Abstract
Objective:
To identify the factors influencing women's choice of maternity care providers in Canada.
Method:
Using the Maternity Experience Survey and a multinomial logit model, this paper examined the influence of various socio-economic and demographic factors on the mix of maternity care providers, while controlling for maternal risk profiles. Additionally, provinces were interacted with maternal age to assess the extent to which regional variations in mix of maternity care providers is influenced by pregnant women's needs.
Results:
Besides maternal risk factors, province of prenatal care and the place of residence were found to be statistically significant determinants of choice of maternity care providers. Analysis involving interaction terms indicated wide regional variations in the mix of providers by maternal age.
Conclusions:
The results suggest a wide provincial variation in the mix of maternity care providers. New provincial government initiatives are needed to enhance the supply and capacity of care providers.
Abstract
Objectif:
Déterminer les facteurs qui influent sur le choix, par les femmes, du fournisseur de soins de maternité au Canada.
Méthode:
S'appuyant sur l'Enquête sur l'expérience de la maternité et à l'aide d'un modèle logistique multinomial, cet article examine l'influence de plusieurs facteurs socioéconomiques et démographiques sur la composition des fournisseurs de soins de maternité, tout en contrôlant les profils de maternité à risque. De plus, nous avons considéré le lien entre les provinces et l'âge à la grossesse pour évaluer à quel point les besoins des femmes enceintes influencent les variations régionales dans la composition des fournisseurs de soins de maternité.
Résultats:
Mis à part les facteurs liés à une maternité à risque, la province où sont donnés les soins prénataux et le lieu de résidence s'avèrent des déterminants statistiquement significatifs du choix quant aux fournisseurs de soins de maternité. L'analyse des interactions démontre une grande variation régionale dans la composition des fournisseurs de soins de maternité, et ce, en fonction de l'âge pendant la grossesse.
Conclusions:
Les résultats font voir une grande variation entre les provinces dans la composition des fournisseurs de soins de maternité. Les gouvernements provinciaux devraient adopter de nouvelles initiatives pour accroître la présence et la capacité des fournisseurs de soins.
Over the past two decades, there has been a change in the mix of providers in the provision of maternity care in Canada. While family physicians are involved in many aspects of maternity services, fewer are providing prenatal and intra-partum care than before (CIHI 2004; Godwin et al. 2002; Reid et al. 2000; Zelmer and Leeb 2004). On the other hand, despite the well-developed evidence that midwives are safe and effective in managing low-risk pregnancies, regulation and public funding of midwifery as autonomous providers is currently limited to only some Canadian provinces (Born et al. 2014; Kornelsen 2003; O'Brien et al. 2011). Each type of health provider offers a different style of care in terms of routine screening and diagnostic care, with obstetricians tending to rely more on medical and surgical interventions such as ultrasounds, labour inductions and caesarean section than other providers (Fraser et al. 2000; Guliani et al. 2013; Klein et al. 2009; Monari et al. 2008; O'Brien et al. 2011; Rosenblatt et al. 1997). The scope of practice among providers also varies widely across the country (CIHI 2004; Reid et al. 2000). Despite different practice styles among care providers, few appreciable differences are seen in birth outcomes for women with low-risk pregnancies (Hutton et al. 2009; Jackson et al. 1996; Khan-Neelofur et al. 1998; O'Brien et al. 2011). Indeed, studies suggest that low-risk pregnant women who received their prenatal care from midwives are more likely to have positive maternity experiences and are less likely to access non-obstetric services such as the emergency department during pregnancy than those who were cared for by family physicians or obstetricians (Harvey et al. 2002; Metcalfe et al. 2013; O'Brien et al. 2011).
The resources required to provide maternity care services vary depending on who provides the care as well as the range of services and tests that are performed. A recent pilot study evaluating the costs and outcomes of integrating independent midwifery care with existing healthcare services in the province of Alberta suggested that choice of regulated and publicly funded midwifery care by low-risk women was a cost-effective intervention without adversely affecting maternal or neo-natal outcomes (O'Brien et al. 2010). It is, therefore, imperative to understand what factors influence women's choice of prenatal care provider. Most research to date has looked at the factors that go into patient's provider choice decision in the context of health-seeking behaviour in general (Bernard et al. 2006; Victoor et al. 2012), but studies on determinants of prenatal care provider choice are virtually non-existent in Canada and elsewhere. Existing studies examining the choice of provider in developed countries are mainly concerned with the factors influencing patients' choice of primary care physicians (Bernard et al. 2006; Bornstein et al. 2000; Grytten and Sorensen 2009; McGlone et al. 2002; Victoor et al. 2012) and the relative importance of physicians' gender in patients' selection of obstetrics and gynaecology provider (Johnson et al. 2005; Makam et al. 2010; Plunkett et al. 2002). To the best of this author's knowledge, only one Canadian study by Liva and colleagues (2012) examines the factors influencing nurses' choice of care provider for their own maternity care. However, little is known about the factors influencing women's choice of various types of maternity care providers.
