapid decline and, then, remaining steady. The seemingly higher prevalence of talk about HWLs in Australia compared to Canada may be due to the simultaneous implementation of plain packaging in Australia, which would be consistent with experimental research indicating that plain packaging makes HWLs more salient (Germain et al., 2010). Finally, talk about HWLs in Mexico remained relatively higher and stable (75%–79%) over time, perhaps due to Mexico regularly rotating HWL content every six months. However, cultural factors that shape conversational norms (i.e., perceptions that significant others value and condone talking about a particular topic) may also come into play (Southwell and Yzer, 2007). Although comparisons across countries should be made cautiously (see below), our hypotheses regarding within-country changes in HWL talk over time were supported.
The correlates of communication about HWLs shed some light on the factors that may promote talk about HWLs. Smokers who intend to quit and who have recently engaged in a cessation attempt were more likely to talk about HWLs in all three countries. The personal relevance of health risk messaging may explain this, as experimental studies have consistently found stronger HWL responses among smokers who intend to quit (Hammond, 2011). Social support to quit, which we did not measure, may influence both quit intentions and talk about HWLs. Future research should examine these relationships and determine how HWLs can be designed to capitalize on and enhance both social support and intentions to quit.
Older smokers were relatively less likely to have engaged in talk about HWLs, as in prior antismoking campaign research (Dunlop et al., 2008, 2014). Network members may have given up communicating with older smokers about smoking because of previously unsuccessful efforts to promote quitting (Yong et al., 2005). Living with children was also significantly associated with engaging in communication about HWLs in Australia and Canada. Parents who live with young children may be particularly likely to discuss issues around secondhand smoke exposure (Dunlop et al., 2014), and the HWLs in each country that we examined included content on the health effects of secondhand smoke for children. Further research is needed to determine whether this particular HWL content is any more or less effective than other content for prompting families to talk about smoking and cessation.
In Australia, but not Canada or Mexico, smokers with relatively higher educational attainment were more likely to have talked about HWLs. Greater perceived efficacy to understand and talk about media campaign topics may motivate conversation about campaigns (Southwell and Yzer, 2007), and higher education may be associated with greater communication efficacy in Australia. However, some antismoking campaign research has found that smokers with relatively lower educational attainment are more likely to report interpersonal communication about quitting because of campaigns (Dunlop et al., 2014). Hence, if perceived efficacy explains education-related differences in talking about anti-smoking communications, it may partly depend on the format (e.g., print HWLs vs. electronic ads) or differential comprehension of message content. Future research should attend to how educational differences shape the effects of HWLs on interpersonal communications, with the aim of addressing tobacco-related disparities, particularly among disadvantaged populations.
Beliefs about smoking-related harms were associated with HWL talk only in Mexico, perhaps because of its shorter tobacco control history compared to Australia and Canada. Greater awareness of smoking-related harms may promote or result from talk about HWLs, particularly during the early phases of implementing comprehensive policies and campaigns that make smoking socially unacceptable. Even so, increasing awareness of the range of smoking-related harms remains a critical goal for HWLs, and new HWLs in all three countries have promoted awareness of less well-known harms (Swayampakala et al. 2015). Such beliefs may not translate into smoking cessation because of the addictive nature of tobacco use. Indeed, we found no association with quit attempts in any country. Nevertheless, beliefs about smoking-related harms likely provide the foundation for cognitive responses to HWLs, which predicted cessation in our study. Because HWLs involve frequent exposure, our measure of cognitive responses to HWLs, which assesses frequency of harm-related thoughts, appears critical to understanding HWL pathways to quit behavior (Yong et al., 2014). Future research should further disentangle these relationships, including whether HWLs can promote personal susceptibility to smoking-related harms.
A better understanding of the content of social interactions around HWLs may help with designing HWLs that are even more effective. Some research suggests that messages with more provocative, emotional appeals are not only most effective in promoting talk (Hafstad and Aaro, 1997), but also in promoting cessation (Durkin et al., 2012). Similarly, experimental research indicates that graphic imagery, including imagery that shows personal suffering from smoking-related consequences, is most effective (Hammond et al., 2012; Thrasher et al., 2012a). Future research should determine which HWL content (e.g., specific health risks, narrative/testimonial vs. factual, calls to action, links to social media) and design features (e.g., format, graphics) are most effective in spurring interpersonal communication that leads to cessation.
