Abstract
Severe cholestasis with anabolic androgenic steroids is well-known to cause acute liver injury. Treatment is usually supportive after withdrawal of the offending agent. Acute kidney injury (AKI) frequently occurs in acute liver injury and may complicate management and prognosis. We highlight the use of plasmapheresis resulting in rapid improvement in cholestatic jaundice with resolution of AKI. Plasmapheresis should be considered in special cases in which there is progressive clinical decline despite supportive care.
Introduction
It has been reported that greater than 40% of the U.S. population consumes herbal and dietary supplements (HDS).1 In the past decade alone, a 3-fold rise in liver-related injury attributable to HDS has been reported.2 HDS containing anabolic androgen steroids (AAS) may cause severe cholestatic jaundice, debilitating pruritus, and persistent acute kidney injury (AKI) from suspected bile acid nephropathy. The cholestasis from AAS is usually bland, may last for several months, and eventually resolves once the offending agent is removed, without the need for liver transplantation in the majority of cases. However, deaths have been reported due to secondary effects of malnutrition, renal failure, and infection.3
Case Report
A 31-year-old man was admitted to the hospital for mild confusion, severe pruritus, jaundice, and AKI. Sixteen weeks prior to presentation, he started an HDS regimen for weight loss and muscle building. On average, he consumed 22 capsules per day from 8 different HDS bottles containing at least 80 ingredients, including a cumulative daily dose (104 mg) of anabolic steroids 4-chloro-17αmethyl-andro-4-ene-3,17β-diol (50 mg) and 2α,3αepithio-17αmethyl-51-androstan-17β-ol (54 mg). After reporting fatigue and change in skin color to his local gastroenterologist, HDS was stopped due to suspected drug-induced liver injury.
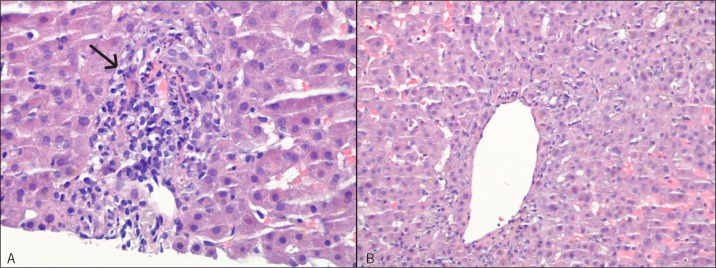
He was hospitalized for severe jaundice with total bilirubin of 53 mg/dL. Viral, autoimmune, and inherited causes of liver disease were ruled out. Magnetic resonance cholangiopancreatography ruled out biliary tract pathology or obstruction. Liver biopsy showed significant cholestasis and mild intraparenchymal neutrophilic infiltrate in hepatocytes surrounding the central veins with no significant necrosis, bile duct injury, or steatosis (Figure 1). Supportive care was provided with intravenous (IV) fluids for pre-renal azotemia, while hydroxyzine, cholestyramine, ursodiol, sertraline, naloxone, and topical emollients were sequentially used for pruritus, with minimal relief. He was started on IV solumedrol 30 mg daily with no improvement in jaundice after 11 days. Over 2 subsequent hospitalizations he continued to have AKI (creatinine 2 mg/dL), persistent jaundice (total bilirubin 46.5 mg/dL), and uncontrolled pruritus. He lost 100 lbs, developed severe insomnia due to pruritus, reported hallucinations, and was re-admitted for concerns of encephalopathy and liver failure. Exam revealed a chronically ill-appearing man with a flat affect, scleral icterus, and pronounced jaundice. He was welloriented to questions but displayed asterixis. He had no tender hepatomegaly, but had extensive excoriations on his torso and extremities induced by pruritus. He had temporal wasting and loss of adipose tissue in his arms and abdomen. Laboratory results during his third hospital admission included an albumin level of 4.7 mg/dL and a prothrombin time of 9.5 s.
Figure 1.
Liver biopsy. (A) Intraparenchymal neutrophilic infiltrate consistent with acute hepatitis. Hepatocyte destruction/necrosis is not significant (grade ¼). Some scattered chronic inflammatory cells are also present (arrow). (B) No appreciable cirrhosis, overt cytopathic effect or fibrosis.
