Abstract
Accommodation consists of changes in family members’ behavior to prevent or reduce patients’ obsessive-compulsive disorder (OCD) rituals or distress. High levels of family accommodation are associated with more severe symptoms and functional impairment on the part of patients, and may also interfere with exposure-based treatment. The purpose of this study was to develop and test a brief, adjunctive intervention to reduce accommodation in the family members of adult OCD patients. Patients (N = 18, mean age = 35.44, 33% male, 94% Caucasian) received a course of standard individual exposure and ritual prevention (ERP) for OCD. Family members (N = 18, mean age = 41.72, 56% male, 94% Caucasian) were randomized to either receive or not receive the adjunctive intervention, consisting of two sessions of psychoeducation and skills training in reducing accommodation. Results revealed that the intervention successfully reduced scores on the clinician-rated the Family Accommodation Scale (Week 8 d = 1.05). Patients whose family members received the intervention showed greater reductions in Y-BOCS scores across treatment than patients whose family members had not (Week 8 d = 1.27), and hierarchical regression analyses revealed that change in family accommodation from baseline accounted for a significant amount of variance in later OCD symptoms (β = .45, p = .02). Results from this preliminary study suggest that this adjunctive intervention produces more rapid treatment response compared to traditional ERP alone. Accommodation is a potentially important target for improving treatment in OCD and other diagnostic groups where accommodation is likely to occur.
Keywords: Accommodation, family, obsessive-compulsive disorder
Introduction
Obsessive-compulsive disorder (OCD) is defined by the experience of repetitive, intrusive, anxiety-provoking thoughts or images (obsessions) and/or the performance of overt or mental rituals for the purpose of relieving anxiety (compulsions) (American Psychiatric Association, 2013). Patients with OCD experience substantial emotional distress in addition to impairment across many life domains (Olatunji, Cisler, & Tolin, 2007), and interpersonal relationships, particularly within families, have been found to be especially negatively affected in OCD (Lebowitz, Panza, Su, & Bloch, 2012; Storch et al., 2007), with high levels of family burden and distress (Calvocoressi et al., 1999).
Indeed, recent research makes it clear that the impact of OCD symptoms extends beyond the individual patient, and also that family reactions may, in turn, affect the course of the disorder (Caporino et al., 2012; Van Noppen & Steketee, 2009). OCD symptoms often center on activities of daily living such as eating, bathing, or being in public, so the disorder can be especially disruptive to patients’ and families’ functioning. Family members are easily drawn into behaviors such as rituals or avoidance via “accommodation,” a term that includes any changes in family members’ behavior aimed at preventing or reducing the patient’s distress related to their OCD symptoms (Calvocoressi et al., 1999) or to decrease the time spent ritualizing. Examples of accommodation by family members include engaging in rituals (e.g., checking or cleaning excessively), providing necessary supplies for rituals (e.g., extra soap), or giving verbal reassurance related to OCD concerns (e.g., telling a patient with disturbing mental images of harming loved ones, “You’re not a dangerous person – I know you’d never hurt anyone!”). Rates of accommodation are high, with reports from relatives of both child and adult patients ranging from 62–100% (Renshaw, Steketee, & Chambless, 2005).
Accommodation occurs for a variety of reasons; it may be directly requested by the patient, or provided out of a practical desire to reduce time-consuming rituals in the moment, or intended to reduce patient distress (Calvocoressi et al., 1999). Accommodation is often “successful” in the short term, in the sense of relieving the patient’s anxiety and facilitating the rapid completion or avoidance of compulsive behavior. However, these family responses prevent the patient from confronting his/her obsessional thoughts and the anxiety that they provoke. Although this may make it somewhat easier for the family to function in the short term, it ultimately contributes to the maintenance of the patient’s obsessions and creates an escalating loop between the accommodation behaviors and the OCD symptoms. Furthermore, accommodation reduces the natural consequences of OCD behavior (e.g., interference with pleasurable or more highly valued activities, or the failure to complete other necessary tasks due to the time spent on rituals), potentially reducing patients’ motivation for change. Research has consistently identified a cross-sectional relationship between higher levels of accommodation and increased symptoms and functional impairment in both pediatric and adult patients (Amir, Freshman, & Foa, 2000; Calvocoressi et al., 1999; Peris et al., 2008; Stewart et al., 2008; Storch, Larson, et al., 2010). Additionally, there is growing evidence that accommodation interferes with exposure and ritual prevention (ERP) treatment, the gold standard intervention for OCD. ERP involves asking patients to deliberately provoke obsessive fears and then to resist performing the associated compulsions. This allows patients to practice tolerating their anxious discomfort and ultimately to experience new learning regarding their feared outcomes. Both cross-sectional and longitudinal studies in adults have shown that higher levels of accommodation are related to poorer treatment outcomes (Amir et al., 2000; Merlo, Lehmkuhl, Geffken, & Storch, 2009). Finally, family members are also negatively affected by accommodation behaviors. Requests for accommodation may lead to resentment or hostility in family members (Renshaw et al., 2005). Increased levels of accommodation are related to significant amounts of family dysfunction; for example, greater accommodation is related to higher levels of depression and anxiety in family members, and to poorer general family functioning (Amir et al., 2000; Calvocoressi et al., 1999; Ramos-Cerqueira, Torres, Torresan, Negreiros, & Vitorino, 2008; Storch et al., 2009).
In order to provide families with the information and skills needed to support patients without inadvertently exacerbating their symptoms, several approaches to “family-inclusive treatments” (FITs) have been implemented in research studies. Because children present unique developmental challenges in treatment, including relatively poorer insight and motivation, most FITs have been focused on this population (e.g., Freeman et al., 2008; Piacentini et al., 2011). Parents are incorporated into treatment as a way to bolster adherence to treatment procedures and to extinguish maladaptive cycles of parental accommodation and overprotection. Despite the preponderance of FITs aimed at pediatric patients, given the previously noted evidence that OCD in adults is also associated with considerable family dysfunction and problematic levels of accommodation, several researchers have tested FITs for adult patients (Boeding et al., 2013; Grunes, Neziroglu, & McKay, 2001; Van Noppen, Steketee, McCorkle, & Pato, 1997). Although pediatric protocols almost exclusively include parents as the family member participants, FITs for adults may include spouses, siblings, or even adult children of the patients.
