Abstract
Background:
Hip fractures are common in the elderly and are likely to become more prevalent as the US population ages. Early functional status is an indicator of longer term outcome, yet in-hospital predictors of functional recovery, particularly time of surgery and composition of support staff, after hip fracture surgery have not been well studied.
Methods:
Ninety-nine consecutive patients underwent hip fracture surgery by a single surgeon between 2009 and 2013. Surgery after 48 hours was deemed as surgical delay, and surgery after 5 pm was deemed as after hours. Surgical support staff experience was determined by experts from our institution as well as documented level of training. Functional status was determined by independent ambulation on postoperative day (POD) 3.
Results:
On POD3, 48 (79%) of 62 patients with no delay were able to ambulate, whereas only 14 (38%) of 37 patients with delayed surgery were able to ambulate (P < .001). This relationship persisted when adjusted for American Society of Anesthesiologist classification. No delay in patients older than 80 (odds ratio [OR], 6.91; 95% confidence interval [CI], 2.16-22.10) and females (OR, 7.05; 95% CI, 2.34-21.20) was associated with greater chance of early ambulation. After-hours surgery was not associated with ambulation (P = .35). Anesthesiologist and circulating nurse experience had no impact on patient’s ambulatory status; however, nonorthopedic scrub technicians were associated with worse functional status (OR 7.50; 95% CI, 1.46-38.44, P = .01).
Conclusion:
Surgical delay and nonorthopedic scrub technicians are associated with worse early functional outcome after hip fracture surgery. Surgical delay should be avoided in older patients and women. More work should be done to understand the impact of surgical team composition on outcome.
Keywords: geriatric trauma, trauma surgery, time to surgery, rehabilitation
Introduction
Hip fracture is one of the most common forms of injury among elderly patients with more than 340 000 occurring in the United States annually.1 Despite advances in surgical technique, implant technology, and rehabilitation, 1-year mortality after hip fracture surgery ranges from 14% to 36%.2 The primary goal of hip fracture surgery is to return patients to their premorbid level of function. For those who were ambulatory prior to their injury, health care providers aim for the patient to recover mobility early postoperatively. Patients who achieve ambulation in the early postoperative period have improved function at 2 months and greater long-term survival.3,4
Prompt surgical care following hospital admission for a hip fracture is associated with improved outcome. In particular, operative delay beyond 24 to 48 hours has been associated with increased rates of mortality, morbidity, postoperative complications, uncontrolled pain, new-onset delirium, pressure ulcers, and longer hospital stays.5–8 Fewer studies have evaluated the association between surgical timing and functional outcomes for patients with hip fracture. Although some studies suggest improved functional outcome with early surgical intervention,9–11 others have reported conflicting results.12,13
In addition, the relationship between the time of day when hip fracture surgery is performed and surgical outcomes has not been clearly elucidated. While researchers have hypothesized that inexperience of surgical support staff, surgeon fatigue, and limited resources during after-hours operations may lead to suboptimal surgical outcomes, results of recent studies suggest that in-house and postdischarge complications as well as mortality are comparable regardless of the time of surgery.14,15 However, there is a paucity of data regarding functional outcome of patients undergoing daytime versus after-hours surgery.
It is not yet established whether surgical delay and surgical time of day are associated with early functional outcome and time to ambulation. The purpose of the current study was to determine whether surgical delay greater than 48 hours, time of day of surgery, and/or experience level of surgical support staff (anesthesia, nursing, and technician) were associated with early ambulation as a marker of early functional outcome. Surgical support staff can be associated with perioperative outcomes and as such can play a theoretical role on functional outcome.
Materials and Methods
Data Collection
Our analysis consists of 99 patients undergoing repair for hip fracture at a tertiary care academic institution from 2009 through 2013. All patient care was provided through the Medical Orthopaedic Trauma Service (MOTS), and all patients underwent similar surgical protocols. The MOTS program is a multidisciplinary team model for fragility fractures implemented in 2008. As part of this program, patients are comanaged by the Departments of Internal Medicine and Orthopaedic Surgery with a dedicated physician extender assigned to each patient. The senior author operated on all patients. Patients admitted to the MOTS program are incorporated into an institutional database in which data are prospectively collected and tracked. This database was retrospectively reviewed for data points of interest. Institutional Review Board approval was obtained prior to initiation of the study.