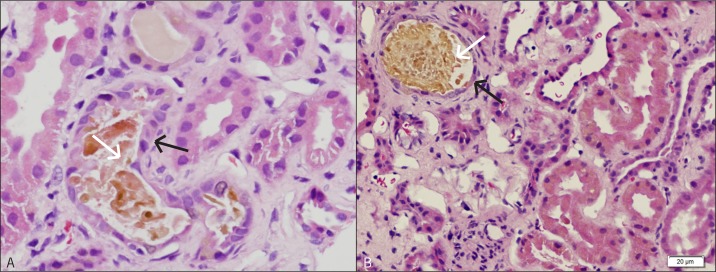
Bile acid nephropathy was suspected due to prolonged exposure to significantly high levels of bile acids at 135 mmol/L (normal <10 mmol/L). Bile acid nephropathy was supported by renal biopsy showing prominent yellow staining of the epithelial lining and the presence of intraluminal bile casts (Figure 2). On hospital day 7, his creatinine was 2.3 mg/dL, BUN 48 mg/dL, and total bilirubin 44.6 mg/dL. Plasmapheresis was initiated to alleviate his pruritus and reduce the burden of circulating bile acids. He underwent 5 sessions of plasmapheresis, which was overall well-tolerated but complicated by the need for one blood transfusion and a minor skin infection. He was discharged on hospital day 20, with total bilirubin 14.4 mg/dL and creatinine 1.3 mg/dL. Six weeks after discharge he was asymptomatic with total bilirubin of 1.2 mg/dL and serum creatinine 0.9 mg/dL.
Figure 2.
Renal biopsy showing prominent brown intraluminal casts, tubular epithelial cells (black arrows), and tubular lumen (white arrows). (A) Many of the tubules are dilated and show epithelial simplification. (B) Tubule with brown staining of the epithelial lining and of the intraluminal cast.
Discussion
Anabolic androgenic steroids (AAS) are considered controlled substances, but are often available online and in health and nutrition shops, marketed as dietary supplements. An internet survey of 500 AAS users found that 78% were noncompetitive bodybuilders or non-athletes.4 C-17 alkylated androgenic steroids, which were integral in our patient’s HDS regimen, are implicated in liver injury resulting in prolonged cholestasis.3 We were not able to exclude concurrent or synergistic hepatotoxicity from the other ingredients in the supplements. Assigning causality in HDS-associated hepatotoxicity is difficult; however, given the pattern of bland and severe cholestasis on his liver biopsy, we strongly suspected AAS as the offending agent. The underlying mechanism for acute and prolonged cholestasis from AAS remains to be elucidated. It is suspected that an unmasking of genetic cholestatic syndromes in predisposed individuals occurs through diminished expression of the bile salt export pump (encoded by ABCB11).5
Cholemic nephrosis, also known as bile acid nephropathy, is a cholestatic condition presumed to occur from direct bile acid-related injury in the form of bile casts, leading to kidney tubular cell damage that result in AKI. Bile acid nephropathy with severe cholestatic liver disease has been described in mice with ligated bile ducts and in jaundiced patients with AKI.6-8 Elevated plasma concentrations of bile salts and bilirubin have been shown to cause nephrotoxicity. However, their exact role in the pathogenesis of jaundice-related nephropathy is not known. Damage to renal tubular cells is considered the cause of the nephropathy, but published data on renal histology has been scarce.9 Our patient’s renal biopsy showed prominent yellow, brown intraluminal tubular casts associated with flattening and simplification of the epithelial lining (Figure 2).
Our patient’s worsening renal function contributed to his prolonged jaundice, as bilirubin is filtered and excreted by the kidneys. His medical condition resulted in depression, inability to work, profound malnutrition, and weight loss. Thus, plasmapheresis, which has anecdotal success in pruritus,10 was undertaken with success. Plasmapheresis is an extracorporeal therapy that removes toxins, protein-bound substances, and even extraneous cells from the body’s circulation. Bile acids and toxins can be removed during plasmapheresis using specialized beads and resins.11 Plasmapheresis has been described in the treatment of pruritus from primary biliary cirrhosis,12 benign recurrent intrahepatic cholestasis,13 acute hepatitis from Epstein-Barr virus,14 and drug-induced liver injury.15 Our patient had a rapid improvement in his cholestatic jaundice, as well as rapid normalization of his renal function at the end of his plasmapheresis sessions, which were sustained during follow-up. Thus, in certain cases of HDS-related liver injury, prolonged persistent cholestasis may lead to persistent kidney injury and pruritus refractory to conventional medical therapy. In selected patients with marked decline from prolonged cholestasis, plasmapheresis may result in a rapid clinical improvement.