A recent meta-analysis examined the overall effect of FITs on OCD symptoms and on functioning. Results indicated that the effects on both outcomes were large (symptoms pooled d = 1.68; functioning pooled d = 0.98) (Thompson-Hollands, Edson, Tompson, & Comer, in press). Interestingly, although the overall extent of family involvement in treatment (i.e., whether the FIT was rated as having a high or low level of family involvement generally) did not significantly moderate the effect of FIT on symptoms or functioning, the inclusion within treatment of specific attention to reducing family accommodation behaviors did significantly moderate functioning outcomes. Those treatments that included a focus on accommodation demonstrated significantly enhanced effects on functioning relative to those treatments that did not. This suggests that the sheer amount of family involvement in treatment is not as important as identifying the most beneficial targets of that treatment. Quality may trump quantity when it comes to including family members, at least in terms of bolstering patient outcomes. A brief, adjunctive intervention, focused narrowly on an area of family behavior where modification is likely to make a substantial impact on the pathology, would therefore be of great value. To our knowledge, no such intervention has yet been tested or proposed.
To address this gap in the literature, the primary aim of the present study was to develop and test a brief family intervention (BFI) specifically targeted at reducing accommodation among the relatives of adult OCD patients. The secondary aim of the study was to determine whether having a family member participate in the BFI resulted in improved outcomes for patients relative to patients whose family members did not receive the intervention. Although the range of previously tested FITs is broad, at this time we are unaware of any previously developed intervention that is similar in brevity (2 sessions) and focus. The BFI was designed specifically for the present study based upon previous work on accommodation in family members (Freeman et al., 2008; Merlo et al., 2009). It is intended to serve as an adjunct to individual-based outpatient ERP and was tailored to complement such treatment; for example, family members are presented with standard ERP-based psychoeducation regarding the function of OCD symptoms and the rationale for exposure-based treatment. The BFI is not intended to act as a standalone treatment for OCD, and therefore only patients who were currently entering ERP treatment were enrolled in the study. The study design was constructive (Behar & Borkovec, 2003), consisting of a group of patients who received ERP alone and a group who received ERP and also had a family member participate in the BFI.
Methods
Participants
Patients were recruited from the incoming patient pools at the Center for Anxiety and Related Disorders (CARD) at Boston University and the OCD and Related Disorders Program at the Massachusetts General Hospital (MGH). The institutional review boards at both sites approved all study procedures. Recruitment flow of participants into the study can be seen in Figure 1. All patients who were seeking to begin psychological treatment at either clinic were contacted regarding this study. Study personnel telephoned patients prior to their first therapy session; the study was described to the patient and a brief screening was completed to assess initial eligibility. Patients were given the opportunity to discuss participation with their family member, and if both individuals agreed to take part in the study the baseline visit was scheduled.
Figure 1. Recruitment flow of patients into the study.
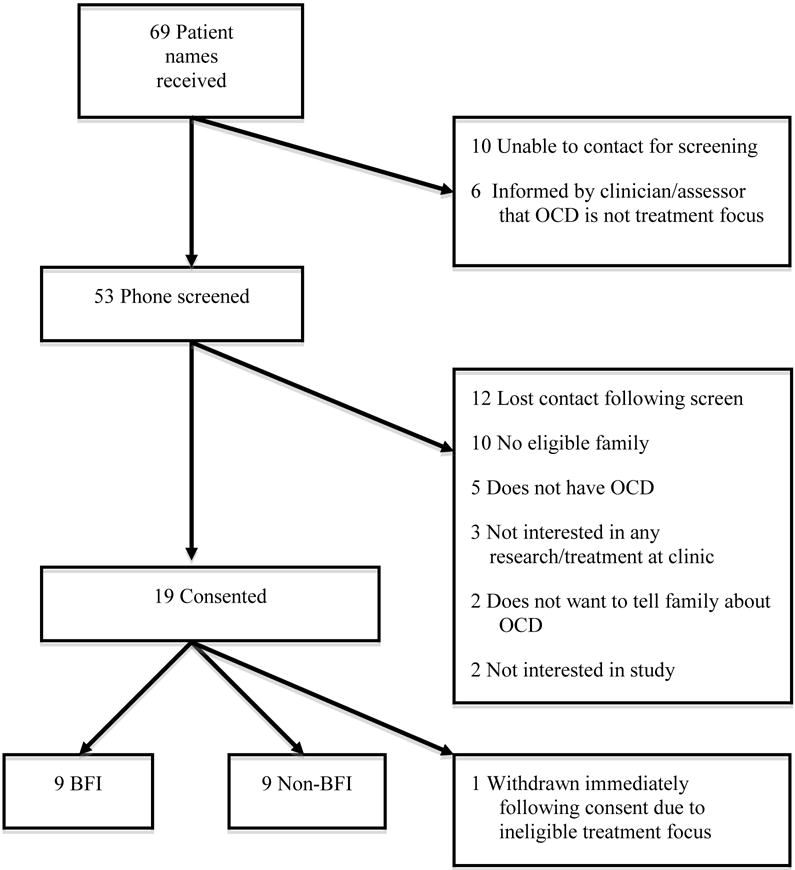
Note. BFI = brief family intervention, OCD = obsessive-compulsive disorder
The final study sample consisted of 36 adult individuals (18 patient and family member dyads). All participants gave informed consent within two weeks of the patient’s first treatment session. In order to take part in the study, OCD needed to be the primary focus of the patient’s treatment. Patients were excluded from the study if they were experiencing current suicidal or homicidal ideation, or if they had met criteria for substance abuse or dependence (excluding nicotine) in the past year. Family members (parents, siblings, spouses/significant others, or other adult relatives of the patient) were required to be living with the patient full-time in order to participate in the study, and they could not be experiencing significant OCD symptoms themselves. If multiple members of a patient’s family met these criteria, the patient was asked to select one family member with whom they had the most interactions or to whom they felt closest.