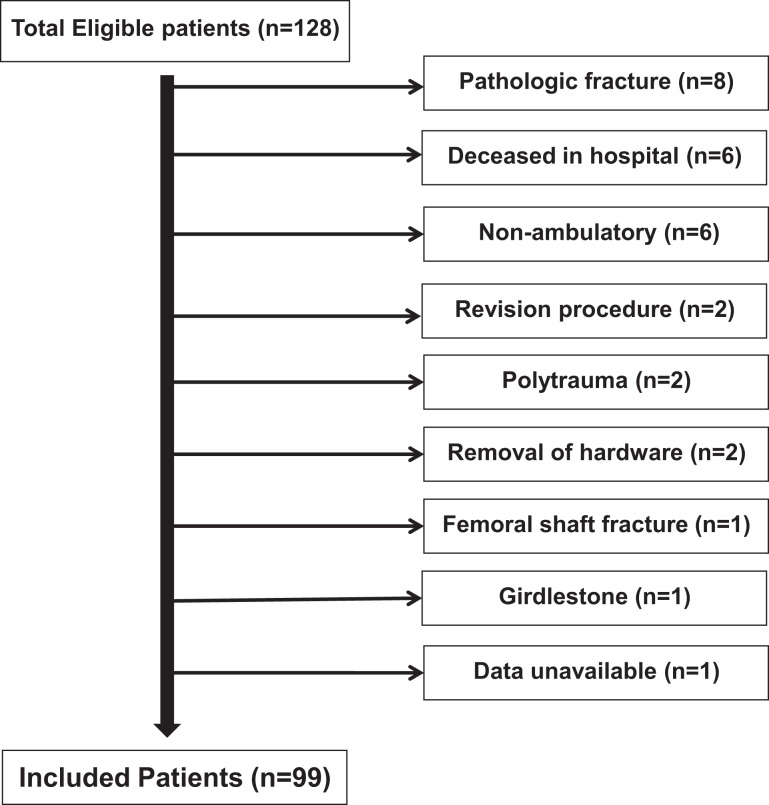
Initially, 128 patients undergoing hip fracture repair were identified during this period, and 29 were excluded due to pathologic fracture, polytrauma, unavailable data, nonambulatory status prior to fracture, girdlestone procedure, removal of hardware, femoral shaft fracture, or revision procedure. Thus, the remaining 99 were included in the analyses (Figure 1).
Figure 1.
Flowchart illustration of patient exclusion.
Patients were assigned to the no delay of surgery group if the time from admission to the inpatient unit and surgery was less than 48 hours and were assigned to the delay of surgery group if this time was greater than 48 hours. To determine the reason for delay of surgery, charts were reviewed and delays were designated as due to “medical reasons” or “nonmedical reasons.” Delay of surgery was classified as due to medical reasons if surgery was delayed pending medical clearance for any reason. If delay was due to family, social, administrative, or scheduling conflicts, or if no medical reason was evident, then delay was classified as due to nonmedical reasons.
Patients who underwent operation (as determined by operation start time) between 6 am and 5 pm on weekdays were considered to be in the daytime surgery group and those undergoing operation between 5 pm and 6 am on weekdays or any time on weekends were considered to be in the after-hours surgery group. These definitions were based on evaluation of prior literature on the topic7,8,11,13,15,16 and the normal operating times at our hospital. Patients were assigned an American Society of Anesthesiologists (ASA) score by the anesthesiologist prior to each procedure. The ASA scores for 4 patients were not recorded at the time of surgery and therefore were not included in subanalyses of delay of surgery stratified by ASA. These patients were included in analyses of time of day of surgery and experience of surgical support staff analyses.
Physical therapy notes were reviewed and ambulatory status including the number of feet and steps walked for each postoperative day (POD) until discharge were recorded. Per hospital protocol, physical therapists aim to have patients with hip fracture begin ambulation on POD1. Time to ambulation was considered to be the first day that the patient was able to walk 2 or more feet independently. Patients who were able to ambulate by POD3 were classified as achieving early ambulation and those who walked after day 3 or who were unable to ambulate during their hospital stay were not considered to have achieved early ambulation.3,4
Anesthesiologists were classified as orthopedic anesthesiologists or nonorthopedic anesthesiologists. This classification was performed in a blinded fashion by a single member of the orthopedic anesthesiologist team based on training level of the anesthesiologist as frequency of work with the orthopedic trauma team. Nursing staff was classified into 2 categories based on training, experience, and prior surgical procedures with an orthopedic service. Surgical technicians were similarly classified into 2 categories based on training, experience, and assignment to orthopedic service.
