Abstract
Background:
Early identification of hip fracture (HF) patients bearing an increased risk for a contralateral occurrence would allow providing preventive measures timely.
Objectives:
To summarize the available evidence describing risk scores, prognostic instruments, or (groups of) parameters predicting contralateral HFs at the time point of the first fracture. Methods/Systematic Review: Articles were identified through searches in MEDLINE and Scopus from inception to April 2014, checking of reference lists of the included studies and reviews. One reviewer assessed all articles for inclusion and abstracted the data. Uncertain cases were discussed and decided with a second reviewer. Salient study and population characteristics were abstracted for each article. Studies reporting the association of a set of risk factors for second HFs were further examined and compared. The number of studies reporting on a risk parameter was assessed.
Results:
Searches identified 3560 records, and 47 studies were included in this review. There was a large spectrum of study designs, patient populations, and follow-up periods. Among 11 studies reporting on a set of parameters, female gender was assessed most commonly (7 times), followed by age (5) and parameters of general health, vision, and stroke (each 4 times). We were unable to depict stringent patterns of risk parameters to be used for decision making in clinical practice.
Conclusions:
The findings of this article call for a conjoint effort to achieve an expert consensus regarding a critical set of parameters for a risk instrument identifying patients bearing an increased risk for contralateral HFs early.
Keywords: contralateral hip fractures, osteoporosis, geriatrics, risk prediction, systematic review
Introduction
Contralateral hip fractures (HFs), particularly among elderly patients, are common and associated with poor prognosis.1 Identifying patients at the time point of the first fracture bearing a substantially increased risk for contralateral HFs would allow planning therapeutic measures on the occasion of the fixation of the first fracture. Besides pharmacologic interventions, surgical treatments should then be considered.2
However, such an invasive approach would only be justified if this group of patients could be selected and described accurately. Unfortunately, the literature reporting the parameters pointing at an increased risk is scattered and not easy to access.2 Clinical experience teaches us that a previous HF is one of the strongest predictors for the next one. But, additional factors may further influence the risk for the next HF. Ideally, a simple algorithm that allows assessing the individual risk for a contralateral HF immediately prior to fixation surgery of the acquainted one should be available.
Using up-to-date systematic review methods, this article identifies and assesses the available evidence and provides an inventory of parameters found to be associated with an increased risk for contralateral HFs.
Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline,3 and the protocol was registered at PROSPERO (CRD42014008972).
Eligibility
We aimed to find articles assessing at least 1 risk parameter at the time of the first fracture and its association with contralateral HFs. Studies were excluded if the type of first or second fracture was not clearly defined, risk factors for first HFs or mortality were investigated exclusively, or incidence of second HFs revealed only. We further excluded studies comparing first to second HFs in the same patient group, as these would not support finding a patient group at risk for second HFs.4–6 One study was not available for full-text review and therefore excluded.7
Identification of Reports
Systematic searches were performed from inception in (pre-) MEDLINE and Scopus. The date of the last search was April 2014. The MEDLINE search is available in Appendix A.
Study Selection
After abstract and title scan, we included studies with German or English language full-text and those mentioning second HFs (also referred to as “contralateral,” “non-simultaneous,” “bilateral,” or “subsequent” “proximal femur” or “proximal femoral” fractures) in elderly patients. Studies with focus on pathological (cancer related or secondary to bisphosphonate treatment), periprosthetic, ipsilateral, or simultaneous bilateral fractures were excluded. Case studies and those referring to HFs as risk factor for other events were also excluded. In 2 studies, abstracts were not available. Therefore, we proceeded to full-text scanning directly. However, both studies did not meet our inclusion criteria.
Data Collection
After eliminating 18 duplicates, both search approaches together revealed 76 articles qualifying for full-text scanning. The main inclusion criteria after full-text review were the presence of at least 1 risk factor or 1 parameter that was compared between patients with and without second HF.
Data Extraction and Summary
Forty-seven articles fulfilled our inclusion criteria and were classified into 3 groups. “Group A” comprises studies revealing a set of risk factors for second HFs. This systematic review targeted at this specific group of articles. Studies of “group B” described to what extent risk parameters differed between groups of patients with a first HF and a second HF. Finally, some studies reported incidence ratios of second HFs in relation to a general population risk for first HF, mainly with standardized incidence rate ratios. Those studies were summarized in “group C.”
Other studies in contrary had looked for previous HF in a cohort of HF patients or investigated risk factors years after the first HF. Some were not defining the time of investigation in detail or allocated patients twice in 1 and 2 HF groups. Randomized controlled studies, matched control group, and intervention cohort studies do not reflect populations at risk and were therefore also not evaluated in group A.
We abstracted parameters that were assessed with similar methods to facilitate comparisons. For example, “functional status and ambulation” was measured by “time on feet < 4 h/d,” “using arms to stand,” “walking speed (m/s),” “using walking aids,” “difficulties standing up/walking up stairs,” and another 11 parameters for group A.
A statistical summary of the exiting evidence was attempted but impossible due to the large variation between individual studies in terms of patients selection, design, and statistical analysis.
Results
Study Selection
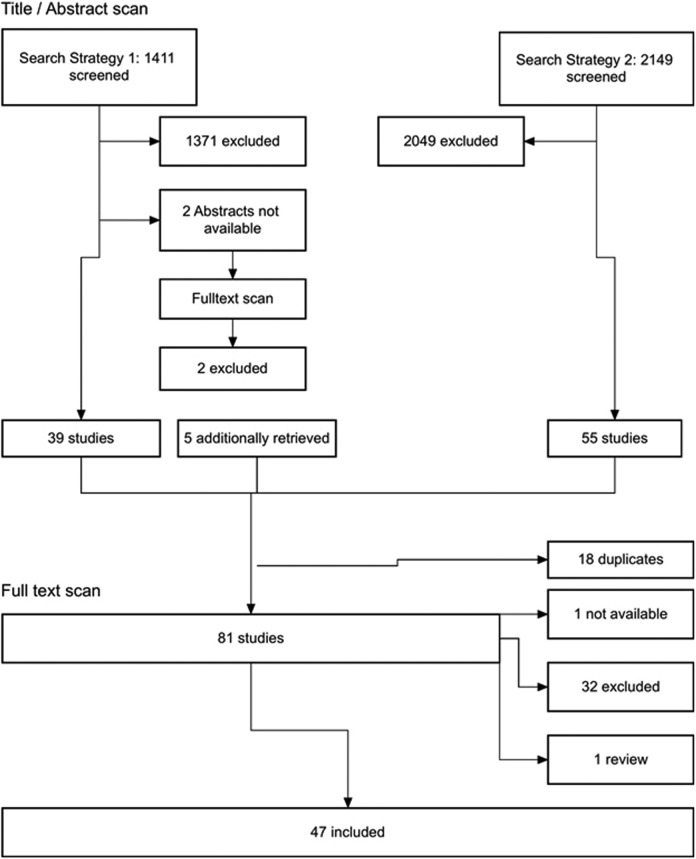
Searches identified 3560 records, of which, after applying the reported selection criteria, 47 articles qualified for inclusion in this review. The detailed selection process is shown in Figure 1.