Mean age of patients was 35.44 (SD = 8.18), and mean age of family members was 41.72 (SD = 12.11). Six patients (33%) and 10 family members (56%) were male. Eleven patients (61%) were taking psychiatric medication at baseline (BFI group = 5, control group = 6). Nearly all participants across the sample were Caucasian (n = 34, 94%), two participants were Hispanic (6%; both identified as racially Caucasian), and two were Asian (6%). Median household income was $90,000–$99,000. Family members had lived with patients for an average of 11.86 (SD = 9.53) years. Relationship of family members to patients in the sample included: 13 spouses/significant others (72%), 4 parents (22%), and 1 sibling (6%).
Patients’ treatment
Patients received treatment as usual consisting of weekly outpatient ERP by highly experienced clinicians. No constraints were placed on the patients’ individual treatment, although number of sessions and any involvement of family members in the individual treatment (either in person or via telephone contact with the therapist) were tracked at each assessment point. Clinicians were not informed of the patients’ participation in the study or their randomization status, and although clinicians were not formally assessed for knowledge of whether any family member was participating in the BFI, we were not aware of any breach of blindness on the part of clinicians.
Intervention
A treatment manual for the BFI was developed for the purposes of the present study. The intervention consisted of two hour-long sessions. The first session was held at baseline (within two weeks of the patient beginning treatment), and the second session was held two weeks later. Only the individual family member attended the BFI; patients were not present. This decision was made in order to create an environment in which family members felt comfortable disclosing frustrations or other negative emotions they might be experiencing towards the patient or OCD more generally; normalizing these reactions was considered particularly important in the context of the present intervention, as we did not want family members to feel “blamed” for accommodating. By openly discussing the difficulties of navigating daily life when a family member has OCD, we presented accommodation as a common and understandable, if ultimately maladaptive, family response.
All BFI sessions were conducted by the first author. The BFI began with psychoeducation regarding the model of OCD and the rationale for ERP. The clinician then introduced the concept of accommodation and discussed the ways that the family member was currently accommodating the patient’s OCD symptoms and avoidance. The clinician explained that accommodation serves the same maladaptive function as compulsions (a short-term reduction or avoidance of distress), and engaged in problem solving with the family member about how to reduce these behaviors. They discussed how to present this change to the patient and role-played how to respond to the patient’s possible reactions. The clinician also provided handouts summarizing the information presented and suggesting alternatives to verbal reassurance for OCD concerns (e.g., “I can see this is really hard for you,” or “I just want to support all of your hard work in treatment”). The second session consisted of further troubleshooting, planning, and responding to any questions the family members had about the approach.
Measures
All participants were assessed at baseline and weeks 4, 8, 16, and 25. The following measures were administered to patients:
The Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L; DiNardo, Brown, & Barlow, 1994) or Adult version (Brown, DiNardo, & Barlow, 1994)
The ADIS is a semi-structured diagnostic clinical interview focusing on current and, in the Lifetime version, lifetime DSM-IV diagnoses of anxiety disorders and their accompanying mood states, somatoform disorders, and substance and alcohol use. The ADIS has demonstrated excellent to acceptable levels of interrater reliability (Brown, DiNardo, Lehman, & Campbell, 2001). The ADIS was administered only at baseline. ADIS raters underwent a rigorous training and certification process, requiring several shadow and collaborative interviews and the achievement of a specified number of “matching” diagnostic classifications compared to a senior interviewer (for additional information see Brown et al., 2001).
Yale-Brown Obsessive-Compulsive Scale-II (Y-BOCS-II; Storch, Rasmussen, et al., 2010)
The Y-BOCS-II is a 10-item clinician-rated scale assessing current obsessive and compulsive symptoms. The scale has shown strong internal consistency (α = .89), test-retest and interrater reliability (ICCs >.85) in a treatment-seeking sample of adults with OCD (Storch, Rasmussen, et al., 2010). Total scores ≥30 are considered “severe” (e.g., Ruscio, Stein, Chiu, & Kessler, 2010). Cronbach’s alpha for the Y-BOCS-II in the present sample was .77.
Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988)
The BAI is a widely used 21-item self-rated scale to assess a subject’s current level of anxiety symptoms. It has shown strong internal consistency (α = .92), test-retest reliability, and discriminant validity (Beck et al., 1988; Steer, Ranieri, Beck, & Clark, 1993). Cronbach’s alpha for the BAI in the patient sample was .85.
Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996)
The BDI-II is a well-established 21-item self-rated scale to assess a subject’s current level of depression symptoms. It has shown strong internal consistency (α = .91) (Steer et al., 1993), and good convergent and discriminant validity (Beck et al., 1996). Cronbach’s alpha for the BDI-II in the patient sample was .92.
Family members completed the BAI and the BDI-II, described above. Cronbach’s alpha for both scales in the family members were excellent (BAI α = .95; BDI-II α = .91) In addition family members also completed the following measures:
Family Accommodation Scale for Obsessive-Compulsive Disorder (FAS; Calvocoressi et al., 1999)
The FAS is a 12-item clinician-rated questionnaire assessing the types of accommodation behaviors that family members engage in and the associated interference. The scale has shown good internal consistency (α = .82) and good convergent and discriminant validity (Calvocoressi et al., 1999). Cronbach’s alpha for the FAS in the present sample was .80.
Obsessive-Compulsive Inventory – Revised (OCI-R; Foa et al., 2002)
The OCI-R is an 18-item self-report questionnaire assessing the presence and distress associated with dimensions of washing, checking, ordering, obsessing, hoarding, and neutralizing. Internal consistency is high (α = .89) and convergent validity is good (Abramowitz & Deacon, 2006). The recommended screening cutoff for the OCI-R is a total score of 14; this score correctly classifies 64.1% of patients with OCD (Abramowitz & Deacon, 2006). Any family members scoring higher than 14 on the OCI-R were further assessed via clinical interview to ensure that they were not experiencing a clinical level of OCD symptoms. Cronbach’s alpha for the OCI-R in the present sample was .65.
Feedback Form
This form was developed for use in the current study and consists of two portions, one completed after each session of the BFI. The ten questions relate to the acceptability and usefulness of the BFI and the family member’s confidence in being able to implement the skills. The form was accompanied by an envelope, into which family members sealed their responses. Cronbach’s alpha for the Feedback Form in the present sample was .50.
