Abstract
We present a series of cases of acute esophageal necrosis along with a video demonstration. The video captures a case showing the severity of necrosis of the esophageal mucosa; an orogastric tube easily passed through the esophageal lumen and into the right hemithorax. The series also demonstrates the severity of this illness, with an associated high mortality rate.
Introduction
Black esophagus is an endoscopic description of acute esophageal necrosis (AEN), a common final pathway for a number of conditions that can result in severe esophageal injury. This condition is often seen in the setting of critical illness, it is more commonly seen in older men and in patients with comorbidities such as diabetes or vascular disease. Commonly reported complications include perforation and stricturing.
Case Report
Case 1
A 62-year-old man with poorly controlled diabetes presented with lower extremity pain, hypotension, fever, leukocytosis, and acute kidney injury, and was diagnosed with necrotizing fasciitis requiring emergent amputation. During the operation, an orogastic tube was placed without reported difficulty. Post-operatively, the patient remained hypotensive and became hypoxic despite intubation. A chest x-ray revealed a large, right-sided pneumothorax with the orogastric tube malpositioned in the right hemithorax (Figure 1). An upper endoscopy showed black necrotic mucosa circumferentially throughout the entire esophagus (Video 1). Additionally, 35 cm from the incisors, the right wall of the esophagus was completely disrupted, allowing entry into the right pleural space and visualization of the right lung and parietal pleura. A diagnosis of AEN was made, and, despite maximal supportive care, the patient’s clinical condition deteriorated and he died.
Figure 1.
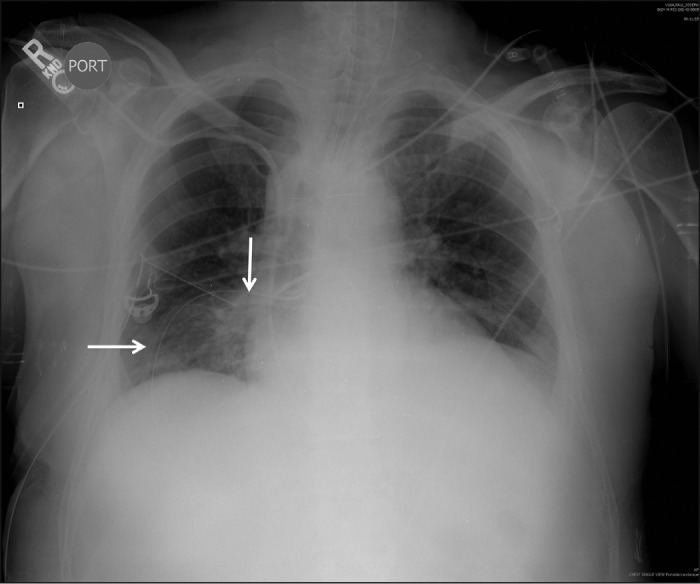
Chest x-ray from case 1 showing a large right-sided pneumothorax with an orogastric tube (arrows) malpositioned in the right hemithorax.
Video 1.
Acute esophageal necrosis complicated by esophageal perforation due to orogastric tube placement. On upper endoscopy, black necrotic mucosa was found throughout the esophagus, and there was a disruption of the distal esophagus where the right pleural space could be entered with visualization of the right lung and parietal pleura. The free esophageal perforation was too large for endoscopic intervention.
Case 2
A 63-year-old man with a history of heart failure, chronic obstructive pulmonary disease, and alcohol abuse presented with acute onset of chest pain, nausea, and hematemesis. Upper endoscopy showed diffuse esophageal necrosis as well as a small segment of denuded mucosa that was actively oozing blood and was injected with epinephrine for hemostasis. The patient was made nil-per-os and started on an intravenous proton pump inhibitor. Esophagram showed no extraluminal extravasation of contrast. Repeat upper endoscopy to assess for progression versus improvement of the necrosis demonstrated some improvement, with necrosis now involving approximately two-thirds of the esophagus. After 9 days of total parenteral nutrition, the patient was started on clear liquids, advanced to a regular diet, and subsequently discharged home.
