Introduction
Hospitalizations of nursing home (NH) residents are known to be frequent, costly, and potentially avoidable (Ouslander et al., 2010). There are approximately 1.6 million residents in the nation’s NHs; in 2006, almost a quarter of those admitted to a NH were transferred back to the hospital within 30 days, costing Medicare $4.34 billion (O'Malley, Caudry & Grabowski, 2011). Such transitions are disruptive and disorienting for frail elders and can significantly lower resident quality of life (Tena-Nelson et al., 2012). Furthermore, NH transfers often expose residents to increased risks associated with hospitalizations such as medication errors and healthcare-associated infections; it has been estimated that 40% of hospital admissions could have been avoided with high quality NH care (Saliba et al., 2000). Reducing these hospitalizations in NH residents has become an important clinical and policy issue and provides an opportunity to improve healthcare delivery and contain costs (Ouslander et al., 2010).
Currently, resident care in NHs is provided almost entirely by or under the direction of registered nurses (RNs). Adequate nurse staffing levels and a workforce characterized by low turnover and high retention have generally been found to improve resident outcomes and lower infection and hospitalization rates (Collier & Harrington, 2008). More recently, Thomas and colleagues (2013) found that NHs with higher retention rates for licensed nurses (RN and Licensed Practical Nurses [LPN]) was associated with a lower 30-day hospital readmission rate (beta = −0.02, p = 0.04). While these findings were based on a single state and the investigators were unable to distinguish differences between RN and LPN retention, it nevertheless has underscored the importance of targeting nurse retention in NHs. It is important to note, while there are relationships between turnover, retention and tenure, these are not identical concepts. Turnover is the number of leavers of an employment setting, retention is the number of “stayers” and tenure is calculated based on the length of time in an organization.
Castle and Engberg (2008) studied tenure in NHs and found that RNs with 5 or more years of experience at a single NH facility was associated with decreased restraint use, resident pain, pressure ulcers and indwelling catheter use. Furthermore, tenure of the nurse workforce has been found to be an important predictor of quality outcomes in both acute and NH settings in the VA (Veterans Administration) (Bartel, Beuileau, Phibbs & Stone, 2014; Uchida-Nakakoji, Stone, Schmitt & Phibbs, 2015).
Both retention and turnover have been associated with the quality and cost of care including the cost of staff hiring and training (Jones, 2008). Despite wide variation in reported estimates (from $22,000 to more than $64,000) it is clear that RN turnover in hospitals is costly. The cost of retention and turnover in NHs has not been as well studied. One group of researchers examined the direct and indirect costs of turnover in NHs and concluded that turnover actually saved facilities on average 2.9% of annual total costs (Mukamel et al., 2010). However, this model was conducted using data from California using a narrow perspective of the NH and did not consider the broader healthcare costs associated with increased hospitalizations or decreased quality of life of the resident. To date, the economic implications of high versus low RN tenure in NHs has not been quantified.
The challenge of improving NH quality of care is growing with the nation’s aging population; in 2009, individuals aged 85 and older represented 14.3 percent of the nation’s NH population (Agency on Aging, 2010). The healthcare challenge related to an aging population is even more severe for the nation’s veterans. The demand for NH services in the VA is likely to increase since the proportion of veterans age 85 was 33 percent in 2000 and has grown to 66 percent in 2010 (GAO, 2006). With the growing number of older adults anticipated to receive care in VA Community Living Centers (CLCs), formerly known as VA NHs, it is important to seek efficient ways to reduce costs while still improving quality. A nurse retention program presents such potential (Jones & Gates, 2007). With the enactment of the 2010 Patient Protection and Affordable Care Act (PPACA) and the Centers for Medicare and Medicaid Services (CMS) NH Value-Based Purchasing Demonstration understanding the associated costs and savings that may be related to RN tenure in NH from a broad perspective is needed (Thomas et al., 2013). Our objective is therefore to better understand the tradeoffs in increasing VA NH nurse tenure, quality of care, and cost-effectiveness.