The Y-BOCS and FAS were rated by a doctoral-level psychologist with expertise in OCD who was blind to treatment condition and was not involved in any portion of patients’ treatment or family members’ BFI sessions. The timing of all assessments was not matched to patients’ treatment sessions, but rather was calculated based upon the date of study enrollment. Assessments were conducted via phone and online with the exception of the baseline assessments, which were completed in person.
Data analytic plan
The sample size for the present study (18 patient and family member dyads) was calculated based upon the study by Merlo et al. (2009), which demonstrated an effect size of f2=0.30 for the effect of change in accommodation on change in symptoms in a pediatric OCD sample. Power analyses conducted for the present study indicated that in order to perform mixed model repeated measures ANOVA tests at 80% power (alpha = .05) with a large expected effect size, a sample size of 18 patient-family member dyads is appropriate (Erdfelder, Faul, & Buchner, 1996).
A very small amount of data was missing across assessment points; for each measure, a total of 0–4 observations were missing across all participants in the study (0–2 missing observations for clinician-rated measures). Given the preliminary nature of the present study and the small sample size, the decision was made to keep the missing data as “missing” and use available data for analyses, resulting in slightly different ns per analysis.
We proposed three a priori hypotheses: (1) Participation in the BFI will be associated with a significant difference in the level of family accommodation compared to the no-intervention condition. We planned to test this hypothesis using a mixed model repeated measures ANOVA to assess for the effects of condition, time, and their interaction on FAS scores. It was expected that the effects of time and time*condition would be significant, and that post-hoc tests would reveal significant group differences in family accommodation early in patient treatment (e.g., at 4 and 8 weeks) due to the timing of the BFI delivery. (2) Family members’ participation in the BFI will be associated with greater improvement in patients’ OCD symptoms. We planned to test this hypothesis using a mixed model repeated measures ANOVA to assess for the effects of condition, time, and their interaction on Y-BOCS-II scores. It was expected that the effects of time and time*condition would be significant, Effect size calculations were also planned for both accommodation and OCD symptoms, as a further estimate of the impact of the intervention between groups. (3) Patients’ OCD symptoms would be predicted by earlier changes in levels of family accommodation, with decreases in accommodation predicting later decreases in symptoms. We planned to test this hypothesis using a multiple regression analysis, using standardized difference scores to represent changes in accommodation.
Results
Baseline severity of the sample
The Y-BOCS-II scores at baseline represented a moderate to severe degree of OCD symptoms across the patient sample (BFI = 28.78 (SD = 6.08), control = 31.89 (SD = 5.58)). Patients’ anxiety and depression severity were moderate (anxiety: BFI = 16.56 (SD = 9.63), control = 23.00 (SD = 9.14); depression: BFI = 15.67 (SD = 13.74), control = 21.67 (SD = 8.08)). There were no significant differences between patient groups on any baseline symptom measures (OCD: t(16) = 1.13, p = .28, d = .53; anxiety: t(16) = 1.46, p = .16, d = .69; depression: t(16) = 1.29, p = .28, d = .55).
Mean levels of family accommodation at baseline were moderate (BFI = 12.33 (SD = 9.57), control = 12.89 (SD = 7.51), t(16) = −.14, p = .89, d = .06). Family members’ anxiety and depression severity were low and not significantly different between groups (anxiety: BFI = 5.11 (SD = 3.26), control = 7.78 (SD = 13.19), t(16) = −.59, p = .56, d = .32; depression: BFI = 9.78 (SD = 8.15), control = 13.78 (SD = 10.95), t(16) = −.88, p = .39, d = .42).
Patient treatment
Patients completed an average of 17.79 sessions (SD = 4.54) over the 25-week study. The two patient groups did not differ in the number of sessions they completed (BFI = 16.83 (SD = 3.19), control = 18.5 (SD = 5.45), t(12) = −.66, p = .52, d = .39). Only one family member attended a treatment session with the patient; this session was solely focused on discussing more intensive treatment options for the patient, who was experiencing severe functional difficulties due to symptoms of depression. This family was in the control group. No other family members in either the control or the BFI groups reported attending a therapy session with the patient or speaking with the patient’s therapist by phone.
Family member responses to the study intervention
Family members reported high levels of satisfaction with the BFI material, as measured by the Feedback Form (mean satisfaction = 6.88/7, SD = .35). They indicated that they found practicing or discussing ways to respond to OCD behavior to be highly useful (mean = 6.29/7, SD = .76) and that they were very interested in changing the way they interact with the patient (mean = 6.67/7, SD = .50). They expressed moderate-to-high confidence in their ability to change their own behavior according to what was discussed in the BFI (mean = 5.56/7, SD = 1.13).
Changes in accommodation
Results of Mauchly’s test of sphericity indicated that the assumption of sphericity was violated (Mauchly’s W = −.272, p = .044), hence the Greenhouse-Geisser correction was used for all within-subjects tests in this analysis (Field, 2009). There was a significant main effect of time on accommodation, F(2.34, 60) = 7.98, p = .001, η2 = .35, indicating that across both groups accommodation decreased over the course of the study. There was no significant main effect of condition on accommodation F(1, 15) = 1.91, p = .19, η2 = .11, however there was a significant interaction effect of time by condition on accommodation, F(2.34, 60) = 4.32, p = .017, η2 = .22. Contrasts revealed that family members in the BFI condition experienced significantly greater reductions in accommodation from baseline than control family members at week 4 (F(1, 15) = 9.34, p = .008, d = 1.12), week 8 (F(1, 15) = 10.38, p = .006, d = 1.05), and a trend towards significance at week 16 (F(1, 15) = 4.33, p = .055, d = .69). The contrast for the interaction effect was not significant when comparing baseline accommodation versus accommodation at week 25 (F(1, 15) = 2.84, p = .113, d = .53). By week 25, family members’ average accommodation scores in the control group remained at 78% of their baseline levels, while accommodation in the BFI group had dropped to 37% of baseline. According to guidelines set forth by Jacobson and Truax (1991), 50% of family members in the BFI group exhibited reliable change in accommodation at week 25, compared to 22% of control group family members. FAS score means, standard deviations, and effect sizes between groups can be seen in Table 1, and changes in accommodation across the two groups are shown in Figure 2.