Figure 1.
Flow chart of the study selection.
In group A, we classified 11 studies1,8–17 (for details, see Table 1), group B contains 5 studies18–22 (see Table 2), and 31 reports went into group C23–51 (for details, see Table A1).
Table 1.
Summary of Studies of Group A.
| Reference | Study design | Study intention | Location | Participants | Age, mean (SD) | Exclusion and deaths | Follow-up time | Time point of factors measured | Time frame observed for second fracture to occur | n, percentage/incidence of second HF | Interval between first and second HF |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chapurlat et al11 | Population-based prospective cohort study (Study of Osteoporotic Fracture [SOF]) | “Examine incidence of and risk factors for a second HF in elderly women” | 4 clinical centers in Portland, Oregon, Minneapolis, Minnesota, Baltimore, Maryland, and Pennsylvania, USA | SOF: non-black women ≥65 years, 1986-1988 = baseline, 632 patients with HF for analysis | Baseline 1 HF group: 75 ± 6, baseline 2 HF group: 75 ± 5 | Exclusion: severe trauma, unable to walk without assistance, bilateral hip replacement, previous HF, deaths including ipsilateral HF | 3.7 years (mean) | Before first HF (1986-1988) | 0-6.8 years | n = 53/632, incidence 0.023/py | 2.3 yr (mean), 6.8 years maximum |
| Berry et al10 | Population-based prospective follow-up cohort study (Framingham Heart Study) | “timing, incidence, risk factors, and mortality associated with second HF” | Framingham, Massachusetts | Framingham Heart Study: 5209 patients. 28-62 years in 1948, 481 first HF patient. April 1952 to December 2003: 178 participants in final model | Baseline 1 HF group: 80.3 ±9.5, baseline 2 HF group: 77.2 ± 10.2 | Exclusion: periprosthetic deaths: 15.9% in 1 year, 45.4% within 5yrs | 4.2 years (IQR, 1.4-8.9) until 2003/second HF/death | Closest to and preceding first HF | 0-52 years | n = 15/89 (analysis) 14.8%, 2.3/100 py, 2.5% at 1 year, 5.7% at 3 years, 8.2% at 5 years, cumulative incidence for second HF/death (accounting for variable length of follow-up, competing risk of death): 0.5 years 1.0/11.9, 1 year 2.5/15.9, 2 years 4.2/24.8, 3 years 5.7/33.6, 5 years 8.2/45.4, 10 years 12.2/72.4 | 4.2 years (median), range: 1 month to 33.3 years |
| Mitani et al14 | Retrospective case record study | “Elucidate the risk factors for second HF” | Shimizu Hospital, Tottori Prefecture, Japan | 400 HF patients, 384 for analysis, index HF January 2001 to December 2007 | 83.1 ± 9.0 (range: 51-102) | Exclusion: pathological HF, high-impact trauma, death within 1 year (n = 11), <50 years (n = 5), | 3.0 ± 1.4 years (mean) | First HF | 0-7 years | n = 49/384, overall incidence of 0.043/py | 21 months (median), 23.5 ± 13.7 (mean), 40.8% 1 year, 67.3% 2 years, 85.7% 3 years |
| Yamanashi et al17 | Prospective follow-up cohort study | “clarify the risk factors for a second HF in patients who had had a previous HF” | 4 hospitals, Japan | 820 HF patients ≥ 65 years, 714 for analysis (1579.5 py), inclusion: January 1996 to December1999 | First HF: 80.7 ± 7.6 years (range 65-99 years) | Exclusion: (106) pathological fracture, high-energy trauma | 2.4 ± 1.4 yr (mean) until September 2001/second HF/death | First HF | 23-71 months | 45/714, incidence 0.029/py, annual incidence: first year 0.038/py, during the second year 0.028/py, during 3rd yr 0.018/py | 44% in 8 months |
| Holt et al12 | Prospective national multicentric audit Scottish Hip Fracture Audit | “Incidence, epidemiology, and outcomes of sequential HF” | All 22 orthopedic hospitals, Scotland, United Kingdom | 28 392 HF patients > 50 years January 1998 to December 2005, 20 267 patients for analysis, 13 874 1-year surviving patients for analysis | 2 HF group: 82, 1 HF group: 80 | Exclusion: 3963 within last 6 months of data collection, not matched to database (214), simultaneous HF (35), ipsilateral HF, death within 6 months of first HF, data not available at 12 months, death: 32% by 12 months (6393) | 3.9 years, maximum 8 years | First HF | 6-12 months for analysis | n = 473 (2.3%) of 20 267, n = 350 (2.5%) of surviving patients/13 874 | NG |
| Lönnroos et al13 | Hospital register and medical records review (with prospective and retrospective inclusion part) | “Review HF to determine which were primary vs secondary, determine what percent of patients with primary HF have a second HF within 2 years, describe characteristics of patients with 2 incident HF including medication use” | 27 municipalities in Central Finland Health Care District Central Finland Hospital, Finland | Prospective inclusion (first HF 2002-2003: 501 first HF patients ≥60 years), follow-up until December 2005, prospective and retrospective inclusion: 573 HF patients in 2002-2003 (41 with previous HF) | Prospective part: baseline 1 HF group: 81 (8), baseline 2 HF group: 80 (7), retrospective part: first HF: 78 (49-92), second HF: 81 (49-99) | Deaths: 230/501 without second HF | 25.5 months (median, range: 0.03-47.9) until 2005 | First HF | 2-4 years/retrospective | Prospective inclusion: n = 34/501 (6.8%), retrospective + prospective: n = 75/573 (41 with previous HF), overall incidence 0.036 (CI: 0.025-0.051)/py, cumulative incidence, 1 year 5.8% (3.30-7.78), 2 years 8.11% (5.73-11.43) | Retrospective inclusion: range 0.03-14.0 years, prospective inclusion: 2-4 year |
| Wolinsky and Fitzgerald16 | Prospective follow-up cohort study, Longitudinal Study on Aging (follow-up on the Supplement on Aging 1984 National Health Interview Survey) | “Assess the risk of subsequent HF” | United States | Start 1984: 7527 patients ≥ 70 years, 368 HF patients, 1984-1991, 27 second HF patients for analysis | 79.7 | Of 51 double billings: exclusion: 3 duplicates, 14 transfers, 7 rehospitalizations | 1984-1991, mean follow-up to death: 674 days, mean follow-up to censoring: 1132days | First HF | 0-8 years | 27/368 (7.3%), 1/33.8py | 613days (mean) |
| Ryg et al1 | Nationwide population-based historical cohort | “Studying incidence of second HF, ensuing mortality, possible impact of comorbidity” | All Danish hospitals, Denmark | 169 145 HF patients, January 1977 to December 2001 | Baseline 77.0 ± 13.0 | Exclusion: patients referred from outpatient clinics, still in hospital after index HF, deaths: 121 953 (72.1%) | 3.8 years (median, 0-25 years), 1 041 177 py, first and second HF 1977-2001 | First HF | 0-25 years | 27 834/169 145, overall incidence: 39/1000 py, cumulative incidence: 9% after 1 year | NG |
| Angthong et al8 | Medical records evaluation | “evaluate which of the predisposing risk factors for first HF would continue to be effective for the development of the second HF in the elderly” | 1 hospital, Bangkok, Thailand | 125 HF patients ≥ 55 years, inclusion: index HF January 2000 to September 2008 (first and second—contralateral—HF) | NG | Exclusion: metabolic bone disease, renal osteodystrophy, ipsilateral primary and secondary tumor lesion, simultaneous HF, bisphosphonate, calcitonin, estrogen treatment, pathological, high-energy trauma | January 2000 to September 2008 | First HF | 0-8.75 years | 28/125 | ≤12 months n = 6 (21.4%), >12 months n = 22 (78.6%) |
| Baudoin et al9 | Prospective study | “Evaluate burden of HF, whether they occurred at home or in a community, in terms of HF incidence and mortality and postoperative complications 2 years after HF” | 34 surgical units, Picardie, France | 1512 HF patients ≥20 years in December 1992 to December 1994, analysis: 1459; 567 for analysis | Community women 85 (7.2), community men 80.5 (10.2), home women 80.3 (9.2), home men 75.4 (11.0) | Exclusion: metastatic or myelomatous fracture, periprosthetic fracture for analysis: <50 years, deaths (at 2-year follow-up): 394 women, 173 men, 87% of surviving patients interviewed at 24 months | 2 years until December 1994 | First HF | 24 months | n = 52, crude incidence 2.94/100 py | NG |
| Omsland et al15 | Retrospective population-based database review | “Examine cumulative incidences of second HF by sex, age, and time after first HF” | All 48 hospitals/health trusts, Norway | 81 867 HF patients ≥50 years, January 1999 to December 2008 | NG | Exclusion: patients with previous HF between 1994 and 1998 | 1999-2008 | First HF | 0-9 years | n = 7943/81 867, crude incidence women 379/10 000 py (CI: 370-389), men 333/10 000 py (CI: 318-349) | Women: 1.5 years (0.5-3.2), men: 1.2 (0.4-2.7); median (IQR) |
Abbreviations: CI, confidence interval; HF, hip fracture; IQR, interquartile range; NG, not given; py, patient-years; SD, standard deviation.