Methods
A cost-effectiveness analysis (CEA) was carried out to evaluate RN tenure scenarios. In a CEA, the incremental effectiveness is measured in common units, such as adverse events avoided, life years saved or quality adjusted life years saved. A key feature of CEA is how the effects are summarized in an incremental cost-effectiveness ratio (ICER), which is calculated as follows:
where C1 equals the cost of the higher level investment (in our case, longer RN tenure), C2 equals the cost of the less costly comparator (shorter RN tenure), with corresponding outcome measures (E1 and E2). This study was guided by the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement (see Appendix 1), which is a 24-item checklist that ensures a standard method for transparent and complete reporting of health economic studies (Husereau et al., 2013). For further discussion of CEA methodology see (Frick, Cohen, & Stone, 2013),
Appendix 1.
CHEERS Statement
| CHEERS Checklist: Items to include when reporting economic evaluations of health interventions | ||
|---|---|---|
| Section/ Topic | # | Checklist Item |
| Title | ||
| Title | 1 | Economic Evaluation of Longer Registered Nurse Tenure on Nursing Home Resident Outcomes |
| Abstract | ||
| Structured summary | 2 |
Objective: To better understand the tradeoffs in NH nurse tenure and quality of care, this study builds on previous and ongoing research to evaluate the cost-effectiveness of two nurse workforce scenarios focusing on RN tenure (high versus low), the associated transfers from NH to the hospital and the associated costs. Perspective: Single healthcare payer perspective (VA) Setting: VA owned and operated NHs and medical centers Methods: CEA using decision tree modeling based on 3 different outcomes Results: Higher tenure is more cost effective and this was a robust finding across the analyses. Conclusions: NHs could realize cost savings by retaining an experienced RN workforce |
| Introduction | ||
| Background | 3 | Little is known about the economic implications of NH RN tenure on resident outcomes |
| Objectives | To better understand the tradeoffs in NH nurse tenure and quality of care, this study builds on previous and ongoing research to evaluate the cost-effectiveness of two nurse workforce scenarios focusing on RN tenure (high versus low), the associated transfers from NH to the hospital and the associated costs. | |
| Methods | ||
| Target population and subgroups | 4 | NH residents cared for by RNs in VA NHs |
| Setting and location | 5 | Setting: VA NH and VA Medical Center Location: National |
| Study perspective | 6 | Healthcare payer (NH and Hospital) |
| Comparators | 7 | RN tenure levels (lowest decile vs highest decile) |
| Time horizon | 8 | 1 month |
| Discount rate | 9 | NA; 1 month time horizon, discounting not needed. |
| Choice of health outcomes | 10 | 3 Outcomes: 1) $ per Hospitalization Avoided, 2) $ per Hospitalization and Death Avoided, 3) $ per Death Avoided |
| Measurement of effectiveness | 11a | Single study based estimates: Hospitalization rates based on RN tenure levels estimated from VA original dataset and VA internal datasets. |
| 11b | Synthesis based estimates: Uncertainty surrounding RN replacement costs and therefore derived from NH literature | |
| Measurement/valuation of preference based outcomes | 12 | No QALYs used |
| Estimating resources and costs | 13a | Single study based estimates: Costs and probabilities calculated from VA databases |
| Currency, price, date, and conversion | 14 | U.S. dollar; all costs inflated to 2012 dollars using Medical CPI |