Table 1.
Changes in accommodation levels and OCD symptoms between BFI and control groups
| FAS | Y-BOCS-II | |||||
|---|---|---|---|---|---|---|
| Time | BFI | Control | d | BFI | Control | d |
| Baseline | 12.33 (9.57) | 12.89 (7.51) | .07 | 28.78 (6.08) | 31.89 (5.58) | .53 |
| Week 4 | 5.22 (5.24) | 13.00 (8.35) | 1.12** | 26.56 (5.34) | 29.56 (7.72) | .45 |
| Week 8 | 4.33 (5.87) | 13.11 (10.26) | 1.05** | 22.11 (4.86) | 28.12 (4.58) | 1.27* |
| Week 16 | 3.75 (4.68) | 10.22 (12.37) | .69 | 16.75 (4.95) | 24.25 (7.01) | 1.24* |
| Week 25 | 4.62 (8.12) | 10.11 (12.06) | .53 | 15.50 (8.12) | 22.62 (7.13) | .93 |
Note. BFI = Brief family intervention.
p<.05,
p<.01
Figure 2. Mean accommodation scores of BFI and control family members across patients’ treatment.
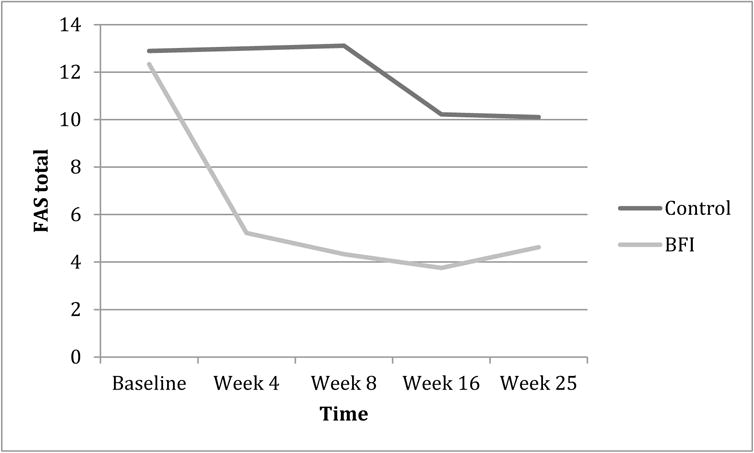
Note. BFI = brief family intervention, FAS = Family Accommodation Scale
Changes in OCD symptoms
There was a significant main effect of time on OCD symptoms, F(4, 52) = 24.49, p < .001, η2 = .65. There was no significant main effect of condition on OCD symptoms, F(1, 13) = 2.69, p = .13, η2 = .17. There was likewise no significant interaction effect of time by condition, F(1, 52) = 1.67, p = .17, η2 = .11.
Because missing data had resulted in several patients not being included in the overall mixed model ANOVA (only 15 out of 18 patients were included), independent t-tests were conducted for each post-baseline time point. Significant differences in Y-BOCS-II scores between groups were found at week 8 (t(15) = 2.62, p = .020, d = 1.27), week 16 (t(14) = 2.47, p = .028, d = 1.24), and nearly at week 25 (t(14) = 1.86, p = .08, d = .93). There was no significant difference between groups at week 4 (t(16) = .96, p = .18, d = .45). In terms of reliable change in OCD symptoms, 88% of patients in the BFI group met criteria at week 25, compared to 75% in the control group. Y-BOCS-II score means, standard deviations, and effect sizes between groups can be seen in Table 1.
Impact of accommodation change on patient symptoms
A hierarchical multiple regression analysis was conducted to evaluate the incremental predictive value of change in family accommodation scores on patients’ later Y-BOCS-II scores. Specifically, in a regression predicting week 8 Y-BOCS-II scores, baseline Y-BOCS-II scores were entered in step 1. This resulted in a significant model (β = .71, p = .001, R2 = .50), indicating that baseline Y-BOCS-II scores significantly predicted week 8 Y-BOCS-II scores. In step 2, baseline scores on the BAI and BDI were entered to account for patients’ general anxiety and distress (BAI β = −.17, p = .47; BDI β = .08, p = .76). This did not result in a significant enhancement of the model (R2 change = .02), indicating that including these variables did not improve the prediction of OCD symptoms at week 8. In the third and final step of the regression, standardized change in family accommodation from baseline to week 4 was entered (β = .45, p = .02). This step resulted in significant improvement to the model (R2 change = .19), indicating that change in family accommodation at week 4 significantly improved prediction of patients’ OCD symptoms at week 8. The final model was significant F (4, 12) = 7.42, p = .003, R2 = .71.
It would be possible that that symptom changes early in treatment drove subsequent accommodation changes, rather than the reverse. We therefore conducted a second regression analysis to examine this possibility. In this regression predicting week 8 FAS scores, baseline Y-BOCS-II scores were entered in step 1. This resulted in a nonsignificant model (β = .22, p = .38, R2 = .22). In step 2, baseline patient scores on the BAI and BDI were entered (BAI β = −.04, p = .88; BDI β = −.09, p = .78). This did not result in a significant enhancement of the model (R2 change = .009). In the third and final step of the regression, standardized change in patient’s OCD symptoms from baseline to week 4 was entered (β = .33, p = .22). This step also failed to result in significant improvement to the model (R2 change = .10). The final model was not significant F (4, 13) = .63, p = .65, R2 = .40.
Discussion
The results of this study provide preliminary support for the feasibility, acceptability, and efficacy of a brief adjunctive intervention to reduce symptom accommodation among the family members of adult patients with OCD. The BFI was highly successful in reducing family accommodation; effect sizes revealed that the impact of the intervention on accommodation was quite large, particularly so earlier in treatment. By the end of the study, family members’ average accommodation scores in the control group remained largely unchanged, while accommodation in the BFI group had dropped substantially (the small sample size likely accounts for the lack of statistical significance at this final time point, despite the relatively large group differences in accommodation). A large portion of family members in the BFI group exhibited reliable change in their levels of accommodation, with a much smaller percentage meeting such criteria in the control group. Overall, these results represent an impressive effect of the BFI on this important interpersonal variable.