Table 2.
Summary of Studies of Group B.
| Reference | Study design | Study intention | Location | Participants | Age, mean | Exclusions and deaths | Follow-up time | Time point of factors measured | Time frame observed for second fracture to Occur | Percentage/incidence of second HF | Interval between first and second hf | Factors assessed |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dirsch et al18 | Prospective, longitudinal study | “Determine whether accelerated loss of bone mineral continues beyond the first year after injury” | University of North Carolina Hospitals, NC, USA | 85 osteoporotic HF patients, 21 for analysis | First HF: 73.1 ± 2.0 | Dropouts: 40 deaths (47% of 1-year subgroup), 12 declined (14%), 12 moved (14%), 6-year surviving subgroup analyzed here | 6.2 years (mean, range: 67-86 months) | First HF, 12-72 months | 67-86 months | n = 5/21 (24%) | ng | BMD baseline, 1 year, 6 years |
| Gordon et al19 | Retrospective data analysis | “Estimate trends in and outcomes following hospitalization for HF” | All hospital separations in South Australia | 8941 first HF admissions, July 2002 to June 2008 | NG | Excluding previous HF deaths: n = 1677 at 1 year (23.1%) | 1 year | NA (only gender) | 1 year | n = 375 (5.16%) 1 year | NG | Gender |
| Nymark et al22 | Database review | “Analyze available medical data for the occurrence of a second HF as distributed over time from the first HF until occurrence of a second HF or death” | Funen County Hip Fracture Register, Funen County, Denmark | 10 177 HF ≥ 50 years, 1994-2004, 9990 HF for analysis | Men 80.7, women 77.5 | Excluding patients with first previous HF (187) | Until Jul 2005/death, minimum 12 months | NA (only gender) | 1-11.5 years | 868/9990 (8.7%), overall incidence men: 2.37/1000 py, women 2.93/1000 py, incidence women: 116/1000 py in 3 months, 15/1000 py in 12 months, incidence men: 73/1000 py in 3 months, 8/1000 py in 12 months | Men: 12 months (CI: 7.4-17.4), women: 19 months (CI 16.7-22.5), 50% in 12 months (men) and 19 months (women) | Age + gender |
| Hagino et al20 | Historical, register based, uncontrolled, follow-up study | “Elucidate the incidence of additional fractures in patients within 1 year after first HF, investigate frequency of prescription of antiosteoporotic pharmaceuticals” | 25 hospitals in Japan (5 areas) | 2663 female HF patients ≥65yr, January 2006 to December 2007, 1076 + 887 for analysis | 83.6 | Excluded pathological, high-impact trauma, fracture before/after study period; dropouts: 61 deaths, 304 lost, including ipsilateral second HF (75.3% contralateral), 1076 (46.6%) returned questionnaire, 887 with medical record follow-up | 1 year | First HF | 12 months | n = 77 (34/1000 py) | n = 40, 51.9% 6 months, n = 48, 62.3%, 8 months | Age, height, weight, BMI, comorbidities, cognitive dysfunction, ambulatory ability, site and type of fracture, surgical procedure, pharmacotherapy during and posthospitalization |
| Lüthje et al21 | Prospective follow-up cohort study | “Identify all fractures prior or subsequent to an index HF among 221 HF patients” | 2 Finnish hospitals, Lahti and Kouvola, Southeastern Finland | 221 patients with index HF, February 2003 to January 2004/April 2004 | Index HF, women: 80.5 ± 10; men: 73 ± 12 | NG, deaths: 74% at 8 years | 8 years | NA (only gender) | Retrospective/8-year prospective/12- or 15-month inclusion | Retrospective: 14, prospective: 22 | NG | Gender |
Abbreviations: BMD, bone mineral density; BMI, body mass index; CI, confidence interval; HF, hip fracture; NA, not available; NG, not given; py, patient-years.
Study Characteristics
In group A, 6 of the 11 studies had a prospective patient enrollment,1,9,12,13,16,17 one was a nationwide population-based historical cohort,1 and 4 assessed clinical data retrospectively.8,13–15 Among the 5 studies of group B, 2 had a prospective patient enrollment.18,21 The observation period across all studies ranged from 6 months to 25 years. In group C, 8 studies assessed HFs retrospectively. Patient enrollment was unclear in 1 study and prospective in all the remaining. Six studies assessed HF risk in contrast to the fracture risk of the general population. Six other studies investigated modifiers of HF risk in the context of randomized controlled studies.
Incidence of Contralateral HFs
Incidence reporting across studies varied considerably and ranged from 2.3% patient-year10,11 to 4.3% patient-year.14 Prevalence of contralateral HFs could not be compared due to the large difference in observation periods. Among studies reporting the cumulative incidences at 1 year, the values ranged from 2.3% to 9.0%.1,12
Frequency of Assessed Risk Factors
The 11 studies of group A underwent a detailed analysis of the definition and description of risk parameters assessed. Overall, 50 parameters were studied. The top 5 parameters where articles agreed were female gender (7 times reported), followed by age (5 reports) and parameters of general health, poor visual status, and stroke (each 4 times). Other important parameters (with 3 counts each) were the body mass index (BMI), presence of dementia, and institutionalization.