| Choice of model | 15 | CEA employing decision tree—2 staffing scenarios (high vs. low RN tenure) |
| Assumptions | 16 | See Table 3. |
| Analytical methods | 17 | Used TreeAge Pro Suite software to calculate costs and effectiveness. One way sensitivity analyses conducted on probabilities for hospitalization, mortality and RN replacement costs. |
| Results | ||
| Study parameters | 18 | From NH to Hospitalization to NH or death |
| Incremental costs and outcomes | 19 | Costs: RN wage costs by tenure level+ daily NH/hospital cost*length of time in respective institution |
| Characterizing uncertainty | 20a | Perspective is only from a single healthcare payer; VA is unique and costs often do not translate to community NHs; VA NHs have higher overhead costs because they share costs with the Medical Center located in close proximity |
| Characterizing heterogeneity | 21 | Sensitivity analyses ran across wide plausible values |
| Discussion | ||
| Study findings, limitations, generalizability, and current knowledge | 22 | Based on one study parameters for VA tenure. Limited generalizability, uncertainty surrounding hospitalization rates and mortality rates. Could not differentiate between medically necessary or inappropriate hospitalization |
| Other | ||
| Sources of funding | 23 | This paper was supported by the National Institutes of Health, National Institute of Nursing Research [F31NR013810], the Robert Wood Johnson Foundation (RWJF #63959) and the Jonas Center for Nursing Excellence |
| Conflicts of interest | 24 | All authors declare no conflict of interest |
Note. RN= Registered Nurse, VA= Veterans Affairs, NH= Nursing Homes
Study Design/Time Horizon
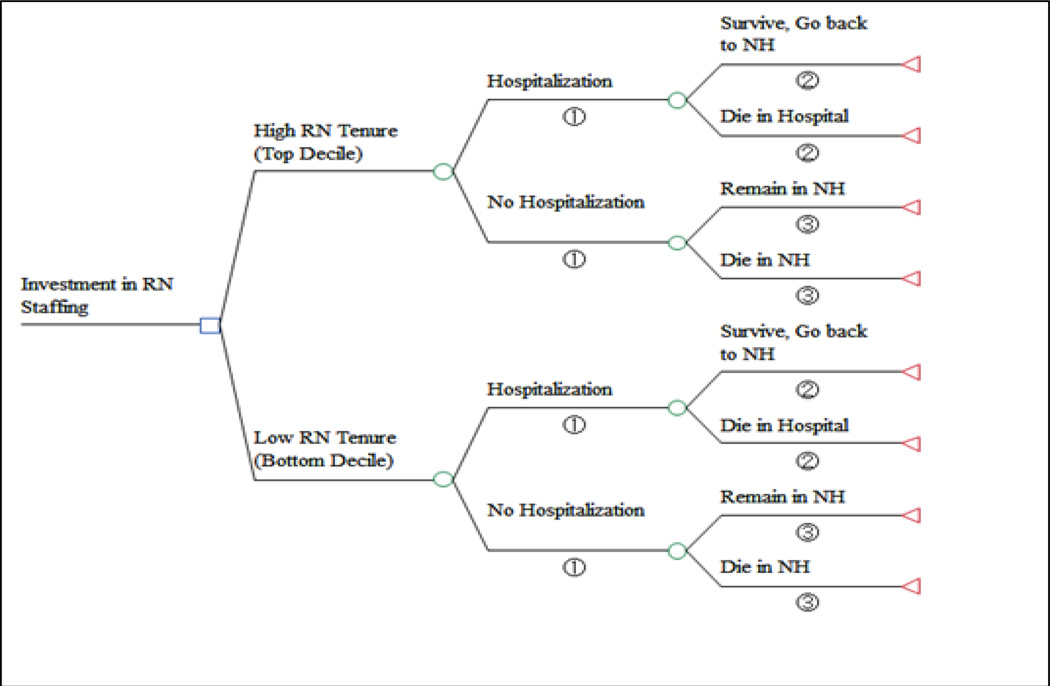
A decision tree (Figure 1) was constructed to compare the incremental costs and effects of RN tenure scenarios on NH resident transfers to the hospital under two NH staffing scenarios: high versus low levels of RN tenure. Three outcomes were modeled: 1) dollars per hospitalization avoided, 2) dollars per hospitalization and death avoided, and 3) dollars per death avoided. The time horizon of the modeling scenario was set to1 month and therefore we did not apply discounting. A short time horizon was chosen for two reasons. First, because the median hospital length of stay of residents transferred from NHs in the VA was 7 days and we were interested in acute transitions. Second, it was pragmatic given the data available lacking individual resident transitions, which would be needed to model a longer time horizon. Because of the short time horizon, life years and quality adjusted life years were deemed inappropriate outcomes. The decision tree was constructed in TreeAge Pro 2013 Suite (TreeAge Software, Williamstown, MA). The study was modeled using a healthcare payer perspective. The model included conditional probabilities and accrued costs from both NHs and hospitals within the VA setting as well as other data sources.
Figure 1.
Decision tree
Note. Decision tree depicted to model investment in RN staffing. ①Hospitalization rates by tenure levels; ② Mortality probability in hospital; ③Mortality probability in NH. RN= Registered Nurse, NH= Nursing Home
Variables and Data Sources
This study builds on retrospective existing dataset of monthly, unit-level resident and nurse workforce data from the VA for fiscal years 2003–2008 (October 2002 to September 2008) compiled for a larger study examining VA long-term care nursing care quality and resident safety (Robert Wood Johnson Foundation Grant No. #63959). Institutional review board approval was obtained from both Columbia University Medical Center and Stanford University.