We suspect that the slight reduction in accommodation seen in the control family members over the course of the study is due to reductions in OCD symptoms in the control patients. Patients in both groups improved with treatment; although our results suggest that changes in accommodation promote subsequent symptom change, we do not doubt that there is some reciprocal action in the opposite direction, with reduced OCD symptoms having some effect in reducing accommodation. It may be that as patients progressed in treatment they were more willing to challenge themselves not to ask for accommodation, and this in turn resulted in lower FAS scores compared to baseline.
We hypothesized that patients whose family members participated in the BFI would experience greater symptom reductions relative to control patients. Although the mixed-model ANOVA analysis indicated only a significant main effect of time, contrary to our hypothesis, effect sizes were large and further analyses revealed significant differences in OCD symptoms across groups. Patients whose family members had participated in the BFI had significantly lower symptoms at weeks 8 and 16, and showed a trend toward significance at week 25, although rates of reliable change were not substantially different between groups. These results are particularly compelling given that all patients in the study were receiving ERP, the “gold standard” intervention for OCD (Kobak, Greist, Jefferson, Katzelnick, & Henk, 1998), at two high-quality centers which specialize in such treatment. For a relatively brief, tailored, adjunctive intervention with family members to have such a powerful effect on the treatment outcomes of patients speaks to the importance of accommodation in the maintenance of OCD pathology.
In addition to predicting that patients in the BFI group would experience greater decreases in OCD symptoms than patients in the control group, we further expected that patients’ OCD symptoms would be predicted by earlier changes in family accommodation. In a regression analysis, patients’ OCD symptoms at week 8 were significantly predicted by family members’ change in accommodation from baseline to week 4, above and beyond the patients’ baseline OCD severity and general anxiety and depression. Change in accommodation at week 4 was found to account for 19% of the variance in OCD symptom levels at week 8. A second regression equation predicting the reverse model of causality (e.g., changes in OCD symptoms driving later accommodation scores) was not significant. This is an important finding and echoes earlier work in a pediatric sample showing that changes in accommodation temporally preceded symptom change (Piacentini et al., 2011).
There are several advantages to implementing a brief, adjunctive intervention for family members of adult patients. The results from this study show that it is possible to achieve impressive effects with only a few sessions, provided those sessions are thoughtfully targeted. Furthermore, asking family members to participate in one or two sessions is much less burdensome than requiring a fully couple- or family-based treatment. During recruitment for the present study, no patient who initially agreed to participate in the study had a family member refuse to take part. Although it is impossible to say what refusal rates may have been given a longer intervention, family members did express satisfaction with the length of the BFI and rarely indicated that there were other topics they wished to have included. Finally, the intervention in the present study draws upon clinicians’ existing individual CBT skills, rather than requiring them to achieve competency in couple or family therapy. True family therapy is a comprehensive intervention approach with unique treatment targets and therapist demands (Dattilio, 2013; Epstein & Baucom, 2002). It has an important place in the landscape of empirically supported treatments, yet the majority of CBT clinicians do not have the expertise to deliver this type of treatment. The BFI that was tested in the present study has the advantages of being highly behaviorally focused in nature and delivered in an individual format. It excellently complements individual ERP for OCD and does not require extensive development of new competencies on the part of the clinician.
Nonetheless, there are potential difficulties in widely implementing a family-inclusive treatment, particularly for adult OCD patients. Studies consistently report low marriage rates in treatment-seeking OCD populations (Koran, 2000; Lensi et al., 1996; Steketee, 1993). Although this speaks to the potentially isolating nature of the disorder, studies have also shown that close to one quarter of adult OCD patients still live with their parents (Steketee & Pruyn, 1998). In a sample of highly severe adult patients entering residential treatment, 75% reported living with at least one first-degree relative (spouse, parent, sibling, or child) (Stewart et al., 2008), providing other possible avenues for family-inclusive treatment. Notably, 81% of the patients screened for the present study lived with an adult family member, and the present sample included spouses, siblings, and parents of adult children within the family member participants. Previous work has found no association between levels of accommodation and whether the relative in question is the spouse or parent of the patient (Calvocoressi et al., 1999).
There are several limitations to the present study that offer directions for future research. First, the individual treatment provided to the patients in the study (both ERP and any psychiatric medication) was uncontrolled. Although this clearly diminishes our ability to determine what portion of the observed differences in patients’ outcomes across the two groups is attributable to family members’ participation in the BFI versus other treatment effects, it remains that all patients received first-line ERP and medication use was approximately equal across groups. Second, the sample size of the present study was small. Although we were adequately powered to assess our main outcomes based on previous research, it is possible that the small number of participants masked potentially significant differences between the two groups. Furthermore, the small sample size prevented us from conducting moderator analyses to examine the possible effect of particular patient or family characteristics, such as the quality or nature (spouse versus parent/sibling) of the relationship. Regarding the issue of relationship quality, past research has indicated that marital satisfaction does not negatively impact response to ERP in OCD (Riggs, Hiss, & Foa, 1992); nonetheless, we were unable to fully explore this question in the present study. Third, it has been suggested that the use of standardized difference scores in a regression analysis may introduce a spurious effect by virtue of the relationship between the endpoint value and the dependent variable (in this case, accommodation at week 4 and OCD symptoms at week 8). Fourth, we did not conduct formal treatment adherence assessments of either patients’ treatment or family members’ BFI sessions. Although all clinicians at both sites are well-trained in ERP techniques and routinely implement exposure-based treatment with their patients, and both clinics specialize in the administration of ERP patients with OCD, we cannot conclusively demonstrate that strict ERP procedures were followed. Regarding the BFI sessions, this intervention is novel and was developed for the purpose of the present study. The BFI was piloted in three families prior to its use in this sample. A treatment manual was developed to structure the intervention and all sessions were conducted by the treatment developer and first author. While these steps considerably diminished the possibility that the therapist may have drifted from the protocol, external adherence measures were not collected, limiting to some degree our ability to speak to the integrity of the treatment. Finally, there was limited anonymity in the collection of the Feedback Form from family members, which may have resulted in biased responses regarding treatment satisfaction.