Using the Maternity Experience Survey (MES) of Statistics Canada, and a multinomial logit model (MNL), this paper assessed the influence of various socio-economic and demographic factors on the mix of maternity care providers, while controlling for maternal risk profiles. Specifically, this study aimed to answer two questions. First, what factors influence women's decision to seek care from alternate types of maternity care providers? Second, are there regional variations in the mix of providers for a given risk factor? Regional variations in the mix of maternity care providers may highlight the effect of policies within provinces and can be used to better understand and improve maternity care services.
Methods
Data
This study utilized the data set of the MES conducted by Statistics Canada in 2006 and sponsored by the Public Health Agency of Canada. The MES is the only available nationwide survey that assessed pregnancy, delivery and postnatal experiences of mothers and their children. Participants eligible for the study were women aged 15 years and older, who had singleton live births and who lived with their babies at the time of data collection. After excluding incomplete information, the sample size reduced to 4,829. These missing observations accounted for less than 3% of the responses for most of the variables except household income. The socio-demographic and maternal risk profiles of the respondents with missing observations revealed few differences to those included in the analysis. However, in the case of household income, young and low-income respondents were more likely to have missing data. Therefore, an additional missing category for household income was used in the analysis.
Analysis
In the event of pregnancy, a woman is assumed to seek care from a healthcare system characterized by a variety of healthcare providers. It is further assumed that a woman knows all provider-specific characteristics and will choose a healthcare provider that would yield maximum expected utility (Bolduc et al. 1996; Canaviri 2007). As women's choice of prenatal care provider is a discrete decision, an MNL was used to assess the association between socio-demographic and maternal risk factors on the choice of prenatal care providers. For the MNL model to be a valid framework for inference, the well-known assumption of the independence of irrelevant alternatives (IIA) must be satisfied. To test for the IIA assumption, the Hausman and McFadden specification test was run, and the results suggest that IIA has not been violated in this study. To account for the complex sampling design, the model was estimated using population and bootstrapping weights. All analyses, including bootstrapping, were conducted using STATA (version 13.0) statistical software.
Measures
The dependent variable – types of providers – was grouped into three major categories: obstetricians/gynaecologists (OB/GYNs), family physicians/general practitioners (FP/GPs) and midwives/nurses/nurse practitioners. The reference alternative in this study was OB/GYNs. The theoretical and empirical literature suggests that a patient's demand for healthcare in general and the choice of providers in particular is influenced by various socio-economic and demographic factors such as age, education, income, distance and transportation, health status of an individual and accessibility of care (Bernard et al. 2006; Guliani et al. 2013; Victoor et al. 2012). These independent variables were grouped into: (1) the maternal risk profile, (2) the reproductive history, (3) prenatal care history and (4) socio-economic and demographic factors. Table 1 provides the summary statistics for all variables used in the estimation.
Table 1.
Summary statistics for the dependent and independent variables
| Variable name | N (%) |
|---|---|
| Dependent variable | |
| Type of healthcare provider | |
| Obstetricians and/or gynaecologists (the reference category) | 2,857 (56.0) |
| Family doctors/general practitioners/doctors (unspecified) | 1,920 (37.7) |
| Midwives/nurses/nurse practitioners | 321 (6.3) |
| Independent variables | |
| Maternal risk profile | |
| Maternal age at selected birth | |
| 15-34 | 4,271 (83,8) |
| ≥35 | 827 (16,2) |
| Health problems before pregnancy | |
| Yes | 813 (16,0) |
| No | 4,285 (84,0) |
| Use of medications or technical procedures to get pregnant | |
| Yes | 253 (5,0) |
| No | 4,845 (95,0) |
| Body mass index before pregnancy | |
| Under weight | 284 (5,6) |
| Normal weight (the reference category) | 2,956 (58,0) |
| Overweight | 1,113 (21,8) |
| Obese | 745 (14,6) |
| Planned caesarean for medical reasons | |
| Yes | 601 (11,8) |
| No | 4,497 (88,2) |
| Reproductive history | |
| Any miscarriage, tubal or ectopic pregnancy or stillbirth history | |
| Yes | 1,595 (31,3) |
| No | 3,503 (68,7) |