The variable definitions, base case values and ranges are outlined in Table 1. NH hospitalization rates, NH mortality rates and RN tenure levels were based on VA NH units with short and long-stay residents, which included 20 VA integrated service networks across 37 states. Hospital mortality rates and median hospital length of stay were calculated from the VA internal databases and resident enrollment files.
Table 1.
Model Baseline Estimates
| Variable | Baseline Estimates | Range |
|---|---|---|
| Hospitalization Rates by Tenure Levels | ||
| Low tenure hospitalization rate % (Bottom 10% RN Tenure) | .044 | 0–1 |
| High tenure hospitalization rate % (Top 10% RN Tenure) | .026 | 0–1 |
| Mortality Probabilities | ||
| Probability death in hospital given transfer from VA NH % | 0.259 | 0–1 |
| Probability of death in VA NH given there is no transfer % | 0.032 | 0–0.56 |
| Length of Stay | ||
| Median hospital length of stay (days) among residents transferred from VA NH | 7 | 5–12 |
| Cost Parameters | ||
| Median daily cost of hospitalization for VA NH residents transferred to hospital | 2024.69 | 0–5,000 |
| Median daily cost of VA NH stay | 669.88 | 0–1,000 |
| Mean hourly wage of VA NH RN | 53.46 | -- |
| RN replacement/ replacement cost | 5,526.13 | 0–10,000 |
| VA wage per step increase % | 0.027 | 0–0.20 |
Note. Costs are displayed in 2012 dollars. All data come from the VA with the exception of the RN replacement cost, which is estimated from the literature. RN= Registered Nurse, VA= Veterans Affairs, CLC= Community Living Centers, formerly known as VA Nursing Homes
Costs
Cost parameters were primarily derived from the VA Health Economics Resource Center national cost estimates for NH and hospital care. Nurse wages was assumed to increase depending on how long one worked within an institution. Although data on annual wage increase by each additional year of tenure was not available; therefore, we used the “step” increases in the salary pay grade as a proxy to quantify wage differentials between high versus low tenure levels. Monthly RN costs were calculated using the mean VA hourly wage. Using the VA payroll data, the average “step increase” differential among RNs in 2003–2008 was 2.5% to 3.5%. In our models, the average “step increase” was interpreted as one year of tenure and a conservative rate of 2.7% was assumed.
To quantify the replacement cost of RNs in NHs, annual pre-and post-hiring costs were calculated based on published literature, then divided by 12 to give a monthly cost (Caudill & Patrick, 1991; Jones, 2008; Jones & Gates, 2007). Pre-hire costs consisted of advertising for recruitment, hiring, and vacancy costs (hiring temporary staff, overtime, productivity losses, etc.). Post-hire costs included orientation and training costs of the new RN, and new RN productivity losses.
Hospital cost per day was based on the actual median cost of a hospital day among residents who were transferred to the hospital from the VA NH. NH cost per day was based on the median cost of a NH day for those residents who remained in the VA NH. All costs were expressed in 2012 U.S. dollars using the Medical Consumer Price Index (Halfhill, 2013).
Strategies Compared: High versus Low RN Tenure
We measured the effects of high and low levels of RN tenure by calculating the resident hospitalization rates stratified by RN tenure levels (deciles) at the unit level. The top and bottom deciles were used as the basis for our baseline conditional probability estimates (Figure 1). In the high tenure scenario, the average RN tenure was 6.7 years compared to the low tenure scenario, in which the average RN tenure was 2.5 years.
Assumptions in Base Case Analysis
Several assumptions were made in the base case analysis to simulate the course of a NH resident’s transition (Appendix 2). First, we assumed a one month scenario for a NH unit with 32 residents under supervision by 1 RN (Centers for Medicare and Medicaid Services, 2001). We modeled four endpoints: for those residents who were hospitalized, they were either discharged back to the VA NH or died during the hospitalization; for those residents who were not hospitalized, they either remained in the NH or died. Given the close proximity of VA NHs to the VA Medical Centers, it was therefore assumed that residents were discharged back to their original NH. Mortality rates for residents hospitalized or not hospitalized were assumed to be the same between the two tenure scenarios and this assumption was varied in sensitivity analyses.
Appendix 2.
