Abstract
Sarcoidosis is a common disease that involve almost constantly the lung. Usually the onset is insidious, and symptoms are slowly ingravescent. Very rarely, as in the case here reported, sarcoidosis can cause an acute respiratory failure with acute respiratory distress syndrome (ARDS). A 20-year-old girl from Pakistan presented for acute fatigue, fever, and cough with a chest X-ray displayed the micronodular interstitial disease. Despite of anti-tuberculosis therapy, ARDS developed in a few days requiring continuous positive airway pressure treatment. Examinations on transbronchial specimens obtained by bronchoscopy permitted to reach the diagnosis of sarcoidosis and steroid therapy improved rapidly clinical conditions. This is the first case report reported in Europe that confirms the rare onset of sarcoidosis as ARDS. Steroid therapy allows to cure rapidly this severe complication.
Key words: Acute respiratory distress syndrome, acute respiratory failure, sarcoidosis
Sarcoidosis is a nonnecrotizing granulomatous disease of unknown etiology. It is present world-wide and can appear at any age with a peak in the 20-40 year age group. It occurs about twice as often in women where it usually takes a more aggressive course. This disorder can involve different organs, more frequently it is localized in mediastinal lymph nodes, lung, skin, liver, and eyes, but it can afflict also the heart, central nervous system, spleen, bone, joint, muscles, nose, and paranasal sinuses. Diagnosis is established finding noncaseating epithelioid-cell granulomas in the absence of organisms in a specimen obtained from involved tissue. Symptomatic patients are treated with steroids, generally with a good clinical response. Pulmonary sarcoidosis often has an insidious onset, more common symptoms are dyspnea, dry cough, chest discomfort, and sometimes, wheezing.[1] Chest radiography is a simple, very helpful examination for a first evaluation of the patient. Chest X-ray display allows to classify this disease in five stages. Stage 0: No evidence of sarcoidosis; Stage 1: Hilar/mediastinal adenoapthies; Stage 2: Adenopathies and lung parenchymal abnormalities, Stage 3: Only parenchymal abnormalities; Stage 4: Pulmonary fibrosis. Chest computed tomography (CT) is certainly more sensitive, and it is performed to evaluate in detail lymphadenopathies and lung disease. Pulmonary parenchyma can be involved by nodules, consolidations, reticular opacities, honeycombing and also bronchial abnormalities.[2]
We present a case of acute worsening of lung function with acute respiratory distress syndrome (ARDS) due to sarcoidosis. To our knowledge, there are a very few cases in the literature describing an acute and severe presentation of sarcoidosis.
Case Report
A 20-year-old girl, born in Pakistan and living in Italy for 8 years, presented to the emergency room for fatigue, fever, and dry cough, lasting for 1 week. The medical history of the patient revealed coeliac disease. She was never-smoker. On physical examination, the patient was cachectic without any other pathological findings, in particular, no superficial lymphoadenopathies were appreciable. Blood examination showed leukocytosis (15,240/mmc), microcytic anaemia (hemoglobin [Hb] 10.4 g/dL), thrombocytosis (593,000/mmc), increased levels of C-reactive protein and erythrocyte sedimentation rate. Chest X-ray [Figure 1] displayed micronodular interstitial disease, with diffuse interstitial-alveolar infiltrates. In the suspect of miliary tuberculosis (TB), the patient was admitted to the Division of Infectious Diseases and it was started immediately anti-TB therapy: Rifampin, isoniazid, ethambutol, and pyrazinamide, firstly intravenous and then per os. Blood exams were repeated and showed normal leukocytes count with a slight monocytosis (12%) and confirmed microcytic iron deficiency anemia (Hb: 9.3 g/dL, ferritin: 7 ng/mL, iron: 25 mcg/dL) and thrombocytosis (485,000/mmc). Moreover, other laboratory tests confirmed cachexia (low levels of triglycerides, cholesterol, albumin, and creatine kinase).
Figure 1.