Our sensitivity analyses of each HWL indicator of the source of talk (i.e., family members, non-family others, anyone) found that the direction, magnitude and statistical significance of associations between HWL talk and downstream cessation were similar for all measures. This is not surprising given the high correlation across HWL talk indicators (i.e., range α= 0.82–0.87 across countries). These results also suggest that the source and content of discussion about HWLs may not matter as much as the fact that HWLs are the topic of discussion. However, the kinds of network-related questions addressed in the present investigation were limited in important ways (e.g., only ego networks were sampled and only a limited range of questions were asked).
HWLs could enhance their impact by targeting social networks. Socially mediated factors affecting smoking cessation likely stem from both direct influences (i.e., person-to-person contact) and indirect influences that depend on how members’ social networks are structured in terms of density, span, centralization and clustering. For example, Christakis and Fowler’s (2008) analysis of 32 years of panel data observed three important structural characteristics related to smoking in social networks: 1) Clusters of smokers typically spanned three degrees of separation, providing a natural “upper bound” to potential social influence effects; 2) Because cessation tended to occur cluster-wide and simultaneously, cluster size tended to remain stable over time despite overall declines in smoking, suggesting that entire clusters tended follow the lead of one or a few individual members; 3) Over time, nonsmokers became increasingly central, and smokers increasingly peripheral, in the larger network, while smokers and nonsmokers also became less socially tied to each other over time. Similar patterns have been found around obesity in adolescent networks (Trogdon et al., 2008) and for vaccination-related decision making (Xia and Liu, 2013). Hence, networks can facilitate or impede the transmission of individual perceptions and behaviors.
Theories of social influence offer directions for explaining, predicting, and capitalizing on these influences. Social Influence Network Theory, for which there is substantial empirical support (Friedkin and Johnsen, 2011), predicts that opinion change happens as a function of the weighted average of the opinions of those with whom we are connected. Social Impact Theory (Latané, 1981) identifies three general factors that align the thoughts and actions of a focal actor with others in his or her immediate social environment: the strength of those others (e.g., high social status, loving familial relationship, frequent positive interaction); their immediacy (e.g., the physical and temporal proximity of the source); and their number. These dimensions of social impact are theorized to interact such that their effects are multiplicative. This suggests that HWL impact will be maximized to the extent that they: 1) induce people to talk with loved ones and authority figures; 2) do so in the immediate contexts of smoking; and 3) involve as many different people as possible. Our results regarding the lack of differential effect for HWL talk on cessation by referent (i.e., family members, non-family others, anyone) may be due to the lack of detail on their strength, immediacy and number. Future research should explore these issues and opportunities to capitalize on key network ties, including the targeting of network nodes, such as opinion leaders and people who bridge networks (Watts and Strogatz, 1998), perhaps through linkage between HWLs and campaigns aired through traditional or social media.
4.1. Limitations
This study has several limitations. The content of HWL talk was not specified, and therefore, it is unclear if the talk was about quitting. Future research should look at whether the content of HWL talk matters, while also considering social network characteristics, source characteristics, channels of communication (e.g., face-to-face vs. social media), and opportunities for HWLs to take advantage of these dimensions of HWL talk. Self-reported frequency of HWL talk in the last month may be biased, although it is unclear whether reports are likely to over- or under-estimate these behaviors. However, evidence for the construct validity of reported HWL talk is evinced by its correlation with quit intentions, quit behavior, and cessation-related cognitive responses to HWLs, all of which would be expected from theories of behavior change. HWL talk may matter most to smokers earlier along the causal pathway from intention to cessation attempts. However, we did not distinguish between cessation attempts and quit success, due to the small sample of smokers that had been quit for a month or longer. Future research may consider the timing of HWL talk to determine whether it contributes meaningfully to successfully quitting.