Case 3
A 72-year-old man with severe peripheral vascular disease, bilateral below the knee amputations, and left femoral-popliteal bypass graft presented with a left groin infection and exposure of his femoral popliteal graft which required surgical intervention. His post-operative course was complicated by a left groin hematoma and surgical evacuation and repair of the bleeding site. Two days later, the patient had melena with a 2-g drop in hemoglobin. Upper endoscopy revealed acute esophageal necrosis from the cricopharyngeus to the gastroesophageal junction, and biopsies showed inflammatory exudate and necrotic debris. The patient was managed conservatively with bowel rest and intravenous proton pump inhibitor. He recovered without complications and was discharged home.
Case 4
A 25-year-old man with insulin dependent diabetes and hypertension presented with diabetic ketoacidosis, melena, acute anemia, and dysphagia. He used alcohol, cocaine, and cannabis multiple times per week, including as recently as within 48 hours prior to admission. Upper endoscopy revealed circumferential necrosis throughout the esophagus and a mid-esophageal stricture 5 cm in length that could not be traversed by the standard upper endoscope (Figure 2). A gastrostomy tube was surgically placed and supportive therapy was provided. During his prolonged hospitalization, the patient underwent a series of Savary dilations, the first of which was 3 weeks after his presentation. His condition improved and he was discharged home, but continues to require serial dilations for a persistent esophageal stricture (Figure 2).
Figure 2.
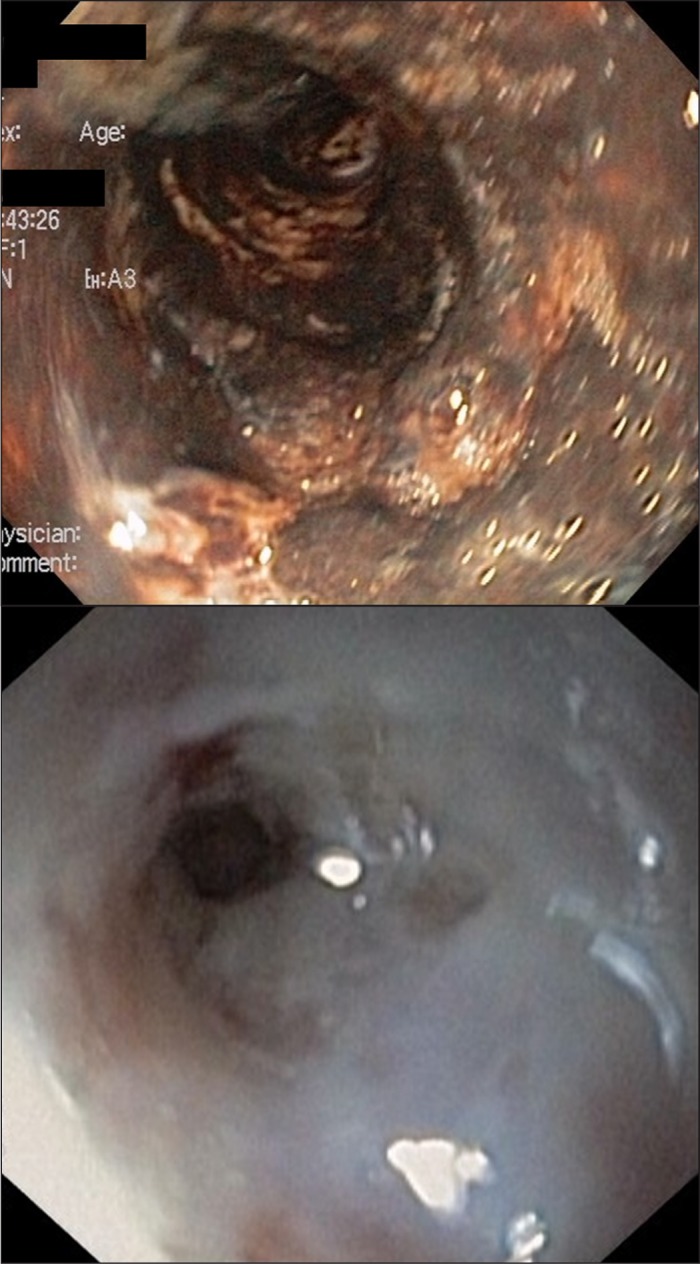
(A) The initial endoscopic appearance in case 4 showing black esophagus with diffuse and circumferential esophageal necrosis. (B) A severe esophageal stricture persisted even after healing, which required serial dilations to maintain patency.