Statistical Methods
All demographic data were analyzed descriptively. Independent categorical data were assessed using contingency tables to test for differences by the chi-square test. Fischer exact test was used for contingency tables with less than 5 values in a given cell. Normally distributed independent continuous variables were tested for differences using the independent sample t test.
Mann-Whitney U test was used to identify differences in length of stay between delay and no delay groups due to the presence of outliers in the sample. A P value of <.05 in 2-sided hypothesis testing was considered significant. Data analyses were conducted using SPSS 18 software package (IBM, Portsmouth, United Kingdom).
Results
Characteristics of our study population are presented in Table 1. The patient population in our study included 99 patients (27 males and 62 females). The mean age (± standard deviation) of our cohort was 79.5 years (±12.6). The mean ASA of our cohort was 2.8 (±0.59), and the majority of patients were in ASA class 3-4 (70.7%). There were 62 patients without surgical delay after their hip fracture, and there were 72 patients in the daytime surgery group. We stratified patient characteristics based on time to surgery and time of day when surgery was performed (Table 2).
Table 1.
Baseline Characteristics of Patients.
| Demographics | Total patients (N = 99) |
|---|---|
| Sex | |
| Male | 27 |
| Female | 62 |
| Age | 79.5 (±12.6) |
| ASA grade | |
| 1-2 | 25 |
| 3-4 | 71 |
| Type of fracture | |
| Subcapital | 9 |
| Subtrochanteric | 1 |
| Femoral neck | 63 |
| Intertrochanteric | 24 |
| Basicervical | 2 |
Table 2.
Patient Characteristics Stratified by Timing of Surgery.a
| Demographics | Delay of surgery | Time of day | ||
|---|---|---|---|---|
| No delay | Delay | Daytime | After hours | |
| Sexb | ||||
| Male | 14 (23) | 13 (35) | 20 (28) | 7 (26) |
| Female | 48 (77) | 24 (65) | 52 (72) | 20 (74) |
| Agec | 78 ± 12 | 82 ± 14 | 79 ± 12 | 82 ± 13 |
| ASA gradeb | ||||
| 1-2 | 18 (30) | 7 (19) | 21 (31) | 4 (15) |
| 3-4 | 41 (70) | 29 (80) | 47 (69) | 23 (85) |
| Arthroplastyb | 40 (65) | 28 (76) | 52 (72) | 16 (59) |
| Type of fractureb | ||||
| Subcapital | 7 (11) | 2 (5) | 6 (8.3) | 3 (11) |
| Subtrochanteric | 1 (2) | 0 (0) | 1 (1) | 0 (0) |
| Femoral neck | 34 (55) | 29 (78) | 49 (68) | 14 (52) |
| Intertrochanteric | 19 (31) | 5 (14) | 14 (19) | 10 (37) |
| Basicervical | 1 (2) | 1 (3) | 2 (3) | 0 (0) |
aThere were no significant p values for any of the comparisons.
bThe values are given as the number of patients with the percentage in parentheses.
cThe values are given as the mean and the standard deviation in years.
Delay of Surgery
At POD3, 48 (77%) of 62 patients with no delay of surgery were able to ambulate at least 2 feet, whereas 14 (38%) of 37 patients who had delayed surgery were able to ambulate at this time point (P < .001; Table 3). Patients with ASA 1 and 2 were significantly more likely to achieve early ambulation if operated on within 48 hours (odds ratio [OR], 12.75; 95% confidence interval [CI], 1.03-157.14, P = .05). Similarly, operation within 48 hours was associated with a greater likelihood of early ambulation for patients with ASA 3 or 4 (OR, 5.95; 95% CI, 2.07,-16.99, P < .01). Thus, early surgery was predictive of good functional outcome even when stratified by ASA class. Operation within 48 hours was also associated with a greater likelihood of ambulation in patients aged 81 years and older (OR, 6.91; 95% CI 2.16-22.10; P < .01) and females (OR, 7.05; 95% CI 2.34-21.20; P < .01).
Table 3.
