Abstract
Background
Gay and bisexual men (GBM) are at elevated risk for gonorrhea and chlamydia trachomatis (GC/CT). Rectal GC/CT symptoms may be less obvious than urethral, increasing opportunities for undiagnosed rectal GC/CT.
Method
A U.S. national sample of 1,071 GBM completed urethral and rectal GC/CT testing and an online survey.
Results
In total, 6.2% were GC/CT positive (5.3% rectal, 1.7% urethral). We calculated adjusted (for education, race, age, relationship status, having health insurance, and income) odds ratios for factors associated with rectal and urethral GC/CT diagnoses. Age was inversely associated with urethral and rectal GC/CT. Compared to White men, Latinos had significantly greater odds of rectal GC/CT. Among men who reported anal sex, those reporting only insertive sex had lower odds of rectal GC/CT than men who reported both insertive and receptive. There was a positive association between rectal GC/CT and number of male partners (<12 months), the number of anal receptive acts, receptive condomless anal sex (CAS) acts, and insertive CAS acts.
Compared to those who had engaged in both insertive and receptive anal sex, those who engaged in only receptive anal sex had lower odds of urethral GC/CT. The number of male partners (<12 months) was associated with increased odds of urethral GC/CT.
Conclusion
Rectal GC/CT was more common than urethral and associated with some demographic and behavioral characteristics. Our finding that insertive CAS acts was associated with rectal GC/CT highlights that providers should screen patients for GC/CT via a full range of transmission routes, lest GC/CT go undiagnosed.
Keywords: men who have sex with men, gonorrhea, chlamydia, gay and bisexual men
Introduction
Gay, bisexual, and other men who have sex with men (GBMSM) represent 4–15% of the U.S. population(1, 2) and are disproportionally affected by sexually transmitted infections, including Neisseria gonorrhoeae (GC) and Chlamydia trachomatis (CT)(3, 4). In 2013, in the U.S. STD surveillance network—comprised of 42 STD clinics within 12 collaborating jurisdictions—GC prevalence was 16.9% (range by site: 10.4%–28.1%) and CT prevalence was 15.2% (range by site: 7.4%–30.7%) among GBMSM(4). Across collaborating jurisdictions, 27.4% of GC cases were estimated to be among GBMSM, 30.5% among men who have sex with women, and 42.1% among women—comparable data on CT were not reported.
Testing for GC and CT has historically been conducted with culture, however, Nucleic Acid Amplification Tests (NAAT) (e.g., the Abbott Real-Time, Aptima COMBO 2 assay, cobas® 4800) are now cleared by the U.S. Food and Drug Administration as the standard diagnostic tests for their increased sensitivity, specificity, and ease of specimen transport(5). The most common methods by which GC and CT are tested are through the collection of urine. Urine-based screening allows for self-collection(6) with minimal sample collection barriers compared to urethral specimens that need to be collected in a clinic setting(7). Patients provide a first-catch urine specimen that is transferred to a test specific transport tube. Fewer studies have examined the prevalence of rectal GC and CT, which is typically identified via a swab of the rectum and culture. NAATs are not FDA cleared for rectal specimens, limiting their accessibility to patients and providers(8). Patients self-swab the inside of the rectum and break off the swab into a test specific transport tube. Self-sampling has been compared to clinic-based testing finding high viability and acceptability with a variety of populations including MSM(6, 9). Although GBMSM do not engage in anal sex every time they have sex(10), there remains a need to test for urethral as well as rectal GC/CT given that many GBMSM do engage in insertive as well as receptive anal sex(11, 12). Studies of GBMSM who engage in anal sex have found that rates of engaging in receptive as well as insertive anal sex (i.e., versatility) ranged from moderate (e.g., 38%(13)) to high (e.g., 73%(14), 83%(15)). Certainly, routine STI screening is contingent upon engaging in sex without a condom, or sex with multiple partners; however, data on rates of receptive and versatile sex among GBMSM suggest that a significant portion should be routinely screened for urethral as well as rectal STIs.
As a result of the continuing HIV and STI epidemics, much of researchers’ attention to GBMSM has been grounded in HIV prevention. And, much of what we know about GBMSM has been based on samples in urban epicenters. As a result, less is known about U.S. GBMSM who live outside of urban centers. Although CDC surveillance data is helpful with identifying incident HIV and STIs, much of these data are limited to urban centers and/or collected at STD clinics (i.e., self-selected samples of individuals who perceive themselves to need, or are referred for, STI testing). Furthermore, surveillance data is restricted in that it provides little context as to social and behavioral factors that are associated with STI diagnoses.
With the expanded use of the Internet both by researchers as well as GBMSM, engaging geographically diverse samples of GBMSM in research has become and increasingly acceptable method of data collection(16–20). Recently, researchers have begun combining online data collection with self-administered biological data collection, particularly for HIV among GBMSM(21, 22). Less is known about the use of at-home self-administered testing for STIs among GBMSM; however studies suggest it is feasible and acceptable(9, 23). To that end, the present study reports on rates of urethral and rectal GC/CT diagnosis in a U.S. national sample of HIV-negative GBM, as well as factors associated with urethral and rectal diagnosis.
