Abstract
We present a 24-year-old combat veteran who underwent extensive work-up for elevated aminotransferases, including liver biopsy, with no underlying pathology identified. Subsequent investigations showed elevated creatinine kinase and aldolase. The patient was later diagnosed with biopsy-proven dysferlin-deficient muscular dystrophy. Persistent transaminase elevation despite negative liver work-up should prompt clinicians to consider extrahepatic sources of enzyme elevation. Promptly correlating aminotransferase elevation with musculoskeletal pathology may present an opportunity for clinicians to detect myopathies such as muscular dystrophy in their preclinical stages.
Introduction
Commonly referred to as markers of liver injury, alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are highly concentrated in the liver and are also found in lesser concentrations in the kidney, heart, brain, skeletal muscle, and red blood cells.1 This distribution of aminotransferases makes them nonspecific markers of liver injury, and cases of extrahepatic transaminase leakage are often diagnostic challenges. Rare cases of transaminase elevation leading to the diagnosis of muscular dystrophy have been reported in young children.2,3 This phenomenon in adults is exceedingly rare and often results in years of diagnostic delay and extensive liver workup with no diagnostic endpoint.4,5
Case Report
A 24-year-old male combat veteran with no past medical history presented to clinic for evaluation of elevated aminotransferases. During a routine physical, he was noted to have ALT 240 IU/L and AST 225 IU/L, with alkaline phosphatase 41 IU/L and bilirubin 0.3 mg/dL. The patient denied any personal or family history of liver disease and complete review of systems was unremarkable. The patient denied alcohol and drug use or any over-the-counter supplements. Physical examination revealed a physically fit young man with 5/5 upper and lower extremity strength with no detectable muscular abnormality.
Initial laboratory work-up revealed negative hepatitis virus serologies with undetectable anti-CMV, anti-EBV, and anti-HSV antibodies. Anti-nuclear, anti-mitochondrial, anti-liver–kidney microsomal, and anti-smooth muscle antibodies were negative, and ceruloplasmin, alpha 1-antitrypsin, and iron studies were all within normal limits. Thyroid-stimulating hormone, comprehensive drug screen, serum protein electrophoresis, and liver sonography were unyielding. A 1-month follow-up visit revealed persistently elevated transaminases with AST 221 IU/L and ALT 241 IU/L. Percutaneous liver biopsy revealed nonspecific grade 1 chronic inflammation, mild patchy periportal fibrosis with portal-portal bridging fibrosis stage II, and trace steatosis (Figure 1). Hepatocellular necrosis was not visualized and a multidisciplinary team was unable to explain the degree of transaminase elevation based on the nonspecific liver biopsy results.
Figure 1.
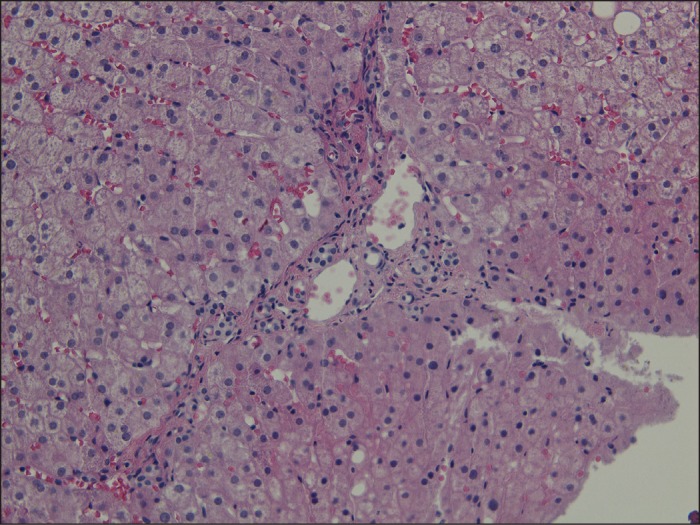
Liver biopsy specimen showing grade 1 chronic inflammation of the portal tract, mild patchy periportal fibrosis with portal-portal bridging bridging fibrosis, and trace steatosis. Pathological findings were determined nonspecific and unable to account for the patient’s degree of chronic transaminase elevation.
The patient returned to clinic with continued elevation of ALT and AST, and new complaints of fatigue. Further laboratory tests revealed elevation of creatinine kinase to 4,956 IU/L and aldolase to 46.9 IU/L. The patient was sent for electromyography, which showed normal nerve conduction with no evidence of myotonia of the distal musculature or paraspinal muscles; however, it did reveal some myopathic features of the iliopsoas muscle. Biopsy of the deltoid muscle showed a mild number of moderately atrophic type I and type II muscle fibers. Further immunohistochemistry for dystrophy-associated proteins demonstrated inconsistent and weak dysferlin expression with normal distribution of sarcoglycan, alphadystroglycan, dystrophin, and collagen type 6 subtypes. The diagnosis of dysferlin-deficient muscular dystrophy was secured and the patient began developing lordosis, difficulty standing, and paraspinal atrophy over the following years.