Case 5
A 64-year-old man with a history of hypertension, stroke, gallstones, and alcohol abuse presented to the emergency room with hematemesis and acute anemia requiring transfusion and intravenous fluids. Upper endoscopy revealed pan-esophageal necrosis with circumferential involvement distally. Despite admission to the intensive care unit and maximal medical support, he had rapidly progressive shock and multiorgan system failure followed by cardiac arrest and death.
Case 6
A 49-year-old man with asthma and hypertension presented with fevers, chills, weakness, and syncope that was attributable to endocarditis. His clinical condition deteriorated, with multiorgan dysfunction, melena, and acute anemia. Upper endoscopy revealed necrosis in the distal third of his esophagus (Figure 3). Due to overwhelming infection and progressive multisystem failure, his family decided to withdraw care.
Figure 3.
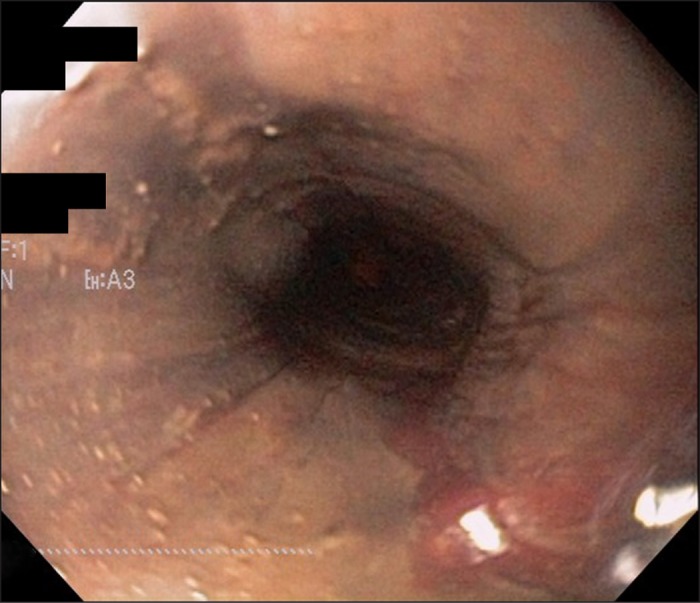
Initial endoscopic appearance in case 6 showing black esophagus with a dusky appearance to the mucosa representing necrosis.
Discussion
Acute esophageal necrosis (AEN), also known as “necrotizing esophagitis,” is a rare but life-threatening condition that is characterized by a striking circumferential black appearance of the esophageal mucosa on endoscopy. This appearance is most frequently seen in the distal esophagus at the gastroesophageal junction, but can extend proximally at various lengths. This pattern may be attributed to a vascular watershed area and a lesser degree of vascularization in the distal esophagus.1,2 Patients with AEN tend to be older men, as medical comorbidities including vascular disease, diabetes, hypertension, renal insufficiency, cardiac disease, pulmonary disease, stroke, and cirrhosis may be more common.3 Younger adults with alcohol or substance abuse can also present with AEN.4 As noted in the above cases, the vast majority of patients are symptomatic and the most common presentation is an upper gastrointestinal bleed with hematemesis or melena seen in up to 90% of cases.3,5
Mortality depends on the underlying condition and is variably reportedly in the literature from 15% to as high as 36% in some series.1,3,6 Causes of death from underlying medical conditions have included systemic infections, sepsis, cardiogenic or hypovolemic shock, pulmonary embolism, and multiple organ dysfunction. However, causes of death specific to underlying esophageal diseases have been reported in less than 10% of cases.2,3 Similarly, in our case series, the 3 patients who did not survive their hospitalization succumbed to multi-organ failure.