Disclosures
Author contributions: All authors wrote the manuscript. A. Flores and RS Rahimi revised the manuscript. RS Rahimi is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Acknowledgments: Claire Adkins, BS, assisted with data collection and Rodrigo Soto, MD, assisted with annotations of the liver biopsy slides.
References
- 1.Seeff LB, Curto TM, Szabo G, et al. . Herbal product use by persons enrolled in the Hepatitis C Antiviral Long-Term Treatment Against Cirrhosis (HALT-C) Trial. Hepatology. 2008;47(2):605–12. [DOI] [PubMed] [Google Scholar]
- 2.Navarro VJ, Barnhart H, Bonkovsky HL, et al. . Liver injury from herbals and dietary supplements in the U.S. Drug-Induced Liver Injury Network. Hepatology. 2014;60(4):1399–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LiverTox Web site. http://livertox.nih.gov. Accessed March 29, 2015.
- 4.Parkinson AB, Evans NA. Anabolic androgenic steroids: A survey of 500 users. Med Sci Sports Exerc. 2006;38(4):644–51. [DOI] [PubMed] [Google Scholar]
- 5.El Sherrif Y, Potts JR, Howard MR, et al. . Hepatotoxicity from anabolic androgenic steroids marketed as dietary supplements: Contribution from ATP8B1/ABCB11 mutations? Liver Int. 2013;33(8):1266–70. [DOI] [PubMed] [Google Scholar]
- 6.Fickert P, Krones E, Pollheimer MJ, et al. . Bile acids trigger cholemic nephropathy in common bile-duct-ligated mice. Hepatology. 2013;58(6):2056–69. [DOI] [PubMed] [Google Scholar]
- 7.van Slambrouck CM, Salem F, Meehan SM, Chang A. Bile cast nephropathy is a common pathologic finding for kidney injury associated with severe liver dysfunction. Kidney Int. 2013;84(1):192–7. [DOI] [PubMed] [Google Scholar]
- 8.Luciano RL, Castano E, Moeckel G, Perazella MA. Bile acid nephropathy in a bodybuilder abusing an anabolic androgenic steroid. Am J Kidney Dis. 2014;64(3):473–6. [DOI] [PubMed] [Google Scholar]
- 9.Betjes MG, Bajema I. The pathology of jaundice-related renal insufficiency: Cholemic nephrosis revisited. J Nephrol. 2006;19(2):229–33. [PubMed] [Google Scholar]
- 10.Beuers U, Kremer AE, Bolier R, and Elferink RP. Pruritus in cholestasis: Facts and fiction. Hepatology. 2014;60:399–407. [DOI] [PubMed] [Google Scholar]
- 11.Jones JS, Dougherty J. Current status of plasmapheresis in toxicology. Ann Emerg Med. 1986;15(4):474-82. [DOI] [PubMed] [Google Scholar]
- 12.Pusl T, Denk GU, Parhofer KG et al. . Plasma separation and anion adsorption transiently relieve intractable pruritus in primary biliary cirrhosis. J Hepatol. 2006;45(6):887–91. [DOI] [PubMed] [Google Scholar]
- 13.Folvik G, Hilde O, Helge GO. Benign recurrent intrahepatic cholestasis: Review and long-term follow-up of five cases. Scand J Gastro. 2012;47(4):482–488. [DOI] [PubMed] [Google Scholar]
- 14.Place E, Wenzel JE, Arumugam R, et al. . Successful plasmapheresis for extreme hyperbilirubinemia caused by acute Epstein-Barr virus. J Pediatr Hematol Oncol. 2007;29:323–6. [DOI] [PubMed] [Google Scholar]
- 15.Suriawinata A, Min AD. A 33-year-old woman with jaundice after azithromycin use. Semin Liver Dis. 2002;22:207–10. [DOI] [PubMed] [Google Scholar]