| Any premature birth before | |
| Yes | 490 (9,6) |
| No | 4,608 (90,4) |
| Parity | |
| 1 (the reference category) | 2,432 (47,7) |
| 2 | 1,913 (37,5) |
| 3 | 544 (10,7) |
| 4 | 147 (2,9) |
| 5 + | 62 (1,2) |
| Prenatal care history | |
| Received prenatal care as early as wanted | |
| Yes | 4,554 (89.3) |
| No | 544 (10.7) |
| Number of prenatal visits | |
| 1-4 | 51 (1.0) |
| ≥5 | 5,047 (99.0) |
| Socio-economic and demographic factors | |
| Area of residence | |
| Rural | 1,103 (21.6) |
| Semi-urban (the reference category) | 1,435 (28.2) |
| Urban | 2,560 (50.2) |
| Province of prenatal care | |
| Atlantic | 918 (18.0) |
| Quebec | 992 (19.5) |
| Ontario (the reference category) | 1,578 (31.0) |
| Manitoba | 291 (5.7) |
| Saskatchewan | 269 (5.3) |
| Alberta | 525 (10.3) |
| British Columbia | 525 (10.3) |
| Maternal education | |
| Less than high school | 359 (7.0) |
| High-school graduate | 702 (13.8) |
| Post-secondary diploma (the reference category) | 2,194 (43.0) |
| University graduate | 1,843 (36.2) |
| Household income | |
| <20,000 | 411 (8.4) |
| $20,000-$39,000 | 921 (18.9) |
| $40,000-$59,000 | 988 (20.2) |
| $60,000-$79,000 | 933 (19.1) |
| ≥$80,000 (the reference category) | 1,631 (33.4) |
| Nativity | |
| Canadians (the reference category) | 4,080 (80,0) |
| Aboriginals | 210 (4,1) |
| Immigrants | 808 (15,9) |
| Marital status | |
| Married (the reference category) | 3,460 (67,9) |
| Common-law partner | 1,229 (24,1) |
| Divorced | 69 (1,4) |
| Single | 340 (6,7) |
| Employment status during pregnancy | |
| Employed | 3,518 (69,0) |
| Not employed | 1,580 (31,0) |
Potential maternal risk factors included the maternal age at selected birth, any health problems before pregnancy that required taking medication for more than two weeks, use of medications or technology to get pregnant and having a planned C-section owing to medical reasons. Another risk indicator was the woman's body mass index before pregnancy, which was here categorized into four groups: underweight, normal weight (the reference category), overweight and obese. A pregnancy was considered to be risky if the woman was obese or overweight before pregnancy. Reproductive history was represented by parity and a history of complications in a prior pregnancy associated with miscarriage, tubal/ectopic pregnancy, stillbirth and premature birth. Similarly, prenatal care variables were included to capture the relationship between choice of prenatal care provider and the timings and frequency of prenatal care. The socio-economic and demographic factors included in this study were the province of prenatal care, an urban or rural place of residence, maternal education, the total household income, the marital status, employment status and the residency status of the woman. Because of the smaller number of observations, the four Atlantic provinces were grouped into one category. The place of residence was classified into three groups: rural, semi-urban (population 30,000–<499,999) and urban (population ≥500,000) (the reference category). Maternal education was measured according to four broad categories: less than high school, high-school graduate, post-secondary diploma (the reference category) and university graduate. The annual household income was categorized into five groups: <$20,000, $20,000–<$40,000, $40,000–<$60,000, $60,000–<$80,000 and $80,000 or more (the reference category). Nativity/ethnicity was measured according to three broad categories: aboriginal Canadians, non-aboriginal Canadians and immigrants.
Results
Descriptive statistics
At the national level, 56% and 38% of women, respectively, reported receiving care from OB/GYNs and FP/GPs for their prenatal care, whereas only 6% percent received care from midwives/nurses. These national averages, however, masked wide variations in the mix of maternity care providers across provinces (Figure 1). The percentage of women who received care from OB/GYNs ranged from 66% to 68% in Quebec and Ontario; 49% to 51% in Atlantic Provinces, Alberta and Manitoba; and 34% to 38% in Saskatchewan and British Columbia. Similarly, the percentage of women who received care from FP/GPs ranged from 52% to 66% in British Columbia and Saskatchewan to 48% to 49% in Alberta and the Atlantic Provinces and 24% to 38% in Ontario, Quebec and Manitoba. The proportion of women who received care from midwives/nurses ranged from 2% in the Atlantic provinces to 10% to 11% in British Columbia and Manitoba. Inter-provincial variations in the provision of maternal care were also noticeable by maternal age.
Figure 1.
Mix of maternity care providers by province (%)
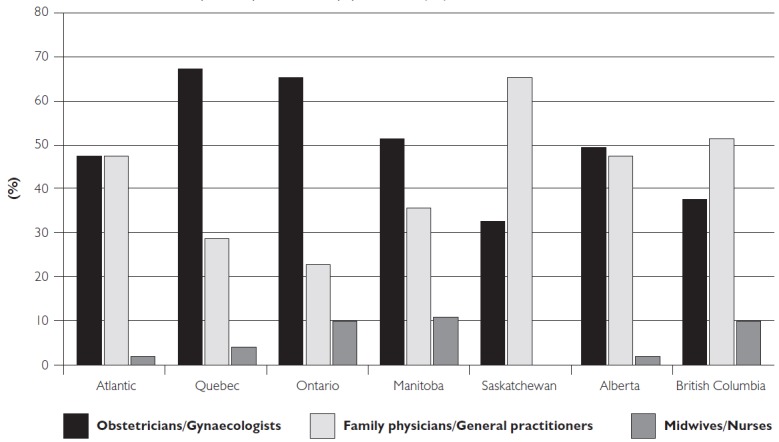
Note: The Statistics Canada disclosure control rules preclude from reporting the estimates for midwives/nurses for Saskatchewan owing to less than minimum required observations.