Study results may have been influenced by nonresponse, attrition and selection biases. Retention rates in our study were moderate, about 60% from one wave to the next, and exclusion from the analytic sample due to lack of follow-up was associated with characteristics that were generally related to greater talk about HWLs (i.e., younger age, intention to quit, recent quit behavior, minors living at home). Hence, we may have underestimated the frequency of HWL talk. Still, our analyses adjusted for these and other differences between the analytic samples and excluded samples, as well as differences in sample composition across waves. Furthermore, the pattern of model results was consistent and study conclusions the same when considering models that adjusted for propensity scores derived from the likelihood of being followed up, when sample data were maximized by including eliminated observations, and when multiple imputation techniques were used. Nevertheless, imputation assumes missing at random, which the attrition analysis indicates was not the case, and study results may have been confounded in unpredictable ways by unmeasured variables and other biases.
The online samples from which we collected data provided limited ability to generalize results to the broader population of smokers, as panels were assembled from no known sampling frame. However, the characteristics of our samples are broadly comparable to the population of smokers in each country except Mexico, where smokers with higher educational attainment are overrepresented due to differential Internet penetration. Hence, inferences regarding cross-country comparisons should be tempered by this concern. Assessments of change over time within country are more reliable, and for this reason provide the primary emphases in our study.
4.2. Conclusions
Limitations aside, our study is the first to examine talk about HWLs amongst adult smokers, who are a key target for HWLs. Our results suggests that the introduction of new HWL and packaging policies can augment HWL talk, and although the frequency of talk declines over time, frequent rotation of new HWL content can sustain HWL talk. Furthermore, our results suggest that the effects of HWL talk on cessation attempts are independent of individual-level psychosocial responses to HWLs, recent quit attempts, quit intentions, and level of addiction, all of which have previously been associated with cessation behavior. Furthermore, the strength of the association between HWL talk and cessation attempts was similar across adult smokers in Australia, Canada and Mexico, suggesting that this relationship is robust across different HWL policy configurations and cultural contexts. Hence, further HWL research should determine how best to catalyze and work in synergy with social network talk about HWLs.
Supplementary Material
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.socscimed.2015.05.042.
References
- Borland R, Yong HH, Wilson N, Fong GT, Hammond D, Cummings KM, Hosking W, McNeill A. How reactions to cigarette packet health warnings influence quitting: findings from the ITC 4 country survey. Addiction. 2009a;104:669–675. doi: 10.1111/j.1360-0443.2009.02508.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R, Wilson N, Fong GT, Hammond D, Cummings KM, Yong HH, Hosking W, Hastings G, Thrasher JF, McNeill AD. Impact of graphic and text warnings on cigarette packs. Tob Control. 2009b;18(5):358–364. doi: 10.1136/tc.2008.028043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle T, Shepherd CC, Pearson G, Monteiro H, McAullay D, Economo K, Stewart S. Awareness and impact of the ‘Bubblewrap’ advertising campaign among Aboriginal smokers in Western Australia. Tob Control. 2010;19(1):83–86. doi: 10.1136/tc.2009.031856. [DOI] [PubMed] [Google Scholar]
- Brennan E, Durkin S, Cotter T, Harper T, Wakefield MA. Mass Media Campaigns Designed to Complement New Pictorial Health Warnings on Cigarette. 2011. [DOI] [PubMed] [Google Scholar]
- Christakis Nicholas A, Fowler James H. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358:2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CCS. Cigarette Package Health Warnings: International Status Report. 4. Candian Cancer Society; Ottawa, Canada: Sep, 2014. [Google Scholar]