Method
Participants and Procedures
The One Thousand Strong panel is a longitudinal study following a U.S. national sample of gay and bisexual men (GBM) for a period of three years(24). Analyses for the present manuscript were based on baseline data. Participants were identified via Community Marketing and Initiatives (CMI) panel of over 45,000 LGBT individuals, over 22,000 of whom are GBM throughout the United States. CMI draws panelists from over 200 sources ranging from LGBT events to social media and non-gay identified venues/mediums (e.g., social media). Participants in the One Thousand Strong panel were targeted to represent the diversity and distribution of GBM in the U.S. population. In so doing, recruitment targets were established using data from the U.S. Census with regard to same sex households and racial and ethnic composition.
CMI emailed potential participants with a brief description of the study along with a link to a brief 2-minute survey that would determine preliminary eligibility criteria (e.g., reside in the U.S., be at least 18 years of age, be biologically male and currently identify as male, identify as gay or bisexual, report having sex with a man in the past year, self-identify as HIV-negative, willing to complete at-home self-administered rapid HIV antibody testing, willing to complete self-administered testing for urine and rectal GC/CT, able to complete assessments in English, have access to the Internet such to complete at-home online assessments, have access to a device that was capable of taking a digital photo (e.g., camera phone, digital camera), have an address to receive mail that was not a P.O. Box, and were residentially stable (i.e., have not moved more than twice in the past 6 months)). Those meeting these preliminary criteria were invited to join the study and presented with informed consent. Those consenting had their contact information shared with the research team to follow up for enrollment in the study. The research team emailed participants a link to a secure online survey that took approximately one-hour to complete. Participants were mailed a kit for self-collection of urine and rectal GC/CT specimens as well as at-home OraQuick© HIV testing. Because the rapid HIV-antibody test must be read between 20 and 40 minutes following collection, participants used their digital device to take a picture of the test paddle and sent that to the research team as confirmation of HIV-negative serostatus. There were 11 men who tested HIV-positive at baseline and these men were not enrolled in the study. The research team contacted these 11 men to facilitate confirmatory testing and treatment. Urine and rectal samples were returned mail to the lab at Emory University for analysis. Participants were compensated $25 for completing the first hour-long at-home survey and an additional $25 for HIV/STI testing procedures.
Participants were enrolled between April 2014-October 2014. The City University of New York (CUNY) Institutional Review Board approved study procedures.
Measures
STI testing
GC/CT were tested using the Abbott m2000 Real-Time assay. Specimens are collected using the Abbott multi-Collect Specimen Collection Kit and can be stored for up to 14 days. This NAAT assay uses a polymerase chain reaction (PCR) testing approach where DNA is extracted. The method of detection has a sensitivity of 95.2% for CT/98.7% for GC and a specificity of 99.3% for CT/99.2% for GC, thus the chances of a false positive and false negative are low(5). If CT and GC are present, their sequences are amplified and detected with fluorescent-labeled oligonucleotide probes(25). To validate the rectal swabs, double rectal swabs were obtained from Emory Medical Labs and each was analyzed both straight and inoculated with CT and GC DNA. The rectal samples inoculated with CT and GC did not show any inhibition. Internal controls are run alongside each test sample to ensure no inhibition. During the enrollment process, there were 26 participants not enrolled in the panel because they failed to complete the STI testing procedures and an additional 7 men whose samples resulted in inconclusive results. Attempts to resample these men were unsuccessful. Meanwhile, among the 1071 enrolled in the panel, only 2.8% (n = 30) experienced an STI sampling error (e.g., fecal contamination of the rectal swab, urine vial improperly sealed and came open in the biohazard bag during transit to the lab, rectal swab inserted into the vial containing urine) and < 1% (n = 8) had to be resent a kit because it was reported as lost in the mail—either not received by participant or not received by lab after reportedly being mailed. Our attempts to resample these 30 participants were successful. In the event of a positive STI result, participants were telephoned to discuss the results and to facilitate getting treatment.
Demographic and behavioral characteristics
Participants reported demographic characteristics including race/ethnicity, education, income, age, sexual identity, whether they had used illegal drugs (cocaine, methamphetamine, ecstasy/MDMA, GHB/GBL, heroin/opiates, ketamine, crack) in the prior 3 months, and whether they had health insurance and a primary doctor. Participants also reported their sexual behavior including the number of times they engaged in receptive and/or insertive condomless anal sex (CAS) with an HIV-positive or unknown status main partner or any casual male partners in the prior 3 months.
Analytic Plan
We first describe the prevalence of rectal and urine GC/CT as well as demographic and behavioral characteristics of the sample. As appropriate, we next report unadjusted and adjusted odds ratios for the association between demographic and behavioral characteristics with testing positive for rectal or urethral CG/CT. Adjusted odds ratios accounted for the effects of education, race, age, relationship status, having health insurance, and income. Finally, using Mann-Whitney U tests, which account for the non-normal distribution of count variables, we reported bivariate associations between various sexual behaviors (e.g., number of anal insertive acts, number of receptive anal sex acts) and diagnosis with rectal or urethral GC/CT.