Econometric results
The regression results from the multinomial model are presented in Table 2. To facilitate interpretation, the estimated coefficients were converted to odds ratios. As expected, choice of healthcare provider was responsive to need. Maternal risk factors such as higher maternal age (≥35), health problems before pregnancy, use of medical procedures to get pregnant and planned caesarean for medical reasons decreased the odds of receiving care from FP/GPs over OB/GYNs (the reference category). Similarly, women who received their prenatal care as early as they wanted were 78% more likely to receive care from FP/GPs over OB/GYNs, but the effect was insignificant for midwives/nurses.
Table 2.
Multinomial regression results for the choice of three types of provider: OB/GYNs (the reference category), FP/GPs and midwives/nurses
| Prob (Y) = FP/GPs | Prob (Y) = midwives/nurses | |||
|---|---|---|---|---|
| Odds ratio | 95% CI | Odds ratio | 95% CI | |
| Maternal risk profile | ||||
| Maternal age at selected birth | 0.81* | 0.66, 0.98 | 1.40 | 1.00, 1.96 |
| Health problems before pregnancy | 0.71** | 0.58, 0.87 | 1.06 | 0.77, 1.47 |
| Technical pregnancy | 0.55** | 0.40, 0.77 | 0.49* | 0.24, 0.98 |
| Body mass index before pregnancy (ref. category: normal weight) | ||||
| Underweight | 1.34 | 1.00, I.8C | 0.90 | 0.49, 1.64 |
| Overweight/Obese | 1.06 | 0.92, 1.23 | 1.05 | 0.79, 1.38 |
| Planned caesarean | 0.61** | 0.49, 0.75 | 0.37** | 0.22, 0.64 |
| Any premature birth before | 1.06 | 0.84, 1.33 | 1.00 | 0.63, 1.58 |
| Any previous miscarriage, tubal/ectopic pregnancy or stillbirth | 0.85* | 0.73, 0.98 | 0.90 | 0.69, 1.19 |
| Parity (ref. category: first birth) | ||||
| 2 | 1.00 | 0.86, 1.16 | 0.83 | 0.64, 1.08 |
| 3 | 1.14 | 0.90, 1.45 | 0.73 | 0.45, 1.19 |
| 4 | 1.25 | 0.82,1.91 | 0.72 | 0.28, 1.91 |
| ≥5 | 1.09 | 0.56,2.13 | 2.10 | 0.82, 5.37 |
| Prenatal care history | ||||
| Early prenatal care | 1.78** | 1.43, 2.23 | 1.20 | 0.78, 1.85 |
| Five or more visits (ref. category: <5 visits) | 0.30* | 0.13, 0.69 | 1.97 | 0.27, 14.23 |
| Socio-economic and demographic factors | ||||
| Province of residence (ref. category: Ontario) | ||||
| Atlantic | 1.81** | 1.50, 2.16 | 0.18** | 0.10, 0.30 |
| Quebec | 1.09 | 0.89, 1.34 | 0.31** | 0.21, 0.47 |
| Manitoba | 1.63** | 1.24, 2.12 | 1.36 | 0.90, 2.06 |
| Alberta | 2 39** | 1.93, 2.95 | 0.36** | 0.20, 0.66 |
| British Columbia | 4.20** | 3.33, 5.30 | 2.00** | 1.41, 2.84 |
| Area of residence (ref. category: urban) | ||||
| Rural | 2,00** | 1,67, 2,39 | 1,32 | 0,93,1,88 |
| Semi-urbar | 2 12** | 1,80, 2,49 | 1,42* | 1,04,1,94 |
| Household income (ref. category: >$80,000) | ||||
| <$20,000 | 1,16 | 0,83, 1,61 | 1,66 | 0,91, 3,03 |
| $20,000-<$40,000 | 1,02 | 0,82, 1,27 | 1 79** | 1,22, 2,63 |
| $40,000-<$60,000 | 0,96 | 0,79, 1,16 | 1,23 | 0,85, 1,77 |
| $60,000-<$80,000 | 0,80* | 0,66, 0,97 | 1,01 | 0,70, 1,44 |
| Education (ref. category: post-secondary diploma) | ||||
| Less than high school | 1,12 | 0,84, 1,51 | 0,66 | 0,36, 1,20 |
| High-school graduate | 1,35* | 1,09, 1,67 | 0,73 | 0,46, 1,16 |
| University graduate | 1,15 | 0,98, 1,35 | 1 99** | 1,48, 2,66 |
| Marital status (ref. category: married) | ||||
| Common-law partner | 0,93 | 0,77, 1,11 | 1,25 | 0,87,1,79 |
| Divorced | 0,72 | 0,38, 1,34 | 1,16 | 0,35, 3,89 |
| Single | 0,98 | 0,71, 1,35 | 0,94 | 0,50,1,76 |
| Nativity (ref. category: Canadian) | ||||
| Aboriginal | 1,06 | 0,75, 1,51 | 1,85* | 1,05, 3,28 |
| Immigrant | 0,57** | 0,46, 0,70 | 0,52** | 0,36, 0,75 |
| Employment status | 0,95 | 0,80, 1,11 | 0,68* | 0,51, 0,91 |
Significant at p < 0.05
Significant at p < 0.01
OB/GYNs = obstetricians/gynaecologists; FP/GPs = family physicians/general practitioners