- Durkin S, Wakefield M. Maximising the impact of emotive anti-tobacco advertising: effects of interpersonal discussion and program placement. Soc Mark Q. 2006;12(3):3–14. [Google Scholar]
- Durkin S, Brennan E, Wakefield M. Mass media campaigns to promote smoking cessation among adults: an integrative review. Tob Control. 2012;21(2):127–138. doi: 10.1136/tobaccocontrol-2011-050345. [DOI] [PubMed] [Google Scholar]
- Dunlop SM, Wakefield M, Kashima Y. The contribution of antismoking advertising to quitting: intra- and interpersonal processes. J Health Commun. 2008;13(3):250–266. doi: 10.1080/10810730801985301. [DOI] [PubMed] [Google Scholar]
- Dunlop SM, Cotter T, Perez D. When your smoking is not just about you: antismoking advertising, interpersonal pressure, and quitting outcomes. J Health Commun. 2014;19(1):41–56. doi: 10.1080/10810730.2013.798375. [DOI] [PubMed] [Google Scholar]
- Friedkin NE, Johnsen EC. Social Influence Network Theory: A Sociological Examination of Small Group Dynamics. Cambridge University Press; New York: 2011. [Google Scholar]
- Germain D, Wakefield MA, Durkin SJ. Adolescents’ perceptions of cigarette brand image: does plain packaging make a difference? J Adolesc Health. 2010;46:385–392. doi: 10.1016/j.jadohealth.2009.08.009. [DOI] [PubMed] [Google Scholar]
- Grigg M, Waa A, Bradbrook SK. Response to an indigenous smoking cessation media campaign – It’s about whānau. Aust N Z J Public Health. 2008;32(6):559–564. doi: 10.1111/j.1753-6405.2008.00310.x. [DOI] [PubMed] [Google Scholar]
- Hafstad A, Aaro LE. Activating interpersonal influence through provocative appeals: evaluation of a mass media-based antismoking campaign targeting adolescents. Health Commun. 1997;9:253–272. [Google Scholar]
- Halkjelsvik T, Lund KE, Kraft P, Rise J. Fear appeals in advanced tobacco control environments: the impact of a national mass media campaign in Norway. Health Educ Res. 2013;28(5):888–897. doi: 10.1093/her/cyt064. [DOI] [PubMed] [Google Scholar]
- Hammond D. Health warning messages on tobacco products: a review. Tob Control. 2011;20(5):327–337. doi: 10.1136/tc.2010.037630. [DOI] [PubMed] [Google Scholar]
- Hammond D, Thrasher JF, Reid JL, Driezen P, Boudreau C, Arillo-Santillán E. Perceived effectiveness of pictorial health warnings among Mexican youth and adults: a population-level intervention with potential to reduce tobacco-related inequities. Cancer Causes Control. 2012;23:57–67. doi: 10.1007/s10552-012-9902-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D, Fong GT, Borland R, Cummings KM, McNeil AD, Driezen P. Text and graphic warnings on cigarette packages: findings from the International Tobacco Control Four Country Study. Am J Prev Med. 2007;32(3):210–217. doi: 10.1016/j.amepre.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D, Fong GT, MacDonald PW, Cameron R, Brown KS. Impact of graphic Canadian warning labels on adult smoking behavior. Tob Control. 2003;12:391–395. doi: 10.1136/tc.12.4.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Addiction. 1989;84:791–800. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- Hitchman SC, Driezen P, Logel C, Hammond D, Fong GT. Changes in effectiveness of cigarette health warnings over time in Canada and the United States, 2002–2011. Nicotine Tob Res. 2014;16(5):536–543. doi: 10.1093/ntr/ntt196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latané Bibb. The psychology of social impact. Am Psychol. 1981;36:343–356. [Google Scholar]
- McAfee T, Davis KC, Alexander RL, Jr, Pechacek TF, Bunnell R. Effect of the first federally funded US antismoking national media campaign. Lancet. 2013;382(9909):2003–2011. doi: 10.1016/S0140-6736(13)61686-4. [DOI] [PubMed] [Google Scholar]
- Morton TA, Duck JM. Enlisting the influence of others: alternative strategies for persuasive media campaigns. J Appl Soc Psychol. 2006;36(2):269–296. [Google Scholar]
- Murukutla N, Turk T, Prasad CV, Saradhi R, Kaur J, Gupta S, Wakefield M. Results of a national mass media campaign in India to warn against the dangers of smokeless tobacco consumption. Tob Control. 2012;21(1):12–17. doi: 10.1136/tc.2010.039438. [DOI] [PubMed] [Google Scholar]