Results
Figure 1 indicates the distribution of participants across the US. Participants represented 49 of 50 states. Table 1 presents descriptive characteristics of the One Thousand Strong panel. In total, 95% were self-identified as gay, 29% were men of color, and the average age was average age of 40.2. Nearly half (48.7%) were in a relationship, 91.8% reported having health insurance, 76.0% reported having a primary care provider, and 10.8% reported drug use in the prior 3 months. With regard to sexual behavior, 39.2% reported having engaged in CAS with a casual male partner or with an HIV-positive or HIV-unknown main partner in the prior 3 months. Nearly half (49.8%) said they had not engaged in any anal sex in the past 3 months, 12.3% reported only acts of anal receptive sex, 20% reported both insertive and receptive anal sex (versatile), and 17.6% reported only anal insertive sex.
Figure 1.
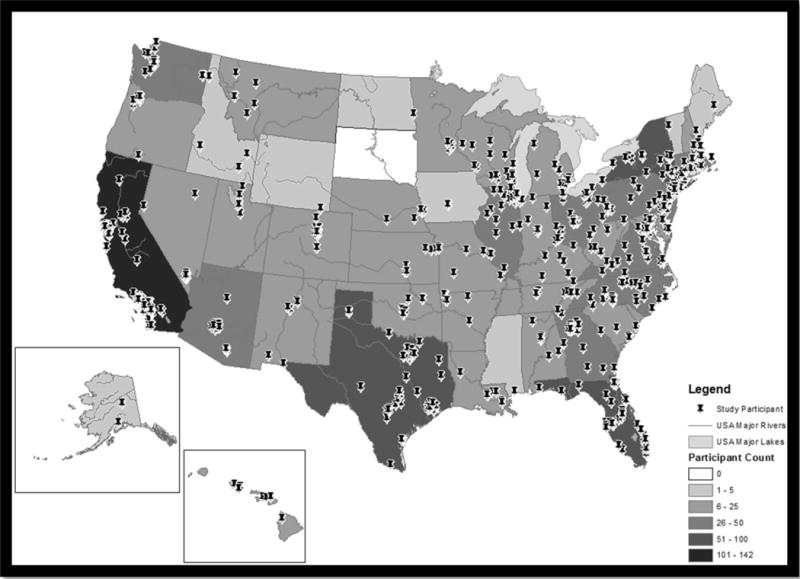
Distribution of One Thousand Strong participants across the United States
Table 1.
Demographic characteristics, N = 1071
| n | % | |
|---|---|---|
| Rectal or urethral GC and/or CT (i.e., any STI diagnosis) | 66 | 6.2 |
| Rectal CG and/or CT | 57 | 5.3 |
| Rectal GC | 19 | 1.8 |
| Rectal CT | 47 | 4.4 |
| Urethral GC and/or CT | 18 | 1.7 |
| Urethral GC | 5 | 0.5 |
| Urethral CT | 15 | 1.4 |
| Income | ||
| < $50,000 | 575 | 53.7 |
| $50,000 + | 496 | 46.3 |
| Sexual identity | ||
| Gay | 1017 | 95.0 |
| Bisexual | 54 | 5.0 |
| Has a 4-year college degree | ||
| No | 474 | 44.3 |
| Yes | 597 | 55.7 |
| Relationship status | ||
| Single | 549 | 51.3 |
| In a relationship | 522 | 48.7 |
| Race and Ethnicity | ||
| Black | 83 | 7.7 |
| Latino | 135 | 12.6 |
| White | 763 | 71.2 |
| Multiracial or “other” | 90 | 8.4 |
| Has health insurance | ||
| Yes | 983 | 91.8 |
| No | 88 | 8.2 |
| Has a primary care provider | 814 | 76.0 |
| Any drug use,1 < 3 months | 107 | 10.8 |
| Anal sexual behavior with casual male partners, < 3 months | ||
| No anal sex | 533 | 49.8 |
| Exclusive bottom | 132 | 12.3 |
| Versatile | 217 | 20.3 |
| Exclusive top | 189 | 17.6 |
| CAS2 with a casual male partner or HIV-positive or HIV-unknown main partner, < 3 months | 420 | 39.2 |
CT Chlamydia trachomatis, GC Neisseria gonorrhoeae
Cocaine, methamphetamine, ecstasy/MDMA, GHB/GBL, heroin/opiates, ketamine, crack
Condomless anal sex
In total, 6.2% tested positive for rectal or urethral GC/CT. Rectal STIs were more common than urethral (5.3% vs. 1.7%), and CT was more common than GC (5.3% vs. 1.8%). Nine men (0.8%) were diagnosed with both rectal and urethral STIs, 9 men (0.8%) with just a urethral STI, and 48 men (4.6%) with just a rectal STI.