Effects of Operative Delay, Time of Surgery, Surgical Staff Experience and ASA on Early Ambulation.
| Ambulation by POD3 Odds ratio (95% confidance interval) | P value | |
|---|---|---|
| No. delay of surgery | 5.50 (2.25-13.47) | <.01 |
| ASA 1-2 | 12.75 (1.03-157.14) | .05 |
| ASA 3-4 | 5.95 (2.07-16.99) | <.01 |
| 80 years or younger | 3.125 (0.523-18.70) | NS |
| 81 years or older | 6.909 (2.16-22.10) | <.01 |
| Male | 5.14 (0.81-32.77) | NS |
| Female | 7.05 (2.34-21.20) | <.01 |
| Daytime surgery | 1.71 (0.69-4.219) | NS |
| Anesthesiologist | 1.47 (0.62-3.50) | NS |
| Circulating Nurse | 1.68 (0.56-5.13) | NS |
| Scrub Technician | 7.50 (1.46-38.44) | <.01 |
| ASA 1-2 | 3.94 (1.22-12.68) | .02 |
Abbreviation: NS, Not significant.
Of the 37 patients with delay of surgery, 30 (81%) of were delayed due to medical optimization prior to surgery. Medical issues that required delay of surgery included but were not limited to cardiac conduction abnormalities requiring telemetry or repeat electrocardiograms, elevated international normalized ratio, and electrolyte or fluid status abnormalities. The remaining 6 (17%) were delayed due to nonmedical reasons, such as awaiting family discussions as well as arranging postoperative living arrangements. Subanalysis of patients with delay of surgery showed that the average time from medical optimization to surgery for all patients was 19 hours and 21 minutes.
Time of Day of Surgery
Forty-nine (68%) of 72 patients undergoing operation in daytime, nonweekend hours, were able to ambulate by POD3, compared to 15 (55%) of 27 patients with operations during after hours (P = .35, Table 3).
Surgical Support Staff Experience Level
Experience level of anesthesiologists and circulating nurses were not associated with early ambulation (P = .50 and P = .39, respectively). Scrub technician experience level was significantly associated with ambulatory status on POD3 (OR 7.50; 95% CI, 1.46-38.44; P = .01). Sixty (68%) of 88 patients undergoing surgery with orthopedic scrub technicians and 2 (22%) of 9 patients with nonorthopedic scrub technicians ambulated by POD3 (Table 3). The mean surgical time in these 9 cases was 124.8 minutes (compared to 118.3 minutes for all patients). Post hoc, we hypothesized that there may have been technical factors relating to poor outcome in these patients. We hand matched these 10 patients (cases) to 10 other patients (controls) using gender, age (± 5 years), and type of hip fracture. We were unable to perform a 1:2 case–control match. The mean ASA class in cases versus controls was 2.5 versus 2.78, respectively. We reviewed operative and post anesthesia care unit (PACU) notes for all 20 patients. There were no recorded intraoperative complications in all 20 cases. In the PACU, 5 of the 10 patients had recorded events: 2 patients had hematocrits less than 20 requiring transfusion, 2 patients were hemodynamically unstable and required an unplanned transfer to a monitored floor, and 1 patient had a wound hematoma requiring compressive dressing. One control patient had atrial fibrillation that responded to beta blockade. Cases were more likely to experience an event in the PACU but this did not reach significance (P = .07).
Baseline Operating Room and Hospital Data
The median waiting time for surgery from admission was 57.1 hours (range: 2.57-346 hours; mean: 57 hours). The mean waiting time in the no delay group was 29.3 hours (range: 2.57-47.6 hours), and the mean waiting time in the delay group was 105 hours (range: 48.0-346 hours). In the delay group, the mean surgical time from incision to closure was 119 minutes (SD: ±41.6) and 120 minutes (±45.1) for the no delay group (P = .90). The mean time of anesthesia was 233 (±70.4) minutes for the delay group and 236.3 (±68.6) minutes for the no-delay group (P = .67).
The mean length of stay after surgery was 5.94 (±2.73) days for the no-delay group and 7.89 (±6.23) days for the delay group (P = .08). Length of stay was defined as the length of time between the end of surgery and discharge to eliminate delay prior to surgery as a confounding variable.
There was no difference in length of stay between delay and no delay groups in patients with ASA of 1 to 2 (P = .48). In patients with ASA of 3 to 4, there was a trend toward lesser length of stay for patients with no delay, but this was not statistically significant (P = .08). Similarly, there was no significant difference in intraoperative blood loss observed between ASA stratified delay and no-delay groups (Table 4). Operating room and hospital data relating to daytime versus nighttime surgery are presented in Table 5.