- Perl R, Stebenkova L, Morozova I, Murukutla N, Kochetova V, Kotov A, Baskakova J. Mass media campaigns within reach: effective efforts with limited resources in Russia’s capital city. Tob Control. 2011;20(6):439–441. doi: 10.1136/tc.2010.041269. [DOI] [PubMed] [Google Scholar]
- Perusco A, Poder N, Mohsin M, Rikard-Bell G, Rissel C, Williams M, Guirguis S. Evaluation of a comprehensive tobacco control project targeting Arabic-speakers residing in south west Sydney, Australia. Health Promot Int. 2010;25(2):153–165. doi: 10.1093/heapro/daq009. [DOI] [PubMed] [Google Scholar]
- van den Putte B, Yzer M, Southwell BG, de Bruijn GJ, Willemsen MC. Interpersonal communication as an indirect pathway for the effect of anti-smoking media content on smoking cessation. J Health Commun. 2011;16(5):470–485. doi: 10.1080/10810730.2010.546487. [DOI] [PubMed] [Google Scholar]
- Southwell BG, Yzer MC. The roles of interpersonal communication in mass media campaigns. In: Beck CS, editor. Communication Yearbook. Vol. 31. Erlbaum; New York: 2007. pp. 419–462. [Google Scholar]
- Swayampakala K, Thrasher JF, Hammond D, Yong HH, Bansal-Travers M, Krugman D, et al. Pictorial health warning label content and smokers’ understanding of smoking-related risks-a cross-country comparison. Health Educ Res. 2015;30(1):35–45. doi: 10.1093/her/cyu022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp LP. Stata/IC 13 for Windows. StataCorp LP; College Station, TX: 2013. [Google Scholar]
- Thrasher JF, Murukutla N, Pérez-Hernández R, Alday J, Arillo-Santillán E, Cedillo C, Gutierrez JP. Linking mass media campaigns to pictorial warning labels on cigarette packages: a cross-sectional study to evaluate impacts among Mexican smokers. Tob Control. 2013;22:e57–e65. doi: 10.1136/tobaccocontrol-2011-050282. [DOI] [PubMed] [Google Scholar]
- Thrasher JF, Arillo-Santillán E, Villalobos V, Pérez-Hernández R, Hammond D, Carter Jarvis, Sebrie E, Sansores R, Regalado-Piñeda J. Can pictorial warning labels on cigarette packages address smoking-related health disparities? Field experiments in Mexico to assess pictorial warning label content. Cancer Causes Control. 2012a;23:69–80. doi: 10.1007/s10552-012-9899-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher JF, Pérez-Hernández R, Arillo-Santillán E, Barrientos-Gutierrez I. Towards informed tobacco consumption in Mexico: effects of pictorial warning labels among smokers. Rev Salud Pública México. 2012b;54:242–253. [PMC free article] [PubMed] [Google Scholar]
- Trogdon Justin G, Nonnemaker James, Pais Joanne. Peer effects in adolescent overweight. J Health Econ. 2008;27(5):1388–1399. doi: 10.1016/j.jhealeco.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behavior. Lancet. 2010;376(9748):1261–1271. doi: 10.1016/S0140-6736(10)60809-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts DJ, Strogatz HS. Collective dynamics of ‘small-world’ networks. Nature. 1998;393:440–442. doi: 10.1038/30918. [DOI] [PubMed] [Google Scholar]
- White V, Webster B, Wakefield M. Do graphic health warning labels have an impact on adolescents’ smoking-related beliefs and behaviors? Addiction. 2008;103(9):1562–1571. doi: 10.1111/j.1360-0443.2008.02294.x. [DOI] [PubMed] [Google Scholar]
- WHO. Guidelines for Implementation of Article 11 of the WHO Framework Convention on Tobacco Control (Packaging and Labelling of Tobacco Products) World Health Organization; Geneva: 2008. [Google Scholar]
- Xia S, Liu J. A computational approach to characterizing the impact of social influence on individuals’ vaccination decision making. PLoS ONE. 2013;8(4):e60373. doi: 10.1371/journal.pone.0060373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yong HH, Borland R, Siahpush M. Quitting-related beliefs, intentions, and motivations of older smokers in four countries: findings from the International Tobacco Control Policy Evaluation Survey. Addict Behav. 2005;30:777–788. doi: 10.1016/j.addbeh.2004.08.023. [DOI] [PubMed] [Google Scholar]
- Yong HH, Borland R, Thrasher JF, Thompson ME, Nagelhout GE, Fong GT, Hammond D, Cummings KM. Mediational pathways of the impact of cigarette warning labels on quit attempts. Health Psychol. 2014;33(11):1410–1420. doi: 10.1037/hea0000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.