Table 2 reports unadjusted and adjusted odds ratios for factors associated with rectal GC/CT diagnosis. Several bivariate associations were no longer significant after adjusting for the effects of other variables. These included income, relationship status, and drug use in the prior 3 months. Compared to White men, Latino men had significantly greater odds of having a rectal STI. Among men who reported anal sex, those reporting only insertive anal sex had significantly lower odds of being diagnosed with a rectal STI than men who reported both insertive and receptive sex. Recent CAS was associated with rectal STIs. There was a negative association between age and rectal GC/CT. There was a positive association between rectal GC/CT and the number of male partners in the past 12 months, the number of anal receptive acts, receptive CAS acts, and insertive CAS acts.
Table 2.
Demographic and behavioral characteristics associated with rectal GC/CT diagnosis
| Rectal GC and/or CT | Odds Ratio | 95% CI | Adj. Odds Ratio a | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|
| No | Yes | |||||||
| n | % | n | % | |||||
|
|
||||||||
| Income | ||||||||
| < $50,000 | 536 | 52.9 | 39 | 68.4 | 0.52 | 0.29 – 0.92 | 0.79 | 0.41 – 1.50 |
| $50,000 + | 478 | 47.1 | 18 | 31.6 | ||||
| Has a 4-year college degree | ||||||||
| No | 444 | 43.8 | 30 | 52.6 | 0.70 | 0.41 – 1.20 | 0.87 | 0.49 – 1.53 |
| Yes | 570 | 56.2 | 27 | 47.4 | ||||
| Relationship status | ||||||||
| Single | 512 | 50.5 | 37 | 64.9 | 0.55 | 0.32 – 0.96 | 0.62 | 0.35 – 1.09 |
| In a relationship | 502 | 49.5 | 20 | 35.1 | ||||
| Race and ethnicity | ||||||||
| White (Ref.) | 729 | 71.9 | 34 | 59.6 | Ref. | -- - -- | Ref. | -- - -- |
| Black | 79 | 7.8 | 4 | 7.0 | 1.09 | 0.38 – 3.14 | 0.96 | 0.56 – 1.64 |
| Latino | 121 | 11.9 | 14 | 24.6 | 2.48 | 1.29 – 4.76 | 2.01 | 1.02 – 3.97 |
| Multiracial or “other” | 85 | 8.4 | 5 | 8.8 | 1.26 | 0.48 – 3.31 | 1.00 | 0.37 – 2.70 |
| Has health insurance | ||||||||
| No | 85 | 8.4 | 8 | 14.0 | 0.56 | 0.26 – 1.22 | 0.73 | 0.33 – 1.64 |
| Yes | 929 | 91.6 | 49 | 86.0 | ||||
| Has a primary care providers | ||||||||
| Yes | 774 | 76.3 | 40 | 70.2 | 1.37 | 0.76 – 2.46 | 0.90 | 0.47 – 1.72 |
| No | 240 | 23.7 | 17 | 29.8 | ||||
| Any drug use,1 < 3 months | ||||||||
| No | 841 | 89.8 | 42 | 79.2 | 2.29 | 1.14 – 4.61 | 1.89 | 0.93 – 3.85 |
| Yes | 96 | 10.2 | 11 | 20.8 | ||||
| Anal sexual behavior with casual male partners, < 3 months, excluding men who did not report anal sex with a casual male partner, valid n = 538 | ||||||||
| Exclusive bottom | 122 | 24.7 | 10 | 22.7 | 0.49 | 0.23 – 1.04 | 0.48 | 0.22 – 1.03 |
| Versatile (Ref.) | 186 | 37.7 | 31 | 70.5 | Ref. | -- - -- | Ref. | -- - -- |
| Exclusive top | 186 | 37.7 | 3 | 6.8 | 0.10 | 0.03 – 0.32 | 0.11 | 0.03 – 0.36 |
| CAS2 with a casual male partner or HIV-positive or HIV-unknown main partner, < 3 months | ||||||||
| No | 633 | 62.4 | 18 | 31.6 | 3.60 | 2.03 – 6.38 | 3.26 | 1.82 – 5.83 |
| Yes | 381 | 37.6 | 39 | 68.4 | ||||
| M | SD | M | SD | t | p | Adj. Odds Ratio a | ||
|
|
||||||||
| Age in years | 40.6 | 13.8 | 34.4 | 13.8 | 3.29 | < .001 | 0.97 | 0.95 – 0.99 |
| Mdn | IQR | Mdn | IQR | U | p | |||
|
|
||||||||
| Male partners in the last 12 months | 4 | 1–10 | 8.0 | 5–15 | 39448.0 | < .001 | 1.02 | 1.01 – 1.03 |
| Sexual behavior with casual male partners in the last 3 months, valid n = 1071 | ||||||||
| Number of anal insertive acts | 0 | 0–2 | 2 | 0–7.5 | 36719.0 | < .001 | 1.01 | 0.993 – 1.04 |
| Number of anal receptive acts | 0 | 0–1 | 2 | 0–7 | 42140.0 | < .001 | 1.03 | 1.01 – 1.06 |
| Number of condomless anal insertive acts | 0 | 0–0 | 1 | 0–3 | 36891.0 | < .001 | 1.06 | 1.02 – 1.10 |
| Number of condomless anal receptive acts | 0 | 0–0 | 1 | 0–3 | 40033.0 | < .001 | 1.04 | 1.01 – 1.08 |
M Mean, SD Standard Deviation, Mdn Median, IQR Interquartile Range, U Mann-Whitney U CT Chlamydia trachomatis, GC Neisseria gonorrhoeae
Adjusted for education, race, age, relationship status, having health insurance, and income Bold items are significant at p < .05
Cocaine, methamphetamine, ecstasy/MDMA, GHB/GBL, heroin/opiates, ketamine, crack
Condomless anal sex
Table 3 reports unadjusted and adjusted odds ratios for factors associated with urethral GC/CT diagnosis. Age was inversely associated with urethral GC/CT diagnosis. No other demographic characteristics were associated with urethral GC/CT diagnosis. However some behavioral characteristics were. Adjusting for the effects of education, race, age, relationship status, having health insurance, and income, compared to those who said they had engaged in both insertive and receptive anal sex, those who said they engaged in only receptive anal sex had significantly lower odds of testing positive for urethral GC/CT. In addition, the number of male partners in the past 12 months was associated with increased odds of urethral GC/CT diagnosis. Interestingly, the number of insertive and receptive anal sex acts with and without a condom were all positively associated with testing positive for urethral GC/CT (at the bivariate level); however, these effects did not hold up after accounting for the effects of education, race, age, relationship status, having health insurance, or income.