Among the socio-economic and demographic factors, the province of prenatal care and the geographic area of residence were found to be the strongest predictors of choice of prenatal care provider, even after controlling for maternal risk factors. The estimated odds ratios on the province of prenatal care were statistically significant (at 1%) for all but Quebec in the FP/GPs model and Manitoba in the midwives/nurses model. The odds of receiving care from FP/GPs over OB/GYNs were 1.6–2.4 times more for women in Manitoba, Atlantic provinces and Alberta compared with women in Ontario (the reference category). The odds of receiving care from FP/GPs over OB/GYNs were more pronounced for British Columbia, where pregnant women were 4.2 times more likely to receive care from FP/GPs than women in Ontario. While women in most provinces were less likely to receive care from midwives/nurses over OB/GYNs, in British Columbia, pregnant women were two times more likely to consult midwives/nurses over OB/GYNs than their counterparts in Ontario (the reference category). Saskatchewan was excluded in our multinomial regression model owing to very few numbers of observations on midwives/nurses for this province. However, the results were robust to the exclusion of Saskatchewan in seeking care from two dominant types of providers – FP/GPs and OB/GYNs. As expected, rural and semi-urban women were two times more likely to receive care from FP/GPs over OB/GYNs than urban women (the reference category). Semi-urban women were also 42% more likely to receive care from midwives/nurses than urban women. No clear pattern was observed between income and the types of prenatal care provider. The odds of receiving care from midwives/nurses over OB/GYNs were 99% more for university graduates compared with post-secondary diploma (the reference category). Compared with non-aboriginal Canadians (the reference category), immigrant women were 43% and 48%, respectively, less likely to receive care from FP/GPs and midwives/nurses over OB/GYNs. The odds of receiving care from midwives/nurses (over OB/GYNs) were 85% more for aboriginal Canadians than non-aboriginal Canadians. However, these results should be interpreted with caution, given that the sample size on aboriginal was very small and heterogeneous, covering only those living off reserves.
To assess whether inter-provincial variations in the mix of providers vary in strength for a given risk factor, the regression model was further extended by interacting provinces with maternal age (Table 3). As there were very few observations by age for midwives/nurses in some provinces, the extended model compares the choice of two dominant types of providers (OB/GYNs and FP/GPs) by maternal age across provinces using logistic regression. Overall, the results suggested that mothers living in Ontario, irrespective of their age, were more likely to receive care from OB/GYNs than their counterparts in other provinces. Compared with Ontario, higher age (∵35), pregnant women in Atlantic, Saskatchewan, Alberta and British Columbia were 56%–76% less likely to receive care from OB/GYNs than FP/GPs. The results for interaction terms between younger women (age <35) and provinces indicated even more widespread differences in receiving care from alternative providers. Low-risk pregnant women (<35) in Western provinces were 44%–76% less likely to receive care from OB/GYNs than their counterparts in Ontario.
Table 3.
Logistic regression results for interaction terms between the maternal age and province of prenatal care for the choice of two types of providers: OB/GYNs (the reference category) and FP/GPsa
| Maternal age x province (ref. category: Ontario) | If age <35 | If age ≥35 | ||
|---|---|---|---|---|
| Odds ratio | 95% CI | Odds ratio | 95% CI | |
| Province | ||||
| Atlantic | 0.58* | 0.47, 0.70 | 0.44* | 0.28, 0.69 |
| Quebec | 0.92 | 0.74, 1.14 | 1.1 | 0.60, 2.04 |
| Manitoba | 0.56* | 0.42, 0.75 | 0.96 | 0.41, 2.28 |
| Saskatchewan | 0.27* | 0.21, 0.36 | 0.31* | 0.14, 0.68 |
| Alberta | 0.45* | 0.36, 0.57 | 0.26* | 0.15, 0.43 |
| British Columbia | 0.24* | 0.18, 0.31 | 0.24* | 0.15, 0.38 |
a Other regressors in the model correspond to those listed in Table 2.