Table 4.
The Impact of Surgical Delay Beyond 48 Hours on Surgical Factors.
| <48 hours (N = 62) | >48 hours (N = 27) | P value | |
|---|---|---|---|
| Surgical time, min | 119 (±41.6) | 120 (±45.1) | .90 |
| Anesthesia time, min | 233 (±70.4) | 236.3 (± 68.6) | .83 |
| Blood loss, mL | 230 (±117) | 250 (±163) | .49 |
| ASA 1-2 | 218 (±126) | 264 (±94.5) | .39 |
| ASA 3-4 | 234 (±114) | 244 (±175) | .78 |
| Length of stay, days | 5.94 (±2.73) | 7.89 (±6.23) | .08 |
| ASA 1-2 | 5.47 (±2.35) | 4.71 (±2.29) | .48 |
| ASA 3-4 | 6.15 (±2.89) | 8.50 (±6.60) | .08 |
Table 5.
The Impact of Surgery After Hours on Surgical Factors.
| Daytime (N = 70) | After Hours (N = 29) | P value | |
|---|---|---|---|
| Surgical time, min | 125 (±42.5) | 104 (±39.4) | .03 |
| Anesthesia time, min | 244 (±67.2) | 205 (±67.8) | .01 |
| Blood loss, mL | 229 (±149) | 202 (±120) | .40 |
| ASA 1-2 | 223 (±121) | 225 (±119) | .91 |
| ASA 3-4 | 247 (±144) | 217 (±131) | .43 |
| Length of stay, days | 6.63 (±4.50) | 6.72 (±4.32) | .93 |
| ASA 1-2 | 4.94 (±2.32) | 6.40 (±2.07) | .22 |
| ASA 3-4 | 7.25 (±4.96) | 6.85 (±4.76) | .76 |
Discussion
Perioperative management plays an important role in determining success rates of surgery and has led to drastic improvements in the clinical pathways for surgical patients over the past few decades. The purpose of this study was to determine the impact of operative timing (time to surgery and time of day) and support staff variables on functional outcome after hip fracture surgery. We found that delay of surgery beyond 48 hours compromises short-term functional recovery regardless of patient comorbidity. We also found that surgical support staff composition may affect outcomes.
Results from this study should be interpreted in the context of a number of study limitations. First, the retrospective nature of this study makes it susceptible to reporting bias. This also prevents assessment of potentially confounding variables such as time of fracture, which would allow correction for preadmissions delay. Second, long-term clinical outcome data were not available due to the retrospective study design; however, the goal of this study was to evaluate in-hospital functional recovery as a surrogate for longer term function. Community-based studies may help to better understand the factors associated with improved function in patients with hip fracture after discharge from the hospital. Third, single-institution studies such as this one have decreased generalizability, as previous literature has shown interinstitutional differences in clinical outcomes of hip fractures. However, because of the single surgeon study design, variance in surgical technique is reduced and an important confounder of functional recovery is eliminated. Finally, because this study was retrospective, we relied on physical therapy notes to determine ambulatory status. Future studies on this topic would benefit from use of a more comprehensive assessment of postoperative recovery, such as the motor portion of the Functional Independence Measure (FIM) scale. The FIM is an instrument used to evaluate physical functioning of a patient based on assessments of locomotion, self-care, and transferring.
The results of this study indicate that delay of hip fracture surgery beyond 48 hours negatively impacts functional outcome without affecting other variables related to poor outcome in this study (length of stay or intraoperative blood loss). Previous studies have investigated the effect of early surgery on mortality and complications, however the impact of early surgery on functional recovery is largely unknown.8,13,17 In a prospective cohort study, Orosz et al13 found that patients undergoing surgery within 24 hours showed improved self-care capacity but no improvement in locomotion at 6 months as measured by the FIM scale. Other studies have concluded that patients undergoing early operation recover weight-bearing capacity at earlier times, return to independent living conditions more frequently, and show improved activities of daily living scores.5,9 Our results are consistent with these latter findings and suggest that early surgery increases the likelihood of early ambulation when accounting for the severity of systemic illness with ASA classification. Surgery prior to 48 hours is generally accepted as the preferred strategy for hip fractures,18 and we suggest that functional gains from early ambulation and return of function contribute to the benefits associated with early surgery after hip fractures.