List of Major Assumptions
Model Overall Assumptions:
|
Transition Assumptions:
|
Resident Transition Cost Assumptions:
|
RN Cost Assumptions:
|
Note. Costs are displayed in 2012 dollars. All data come from the VA with the exception of the RN replacement cost, which is estimated from the literature. RN= Registered Nurse, NH= Nursing Home, VA= Veterans Affairs, VA NH= Commuity Living Centers (CLC)
Although we were able to retrieve estimates of the median length of stay in hospitals, data on length of stay prior to dying in a hospital was not available. Therefore, it was assumed that a resident died within 48 hours of being hospitalized. For these residents, daily hospital costs were counted for 2 days. An additional 15 days of daily NH costs were added to the final cost calculation because it was assumed that residents could be hospitalized anytime during a month following a uniform distribution. For instance, if the resident was hospitalized and died, then costs were calculated as (2 days*daily hospital cost) + (15 days* daily NH cost). The same logic was applied to cases in which residents remained in the NH and died (15 days *daily NH cost).
The models assumed care under 1 RN based on a NH unit size of 32 beds. Based on minimum RN staffing hours in many states, it is reasonable to assume that a typical NH RN worked for 8 hours a day and 5 days a week. We assumed an annual wage increase of 2.7% for each additional year of tenure; given the average tenure ranged 4 years in the data, the total wage increase was therefore compounded by 4 years (the rounded difference in tenure between the high versus low) and multiplied by the monthly RN cost.
RN replacement costs were estimated from the average of 2 previously reported study results. Using 1990 dollars, Caudill and Patrick (1991) reported over $7,000 annually to replace one RN. Inflated, this converts to $17,829 per RN in 2012 dollars. While this study was specific to NHs, the data are old. In 2008, Jones (2008) reported annual replacement cost per RN in hospitals to be over $82,000 in 2007 dollars (which translates to $96,969 in 2012 dollars). Because hospitals require more resources to train and fill vacancies, we made a conservative assumption of a 50% reduction in these costs for NHs and again divided the annual costs by 12 to obtain the monthly cost. Assuming 2 RNs are replaced in a year, we calculated an average monthly RN replacement cost and added this value to the RN cost of the low tenure branch.
Sensitivity Analysis
A number of key variables (i.e., hospitalization rate, RN replacement cost) were subjected to a one-way sensitivity analysis. In a one-way analysis, an input variable is allowed to vary (while holding all else constant) from the minimum to the maximum value of its range. Because VA owned and operated NHs likely differ from typical community based NHs (in terms of its resources and resident mix), we attempted to reflect these differences by testing our variables across a wide range of possible values.
Results
Table 2 displays results of the 3 different outcomes. The total costs of care for the low tenure scenario were $34,108 per month compared to the high tenure scenario at $29,442 per month. Effectiveness of the high tenure was greater across all 3 outcomes (incremental effectiveness ranged from 0.925 to 0.974 depending on outcome), indicating that high tenure was the dominant strategy (that is less costly and more effective). The incremental cost difference per month between the high and low tenure scenario was $4,655. The magnitude of this cost is substantial when considering the potential savings to the VA healthcare system. Assuming a median size NH unit with 32 patients, if the NH is able to create working environments that lead to higher RN tenure, the annual net savings translates to greater than $55,000 per unit (i.e., 4,655*12 = 55,860). With 133 VA NH facilities across the nation with 340 units, this roughly translates to savings of over $18 million (55,860*340 = 18,992,400).
Table 2.
Summary of 3 Base Case Models
| Outcome Measure | Staffing Scenario |
Total Costs, $ |
Incremental Costs |
Effectiveness: |
|---|---|---|---|---|
| 1) Hospitalization Avoided | High Tenure | $29,442.36 | −$4,665.74 | 0.974 |
| Low Tenure | $34,108.10 | -- | 0.956 | |
| 2) Hospitalizationor Deaths Avoided | High Tenure | $29,442.36 | −$4,665.74 | 0.942 |
| Low Tenure | $34,108.10 | -- | 0.925 | |
| 3) Death Avoided | High Tenure | $29,442.36 | −$4,665.74 | 0.962 |
| Low Tenure | $34,108.10 | -- | 0.958 |
Note. $ = 2012 U.S. Dollars
A summary of the sensitivity analyses are presented in Table 3. The results were insensitive to variations in NH cost and hospital daily costs. However, across all 3 outcomes, the results of the base case were sensitive to changes in hospitalization rates, RN replacement costs and RN wage increases by tenure. For instance, when RN replacement costs went below $1,000 per month, the high tenure strategy was no longer dominant. When RN wage step increases went above 9.76%, high RN tenure was no longer dominant. Only when deaths avoided was modeled were the results sensitive to hospital mortality probabilities beyond 10% and NH mortality rates less than 20%. In other words, when hospital mortality rates are above 10% or NH mortality rates are below 20%, then high RN tenure strategy was dominant for reducing dollars per life saved; however, if monthly mortality probabilities changed beyond these rates, then having higher RN tenure was no longer cost saving. In scenario 3 where the outcome measure was dollars per death avoided, the only parameters that the results were sensitive to were the probabilities of mortality.