* Significant at p < 0.05
** Significant at p < 0.01
OB/GYNs = obstetricians/gynaecologists; FP/GPs = family physicians/general practitioners
Discussions and Conclusions
This study empirically assessed the influence of various socio-economic and demographic factors on the mix of maternity care providers in Canada, while controlling for various maternal risk factors. The results suggested that besides maternal risk factors, province of prenatal care and the place of residence were found to be statistically significant determinants of mix of maternity care providers. The results were more noticeable in the choice of OB/GYNs versus FP/GPs than for midwives/nurses. Additional analysis involving interactions between provinces and maternal age indicated wide interprovincial variations in the mix of providers for a given risk factor.
Province and area of residence were found to be the strongest predictors of mix of prenatal care providers. A study from the US also suggests that economics and geography are stronger predictors of a woman's initial choice of provider than medical and obstetric risk factors (Dobie et al. 1994). Compared with Ontario, women in all other provinces were more likely to receive care from FP/GPs over OB/GYNs, with the odds being particularly more pronounced for residents of British Columbia and Alberta. Similarly, except for British Columbia, women in all other provinces were more likely to choose OB/GYNs over midwives/nurses. The results also suggested that FP/GPs were the preferred form of care in rural and semi-urban areas than in the urban area. These provincial and geographic variations reflect differences in the distribution and characteristics of alternative providers and the scope of practice among these providers in a given region or healthcare policies in these regions (Wennberg and Gittelsohn 1982; Zuckerman et al. 2010). The supply of FP/GPs and OB/GYNs varies across provinces, with Alberta and British Columbia having the lowest number of OB/GYNs per 100,000 (CIHI 2013). Given the higher proportion of OB/GYNs in Ontario and to the extent that patient's perception of quality of care is equated with the provision of high-tech care, women in this province are more likely to choose OB/GYNs irrespective of their maternal risk (Guliani 2013; Ikegami and Campbell 1999). Similarly, the number of midwives per 100,000 ranges from five in Manitoba to one in Saskatchewan (CIHI 2014). These numbers have not changed substantially over the past decade. Even though midwifery has now been regulated in most provinces (with the exception of Prince Edward Island and Yukon), progress to formally integrate them into the health system has been slow and uneven across the country (Born et al. 2014; CAM 2012). For instance, despite the approval of the Midwifery Act in 2010, New Brunswick had no practicing registered midwives until 2013 (CAM 2013). Similarly, Newfoundland and Labrador had no licensed or practicing midwives regardless of incorporation of midwives in the Health Professions Act (Born et al. 2014; CAM 2013). Access to any type of maternity care providers has always remained limited in rural areas of Canada, and the picture is getting bleaker every year with more and more FPs opting out of maternity care practice as well as a national shortage of midwives. Thus, even though care is publicly funded and women may choose their care providers, choices may be limited in practice owing to unequal distribution of various providers across the country (O'Brien et al. 2011). The results from the interaction terms also suggested that OB/GYNs were the dominant type of maternity care provider in Ontario, irrespective of maternal age. Regional variations for a given risk factor further highlighted variations in the availability and distribution of providers, differences in provider style of practice or healthcare policies in these regions.
Some caveats are in order. First, the timing of interviews in the MES varied from 5 to 14 months postpartum, which might have influenced both maternal recall and perceptions of some events and experiences. Second, the data did not allow us to control for providers' practice characteristics, nor for the supply of providers in the region. However, to the extent to which the supply of providers varies by province, the inclusion of a province dummy variable may capture, at least partly, the relationship between the supply of providers and women's use of maternity provider. Third, results may have been subject to endogeneity bias, if there were unobserved factors such as the perception of the quality and service of the provider, preference for certain medical procedures or just a preference for being treated in a certain way may influence the mix of provider.
In conclusion, the results of this study have important policy implications with respect to the utilization of maternity care in Canada. New provincial government initiatives are needed to support collaborative and integrated care for expectant mothers. Policies aimed at enhancing the supply and capacity of FPs and midwives/nurses in providing a broad range of clinical services to low-risk patients will make a greater contribution to maternity care (CIHI 2004; Kornelsen 2003). By increasing the availability and widening the mix of providers, these initiatives will broaden the choice set of low-risk pregnant women and their families in the birthing process.