Table 3.
Demographic and behavioral characteristics associated with urethral GC/CT diagnosis
| Urethral GC and/or CT | Odds Ratio | 95% CI | Adj. Odds Ratio a | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|
| No | Yes | |||||||
| n | % | n | % | |||||
|
|
||||||||
| Income | ||||||||
| < $50,000 | 562 | 53.4 | 13 | 72.2 | 0.44 | 0.16 – 1.24 | 0.98 | 0.30 – 3.20 |
| $50,000 + | 491 | 46.6 | 5 | 27.8 | ||||
| Has a 4-year college degree | ||||||||
| No | 462 | 43.9 | 12 | 66.7 | 0.39 | 0.15 – 1.05 | 0.47 | 0.17 – 1.34 |
| Yes | 591 | 56.1 | 6 | 33.3 | ||||
| Relationship status | ||||||||
| Single | 540 | 51.3 | 9 | 50 | 1.05 | 0.42 – 2.67 | 1.26 | 0.49 – 3.27 |
| In a relationship | 513 | 48.7 | 9 | 50 | ||||
| Race and ethnicity | ||||||||
| White (Ref.) | 750 | 71.2 | 13 | 72.2 | Ref. | -- - -- | Ref. | -- - -- |
| Black | 81 | 7.7 | 2 | 11.1 | 1.42 | 0.32 – 6.41 | 1.09 | 0.51 – 2.35 |
| Latino | 133 | 12.6 | 2 | 11.1 | 0.87 | 0.19 – 3.89 | 0.49 | 0.11 – 2.25 |
| Multiracial or “other” | 89 | 8.5 | 1 | 5.6 | 0.65 | 0.08 – 5.01 | 0.48 | 0.06 – 3.77 |
| Has health insurance | ||||||||
| No | 90 | 8.5 | 3 | 16.7 | 0.47 | 0.13 – 1.65 | 0.62 | 0.17 – 2.27 |
| Yes | 936 | 91.5 | 15 | 83.3 | ||||
| Has a primary care providers | ||||||||
| Yes | 803 | 76.3 | 11 | 61.1 | 2.04 | 0.78 – 5.33 | 1.24 | 0.43 – 3.57 |
| No | 250 | 23.7 | 7 | 38.9 | ||||
| Any drug use,1 < 3 months | ||||||||
| No | 869 | 89.3 | 14 | 82.4 | 1.79 | 0.51 – 6.33 | 1.37 | 0.37 – 4.95 |
| Yes | 104 | 10.7 | 3 | 17.6 | ||||
| Anal sexual behavior with casual male partners, < 3 months, excluding men who did not report anal sex with a casual male partner, valid n = 538 | ||||||||
| Exclusive bottom | 131 | 25 | 1 | 7.1 | 0.16 | 0.02 – 1.25 | 0.12 | 0.01 – 0.95 |
| Versatile (Ref.) | 207 | 39.5 | 10 | 71.4 | Ref. | -- - -- | Ref. | -- - -- |
| Exclusive top | 186 | 35.5 | 3 | 21.4 | 0.33 | 0.09 – 1.23 | 0.36 | 0.09 – 1.38 |
| CAS2 with a casual male partner or HIV-positive or HIV-unknown main partner, < 3 months | ||||||||
| No | 647 | 61.4 | 4 | 22.2 | 5.58 | 1.82 – 17.06 | 5.55 | 1.78 – 17.29 |
| Yes | 406 | 38.6 | 14 | 77.8 | ||||
| M | SD | M | SD | t | p | Adj. Odds Ratio a | ||
|
|
||||||||
| Age in years | 40.4 | 13.8 | 31.0 | 10.7 | 2.87 | 0.004 | 0.94 | 0.90 – 0.99 |
| Mdn | IQR | Mdn | IQR | U | p | |||
|
|
||||||||
| Male partners in the last 12 months | 4.0 | 1–10 | 10.5 | 4–20 | 13121.0 | 0.01 | 1.03 | 1.01 – 1.05 |
| Sexual behavior with casual male partners in the last 3 months, valid n = 1071 | ||||||||
| Number of anal insertive acts | 0 | 0–2 | 4.0 | 0–7.5 | 13220.0 | 0.001 | 1.02 | 0.99 – 1.06 |
| Number of anal receptive acts | 0 | 0–1 | 1.0 | 0–7.75 | 12637.0 | 0.004 | 1.03 | 1.00 – 1.06 |
| Number of condomless anal insertive acts | 0 | 0–0 | 1.0 | 0–4.25 | 13894.0 | < .001 | 1.07 | 1.00 – 1.14 |
| Number of condomless anal receptive acts | 0 | 0–0 | 0.0 | 0–4.5 | 11625.0 | 0.02 | 1.03 | 0.99 – 1.06 |
M Mean, SD Standard Deviation, Mdn Median, IQR Interquartile Range, U Mann-Whitney U CT Chlamydia trachomatis, GC Neisseria gonorrhoeae
Adjusted for education, race, age, relationship status, having health insurance, and income Bold items are significant at p < .05
Cocaine, methamphetamine, ecstasy/MDMA, GHB/GBL, heroin/opiates, ketamine, crack
Condomless anal sex
Discussion
Participants completed at-home self-administered STI sample collection and mailed those to a lab for analyses with minimal errors, suggesting high feasibility and acceptability for incorporating at-home self-administered STI sample collection into studies that would otherwise be entirely online. In this study 6.2% tested positive for rectal or urethral GC/CT with rectal STIs being more common than urethral (5.3% vs. 1.7%), and CT was more common than GC (5.3% vs. 1.8%). Our rates of new diagnoses were lower than CDC surveillance; however, it is worth noting the intrinsic differences between surveillance data and our sample. Surveillance data are collected via STD clinics, and those attending clinics are likely doing so because they are experiencing symptoms of an infection. Our sample also excluded HIV-positive men, who are included in surveillance data.