Table 3.
Sensitivity Analyses
| Variables | Range of Values | Point at which Low Tenure strategy is no longer dominated |
|
|---|---|---|---|
| Minimum | Maximum | ||
| Hospitalization Rate (High Tenure) | 0 | 1 | 0.06 |
| Hospitalization Rate (Low Tenure) | 0 | 1 | 0.04 |
| Probability of Hospital Mortality* | 0 | 1 | 0.1 |
| Probability of NH Mortality* | 0 | 1 | 0.2 |
| Daily Hospital Cost | 1 | 5,000 | Dominated |
| Daily NH Cost | 1 | 1,000 | Dominated |
| Monthly RN Replacement/Recruitment Cost | 0 | 10,000 | 1,000 |
| Wage Increase Differential by Tenure | 0 | 0.2 | 0.0976 |
Note.
Only Sensitive with Model 3: $ per Life Saved; Costs are displayed in 2012 dollars.
NH= Nursing Home
Discussion
Higher RN tenure in VA CLCs was cost-saving and this was a robust finding. This is markedly different from the model based on California NH data that found high nursing turnover was cost-savings (Mukamel et al., 2013). This difference is likely due to the methodology and perspective resulting in different costs included. In our study we used a broader healthcare perspective applicable to the VA and includes costs of transfers to the hospital; whereas the California study used only the costs to the NH setting itself.
The findings from our analysis have implications for NH administrators and policymakers and echo recommendations from previous researchers to focus attention on retaining a skilled RN workforce. The idea for building a business case for RN retention is not a new phenomenon (Horn, 2008; Jones, 2008). However, little was known about cost savings that could be realized from retaining a skilled RN workforce in NHs. Furthermore, these savings provide additional resources that could be invested to further improve resident quality of life such as training for RNs in the area of gerontology (Maas, Specht, Buckwalter, Gittler, & Bechen, 2008). It is important to note that while higher RN tenure may result in higher salary costs per RN, in our analysis these costs outweighed the additional required expenditures in units staffed by RNs with lower tenure related to worse resident outcomes and recruiting and replacing the workforce.
A strength of our study is the sensitivity analyses and our finding, higher tenure was cost savings, was similar under a number of different likely scenarios. For example, we calculated NH RN costs using a wage increase of 2.7% and the findings were consistent up to a 9.76%. While wage increases may not be linear and can depend on local market characteristics (Rondeau, Williams, & Wagar, 2008) it is unlikely that RNs in NHs are getting annual increases at almost ten percent, giving us confidence in these results.
While VA NH mortality rates were quite comparable to community NH values, 3.2% in our study and 2.5% reported in community NHs (Bronskill et al., 2009), the hospital mortality rates in the VA were high (i.e., 25.9%). Spector and colleagues (2012) reported a 8.1% hospital mortality rate among residents transferred from a NH. This rate falls under 10% range examined in our sensitivity analysis. While direct comparisons cannot be made between VA NHs and non-VA community NHs, differences in resident characteristics and reasons for transferring residents have been reported (French, Campbell & Rubenstein, 2008), which likely impact these rates. Furthermore, because VA NHs are often not free standing and closely located within VA Medical Centers, it could be that residents were only transferred to the hospital under the most serious conditions.
While this study has a number of strengths, it also has a number of limitations. This analysis did not consider cases in which residents could be discharged to the community. Patient preferences (e.g., advanced directives) and provider attitudes (e.g., overburdening of staff), factors previously found to be associated with increased resident hospitalizations were also not considered. Not being able to differentiate between short-stay and long-stay residents limits our analysis because residents may have different resource utilization profiles. The level and content of specialty training and leadership skills each nurse may have was not considered, which may impact the NH hospitalization rates. For instance, a RN with recent specialty training may potentially reduce hospitalizations regardless of the number of years with an institution. Quality of life factors were not adjusted in our scenarios; however, given the very short time horizon it would have been inappropriate to assign a quality of life weight. Finally, our study has limited generalizability in that the analysis was conducted under a single healthcare payer perspective, which is not typical of all NHs across the nation. Nevertheless, the estimates of the effects from this study may be useful in setting parameters and for considering the potential cost savings at a national level. Unlike the private sector, where the decision to hospitalize a resident may be influenced by financial incentives (i.e., NH care paid for by state Medicaid programs and hospitalizations paid for by Medicare), the VA NHs do not operate under such incentives (French et al., 2008) and therefore this distinct feature may generate additional opportunities to benchmark cost estimates of nurse tenure on reducing resident adverse outcomes.