References
- Bernard M.E., Sadikman J.C., Sadikman C.L. 2006. “Factors Influencing Patients' Choice of Primary Medical Doctors.” Minnesota Medicine 89(1): 46–50. [PubMed] [Google Scholar]
- Bolduc D., Lacriox G., Muller C. 1996. “The Choice of Medical Providers in Rural Bénin: A Comparison of Discrete Choice Models.” Journal of Health Economics 15(4): 477–98. [DOI] [PubMed] [Google Scholar]
- Born K., Chiasson C.-A., Gutfreund S., Jackson L., Levy E., Litwack-Goldman J. et al. 2014. “Midwifery: Special Delivery” in Deber R.A., Mah's C.L., eds., Case Studies in Canadian Health Policy and Management (2nd ed.). Toronto: University of Toronto Press. [Google Scholar]
- Bornstein B.H., Marcus D., Cassidy W. 2000. “Choosing a Doctor: An Exploratory Study of Factors Influencing Patients' Choice of a Primary Care Doctor.” Journal of Evaluation in Clinical Practice 6(3): 255–62. [DOI] [PubMed] [Google Scholar]
- Canadian Association of Midwives (CAM). 2012. “Annual Report 2011–12.” Retrieved March 2, 2015. <http://www.canadianmidwives.org/DATA/DOCUMENT/Annual_Report2011_2012FINAL_ENG.pdf>.
- Canadian Association of Midwives (CAM). 2013. “Midwifery in Canada – Provinces/Territories.” Retrieved March 2, 2015. <http://www.canadianmidwives.org>.
- Canadian Institute for Health Information (CIHI). 2004. Giving Birth in Canada: Providers of Maternity and Infant Care. Ottawa: Canadian Institute for Health Information; Retrieved September 20, 2014. <https://secure.cihi.ca/free_products/GBC2004_report_ENG.pdf>. [Google Scholar]
- Canadian Institute for Health Information (CIHI). 2013. Supply, Distribution and Migration of Canadian Physicians. Ottawa: Canadian Institute for Health Information; ” Retrieved October 13, 2014. <https://secure.cihi.ca/estore/productSeries.htm?pc=PCC34>. [Google Scholar]
- Canadian Institute for Health Information (CIHI). 2014. Canada's Health Care Providers: Provincial Profiles – 2012. Ottawa: Canadian Institute for Health Information. [Google Scholar]
- Canaviri J. 2007. “A Random Parameter Logit Model for Modeling Health Care Provider Choice in Bolivia.” Available at SSRN: <http://dx.doi.org/10.2139/ssrn.987101>.
- Dobie S.A., Hart L.G., Fordyce M., Rosenblatt R.A. 1994. “Do Women Choose Their Obstetric Providers Based on Risks at Entry into Prenatal Care? A Study of Women in Washington State.” Obstetrics & Gynecology 84(4): 557–64. [PubMed] [Google Scholar]
- Fraser W., Hatem-Asmar M., Krauss I., Maillard F., Bréart G., Blais R. 2000. “Comparison of Midwifery Care to Medical Care in Hospitals in the Quebec Pilot Projects Study: Clinical Indicators.” Canadian Journal of Public Health 91(1): 5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godwin M., Hodgetts G., Seguin R., MacDonald S. 2002. “The Ontario Family Medicine Residents Cohort Study: Factors Affecting Residents' Decisions to Practise Obstetrics.” Canadian Medical Association Journal 166(2): 179–84. [PMC free article] [PubMed] [Google Scholar]
- Grytten J., Sorensen R.J. 2009. “Patient Choice and Access to Primary Physician Services in Norway.” Health Economics, Policy and Law 4(1): 11–27. [DOI] [PubMed] [Google Scholar]
- Guliani H., Sepehri A., Serieux J. 2013. “Does the Type of Provider and the Place of Residence Matter in the Utilization of Prenatal Ultrasonography? Evidence from Canada.” Applied Health Economics and Health Policy 11(5): 471–84. [DOI] [PubMed] [Google Scholar]
- Harvey S., Rach D., Stainton M.C., Jarrell J., Brant R. 2002. “Evaluation of Satisfaction with Midwifery Care.” Midwifery 18(4): 260–67. [DOI] [PubMed] [Google Scholar]
- Hutton E.K., Reitsma A.H., Kaufman K. 2009. “Outcomes Associated with Planned Home and Planned Hospital Births in Low-Risk Women Attended by Midwives in Ontario, Canada, 2003–2006: A Retrospective Cohort Study.” Birth 36(3): 180–98 [DOI] [PubMed] [Google Scholar]
- Ikegami N., Campbell J. 1999. “Health Care Reform in Japan: The Virtues of Muddling Through.” Health Affairs 18(3): 26–36. [DOI] [PubMed] [Google Scholar]
- Jackson E.A., Francke L., Vsilenko P. 1996. “Management of Gestational Diabetes by Family Physicians and Obstetricians.” Journal of Family Practice 43(4): 383–88. [PubMed] [Google Scholar]