While the exact etiology of AEN is unknown, several risk factors have been identified, including gastric outlet obstruction, infections, hyperglycemia, underlying malignancy, irradiation, shock, volvulus, Stevens-Johnson syndrome, acute alcohol abuse, malnourishment, and hypoperfusion. Hypoperfusion can stem from a variety of causes such as sepsis, cocaine use, or volume loss. Often, however, the pathological insult is multifactorial and results from a combination of local ischemia from hypoperfusion, increased acid exposure, and decreased esophageal clearance, which may exacerbate the course of disease process.3,5 The above-mentioned stressors coupled with a dampened mucosal defense with impaired esophageal barrier function can further promote AEN.
The diagnosis and extent of AEN can be determined endoscopically. Histologic data, while not required, can also be supportive. Pathologic examination can reveal necrotic debris, absence of epithelium, deranged muscle fibers, or granulation tissue with leukocytic infiltrates involving the deep esophageal layers.2,4,6 Local complications related to AEN can include perforation, mediastinitis, and stricture formation.
Therapeutic modalities vary, but most authors agree that treatment of AEN should focus on supportive care to maximize organ perfusion, optimization of acid suppression with intravenous proton pump inhibitors, and treatment of infection or sepsis, if present, with appropriate broad-spectrum antibiotic coverage. Treatment of underlying medical conditions is also imperative. Early surgical intervention may also be required in cases of esophageal perforation and/or mediastinal abscess.6
As illustrated by our first case, a high level of caution should be used in situations where naso- or orogastric tubes must be passed, given the fragility of the necrotized esophageal wall, and patients should remain nil-per-os. Likewise, considerations for total parental nutrition can be made on a case-by-case basis in order to avoid enteral feeding-related trauma. Overall, successful management requires multidisciplinary care with intensivists, gastroenterologists, and surgeons. If patients survive, esophageal strictures can be common (10–25%) and generally occur as early as 1 to 2 weeks after the initial diagnosis. The strictures may be refractory and require serial endoscopies with long-term dilation programs.2,3,6-8
Disclosures
Author contributions: All authors contributed to the revision and approval of the manuscript. S. Shafa drafted the manuscript. N. Sharma, J. Keshishian, and ES Dellon collected data and edited the video. ES Dellon is the article guarantor.
Financial disclosure: None to report.
This project was deemed exempt from ongoing review by the UNC and USF IRBs. Informed consent from individual patients or next of kin was not obtained due to this institutional advisement, but all efforts to obscure patient identifiers were made.
References
- 1.Worrell SG, Oh DS, Greene CL, et al. Acute esophageal necrosis: A cases series and long term follow-up. Ann Thorac Surg. 2014;98(1):341–2. [DOI] [PubMed] [Google Scholar]
- 2.Kimura Y, Seno H, Yamashita Y. A case of acute necrotizing esophagitis. Gastrointestinal Endosc. 2014;80(3):525–526. [DOI] [PubMed] [Google Scholar]
- 3.Gurvitis GE, Cherian K, Shami MN, et al. Black esophagus: New insights and multicenter international experience in 2014. Dig Dis Sci. 2015;60(2):444–453. [DOI] [PubMed] [Google Scholar]
- 4.Altenburger DL, Wagner AS, Li S, Garavaglia J. A case of black esophagus with histopathologic description and characterization. Arch Pathol Lab Med. 2011;135(6):797–8. [DOI] [PubMed] [Google Scholar]
- 5.Grudell AB, Mueller PS, Viggiano TR. Black esophagus: Report of six cases and review of the literature, 1963–2003. Dis Esophagus. 2006;19(2):105–110. [DOI] [PubMed] [Google Scholar]
- 6.Gurvitis GE, Shapsis A, Lau N, et al. Acute esophageal necrosis: A rare syndrome. J Gastroenterol. 2007;42(1):29–38. [DOI] [PubMed] [Google Scholar]
- 7.Garas G, Wou C, Sawyer J, et al. Acute oesophageal necrosis syndrome. BMJ Case Reports. 2011:bcr1020103423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akkinepally S, Poreddy V, Moreno A. Black esophagus. Cleve Clin J Med. 2009;76(7):400. [DOI] [PubMed] [Google Scholar]