Although a decision tree model is an appropriate way to compare the cost-effectiveness of the two staffing scenarios, other modeling techniques may also be beneficial. In our analysis we did not consider resident transitions as a recursive event. Compared to a decision tree where there is a finite time horizon and transitions can only occur once, a Markov simulation model allows residents to transition through the health states more than once, and may provide a more realistic picture of the costs and effects associated with different workforce profiles. We recommend a Markov simulation model be developed that differentiates short and long-stay residents and uses a longer time horizon.
Conclusions
Aligning quality outcomes with cost effectiveness is imperative to driving the direction of health policy in the U. S. While there has been policy interest in lowering NH hospitalizations and improving nurse retention, there has been little research documenting the associated financial costs incorporating higher RN salaries associated with higher tenure and resident care costs associated with preventable adverse events. In this paper, we have attempted to quantify those costs so NH administrators and policymakers can allocate NH resources more efficiently. Better prevention of hospitalizations by having an experienced RN workforce will not only improve resident quality of care but allow NHs to realize the value of retaining a skilled workforce by decreasing resident care costs associated with hospitalizations.
Acknowledgments
Funding Sources: This paper was generously supported by the National Institutes of Health, National Institute of Nursing Research [F31NR013810, R01NR013687], the Robert Wood Johnson Foundation [#63959], VA HSR&D, RWJ [08-274], and the Jonas Center for Nursing Excellence.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Conflicting Interests:
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Agency on Aging. A Profile of Older Americans, Living Arrangements. [Retrieved September 23rd, 2011];2010 http://www.aoa.gov/AoARoot/Aging_Statistics/Profile/2010/6.aspx.
- Bartel AP, Beaulieu ND, Phibbs CS, Stone PW. Human Capital and Productivity in a Team Environment: Evidence from the Healthcare Sector. American Economic Journal: Applied Economics. 2014;6(2):231–259. [Google Scholar]
- Bronskill SE, Rochon PA, Gill SS, Herrmann N, Hillmer MP, Bell CM, Stukel TA. The relationship between variations in antipsychotic prescribing across nursing homes and short-term mortality: quality of care implications. Medical Care. 2009;47(9):1000–1008. doi: 10.1097/MLR.0b013e3181a3943f. [DOI] [PubMed] [Google Scholar]
- Castle NG, Engberg J. Further examination of the influence of caregiver staffing levels on nursing home quality. Gerontologist. 2008;48(4):464–476. doi: 10.1093/geront/48.4.464. [DOI] [PubMed] [Google Scholar]
- Caudill ME, Patrick M. Costing nurse turnover in nursing homes. Nursing Management. 1991;22(11):61–62. 64. doi: 10.1097/00006247-199111000-00022. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Report to Congress: Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes (Vol. Phase II Final, Volumes I–III) Baltimore, MD: 2001. [Google Scholar]
- Collier E, Harrington C. Staffing characteristics, turnover rates, and quality of resident care in nursing facilities. Research in Gerontological Nursing. 2008;1(3):157–170. doi: 10.3928/19404921-20080701-02. [DOI] [PubMed] [Google Scholar]
- Frick K, Cohen C, Stone PW. Economic outcomes and analyses in advanced practice nursing. In: Kleinpell R, editor. Outcome Assessment in Advanced Practice Nursing. 3rd ed. 2013. [Google Scholar]
- French DD, Campbell RR, Rubenstein LZ. Long-stay nursing home residents' hospitalizations in the VHA: the potential impact of aligning financial incentives on hospitalizations. Journal of the American Medical Directors Association. 2008;9(7):499–503. doi: 10.1016/j.jamda.2008.03.015. [DOI] [PubMed] [Google Scholar]