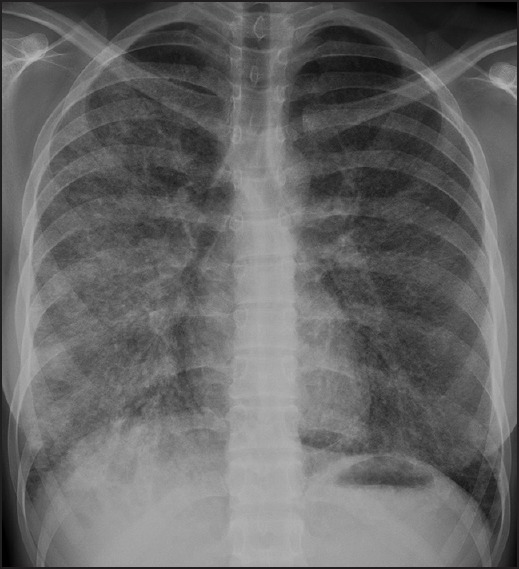
Chest X-ray (posteroanterior view) shows bilateral diffuse micronodular infiltrates
Despite the prompt beginning of antitubercular therapy, the clinical condition worsened day by day. Persistent fever was present and after 5 days since admission, respiratory failure developed requiring oxygen-therapy. Blood culture for Gram-positive and negative bacteria resulted negative.
To clarify the involvement of the lung, it was performed a bronchoscopy with bronchial washing. The evaluation at the microscope on this specimen resulted negative for mycobacterium. Furthermore also QuantiFERON-TB resulted negative. Chest CT [Figure 2] displayed lung hilar and mediastinal lymphadenopathies (up to 3 cm) associated to diffuse parenchymal opacities (ground glass) and small nodules. The radiological features were not typical for miliar TB, but could be an expression of other diseases, such as lymphoproliferative disorders.
Figure 2.
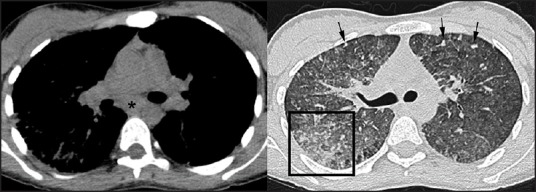
Computed tomography images demonstrate subcarinal adenopathy (asterisk) and diffuse ground-glass opacities with small nodules (arrows) which tend to be confluent in some areas of the lung (box)
Fifteen days after the admission, patient's clinical condition worsened further with respiratory failure, hypotension, and tachycardia, and she was moved to the Intensive Care Unit. Despite the continuous positive airway pressure (CPAP) with inspiratory oxygen fraction 80% applied, PaO2 was lower than 50 mmHg. Clinical and echocardiographic parameters required to make a diagnosis of ARDS were satisfied. Intravenous therapies with methylprednisolone 20 mg twice a day and levofloxacin 500 mg twice a day were started. Bronchoscopy was repeated one more time performing bronchoalveolar lavage (BAL) and transbronchial biopsies (TBBs).
After the onset of the therapy, respiratory and cardiovascular parameters improved abruptly. CPAP treatment was discontinued the day after, dyspnea got better progressively. On serological examinations human immunodeficiency virus-test and lymphocyte typing were negative. Instead angiotensin conversion enzyme and lactic dehydrogenase were slightly increased. These results and the clinical response to steroid therapy suggested sarcoidosis.
This diagnosis was confirmed by BAL fluid examination which revealed lymphocytic alveolitis with CD4/CD8 ratio 1.2 and TBB was positive for nonnecrotizing granulomas consistent with sarcoidosis [Figure 3]. Antitubercular therapy and levofloxacin were stopped, and methylprednisolone was continued.
Figure 3.
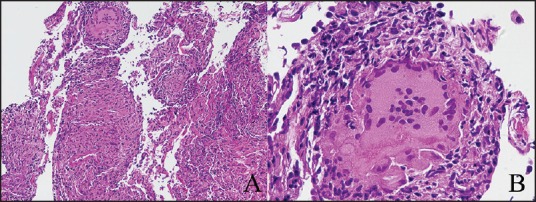
Transbronchial biopsy (TBB) showing granulomas. H and E, assay ×100 (a), ×200 (b). TBB was mainly characterized by the presence of nonnecrotizing granulomas. Other inflammatory cells were poorly represented, mainly lymphocytes around granulomas. Alveolar septa were overshadowed by granulomatous component. Some central necrosis (b) revealing very active sarcoidosis can be identified. Special stains for fungi (PAS) and mycobacteria resulted negative. Images courtesy of Tironi Andrea MD, Division of Anatomic Pathology, Spedali Civili, Brescia.