In those 4 articles that reported the results of multivariate analyses, the largest model contained 4 parameters (age, gender, BMI, and functional status). The capacity of single parameters or models to identify patients with an increased risk of second HFs ranged substantially. A detailed description of risk factor groups, individual risk factors assessed, and corresponding association measures are shown in Table 3.
Table 3.
Risk Factors Assessed in Articles of Group A.
| Risk factor groups | Risk factor | No. of studies | Angthong et al8 | Baudoin et al9 | Berry et al10 | Chapurlat et al11 | Holt et al12 | Lönnroos et al13 | Mitani et al14 | Omsland et al15 | Ryg et al1 | Wolinsky and Fitzgerald16 | Yamanashi et al17 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | 7 | x | x | x | x | x | x | x | x | x | x | x | ||||||||||
| Age | 5 | x | x | x | x | x | x | x | ||||||||||||||
| Age group | Age group | 4 | 50-74 yrs | x | ||||||||||||||||||
| <65 yrs | ||||||||||||||||||||||
| 65-74 yrs | x | |||||||||||||||||||||
| 75-84 yrs | x | x | x | |||||||||||||||||||
| ≥85 yrs | x | x | x | |||||||||||||||||||
| 50-79 yrs | x | x | x | |||||||||||||||||||
| ≥80 yrs | x | x | ||||||||||||||||||||
| 55-74 yrs | x | |||||||||||||||||||||
| Place of living | Institutionalization | 3 | Nursing home residence/institution | x | x | x | x | x | ||||||||||||||
| Rural residence | 1 | Rural residence | x | |||||||||||||||||||
| Southern residence | 1 | Southern residence | x | |||||||||||||||||||
| Living alone | 2 | Living alone | x | x | ||||||||||||||||||
| Functional status and ambulation | 3 | On feet <4 h/d | x | |||||||||||||||||||
| Use arms to stand | x | |||||||||||||||||||||
| Walking speed (m/s) lowest vs highest quartile | x | |||||||||||||||||||||
| Use of walking aids | x | |||||||||||||||||||||
| Difficulties standing up/walking up stairs | x | |||||||||||||||||||||
| Functional status high vs moderate | x | x | ||||||||||||||||||||
| Functional status low vs moderate | x | x | ||||||||||||||||||||
| Difficulties: walking 1/4 miles | x | |||||||||||||||||||||
| Walking up 10 steps | x | |||||||||||||||||||||
| Standing for 2 hours | x | |||||||||||||||||||||
| Sitting for 2 hours | x | |||||||||||||||||||||
| Stooping, crouching, kneeling | x | |||||||||||||||||||||
| Reaching over head | x | |||||||||||||||||||||
| Shaking hands | x | |||||||||||||||||||||
| Using fingers to grasp | x | |||||||||||||||||||||
| Carrying 25 pounds | x | |||||||||||||||||||||
| Fracture type | 1 | Cervical | x | x | ||||||||||||||||||
| Trochanteric | x | x | ||||||||||||||||||||
| Subtrochanteric | x | x | ||||||||||||||||||||
| Comorbidities | General health | 4 | Number of comorbidities | |||||||||||||||||||
| Charlson index/0 | x | |||||||||||||||||||||
| 1-2 | x | |||||||||||||||||||||
| 3-4 | x | |||||||||||||||||||||
| ≥5 | x | x | x | |||||||||||||||||||
| Health in last 12 months, poor | x | |||||||||||||||||||||
| Poor perceived health status | x | x | ||||||||||||||||||||
| Hospitalized in the year before baseline | x | |||||||||||||||||||||
| Vision | 4 | Visual problems | x | |||||||||||||||||||
| Visual acuity | x | |||||||||||||||||||||
| Cataract (self-report) | x | x | x | |||||||||||||||||||
| Eye disease | x | x | ||||||||||||||||||||
| Hearing | 1 | Problems | x | |||||||||||||||||||
| Hyperthyroidism | 1 | x | ||||||||||||||||||||
| Stroke | 4 | x | x | x | x | x | ||||||||||||||||
| Parkinson | 1 | x | x | |||||||||||||||||||
| Depth perception | 1 | x | x | |||||||||||||||||||
| Dementia | 3 | x | x | x | x | |||||||||||||||||
| Neurological disease | 1 | x | x | |||||||||||||||||||
| Dizziness | 1 | x | x | |||||||||||||||||||
| Syncope | 1 | Fainted in the last 12 months | x | |||||||||||||||||||
| Arthritis | 3 | Osteoarthritis (self-report) | x | x | ||||||||||||||||||
| RA | x | x | ||||||||||||||||||||
| Osteoporosis | 2 | Osteoporosis | x | |||||||||||||||||||
| Singh index grade 1-3 | x | x | ||||||||||||||||||||
| Respiratory disease | 2 | Respiratory disease | x | |||||||||||||||||||
| COPD | x | x | ||||||||||||||||||||
| Hypertension | 1 | x | x | |||||||||||||||||||
| Diabetes mellitus | 2 | x | x | x | ||||||||||||||||||
| Ischemic Heart Dis. | 1 | x | x | |||||||||||||||||||
| Gynaecological disease | 1 | x | x | |||||||||||||||||||
| Alcoholism | 1 | x | ||||||||||||||||||||
| Medications | Calcium | 1 | Ever taken tums regularly | x | ||||||||||||||||||
| Ever taken other Ca supplements | x | |||||||||||||||||||||
| Calcium intake from food per week | x | |||||||||||||||||||||
| Estrogen | 1 | Currently systemic estrogen | x | x | ||||||||||||||||||
| Ever taken oral estrogen | x | x | ||||||||||||||||||||
| Long-acting benzodiazepines | 1 | Currently | x | |||||||||||||||||||
| Vitamin D | 1 | x | ||||||||||||||||||||
| Alcohol | 1 | Alcohol (no drinks/week) | x | |||||||||||||||||||
| Drank alcohol in past 12 months | x | |||||||||||||||||||||
| Caffeine | 1 | Daily caffeine (g) | x | |||||||||||||||||||
| Smoking | 1 | Smoking (cigarette packs/yr) | x | |||||||||||||||||||
| Thyroid hormone | 1 | x | ||||||||||||||||||||
| Intervention | Walking for exercise | 1 | x | x | ||||||||||||||||||
| BMD | BMD calcaneal | 1 | x | x | ||||||||||||||||||
| BMD total hip | 1 | x | x | |||||||||||||||||||
| Body height | Body height | 1 | Height | x | ||||||||||||||||||
| Height at age 25 yrs (cm) | x | |||||||||||||||||||||
| Body weight | Body weight | 2 | Kg | x | ||||||||||||||||||
| Gain since age 25 yrs | x | x | ||||||||||||||||||||
| kg at age 25 yrs | x | |||||||||||||||||||||
| 4-yr weight change | x | |||||||||||||||||||||
| BMI | BMI | 3 | /unit | x | x | x | x | x | ||||||||||||||
| Falls | Falls | 2 | Prior falls | x | x | |||||||||||||||||
| Previous fractures | Previous fractures | 2 | Prior fracture | x | ||||||||||||||||||
| Prevalent vertebral fracture at baseline | x | |||||||||||||||||||||
| Others | Pulse rate | 1 | Pulse rate lying down (beats/min) | x | ||||||||||||||||||
| Education | 2 | x | x | |||||||||||||||||||
| Mother’s history of HFs | 1 | x | ||||||||||||||||||||
| Black race | 1 | x | ||||||||||||||||||||
| Kin social support | 1 | Kin social supports, nonkin social supports | x x | |||||||||||||||||||
| Income | 1 | x | ||||||||||||||||||||
| Combinations | Place of living + ambulation | 1 | Lived at home + unaccompanied indoors walking | x | ||||||||||||||||||
| Living at home + walking with aids or accompanied | x | |||||||||||||||||||||
| Nursing home + unaccompanied indoors walking | x | |||||||||||||||||||||