Reasons for these surgical delays can be medical or nonmedical. Previous reports indicate that delay of hip fracture repair are more often due to medical issues such as stabilizing for comorbid diseases, improving INR coagulation rating, discontinuing metformin use, and controlling arrhythmias and heart disease than delay due to administrative issues or family discussions.13,19 Still 5% to 29% may be due to nonmedical factors.20–22 In the current study, 17% of the surgical delays were due to nonmedical reasons, illustrating an opportunity to further improve efficiency to expedite surgery after admission.
In this study, the time of day for surgery did not influence functional outcome or other perioperative markers of poor outcome. In a prior study, Ricci et al16 found that there is an increased risk of unplanned reoperation and removal of painful hardware during after-hours hip fracture surgery when compared to day time surgery. Chacko et al14 found that utilization of a dedicated trauma room during the day time was associated with decreased mortality risk compared to after-hours surgery. However, in the absence of a dedicated trauma room, there was no significant difference in mortality between day time and nighttime surgery. Only 1 prior study has investigated the impact of after-hours surgery on functional status—Rashid et al15 found that time of day for hip fracture surgery was not associated with early functional outcome. Our study confirms this previous finding using rigorous chart analysis and risk stratification. After-hours surgery is sometimes necessary, as patients who have severe or unstable injuries or medical conditions may require emergent surgery outside the ideal operating times.
The experience level of anesthesiologists and circulating nurses were not associated with differences in patient recovery. However, the assistance of a dedicated orthopedic scrub technician was associated with a greater likelihood of early ambulation after surgery compared to a nonorthopedic scrub technician. Subgroup analysis showed that nonorthopedic scrub technician-assisted cases were longer on average and more prone to complication in the PACU. Although there were no noted technical complications, the recorded incidents relating to blood transfusion, hemodynamic instability, and wound breakdown may be related to technical factors relating to suboptimal intraoperative assistance. Two prior studies prospectively observed the impact of intraoperative behaviors on patient outcome. Catchpole et al23 observed 42 procedures (including 18 orthopedic procedures) and evaluated the efficacy of team performance using a scoring system employed for teamwork assessment in the airline industry. The authors found that although all procedures had successful outcome, there were “latent failures” that could have potentially lead to patient harm. Specific to orthopedic surgery, the authors identified equipment problems and the absence of procedure-specific instrumentation as being particularly disruptive to effective team performance. This finding may explain why in our study nonorthopedic scrub technicians were associated with worsened outcome, whereas nonorthopedic circulating nurses and nonorthopedic anesthesiologists had no significant impact on outcome. Another study on the topic found that for 293 prospectively observed surgeries, team practices such as poor handoff, lack of contingency management, inaccurate information sharing, and incomplete briefing can lead to increased risk of 30-day complication and mortality.24 The power of this sample is significantly limited with only 9 cases with an inexperienced scrub technician were included, but the finding suggests further investigation is necessary to understand how the composition of an orthopedic team influences patient outcome.
Based on our findings, patients with hip fracture should undergo operation within 48 hours to allow for the greatest chance of early ambulation. After-hours surgery should be considered for patients who may benefit from surgery within 48 hours from admission. Cases with hip fracture should be staffed with scrub technicians who are experienced in orthopedic-specific procedures.