Positive STI results are behaviorally driven and infection location is indicative of sexual acts performed. We believe the discrepancy between urethral and rectal GC/CT might be a combined result of multiple variables operating at different levels of the sexual health care continuum(26–28). These include an individual’s own failure to recognize the symptoms of rectal STI infection (which can include discharge or be asymptomatic)(29) relative to the more pronounced symptoms of urethral infection, and thus a patients’ failure to seek out testing/treatment. Second, there may be lower acceptability—by providers and by patients—of the method by which samples for rectal STI are collected (e.g., a medical provider inserting a swab into the rectum vs. self-collection through routine urination). Third, both patients and providers may have discomfort around discussing sexual behavior and sexual health, particularly anal sexual health, or disclosing that they engaged in condomless anal sex. Fourth, a failure on behalf of medical providers to suggest/provide rectal STI testing to their GBM patients as a part of his routine medical care as well as a failure on behalf of patients to request it. Fifth, there may be insurance coverage gaps whereby routine testing for urethral STIs is covered but rectal STIs is not. Sixth, some individuals may believe that routine urine collection or blood work by their physician also tested then for rectal STIs. Our study did not assess frequency of STI testing nor methods of STI testing (e.g., urethral and rectal) thus cannot comment as to the extent that higher rates of rectal STIs are a factor of one of the aforementioned hypotheses. In addition, we did not collect data on perceived STI symptoms (e.g., pain, discharge), which would have been useful for the present study.
In our study, STI diagnoses appeared to be more so a factor of behavioral as opposed to demographic characteristics. That is, and perhaps unsurprising, men who reported a history of CAS were more likely to also be diagnosed with GC/CT, and there was a positive association between number of male partners in the prior 12 months and GC/CT diagnoses. Although it may seem counterintuitive that, for example, receptive CAS acts were associated with urethral CT/GC, we highlight that receptive CAS was positively correlated with insertive CAS.
Limitations
Although we used parameters taken from the Census to establish recruitment targets (e.g., geographic distribution of same-sex male couples, age, race and ethnicity), this was based on data on same-sex households (i.e., couples). The Census does not collect data on sexual identity or sexual behavior, thus the true prevalence/distribution of GBM across the U.S. remains unknown. It is possible to weight our data to correct for deviation in our sample (with regard to characteristics such as race and ethnicity, geographic diversity, and age), but this requires for the population characteristics to be known. Certainly other datasets could also be used for post hoc sample weights (e.g., CDC surveillance data); however, we also highlight that adding sample weights to match our dataset to CDC surveillance data simply corrects for our sample to match another sample, not to a population.
We tested only for GC/CT, but not other STIs such as genital warts, genital herpes, or syphilis. These STIs are detected via blood draw, which would not have been feasible for the present study. Further, we did not assess for pharyngeal infections.