After 6 days, the patient was discharged from the Intensive Care Unit in good clinical condition and without oxygen support. A chest X-ray of control showed a reduction of the lung infiltrates bilaterally.
The patient was finally discharged with a diagnosis of ARDS in pulmonary sarcoidosis (Stage II) and the prescription of prednisone 25 mg a day.
The patient was followed in our interstitial lung diseases surgery. Chest X-ray and CT scan, performed 6 and 16 months after the discharge respectively, demonstrated almost complete regression of lymphadenopathies and pulmonary abnormalities [Figure 4]. During this period also the symptoms progressively improved, and steroid therapy (prednisone) could be tapered to a dose of 5 mg once a day.
Figure 4.
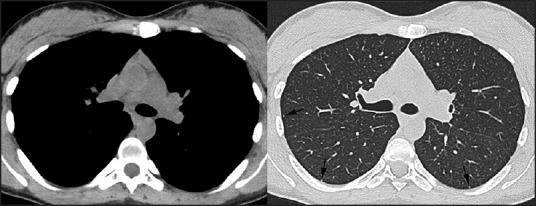
Computed tomography images show complete resolution of lymphadenopathies and ground-glass opacities; only a few small nodules are detected (arrows)
Discussion
In this case report, an extremely rare presentation of a very common disease has been reported. Indeed, in English language medical literature only 7 previous cases of sarcoidosis causing respiratory failure can be found[3,4,5,6,7,8,9] and this is the first one in Europe. In our experience patient's conditions progressively worsened, developing respiratory failure with ARDS and requiring intensive treatment with CPAP. Improvement of clinical condition was obtained introducing methylprednisolone before detecting the underlying disease, allowing the performance of a bronchoscopy with TBB and the establishment of the diagnosis.
These cases remind us that, even though very rarely, sarcoidosis can present acutely and can be life-threatening for the patient if not rapidly treated. Then, when we cannot detect an infection or any other diseases that can cause ARDS, it is important to think also of sarcoidosis. Starting rapidly steroid-therapy even before pathological confirmation is essential because, even though patient's condition is very serious, it should improve rapidly.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors thank Tironi Andrea, MD, for his important advice and his contributes. The authors thank Tantucci Claudio, PhD for his revision.
References
- 1.Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357:2153–65. doi: 10.1056/NEJMra071714. [DOI] [PubMed] [Google Scholar]
- 2.Little BP. Sarcoidosis: Overview of pulmonary manifestations and imaging. Semin Roentgenol. 2015;50:52–64. doi: 10.1053/j.ro.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Essop AR, Moosa MR, Ally R. Atypical pulmonary sarcoidosis. A case report. S Afr Med J. 1984;66:71–4. [PubMed] [Google Scholar]
- 4.Suyama T, Satoh H, Inoue T, Noguti Y, Ohtsuka M, Yosizawa Y, et al. A case of sarcoidosis presenting with high fever and acute respiratory failure. Kekkaku. 1990;65:811–9. [PubMed] [Google Scholar]
- 5.Sabbagh F, Gibbs C, Efferen LS. Pulmonary sarcoidosis and the acute respiratory distress syndrome (ARDS) Thorax. 2002;57:655–6. doi: 10.1136/thorax.57.7.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chirakalwasan N, Dallal MM. Pulmonary sarcoidosis presenting with acute respiratory failure. South Med J. 2005;98:382–4. doi: 10.1097/01.SMJ.0000154317.31912.E1. [DOI] [PubMed] [Google Scholar]
- 7.Shibata S, Saito K, Ishiwata N, Ieki R. A case of sarcoidosis presenting with high fever and rash progressing to acute respiratory failure. Nihon Kokyuki Gakkai Zasshi. 2007;45:691–7. [PubMed] [Google Scholar]
- 8.Gupta D, Agarwal R, Paul AS, Joshi K. Acute hypoxemic respiratory failure in sarcoidosis: A case report and literature review. Respir Care. 2011;56:1849–52. doi: 10.4187/respcare.01174. [DOI] [PubMed] [Google Scholar]
- 9.Gera K, Gupta N, Ahuja A, Shah A. Acute alveolar sarcoidosis presenting with hypoxaemic respiratory failure. BMJ Case Rep. 2014 doi: 10.1136/bcr-2013-202247. doi:10.1136/bcr-2013-202247. [DOI] [PMC free article] [PubMed] [Google Scholar]