| Nursing home + walking with aids or accompanied | x | |||||||||||||||||||||
| Women vs men + time after first HF | 1 | 3 months | x | |||||||||||||||||||
| 6 months | x | |||||||||||||||||||||
| 1 yr | x | |||||||||||||||||||||
| 2 yrs | x | |||||||||||||||||||||
| 3 yrs | x | |||||||||||||||||||||
| 4 yrs | x | |||||||||||||||||||||
| 5 yrs | x | |||||||||||||||||||||
| 10 yrs | x | |||||||||||||||||||||
| Women vs men + age group | 1 | 50-59 | x | |||||||||||||||||||
| 60-69 | x | |||||||||||||||||||||
| 70-79 | x | |||||||||||||||||||||
| 80-89 | x | |||||||||||||||||||||
| Model | u | m | m | u | m | b | m | |||||||||||||||
| crude/adjusted rate ratio | c | a | a | a | a | a | c | a | c | a | ||||||||||||
| Association measure | OR | OR | CRR | ARR | HR | HR | RR | OR | HR | HR | HR | HR | CRR | HR | HR | HR | ||||||
| Number of parameters assessed | 4 | 3 | 3 | 3 | 9 | 4 | 26 | 6 | 2 | 6 | 6 | 4 | 1 | 3 | 7 | 19 | 2 | 10 | 10 | |||
Abbreviations: a, adjusted; ARR, absolute risk reduction; b, bivariate; BMD, bone mass density; BMI, body mass index; c, crude; COPD, chronic obstructive pulmonary disease; CRR, crude rate ratio; m, multivariate; HF, hip fracture; HR, hazard ratio; OR, odds ratio; RA, rheumatoid arthritis; RR, relative risk; u, univariate; yr, year.
Discussion
Main Findings
This systematic review found a substantial amount of studies investigating risk parameters for contralateral HFs in various populations and health care contexts without being able to depict a stringent set of parameters associated with a higher risk of contralateral HFs, which can be used in clinical practice. Moreover, association measures for single parameters varied considerably across studies.
Results in Context With the Existing Literature
We are unaware of any review proving a comprehensive inventory of studies assessing the role of various clinical characteristics as risk factors for second HFs. We are aware of one eminent large study by Ryg and coworkers that, although having a somewhat other focus, provide data from survival analyses allowing estimations of contralateral HFs over time.1 Ryg and colleagues set out to study the incidence of contralateral HFs and its associated mortality risk. Moreover, they assessed whether specific comorbidity patterns were modifiers of that risk. They found a high incidence of second fractures within the first 5 years and a cumulative risk for fractures of up to 23% in that time period. Female gender, any previous fracture, diagnosis of alcoholism (based on the prescription of disulfiram or a corresponding diagnosis in the national Hospital Discharge Register or the Psychiatric Central Register), and living alone were parameters associated with a higher risk of mortality.
Strength and Limitations
To our knowledge, this is the first systematic inventory of prognostic parameters for contralateral HFs. The overview allows depicting patient patterns bearing an increased risk in a straightforward fashion. However, despite applying rigorous review methods, we were unable to go beyond a presentation of the available evidence. The evidence is very heterogeneous in terms of patient inclusions, design, and analysis to perform a methodologically sound meta-analysis. This is a common problem in descriptive prognostic research and meta-analyses thereof.53,54 Due to the lack of articles developing or validating prediction models, we therefore had to limit ourselves to the presentation of single parameters or parameter groups and their association with contralateral HFs. Due to the data at hand, we had to ignore the possible correlation and interaction between individual risk parameters, making the comparison between individual studies challenging.
Implications for Practice
From our findings, no direct implications for clinical practice can be drawn because we were unable to identify studies reporting on diagnostic tools available at the moment of the first HFs, allowing to identify a subgroup of geriatric HF patients with a substantially increased risk of sustaining a short-term contralateral HF. Thus, postoperative pharmacological and physiotherapeutical treatment remain the most important cornerstones of secondary fracture prevention.55 For patients who are unable to receive or adhere to adequate medical treatment like very old patients, those with low compliance, or contraindications, the treatment armamentarium remains limited at present.
However, this review identified some level of agreement regarding the relevance of female gender, patients’ age, the general health level, poor visual status, and stroke. Also, the BMI, presence of dementia, and institutionalization were commonly reported. In the absence of a carefully developed and also validated risk tool, these findings may give some indication in respect of an individual patient’s risk level.
Implications for Research and Conclusions
The findings of this article call for a conjoint effort to achieve an expert consensus for a critical set of parameters that, used in combination, could be used in a risk instrument for early identification and treatment of patients bearing an increased risk for contralateral HFs. This agreed set of risk parameters with a strong association with contralateral HFs should then be empirically tested in terms of discrimination and calibration within a sufficiently sized cohort of patients. The minimum set of parameters with the strongest predictive capacity should then undergo careful validation in new cohorts, ideally in different geographical regions, as differences in the baseline risk found in different countries may require adaptation of the risk instrument. At the same time, the effectiveness of an up-to-date medical treatment must be taken into consideration.
Appendix A
Search Strategy for MEDLINE (PubMed Interface)
((“hip fractures/drug therapy” [MeSH Terms] AND (“epidemiology” [Subheading] OR “epidemiology” [MeSH Terms])) OR (“hip fractures/epidemiology” [MeSH Terms] AND (“etiology” [Subheading] OR “etiology” [All Fields] OR “causality” [MeSH Terms] OR “causality” [All Fields])) OR (“hip injuries/epidemiology” [MeSH Terms] AND “etiology” [Subheading] AND “radiography” [Subheading]) OR (“hip fractures/complications” [MeSH Terms] AND epidemiology/*etiology [All Fields]) OR “hip fractures/mortality” [MeSH Terms] OR (“femoral neck fractures/complications” [MeSH Terms] AND “etiology” [Subheading])) AND (“risk factors” [MeSH Terms] OR (“risk” [All Fields] AND “factors” [All Fields]) OR “risk factors” [All Fields]).
Table A1.