By partnering with CMI to enroll members from their LGBT panel, we were able to engage a population that is already attuned to participating in web-based studies. This ensures participants are familiar with, for example, how to complete a survey online as well as how to use a computer. Individuals who do not know how to use a computer or do not have Internet access would not be eligible to be a CMI panelist and thus would not be represented in this present study. This bias toward a more technologically savvy population should be noted.
Conclusions
The One Thousand Strong panel is prospectively following 1,071 HIV-negative GBM from across the United States. In addition to online components, we were able to engage the panel in self-administered at-home STI testing and only a small proportion of potential participants failed to complete these procedures. This suggests that there is high feasibility and acceptability in incorporating self-administered STI testing into research studies that would be otherwise fully online. Rectal GC/CT was more common than urethral and associated with some demographic and behavioral characteristics. Our finding that insertive CAS acts was associated with rectal GC/CT highlights the importance for providers to screen patients for GC/CT via a full range of transmission routes, lest GC/CT go undiagnosed. Because as much as 14.6% of HIV infections among GBMSM may be attributable to GC/CT co-infection(30), testing and treating GC/CT may dually serve to reduce HIV incidence within this population.
Acknowledgments
The One Thousand Strong study was funded by NIH/NIDA (R01 DA 036466: Jeffrey T. Parsons & Christian Grov). H. Jonathon Rendina was funded by a Career Development Award from NIH/NIDA (K01-DA039030). We would like to acknowledge other members of the One Thousand Strong Study Team (Dr. Tyrel Starks, Michael Castro, Ruben Jimenez, Dr. Jonathan Lassiter, Brett Millar, Chloe Mirzayi, Raymond Moody, and Anita Viswanath) and other staff from the Center for HIV/AIDS Educational Studies and Training (Qurrat-Ul Ain, Andrew Cortopassi, Chris Hietikko, Doug Keeler, Chris Murphy, Carlos Ponton, and Brian Salfas). We would also like to thank the staff at Community Marketing Inc (David Paisley, Thomas Roth, and Heather Torch) and Dr. Patrick Sullivan, Jessica Ingersoll, Deborah Abdul-Ali, and Doris Igwe at the Emory Center for AIDS Research (P30 AI050409). Finally, special thanks to Dr. Jeffrey Schulden at NIDA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest: None
References
- 1.Purcell DW, Johnson CH, Lansky A, et al. Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. Open AIDS Journal. 2012;6(1):98–107. doi: 10.2174/1874613601206010098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Milrod C, Monto MA. The hobbyist and the girlfriend experience: Behaviors and preferences of male customers of internet sexual service providers. Deviant Behavior. 2012;33(10):792–810. [Google Scholar]
- 3.Kirkcaldy RD, Zaidi A, Hook EW, et al. Neisseria gonorrhoeae antimicrobial resistance among men who have sex with men and men who have sex exclusively with women: the Gonococcal Isolate Surveillance Project, 2005–2010. Annals of Internal Medicine. 2013;158(5_Part_1):321–8. doi: 10.7326/0003-4819-158-5-201303050-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CDC. 2014 Pages. Accessed at http://www.cdc.gov/std/stats13/surv2013-print.pdf. Accessed September 17 2015.
- 5.CDC. Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae–2014. MMWR Recomm Report. 2014;14(63 (RR-02)):1–19. [PMC free article] [PubMed] [Google Scholar]
- 6.Lunny C, Taylor D, Hoang L, et al. Self-collected versus clinician-collected sampling for Chlamydia and Gonorrhea screening: a systemic review and meta-analysis. PloS One. 2015;10(7):e0132776. doi: 10.1371/journal.pone.0132776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kohl KS, Markowitz LE, Koumans EH. Developments in the screening for Chlamydia trachomatis: a review. Obstetrics and Gynecology Clinics of North America. 2003;30(4):637–58. doi: 10.1016/s0889-8545(03)00076-7. [DOI] [PubMed] [Google Scholar]
- 8.Gunn RA, O’Brien CJ, Lee MA, Gilchick RA. Gonorrhea screening among men who have sex with men: value of multiple anatomic site testing, San Diego, California, 1997–2003. Sex Transm Dis. 2008;35(10):845–8. doi: 10.1097/OLQ.0b013e318177ec70. [DOI] [PubMed] [Google Scholar]
- 9.Wayal S, Llewellyn C, Smith H, et al. Self-sampling for oropharyngeal and rectal specimens to screen for sexually transmitted infections: acceptability among men who have sex with men. Sex Transm Infect. 2009;85(1):60–4. doi: 10.1136/sti.2008.032193. [DOI] [PubMed] [Google Scholar]
- 10.Rosenberger JG, Reece M, Schick V, et al. Sexual behaviors and situational characteristics of most recent male-partnered sexual event among gay and bisexually identified men in the United States. Journal of Sexual Medicine. 2011;8:3040–50. doi: 10.1111/j.1743-6109.2011.02438.x. [DOI] [PubMed] [Google Scholar]