Acknowledgments
We thank Kara Gasriorowski for assisting in classifying the experience level of the nursing staff. We also thank Ana Urso for reviewing physical therapy data and Jin Chen for performing data collection.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Matthew R. Cohn, BS; Guang-Ting Cong, BS; Benedict U. Nwachuckwu, MD, MBA; Minda L. Patt, MD; and Lester Zambrana, BA have declared that they have no conflict of interest. Joseph M. Lane, MD reports personal fees from Agnovos, Bone Therapeutics SA, Graftys, Merk, Harvest, ISTO, Kuros, CollPlant Ltd., BiologicsMD, RoyalPainMD, outside the work.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Blackman DK, Kamimoto LA, Smith SM. Overview: surveillance for selected public health indicators affecting older adults--United States. MMWR CDC Surveill Summ. 1999;48(8):1–6. [PubMed] [Google Scholar]
- 2. Zuckerman JD. Hip fracture. N Engl J Med. 1996;334(23):1519–1525. [DOI] [PubMed] [Google Scholar]
- 3. Oldmeadow LB, Edwards ER, Kimmel LA, Kipen E, Robertson VJ, Bailey MJ. No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ J Surg. 2006;76(7):607–611. [DOI] [PubMed] [Google Scholar]
- 4. Siu AL, Penrod JD, Boockvar KS, Koval K, Strauss E, Morrison RS. Early ambulation after hip fracture: effects on function and mortality. Arch Intern Med. 2006;166(7):766–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Al-Ani AN, Samuelsson B, Tidermark J, et al. Early operation on patients with a hip fracture improved the ability to return to independent living. A prospective study of 850 patients. J Bone Joint Surg Am. 2008;90(7):1436–1442. [DOI] [PubMed] [Google Scholar]
- 6. Hapuarachchi KS, Ahluwalia RS, Bowditch MG. Neck of femur fractures in the over 90 s: a select group of patients who require prompt surgical intervention for optimal results. J Orthop Traumatol. 2014;15(1):13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rodriguez-Fernandez P, Adarraga-Cansino D, Carpintero P. Effects of delayed hip fracture surgery on mortality and morbidity in elderly patients. Clin Orthop Relat Res. 2011;469(11):3218–3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995;77(10):1551–1556. [DOI] [PubMed] [Google Scholar]
- 9. Doruk H, Mas MR, Yildiz C, Sonmez A, Kyrdemir V. The effect of the timing of hip fracture surgery on the activity of daily living and mortality in elderly. Arch Gerontol Geriatr. 2004;39(2):179–185. [DOI] [PubMed] [Google Scholar]
- 10. Fox HJ, Pooler J, Prothero D, Bannister GC. Factors affecting the outcome after proximal femoral fractures. Injury. 1994;25(5):297–300. [DOI] [PubMed] [Google Scholar]
- 11. Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87(8):1123–1126. [DOI] [PubMed] [Google Scholar]
- 12. Cree AK, Nade S. How to predict return to the community after fractured proximal femur in the elderly. Aust N Z J Surg. 1999;69(10):723–725. [DOI] [PubMed] [Google Scholar]
- 13. Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291(14):1738–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chacko AT, Ramirez MA, Ramappa AJ, Richardson LC, Appleton PT, Rodriguez EK. Does late night hip surgery affect outcome? J Trauma. 2011;71(2):447–453; discussion 53. [DOI] [PubMed] [Google Scholar]
- 15. Rashid RH, Zubairi AJ, Slote MU, Noordin S. Hip fracture surgery: does time of the day matter? A case-controlled study. Int J Surg. 2013;11(9):923–925. [DOI] [PubMed] [Google Scholar]
- 16. Ricci WM, Gallagher B, Brandt A, Schwappach J, Tucker M, Leighton R. Is after-hours orthopaedic surgery associated with adverse outcomes? A prospective comparative study. J Bone Joint Surg Am. 2009;91(9):2067–2072. [DOI] [PubMed] [Google Scholar]
- 17. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87(3):483–489. [DOI] [PubMed] [Google Scholar]
- 18. Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40(7):692–697. [DOI] [PubMed] [Google Scholar]
- 19. Fantini MP, Fabbri G, Laus M, et al. Determinants of surgical delay for hip fracture. Surgeon. 2011;9(3):130–134. [DOI] [PubMed] [Google Scholar]
- 20. Charalambous CP, Yarwood S, Paschalides C, Siddique I, Hirst P, Paul A. Factors delaying surgical treatment of hip fractures in elderly patients. Ann R Coll Surg Engl. 2003;85(2):117–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Muhm M, Klein D, Weiss C, Ruffing T, Winkler H. Mortality after proximal femur fracture with a delay of surgery of more than 48Â h. Eur J Trauma Emerg Surg. 2014;40(2):201–212. [DOI] [PubMed] [Google Scholar]
- 22. Petermann A, Tadvi J, Calthorpe D. Does Early Surgery Improve the Outcome of Hip Fracture Surgery? A Prospective Study. J Bone Joint Surg. 2003;85-b(suppl 1):37. [Google Scholar]
- 23. Catchpole KR, Giddings AE, Wilkinson M, Hirst G, Dale T, de Leval MR. Improving patient safety by identifying latent failures in successful operations. Surgery. 2007;142(1):102–110. [DOI] [PubMed] [Google Scholar]
- 24. Mazzocco K, Petitti DB, Fong KT, et al. Surgical team behaviors and patient outcomes. Am J Surg. 2009;197(5):678–685. [DOI] [PubMed] [Google Scholar]