Summary of Studies Reporting the Incidence Ratios of Second HFs in Relation to a General Population Risk.
| Retrospective/prospective inclusion of previous/subsequent HF | Time of assessment of risk factors | Patient groups compared | Study design | Study intention | |
|---|---|---|---|---|---|
| Assessment years after HF, n = 1 | |||||
| Stewart et al49 | Prospective | After first HF | 1 HF group vs 2 HF group | Prospective follow-up cohort study | Identify the best factor technique(s) to predict a second HF |
| Retrospective inclusion of previous HF, n = 7 | |||||
| von Friesendorff et al51 | Retrospective | First vs second HF | 1 HF group vs 2 HF group | Retrospective database review | Evaluate survival and fracture risk after HF in women at different ages |
| Khan et al35 | Retrospective | First vs second HF (?) | 1 HF group vs 2 HF group | Retrospective chart review | Investigate factors influencing LOS and mortality in first and second HF |
| Dinah26 | Retrospective | First vs second HF | 1 HF group vs 2 HF group | Retrospective case record study | Determine whether the rate of sequential HF in elderly patients has changed over the past 20 years |
| Fukushima et al31 | Retrospective | First vs second HF (?) | 1 HF group vs 2 HF group | Retrospective case record study | Investigate incidence, prognosis, and risk factors of bilateral HF |
| Dretakis et al28 | Retrospective | First vs first HF and first vs second HF | 1 HF group vs 2 HF group | Mainly retrospective population-based case record study (4 cases prospective) | Investigate factors that might play a role in the occurrence of the second or bilateral HF and tries to answer whether the type of the first fracture makes some patient susceptible to a second one |
| Shabat et al47 | Retrospective | First vs First HF | 1 HF group (matched for time of admittance) vs 2 HF group | Retrospective database review | Review this group (with past HF) of patients in terms of their comorbidities, type of fractures, operations, and potential of rehabilitation |
| Finsen and Benum30 | Retrospective | First vs first HF | 1 HF group vs 2 HF group | Prospective cohort (?) | Examine the relationship between the first and the second HF (of fracture affecting the same hip) |
| Prospective and retrospective inclusion, n = 1 | |||||
| Vochteloo et al50 | Prospective and retrospective | First vs first HF and first vs second HF | 1 HF group vs 2 HF group | Observational cohort study, partly retrospective and prospective | Assess the 1-year risk and absolute risk of sustaining a contralateral HF in our cohort and identify possible risk factor for sustaining a contralateral HF |
| Double inclusion of patients, n = 3 | |||||
| Rodaro et al42 | Prospective (?) | First vs second HF (?) | All vs 2 HF group (?), double inclusion (?) | Retrospective database review | Evaluate epidemiological and functional variables in proximal femur fracture inpatients |
| Sawalha and Parker43 | Prospective and retrospective | First vs second HF | All HF vs 2 HF group, double inclusion | Database review | Characteristics and outcome, site, and time between fractures |
| Dretakis et al27 | Retrospective (?) | First vs first HF (age) and first vs second HF | All HF vs 2 HF group (?), double inclusion (?) | Retrospective chart review | Comparison of unilateral and bilateral group: marked similarity between the 2 fractures in the majority of the patients |
| Matched control group/intervention cohorts, n = 5 | |||||
| Lee et al37 | Retrospective | First vs second HF (?) | Matched 1 HF group vs 2 HF group | Matched pair cohort study | Analyzing risk factors of SHF and the effect of osteoporosis treatment on the prevention on SHF |
| Saxena and Shankar44 | Prospective | After first HF (?) | Matched one HF group vs 2 HF group | Case–control study (case records): 2 HF group + matched controls | Analyzing reasons for recurrent falls to ascertain if certain medical conditions are more common in those who sustain a second fracture |
| Osaki et al41 | Prospective | First HF | Bisphosphonate cohort vs matched control group | Prospective matched cohort study | Investigate the preventive effect of risedronate on second HF immediately following a first HF in Japanese female patients with osteoporosis with unilateral HF |
| Segal et al46 | Prospective | First HF | Postsurgical osteoporosis treatment program (PSOTP) cohort vs community-treated patients (CTP) cohort | Longitudinal observational cohort study | Assessed standards of care, following an index HF, and the rate of second HF in elderly patients treated in the CTP and compared it with the rate in the participants of PSOTP |
| Cree et al25 | Prospective | NA | All vs patients receiving osteoporosis treatment | Original prospective inception cohort study, plus database review | Determine if patients were receiving osteoporosis treatment following HF and whether this treatment was beneficial in reducing mortality and morbidity. Also investigating association between continuity of care and osteoporosis therapy in pat. after HF |
| Intervention cohorts with additional analysis of parameters in association with second HF, n = 2 | |||||
| Lee et al38 | Prospective | First HF (compliance after 1 year) | Noncompliant user vs compliant user nonpersistent user vs persistent user. Multivariate analysis for second HF available (gender, 5-year increments of age, compliant, and persistent use of bisphosphonate) | Retrospective epidemiological review of prospectively collected database of health insurance | Determine whether the adherent use of bisphosphonate was associated with a decreased risk of second HF |
| Lee et al39 | Prospective | First HF (compliance after 1 year) | Compliant users vs nonusers. Univariate comparison and Cox regression analysis available for second HF group vs no fracture group (age, gender, BMI, neuropsychiatric disease, liver disease, hematologic disease, renal disease, Charlson comorbidity index) | Retrospective case record study | Determine the incidence of second HF and to evaluate whether compliant users of bisphosphonate had a lower incidence of second HF after prior HF |
| Risk for second HF compared to general population risk of first HF, n = 6 | |||||
| Schrøder et al45 | Prospective | NA (men vs women) | Risk of first HF vs risk of second HF | Retrospective case record study | A more elaborate estimate of the epidemiology of the second HF |
| Lawrence et al36 | Prospective | NA (age first HF, men vs women) | Risk of first HF vs risk of second HF | Prospective epidemiological study | Determine the age-specific incidence of a second fracture and to compare it with the incidence of a primary fracture within the general population |