Discussion
In the absence of musculoskeletal complaints, clinical suspicion for muscle disease often remains low when evaluating elevated aminotransferases. Skeletal muscle is rich in AST, ALT, lactate dehydrogenase, creatinine kinase, aldolase, and pyruvate kinase.6 Creatinine kinase is the most commonly elevated enzyme in myopathies and represents the preferred diagnostic laboratory test for suspected myopathy.6 Any of the aforementioned enzymes may be elevated in musculoskeletal pathology, and a thorough understanding of enzyme distribution may aid clinicians in the diagnosis of extrahepatic illness.7
The presentation of asymptomatic aminotransferase elevation leading to the diagnosis of muscular dystrophy represents a rare phenomenon that is more common in children than adults, often leading to the diagnosis of Duchenne or Becker muscular dystrophy.3 A case series described 5 children who initially presented with elevated transaminases and were diagnosed with either Duchenne or Becker muscular dystrophy.3 Another series reviewed the aminotransferase distribution in 4 children with muscular dystrophy; despite the increased concentration of AST in skeletal muscle when compared to ALT, a relatively equal elevation of aminotransferases was seen in cases of muscular dystrophy.2 Clinical suspicion for underlying muscle pathology often remains higher in children than adults, and atypical musculoskeletal diseases presenting with aminotransferase elevation in adults are often a diagnostic challenge.4,5 The literature reports multiple cases of individuals undergoing many years of work-up for elevated transaminases including liver biopsies before being diagnosed with muscular dystrophy.4,5 Earlier consideration for musculoskeletal pathology may provide an opportunity to diagnose muscular dystrophy in the preclinical stages.
Dysferlin-deficient muscular dystrophy is a slowly progressive autosomal recessive disease that usually presents in late childhood or young adulthood.8 In the early stages of disease, serum muscle enzymes and aminotransferases are elevated prior to the onset of clinically detectable muscle weakness.9 Many patients, as in the presented case, live physically active lifestyles prior to the onset of neuromuscular symptoms, often further diminishing clinical suspicion for musculoskeletal disease.9
Often thought to be exclusive to the liver and commonly mislabeled as markers of liver function, AST and ALT are present in a variety of extrahepatic sites including skeletal muscle. The persistence of transaminase elevation despite negative liver work-up should trigger clinicians to seek extrahepatic causes of transaminase elevation. Work-up in these circumstances should include serum creatinine kinase to evaluate for myopathy along with a thorough history. Correlating aminotransferase elevation with musculoskeletal pathology promptly may represent an opportunity for clinicians to detect myopathies such as muscular dystrophy in their preclinical stages.
Disclosures
Author contributions: T. Aasen drafted the manuscript and performed the literature review, and is the article guarantor. H. Achdjian co-wrote, edited, and revised the manuscript. Y. Usta co-wrote, edited, and critically revised the manuscript. R. Nanda co-wrote and critically revised the manuscript and provided project guidance.
Financial disclosure: None to report.
Acknowledgment: The authors would like to acknowledge the Phoenix VA Health Care System Department of Pathology and Dr. Glenda Amog-Jones for obtaining pathological imaging and providing detailed pathological analysis.
Informed consent was obtained for this case report.
References
- 1.Giannini EG, Testa R, Savarino V. Liver enzyme alteration: A guide for clinicians. CMAJ. 2005;172(3):367–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kohli R, Harris DC, Whitington PF. Relative elevations of serum alanine and aspartate aminotransferase in muscular dystrophy. J Pediatr Gastroenterol Nutr. 2005;41(1):121–4. [DOI] [PubMed] [Google Scholar]
- 3.Zamora S, Adams C, Butzner JD, et al. . Elevated aminotransferase activity as an indication of muscular dystrophy: Case reports and review of the literature. Can J Gastroenterol. 1996;10(6):389–93. [DOI] [PubMed] [Google Scholar]
- 4.Li F, Yin G, Xie Q, Shi G. Late-onset dysferlinopathy presented as “liver enzyme” abnormalities: A technical note. J Clin Rheumatol. 2014;20(5):275–7. [DOI] [PubMed] [Google Scholar]
- 5.Lash T, Kraemer RR. Elevated liver enzymes indicating a diagnosis of limb-girdle muscular dystrophy. J Gen Intern Med. 2014;29(5):813–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolf PL. Abnormalities in serum enzymes in skeletal muscle diseases. Am J Clin Pathol. 1991;95(3):293–6. [DOI] [PubMed] [Google Scholar]
- 7.Rosalki SB. Enzyme assays in diseases of the heart and skeletal muscle. J Clin Pathol Supple (Assoc Clin Pathol). 1970;4:60–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klinge L, Aboumousa A, Eagle M, et al. . New aspects on patients affected by dysferlin deficient muscular dystrophy. J Neurol Neurosurg Psychiatry. 2010;81(9):946–953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Urtizberea JA, Bassez G, Leturcq F, et al. . Dysferlinopathies. Neurol India. 2008;56(3):289–97. [DOI] [PubMed] [Google Scholar]