- Ganz DA, Simmons SF, Schnelle JF. Cost-effectiveness of recommended nurse staffing levels for short-stay skilled nursing facility patients. BMC Health Services Research. 2005;5:35. doi: 10.1186/1472-6963-5-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GAO. VA Long-Term Care: Trends and Planning Challenges in Providing Nursing Home Care to Veterans (Rep. No. GAO-06-333T) Washington DC: United States Government Accountability Office; 2006. [Google Scholar]
- Halfhill T. Tom's Inflation Calculator. [Retrieved October 24th, 2013];2013 from http://www.halfhill.com/inflation.html. [Google Scholar]
- Horn SD. The business case for nursing in long-term care. Policy, Politics, & Nursing Practice. 2008;9(2):88–93. doi: 10.1177/1527154408320420. [DOI] [PubMed] [Google Scholar]
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, Force CT. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Value in Health. 2013;16(2):e1–e5. doi: 10.1016/j.jval.2013.02.010. [DOI] [PubMed] [Google Scholar]
- Jones CB. Revisiting nurse turnover costs: adjusting for inflation. Journal of Nursing Administration. 2008;38(1):11–18. doi: 10.1097/01.NNA.0000295636.03216.6f. [DOI] [PubMed] [Google Scholar]
- Jones CB, Gates M. The Costs and Benefits of Nurse Turnover: A Business Case for Nurse Retention. The Online Journal of Issues in Nursing. 2007;12(3) [Google Scholar]
- Maas ML, Specht JP, Buckwalter KC, Gittler J, Bechen K. Nursing home staffing and training recommendations for promoting older adults' quality of care and life: Part 2. Increasing nurse staffing and training. Research in Gerontological Nursing. 2008;1(2):134–152. doi: 10.3928/19404921-20080401-04. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Spector WD, Limcangco R, Wang Y, Feng Z, Mor V. The costs of turnover in nursing homes. Medical Care. 2009;47(10):1039–1045. doi: 10.1097/MLR.0b013e3181a3cc62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Malley AJ, Caudry DJ, Grabowski DC. Predictors of nursing home residents' time to hospitalization. Health Services Research. 2011;46(1 Pt 1):82–104. doi: 10.1111/j.1475-6773.2010.01170.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouslander JG, Lamb G, Perloe M, Givens JH, Kluge L, Rutland T, Saliba D. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs. Journal of the American Geriatrics Society. 2010;58(4):627–635. doi: 10.1111/j.1532-5415.2010.02768.x. [DOI] [PubMed] [Google Scholar]
- Rondeau KV, Williams ES, Wagar TH. Turnover and vacancy rates for registered nurses: do local labor market factors matter? Health Care Management Review. 2008;33(1):69–78. doi: 10.1097/01.HMR.0000304494.87898.bc. [DOI] [PubMed] [Google Scholar]
- Saliba D, Kington R, Buchanan J, Bell R, Wang M, Lee M, Rubenstein L. Appropriateness of the decision to transfer nursing facility residents to the hospital. Journal of the American Geriatrics Society. 2000;48(2):154–163. doi: 10.1111/j.1532-5415.2000.tb03906.x. [DOI] [PubMed] [Google Scholar]
- Spector W, Mutter R, Owens P, Limcangco R. HCUP Statistical Brief #141. Rockville, MD: Agency for Healthcare Research and Quality; 2012. Transitions between Nursing Homes and Hospitals in the Elderly Population, 2009. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb141.pdf. [PubMed] [Google Scholar]
- Tena-Nelson R, Santos K, Weingast E, Amrhein S, Ouslander J, Boockvar K. Reducing potentially preventable hospital transfers: results from a thirty nursing home collaborative. Journal of the American Medical Directors Association. 2012;13(7):651–656. doi: 10.1016/j.jamda.2012.06.011. [DOI] [PubMed] [Google Scholar]
- Thomas KS, Mor V, Tyler DA, Hyer K. The relationships among licensed nurse turnover, retention, and rehospitalization of nursing home residents. Gerontologist. 2013;53(2):211–221. doi: 10.1093/geront/gns082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchida-Nakakoji M, Stone PW, Schmitt SK, Phibbs CS. Nurse Workforce Characteristics and Infection Risk in VA Community Living Centers: A Longitudinal Analysis. Medical care. 2015;53(3):261–267. doi: 10.1097/MLR.0000000000000316. [DOI] [PMC free article] [PubMed] [Google Scholar]