| Melton et al40 | Prospective | NA (age first HF, men vs women) | Risk of first HF vs risk of second HF | Population-based case record study | Estimate overall HF recurrence rate using actuarial methods, evaluate contralateral and ipsilateral recurrences, identify variation in risk of recurrence based on age, sex degree of trauma, site of initial fracture, describe site of recurrent fracture, and interval between initial and subsequent fracture |
| Johnell et al33 | Prospective | NA (age first HF, men vs women) | Risk of first HF vs risk of second HF | Retrospective database review | Determine the pattern of risk of fractures occurring the years after a HF, clinical vertebral fracture, or shoulder fracture in outpatients and hospitalized patients |
| Omsland et al15 | Prospective | NA (men vs women) | Risk of first HF vs risk of second HF | Retrospective population-based database review | Examine whether total age-specific HF rates have changed in Norway between 1999 and 2008, compare overall rates of first and second HF in both genders, investigate whether the incidence rate of second HF has changed over time |
| Melton et al52 | Prospective | First HF | Risk of first HF vs risk of second HF. Multivariate Anderson-Gill analysis mentioned (age, calendar year) | Population-based database review | Focus on declining incidence of first HF and trends in the risk of HF recurrence |
| RCTs, n = 6 | |||||
| Colon-Emeric et al24 | Prospective | NA | ZOL/placebo | Post hoc analysis | Determine which clinical risk factors are associated with subsequent fracture (not HF) following a low-trauma HF, determine whether clinical risk factors for subsequent fracture are different in patients treated with ZOL compared with placebo |
| Birks et al23 | Prospective | NA | Hip protector/control | Pragmatic RCT | Assess whether hip protectors prevented second HF among community-dwelling older people |
| Eriksen et al29 | Prospective | NA | ZOL/placebo | Post hoc analysis | Examine whether timing of first infusion had any relationship to fracture and mortality benefit |
| Stenvall et al48 | Prospective | NA | Postoperative geriatric specialty ward/control | RCT | Evaluate if a postoperative multidisciplinary, multifactorial intervention program could reduce inpatient fall-related injuries in patients with femoral neck fractures |
| Karachalios et al34 | Prospective | NA | Calcitonin spray/placebo | RCT | Investigate the early and midterm effects of the intranasal administration of 200 IU of salmon calcitonin on biochemical bone markers, BMD, and the occurrence of further fracture |
| Galvard and Samuelsson32 | Prospective | NA | Orthopedic/geriatric department rehabilitation | RCT | End points: primary mortality, number of hip prostheses during the first postoperative year |
Abbreviations: BMD, bone mineral density; BMI, body mass index; HF, hip fracture; LOS, length of hospital stay; NA, not available; RCT, randomized controlled trial; SHF, second hip fracture; ZOL, zoledronate.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P. Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977-2001. J Bone Miner Res. 2009;24(7):1299–1307. [DOI] [PubMed] [Google Scholar]
- 2. Liem IS, Kammerlander C, Suhm N, et al. Identifying a standard set of outcome parameters for the evaluation of orthogeriatric co-management for hip fractures. Injury. 2013;44(11):1403–1412. [DOI] [PubMed] [Google Scholar]
- 3. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269, w264. [DOI] [PubMed] [Google Scholar]
- 4. Chiu KY, Pun WK, Luk KD, Chow SP. Sequential fractures of both hips in elderly patients—a prospective study. J Trauma. 1992;32(5):584–587. [DOI] [PubMed] [Google Scholar]
- 5. Ip D, Ip FK. Elderly patients with two episodes of fragility hip fractures form a special subgroup. J Orthop Surg (Hong Kong). 2006;14(3):245–248. [DOI] [PubMed] [Google Scholar]
- 6. Kaukonen J-P, Lüthje P, Nurmi-Lüthje I, Kataja M, Naboulsi H. Second hip fracture and patients’ medication after the first hip fracture: a follow-up of 221 hip fracture patients in Finland. Arch Gerontol Geriatr. 2011;52(2):185–189. [DOI] [PubMed] [Google Scholar]
- 7. Kaper BP, Mayor MB. Incidence of bilateral proximal femoral fractures in a tertiary care center. Orthopedics. 2001;24(6):571–574. [DOI] [PubMed] [Google Scholar]
- 8. Angthong C, Suntharapa T, Harnroongroj T. [Major risk factors for the second contralateral hip fracture in the elderly]. Acta Orthop Traumatol Turc. 2009;43(3):193–198. [DOI] [PubMed] [Google Scholar]
- 9. Baudoin C, Fardellone P, Bean K, Ostertag-Ezembe A, Hervy F. Clinical outcomes and mortality after hip fracture: a 2-year follow-up study. Bone. 1996;18(3 suppl):149s–157s. [DOI] [PubMed] [Google Scholar]
- 10. Berry SD, Samelson EJ, Hannan MT, et al. Second hip fracture in older men and women: the Framingham Study. Arch Intern Med. 2007;167(18):1971–1976. [DOI] [PubMed] [Google Scholar]
- 11. Chapurlat RD, Bauer DC, Nevitt M, Stone K, Cummings SR. Incidence and risk factors for a second hip fracture in elderly women. The Study of Osteoporotic Fractures. Osteoporos Int. 2003;14(2):130–136. [DOI] [PubMed] [Google Scholar]
- 12. Holt G, Smith R, Duncan K, Hutchison JD, Gregori A, Reid D. Outcome after sequential hip fracture in the elderly. J Bone Joint Surg Am. 2012;94(19):1801–1808. [DOI] [PubMed] [Google Scholar]
- 13. Lönnroos E, Kautiainen H, Karppi P, Hartikainen S, Kiviranta I, Sulkava R. Incidence of second hip fractures. A population-based study. Osteoporos Int. 2007;18(9):1279–1285. [DOI] [PubMed] [Google Scholar]
- 14. Mitani S, Shimizu M, Abo M, Hagino H, Kurozawa Y. Risk factors for second hip fractures among elderly patients. J Orthop Sci. 2010;15(2):192–197. [DOI] [PubMed] [Google Scholar]
- 15. Omsland TK, Emaus N, Tell GS, et al. Ten-year risk of second hip fracture. A NOREPOS study. Bone. 2013;52(1):493–497. [DOI] [PubMed] [Google Scholar]
- 16. Wolinsky FD, Fitzgerald JF. Subsequent hip fracture among older adults. Am J Public Health. 1994;84(8):1316–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yamanashi A, Yamazaki K, Kanamori M, et al. Assessment of risk factors for second hip fractures in Japanese elderly. Osteoporos Int. 2005;16(10):1239–1246. [DOI] [PubMed] [Google Scholar]
- 18. Dirschl DR, Piedrahita L, Henderson RC. Bone mineral density 6 years after a hip fracture: a prospective, longitudinal study. Bone. 2000;26(1):95–98. [DOI] [PubMed] [Google Scholar]
- 19. Gordon J, Pham CT, Karnon J, Crotty M. Monitoring progress in the management of hip fractures in South Australia, Australia. Arch Osteoporos. 2012;7(1-2):267–273. [DOI] [PubMed] [Google Scholar]
- 20. Hagino H, Sawaguchi T, Endo N, Ito Y, Nakano T, Watanabe Y. The risk of a second hip fracture in patients after their first hip fracture. Calcif Tissue Int. 2012;90(1):14–21. [DOI] [PubMed] [Google Scholar]
- 21. Lüthje P, Helkamaa T, Kaukonen J-P, Nurmi-Lüthje I, Kataja M. A long-term follow-up of 221 hip fracture patients in southeastern Finland: analysis of survival and prior or subsequent fractures. Arch Gerontol Geriatr. 2012;54(3):e294–e299. [DOI] [PubMed] [Google Scholar]