Given the encouraging results of this small RCT combined with its various limitations, a larger, more well-controlled trial is clearly needed to replicate and extend these findings, as well as to explore mechanisms and moderators of the effects. In addition to further evaluations within OCD, it is also possible that the BFI could be productively applied in other emotional disorders such as anxiety and mood disorders, post-traumatic stress disorder, and others. These disorders are known to share many characteristics and may in fact represent variations on a single “general neurotic syndrome” (Barlow, Sauer-Zavala, Carl, Bullis, & Ellard, 2014; Brown & Barlow, 2009). A treatment explicitly targeting the core underlying commonalities across these diagnoses, the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (Barlow et al., 2011), has now been developed and shown early promise (Ellard, Fairholme, Boisseau, Farchione, & Barlow, 2010; Farchione et al., 2012). Although accommodation across the emotional disorders has only recently begun to be studied (Lebowitz et al., 2013; (Thompson-Hollands, Kerns, Pincus, & Comer, under review), given our knowledge of the importance of interpersonal relationships in psychopathology it is likely that an intervention targeting the relevant processes could have similar effects in other disorders.
Acknowledgments
Disclosure statement: This research was supported by a fellowship from the National Institutes of Mental Health to the first author (JTH) under award number F31MH092996. The content reported here is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Financial support for the present study was also provided to JTH from the Association of Behavioral and Cognitive Therapies.
References
- Abramowitz JS, Deacon BJ. Psychometric properties and construct validity of the Obsessive–Compulsive Inventory—Revised: Replication and extension with a clinical sample. Journal of Anxiety Disorders. 2006;20(8):1016–1035. doi: 10.1016/j.janxdis.2006.03.001. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Publishing, Inc; 2013. [Google Scholar]
- Amir N, Freshman M, Foa EB. Family distress and involvement in relatives of obsessive-compulsive disorder patients. Journal of Anxiety Disorders. 2000;14(3):209–217. doi: 10.1016/S0887-6185(99)00032-8. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, Ehrenreich-May J. The unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. New York: Oxford University Press; 2011. [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, Ellard KK. The Nature, Diagnosis, and Treatment of Neuroticism Back to the Future. Clinical Psychological Science. 2014;2(3):344–365. doi: 10.1177/2167702613505532. [DOI] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Behar ES, Borkovec TD. Handbook of Psychology. John Wiley & Sons, Inc; 2003. Psychotherapy Outcome Research. [Google Scholar]
- Boeding SE, Paprocki CM, Baucom DH, Abramowitz JS, Wheaton MG, Fabricant LE, Fischer MS. Let me check that for you: symptom accommodation in romantic partners of adults with Obsessive-Compulsive Disorder. Behaviour Research and Therapy. 2013;51(6):316–322. doi: 10.1016/j.brat.2013.03.002. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: Implications for assessment and treatment. Psychological Assessment. 2009;21:256–271. doi: 10.1037/a0016608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, DiNardo PA, Barlow DH. Anxiety disorders interview schedule for DSM-IV: Treatment follow-up version (Adult-ADIS-IV) New York: Oxford University Press; 1994. [Google Scholar]
- Brown TA, DiNardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disordrs: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Calvocoressi L, Mazure C, Stanislav K, Skolnick J, Fisk D, Vegso S, Price LH. Family accommodation of obsessive-compulsive symptoms: Instrument development and assessment of family behavior. Journal of Nervous and Mental Disease. 1999;187(10):636–642. doi: 10.1097/00005053-199910000-00008. [DOI] [PubMed] [Google Scholar]
- Caporino N, Morgan J, Beckstead J, Phares V, Murphy T, Storch EA. A structural equation analysis of family accommodation in pediatric obsessive-compulsive disorder. Journal of Abnormal Child Psychology. 2012;40(1):133–143. doi: 10.1007/s10802-011-9549-8. [DOI] [PubMed] [Google Scholar]
- Dattilio FM. Cognitive-behavioral therapy with couples and families: A comprehensive guide for clinicians. New York: The Guilford Press; 2013. [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety disoders interview schedule for DSM-IV: Lifetime version (ADIS-IV-L) New York: Oxford University Press; 1994. [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, Barlow DH. Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cognitive and Behavioral Practice. 2010;17(1):88–101. doi: 10.1016/j.cbpra.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein NB, Baucom DH. Enhanced cognitive-behavioral therapy for couples: A contextual approach. Washington D.C.: American Psychological Association; 2002. [Google Scholar]
- Erdfelder E, Faul F, Buchner A. GPOWER: A general power analysis program. Behavior Research Methods, Instruments, and Computers. 1996;28:1–11. [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, Barlow DH. Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behavior Therapy. 2012;43(3):666–678. doi: 10.1016/j.beth.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field A. Discovering statistics using SPSS. 3rd. Thousand Oaks, CA: SAGE Publications Inc; 2009. [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, Salkovskis PM. The obsessive-compulsive inventory: Development and validation of a short version. Psychological Assessment. 2002;14(4):485–496. doi: 10.1037/1040-3590.14.4.485. [DOI] [PubMed] [Google Scholar]
- Freeman JB, Garcia AM, Coyne A, Przeworski A, Himle M, Compton S, Leonard HL. Early childhood OCD: Preliminary findings from a family-based cognitive-behavioral approach. 2008 May; doi: 10.1097/CHI.0b013e31816765f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunes MS, Neziroglu F, McKay D. Family involvement in the behavioral treatment of obsessive-compulsive disorder: A preliminary investigation. Behavior Therapy. 2001;32(4):803–820. doi: 10.1016/S0005-7894(01)80022-8. [DOI] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037/0022-006X.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kobak KA, Greist JH, Jefferson JW, Katzelnick DJ, Henk HJ. Behavioral versus pharmacological treatments of obsessive compulsive disorder: A meta-analysis. Psychopharmacology. 1998;136:205–216. doi: 10.1007/s002130050558. [DOI] [PubMed] [Google Scholar]