- Johnson A., Schnatz P., Kelsey A., Ohannessian C. 2005. “Do Women Prefer Care from Female or Male Obstetrician-Gynecologists? A Study of Patient Gender Preference.” BMC Medical Education 105: 369–79. [PubMed] [Google Scholar]
- Khan-Neelofur D., Gulmezoglu M., Villar J. 1998. “Who Should Provide Routine Antenatal Care for Low-Risk Women, and How Often? A Systematic Review of Randomized Controlled Trials. WHO Antenatal Care Trial Research Group.” Paediatric and Perinatal Epidemiology 12(2): 7–26. [DOI] [PubMed] [Google Scholar]
- Klein M.C., Kaczorowski J., Hall W.A., Fraser W.D., Liston R.M., Eftekhary S. et al. 2009. “The Attitudes of Canadian Maternity Care Practitioners towards Land Birth: Many Differences but Important Similarities.” Journal of Obstetrics and Gynaecology Canada 31(9): 827–40. [DOI] [PubMed] [Google Scholar]
- Kornelsen J. 2003. Solving the Maternity Care Crisis: Making Way for Midwifery's Contribution. Vancouver: British Columbia Centre of Excellence for Women's Health; Retrieved September 18, 2014. <http://bccewh.bc.ca/wp-content/uploads/2012/05/2003_Solving-the-Maternity-Care-Crisis-Policy-Brief.pdf>. [Google Scholar]
- Liva S.J., Hall W.A., Klein M.C., Wong S.T. 2012. “Factors Associated with Differences in Canadian Perinatal Nurses' Attitudes towards Birth Practices.” Journal of Obstetric, Gynecologic, & Neonatal Nursing 41(6): 761–73. 10.1111/j.1552-6909.2012.01412.x. [DOI] [PubMed] [Google Scholar]
- Makam A., Mallappa S., Edwards G. 2010. “Do Women Seeking Care from Obstetrician-Gynaecologists Prefer to See a Female or a Male Doctor?” Archives of Gynecology and Obstetrics 281(3): 443–47. 10.1007/s00404-009-1199-5. [DOI] [PubMed] [Google Scholar]
- McGlone T.A, Butler E.S., McGlone V.L. 2002. “Factors Influencing Consumers' Selection of a Primary Care Physician.” Health Marketing Quarterly 19(3): 21–37. [DOI] [PubMed] [Google Scholar]
- Metcalfe A., Grabowska K., Weller C., Tough S.C. 2013. “Impact of Prenatal Care Provider on the Use of Ancillary Health Services During Pregnancy.” BMC Pregnancy and Childbirth 13(62). 10.1186/1471-2393-13-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monari F., Di S., Facchinetti Mario, F., Basevi V. 2008. “Obstetricians' and Midwives' Attitudes toward Caesarean Section.” Birth 35(2): 129–35. [DOI] [PubMed] [Google Scholar]
- O'Brien B., Chalmers B., Fell D., Heaman M., Darling E., Herbert P. 2011. “The Experience of Pregnancy and Birth with Midwives: Results from the Canadian Maternity Experiences Survey.” Birth 38(3): 207–15. 10.1111/j.1523-536X.2011.00482.x. [DOI] [PubMed] [Google Scholar]
- O'Brien B., Harvey S., Sommerfeldt S., Beischel S., Newburn-Cook C., Schopflocher D. 2010. “Comparison of Costs and Associated Outcomes between Women Choosing Newly Integrated Autonomous Midwifery Care and Matched Controls: A Pilot Study.” Journal of Obstetrics and Gynaecology Canada 32(7): 650–56. [DOI] [PubMed] [Google Scholar]
- Plunkett B., Kohli P., Milad M. 2002. “The Importance of Physician Gender in the Selection of an Obstetrician or a Gynecologist.” American Journal of Obstetrics and Gynecology 186(5): 926–28. [DOI] [PubMed] [Google Scholar]
- Reid A.J., Grava-Gubins I., Carroll J.C. 2000. “Family Physicians in Maternity Care: Still in the Game? Report from the CFPC's Janus Project.” Canadian Family Physician 46(3): 601–06, 609-11. [PMC free article] [PubMed] [Google Scholar]
- Rosenblatt R., Dobie S., Hart Gary L. 1997. “Interspecialty Differences in Obstetric Care of Low-Risk Women.” American Journal of Public Health 87(3): 344–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victoor A., Delnoij D., Friele R., Rademakers J. 2012. “Determinants of Patient Choice of Healthcare Providers: A Scoping Review.” BMC Health Services Research 12(27). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg J, Gittelsohn A. 1982. “Variations in Medical Care among Small Areas.” Scientific American 246(4): 120–34. [DOI] [PubMed] [Google Scholar]
- Zelmer J., Leeb K. 2004. “Challenges for Providing Maternity Services: The Impact of Changing Birthing Practices.” Healthcare Quarterly 7(3): 21–23. [DOI] [PubMed] [Google Scholar]
- Zuckerman S., Waidmann T., Berenson R., Hadley J. 2010. “Clarifying Sources of Geographic Differences in Medicare Spending.” New England Journal of Medicine 363(1): 54–62. [DOI] [PubMed] [Google Scholar]