- 22. Nymark T, Lauritsen JM, Ovesen O, Rock ND, Jeune B. Short time-frame from first to second hip fracture in the Funen County Hip Fracture Study. Osteoporos Int. 2006;17(9):1353–1357. [DOI] [PubMed] [Google Scholar]
- 23. Birks YF, Hildreth R, Campbell P, Sharpe C, Torgerson DJ, Watt I. Randomised controlled trial of hip protectors for the prevention of second hip fractures. Age Ageing. 2003;32(4):442–444. [DOI] [PubMed] [Google Scholar]
- 24. Colon-Emeric CS, Lyles KW, Su G, et al. Clinical risk factors for recurrent fracture after hip fracture: a prospective study. Calcif Tissue Int. 2011;88(5):425–431. [DOI] [PubMed] [Google Scholar]
- 25. Cree MW, Juby AG, Carriere KC. Mortality and morbidity associated with osteoporosis drug treatment following hip fracture. Osteoporos Int. 2003;14(9):722–727. [DOI] [PubMed] [Google Scholar]
- 26. Dinah AF. Sequential hip fractures in elderly patients. Injury. 2002;33(5):393–394. [DOI] [PubMed] [Google Scholar]
- 27. Dretakis E, Kritsikis N, Economou K, Christodoulou N. Bilateral non-contemporary fractures of the proximal femur. Acta Orthop Scand. 1981;52(2):227–229. [DOI] [PubMed] [Google Scholar]
- 28. Dretakis KE, Dretakis EK, Papakitsou EF, Psarakis S, Steriopoulos K. Possible predisposing factors for the second hip fracture. Calcif Tissue Int. 1998;62(4):366–369. [DOI] [PubMed] [Google Scholar]
- 29. Eriksen EF, Lyles KW, Colon-Emeric CS, et al. Antifracture efficacy and reduction of mortality in relation to timing of the first dose of zoledronic acid after hip fracture. J Bone Miner Res. 2009;24(7):1308–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Finsen V, Benum P. The second hip fracture. An epidemiologic study. Acta Orthop Scand. 1986;57(5):431–433. [DOI] [PubMed] [Google Scholar]
- 31. Fukushima T, Sudo A, Uchida A. Bilateral hip fractures. J Orthop Sci. 2006;11(5):435–438. [DOI] [PubMed] [Google Scholar]
- 32. Galvard H, Samuelsson SM. Orthopedic or geriatric rehabilitation of hip fracture patients: a prospective, randomized, clinically controlled study in Malmo, Sweden. Aging (Milano). 1995;7(1):11–16. [DOI] [PubMed] [Google Scholar]
- 33. Johnell O, Kanis JA, Oden A, et al. Fracture risk following an osteoporotic fracture. Osteoporos Int. 2004;15(3):175–179. [DOI] [PubMed] [Google Scholar]
- 34. Karachalios T, Lyritis GP, Kaloudis J, Roidis N, Katsiri M. The effects of calcitonin on acute bone loss after pertrochanteric fractures. A prospective, randomised trial. J Bone Joint Surg Br. 2004;86(3):350–358. [DOI] [PubMed] [Google Scholar]
- 35. Khan SK, Rushton SP, Dosani A, Gray AC, Deehan DJ. Factors influencing length of stay and mortality after first and second hip fractures: an event modeling analysis. J Orthop Trauma. 2013;27(2):82–86. [DOI] [PubMed] [Google Scholar]
- 36. Lawrence TM, Wenn R, Boulton CT, Moran CG. Age-specific incidence of first and second fractures of the hip. J Bone Joint Surg Br. 2010;92(2):258–261. [DOI] [PubMed] [Google Scholar]
- 37. Lee SH, Lee TJ, Cho KJ, Shin SH, Moon KH. Subsequent hip fracture in osteoporotic hip fracture patients. Yonsei Med J. 2012;53(5):1005–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lee Y-K, Ha Y-C, Choi HJ, et al. Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int. 2013;24(11):2887–2892. [DOI] [PubMed] [Google Scholar]
- 39. Lee Y-K, Ha Y-C, Yoon B-H, Koo K-H. Incidence of second hip fracture and compliant use of bisphosphonate. Osteoporos Int. 2013;24(7):2099–2104. [DOI] [PubMed] [Google Scholar]
- 40. Melton L, Jr, Ilstrup DM, Beckenbaugh RD, Riggs BL. Hip fracture recurrence. A population-based study. Clin Orthop Relat Res. 1982:(167):131–138. [PubMed] [Google Scholar]
- 41. Osaki M, Tatsuki K, Hashikawa T, et al. Beneficial effect of risedronate for preventing recurrent hip fracture in the elderly Japanese women. Osteoporos Int. 2012;23(2):695–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rodaro E, Pasqualini M, Iona LG, Di Benedetto P. Functional recovery following a second hip fracture. Eura Medicophys. 2004;40(3):179–183. [PubMed] [Google Scholar]
- 43. Sawalha S, Parker MJ. Characteristics and outcome in patients sustaining a second contralateral fracture of the hip. J Bone Joint Surg Br. 2012;94(1):102–106. [DOI] [PubMed] [Google Scholar]
- 44. Saxena P, Shankar J. Contralateral hip fractures—can predisposing factors be determined? Injury. 2000;31(6):421–424. [DOI] [PubMed] [Google Scholar]
- 45. Schrøder HM, Petersen KK, Erlandsen M. Occurrence and incidence of the second hip fracture. Clin Orthop Relat Res. 1993;(289):166–169. [PubMed] [Google Scholar]
- 46. Segal E, Zinnman C, Raz B, et al. Second hip fracture in elderly hip fracture patients: cost and effectiveness of fracture prevention treatment. Age Ageing. 2005;34(5):507–510. [DOI] [PubMed] [Google Scholar]
- 47. Shabat S, Gepstein R, Mann G, Kish B, Fredman B, Nyska M. The second hip fracture--an analysis of 84 elderly patients. J Orthop Trauma. 2003;17(9):613–617. [DOI] [PubMed] [Google Scholar]
- 48. Stenvall M, Olofsson B, Lundström M, et al. A multidisciplinary, multifactorial intervention program reduces postoperative falls and injuries after femoral neck fracture. Osteoporos Int. 2007;18(2):167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Stewart A, Walker LG, Porter RW, Reid DM, Primrose WR. Predicting a second hip fracture: the potential role of dual x-ray absorptiometry, ultrasound, and other risk factors in targeting of preventive therapy. J Clin Densitom. 1999;2(4):363–370. [DOI] [PubMed] [Google Scholar]
- 50. Vochteloo AJH, Borger van der Burg BLS, Röling MA, et al. Contralateral hip fractures and other osteoporosis-related fractures in hip fracture patients: incidence and risk factors. An observational cohort study of 1,229 patients. Arch Orthop Trauma Surg. 2012;132(8):1191–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. von Friesendorff M, von Friesendorff M, Besjakov J, Besjakov J, Akesson K, Akesson K. Long-term survival and fracture risk after hip fracture: a 22-year follow-up in women. J Bone Miner Res. 2008;23(11):1832–1841. [DOI] [PubMed] [Google Scholar]
- 52. Melton LJ, Kearns AE, Atkinson EJ, et al. Secular trends in hip fracture incidence and recurrence. Osteoporos Int. 2009;20(5):687–694. doi:10.1007/s00198-008-0742-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Huston P, Naylor CD. Health services research: reporting on studies using secondary data sources. CMAJ. 1996;155(12):1697–1709. [PMC free article] [PubMed] [Google Scholar]
- 54. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. [DOI] [PubMed] [Google Scholar]
- 55. Chesser TJ, Handley R, Swift C. New NICE guideline to improve outcomes for hip fracture patients. Injury. 2011;42(8):727–729. [DOI] [PubMed] [Google Scholar]