- Koran LM. Quality of life in obsessive-compulsive disorder. Psychiatric Clinics of North America. 2000;23:509–517. doi: 10.1016/s0193-953x(05)70177-5. [DOI] [PubMed] [Google Scholar]
- Lebowitz ER, Panza KE, Su J, Bloch MH. Family accommodation in obsessive–compulsive disorder. Expert Review of Neurotherapeutics. 2012;12(2):229–238. doi: 10.1586/ern.11.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz ER, Woolston J, Bar-Haim Y, Calvocoressi L, Dauser C, Warnick E, Leckman JF. Family accommodation in pediatric anxiety disorders. Depression and Anxiety. 2013;30(1):47–54. doi: 10.1002/da.21998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lensi P, Cassano GB, Correddu G, Ravagli S, Kunovac JL, Akiskal HS. Obsessive-compulsive disorder: Familial-developmental history, symptomology, comorbidity and course with special reference to gender-related differences. British Journal of Psychiatry. 1996;169:101–107. doi: 10.1192/bjp.169.1.101. [DOI] [PubMed] [Google Scholar]
- Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA. Decreased family accommodation associated with improved therapy outcome in pediatric obsessive–compulsive disorder. Journal of Consulting and Clinical Psychology. 2009;77(2):355–360. doi: 10.1037/a0012652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders. Clinical Psychology Review. 2007;27:572–581. doi: 10.1016/j.cpr.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J. Correlates of accommodation of pediatric obsessive-compulsive disorder: Parent, child, and family characteristics. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:1173–1181. doi: 10.1097/CHI.0b013e3181825a91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piacentini J, Bergman RL, Chang S, Langley A, Peris T, Wood JJ, McCracken J. Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(11):1149–1161. doi: 10.1016/j.jaac.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos-Cerqueira AT, de A, Torres AR, Torresan RC, Negreiros APM, Vitorino CN. Emotional burden in caregivers of patients with obsessive-compulsive disorder. Depression and Anxiety. 2008;25(12):1020–1027. doi: 10.1002/da.20431. [DOI] [PubMed] [Google Scholar]
- Renshaw KD, Steketee G, Chambless DL. Involving family members in the treatment of OCD. Cognitive Behaviour Therapy. 2005;34(3):164–175. doi: 10.1080/16506070510043732. [DOI] [PubMed] [Google Scholar]
- Riggs DS, Hiss H, Foa EB. Marital distress and the treatment of obsessive compulsive disorder. Behavior Therapy. 1992;23(4):585–597. doi: 10.1016/S0005-7894(05)80223-0. [DOI] [Google Scholar]
- Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Molecular Psychiatry. 2010;15:53–63. doi: 10.1038/mp.2008.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steer RA, Ranieri WF, Beck AT, Clark DA. Further evidence for the validity of the beck anxiety inventory with psychiatric outpatients. Journal of Anxiety Disorders. 1993;7(3):195–205. doi: 10.1016/0887-6185(93)90002-3. [DOI] [Google Scholar]
- Steketee G. Social support and treatment outcome of obsessive-compulsive disorder at 9-month follow-up. Behavioural Psychotherapy. 1993;21:81–95. [Google Scholar]
- Steketee G, Pruyn NA. Families of individuals with obsessive-compulsive disorder. In: Swinson RP, Antony MM, Rachman S, Richter MA, editors. Obsessive-compulsive disorder: Theory, research, and treatment. New York: Guilford Press; 1998. pp. 120–140. [Google Scholar]
- Stewart SE, Beresin C, Haddad S, Stack DE, Fama J, Jenike M. Predictors of family accommodation in obsessive-compulsive disorder. Annals of Clinical Psychiatry. 2008;20:65–70. doi: 10.1080/10401230802017043. [DOI] [PubMed] [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ, Jacob ML, Murphy TK, Goodman WK, Grabill K. Family accommodation in pediatric obsessive–compulsive disorder. Journal of Clinical Child & Adolescent Psychology. 2007;36(2):207–216. doi: 10.1080/15374410701277929. [DOI] [PubMed] [Google Scholar]
- Storch EA, Larson MJ, Muroff J, Caporino N, Geller D, Reid JM, Murphy TK. Predictors of functional impairment in pediatric obsessive-compulsive disorder. Journal of Anxiety Disorders. 2010;24(2):275–283. doi: 10.1016/j.janxdis.2009.12.004. [DOI] [PubMed] [Google Scholar]
- Storch EA, Lehmkuhl H, Pence S, Geffken G, Ricketts E, Storch J, Murphy T. Parental experiences of having a child with obsessive-compulsive disorder: Associations with clinical characteristics and caregiver adjustment. Journal of Child & Family Studies. 2009;18(3):249–258. doi: 10.1007/s10826-008-9225-y. [DOI] [Google Scholar]
- Storch EA, Rasmussen SA, Price LH, Larson MJ, Murphy TK, Goodman WK. Development and psychometric evaluation of the Yale–Brown Obsessive-Compulsive Scale—Second Edition. Psychological Assessment. 2010;22(2):223–232. doi: 10.1037/a0018492. [DOI] [PubMed] [Google Scholar]
- Thompson-Hollands J, Edson A, Tompson MC, Comer JS. Family involvement in the psychological treatment of obsessive-compulsive disorder: A meta-analysis. Journal of Family Psychology. doi: 10.1037/a0036709. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson-Hollands J, Kerns CE, Pincus DB, Comer JS. Parental accommodation of child anxiety and related symptoms: Range, impact, and correlates. doi: 10.1016/j.janxdis.2014.09.007. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Noppen B, Steketee G. Testing a conceptual model of patient and family predictors of obsessive compulsive disorder (OCD) symptoms. Behaviour Research and Therapy. 2009;47(1):18–25. doi: 10.1016/j.brat.2008.10.005. [DOI] [PubMed] [Google Scholar]
- Van Noppen B, Steketee G, McCorkle BH, Pato M. Group and multifamily behavioral treatment for obsessive compulsive disorder: A pilot study. Journal of Anxiety Disorders. 1997;11(4):431–446. doi: 10.1016/S0887-6185(97)00021-2. [DOI] [PubMed] [Google Scholar]