- 11.Peinado J, Goodreau SM, Goicochea P, et al. Role versatility among men who have sex with men in urban Peru. Journal of Sex Research. 2007;44(3):233–9. doi: 10.1080/00224490701443676. [DOI] [PubMed] [Google Scholar]
- 12.Moskowitz DA, Rieger G, Roloff ME. Tops, bottoms and versatiles. Sexual and Relationship Therapy. 2008;23(3):191–202. [Google Scholar]
- 13.Grov C, Saleh LD, Lassiter JM, Parsons JT. Challenging race-based stereotypes about gay and bisexual men’s sexual behavior, and perceived penis size and size satisfaction. Sexuality Research and Social Policy. 2015;12(3):224–35. [Google Scholar]
- 14.Grov C, Rendina HJ, Ventuneac A, Parsons JT. HIV risk in group sexual encounters: an event-level analysis from an online survey of MSM in the U.S. Journal of Sexual Medicine. 2013;10:2285–94. doi: 10.1111/jsm.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lyons A, Pitts M, Smith G, et al. Versatility and HIV vulnerability: investigating the proportion of Australian gay men having both insertive and receptive anal intercourse. Journal of Sexual Medicine. 2011;8(8):2164–71. doi: 10.1111/j.1743-6109.2010.02197.x. [DOI] [PubMed] [Google Scholar]
- 16.Grov C, Breslow AS, Newcomb ME, Rosenberger JG, Bauermeister JA. Gay and bisexual men’s use of the Internet: Research from the 1990s through 2013. Annual Review of Sex Research. 2014;51(4):390–409. doi: 10.1080/00224499.2013.871626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bauermeister JA, Pingel E, Zimmerman M, Couper M, Carballo-Dieguez A, Strecher VJ. Data quality in HIV/AIDS web-based surveys: Handling invalid and suspicious data. Field Methods. 2012;24(3):272–91. doi: 10.1177/1525822X12443097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Teitcher JEF, Bockting WO, Bauermeister JA, Hoefer CJ, Miner MH, Klitzman RL. Detecting, preventing, and responding to “fraudsters” in Internet research: ethics and tradeoffs. The Journal of Law, Medicine & Ethics. 2015;43(1):116–33. doi: 10.1111/jlme.12200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chiasson MA, Parsons JT, Tesoriero JM, Carballo-Dieguez A, Hirshfield S, Remien RH. HIV behavioral research online. Journal of Urban Health. 2006;83(1):73–85. doi: 10.1007/s11524-005-9008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sullivan PS, Khosropour CM, Luisi N, et al. Bias in online recruitment and retention of racial and ethnic minority men who have sex with men. J Med Internet Res. 2011;13(2):e38. doi: 10.2196/jmir.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khosropour CM, Sullivan PS. At-home HIV testing of MSM enroleld in an online HIV behavioral risk study. National HIV Prevention Conference; Atlanta. 2011. [Google Scholar]
- 22.Khosropour CM, Johnson BA, Ricca AV, Sullivan PS. Enhancing retention of an Internet-based cohort study of men who have sex with men (MSM) via text messaging: randomized controlled trial. Journal of Medical Internet Research. 2013;15(8):e194. doi: 10.2196/jmir.2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mustanski B, Madkins K, Parsons JT, Sullivan PS. Rectal and urethral STIs among young MSM: Prevalence, demographic and behavioral risk factors, and implications for HIV risk. American Public Health Association; Chicago: 2015. [Google Scholar]
- 24.Grov C, Cain D, Whitfield THF, et al. Recruiting a U.S. national sample of HIV-negative gay and bisexual men to complete at-home self-administered HIV/STI testing and surveys: Challenges and opportunities. Sexuality Research & Social Policy. doi: 10.1007/s13178-015-0212-y. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abbott Laboratories. 2010 Pages. Accessed at https://www.abbottmolecular.com/static/cms_workspace/pdfs/US/CTNG_8L07-91_US_FINAL.pdf. Accessed October 1 2015.
- 26.Dodge B, Van Der Pol B, Rosenberger JG, et al. Field collection of rectal samples for sexually transmitted infection diagnostics among men who have sex with men. International Journal of STD & AIDS. 2010;21(4):260–4. doi: 10.1258/ijsa.2009.009056. [DOI] [PubMed] [Google Scholar]
- 27.Hoover KW, Butler M, Workowski K, et al. STD screening of HIV-infected MSM in HIV clinics. Sexually Transmitted Diseases. 2010;37(12):771–6. doi: 10.1097/OLQ.0b013e3181e50058. [DOI] [PubMed] [Google Scholar]
- 28.Ryder N, Bourne C, Rohrsheim R. Clinical audit: adherence to sexually transmitted infection screening guidelines for men who have sex with men. International Journal of STD & AIDS. 2005;16(6):446–9. doi: 10.1258/0956462054093980. [DOI] [PubMed] [Google Scholar]
- 29.Whitlow CB. Bacterial sexually transmitted diseases. Clinics in Colon and Rectal Surgery. 2004;17(4):209. doi: 10.1055/s-2004-836940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beck EC, Birkett M, Armbruster B, Mustanski B. A data-driven simulation of HIV spread among young men who have sex with men: role of age and race mixing and STIs. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2015;70(2):186–94. doi: 10.1097/QAI.0000000000000733. [DOI] [PMC free article] [PubMed] [Google Scholar]


