Abstract
Cryptosporidium parvum is an intracellular spore-forming protozoa which predominantly causes intestinal diseases. It causes severe and life-threatening diarrheal diseases in immunocompromised hosts and usually self-limiting disease in immunocompetent hosts. Extra-intestinal manifestations of cryptosporidium infection are very rare. Herein, we report a case of pulmonary cryptosporidiosis in a 35-yrs-old immunocompetent host, who presented with fever, cough and breathlessness which was soon followed by diarrhea and vomiting, had lung consolidation, and treated successfully with nitazoxanide.
KEY WORDS: Cryptosporidium, HIV, immunocompetent, nitazoxanide, oocysts
INTRODUCTION
Cryptosporidium parvum is an intracellular spore forming protozoan. It primarily infects epithelial cells of small intestinal and responsible for major cause of diarrheal disease in both immunocompetent as well as immunocompromised individuals. The cryptosporidium diarrheal disease in immunocompetent individual is usually of short duration and self limiting. It causes severe and life-threatening diarrheal disease in immunocompromised individuals mainly in those suffering from HIV/AIDS.[1] Extra-intestinal cryptosporidium disease has been reported in patient with AIDS.[2,3] Acalculous cholecystitis or papillary stenosis, pancreatitis, lung, and middle ear infection have been found in the literature.[4]
Pulmonary disease is a rare extra-intestinal manifestation of cryptosporidium infection and its presence in an immunocompetent host makes it further rarer. Herein, we report a case of pulmonary cryptosporidiosis in an immunocompetent host, which was soon followed by intestinal disease symptoms, treated successfully with nitazoxanide.
CASE REPORT
A 35-year-old non-alcoholic rural male presented with 5-days history of intermittent fever with chills, cough with expectoration and breathlessness. After admission patient had history of four episodes of profuse watery diarrhea associated with nausea and one episode of watery vomiting. There was no history of hemoptysis, blood in stool, and weight loss. He had a history of farming before hospitalization. He was not suffering from any chronic illness and had no addiction to any drugs.
On examination, the patient was febrile, conscious, cooperative, and well-oriented. His blood pressure was 110/80 mm of Hg, pulse rate 106 beats/min regular, respiratory rate 22 breaths/min, temperature 38.2°C by axilla and oxygen saturation on room air was 98%. On chest auscultation crepitations were found on right lower zone. Other systemic examinations were normal. Routine blood investigations were sent before he was put on intravenous fluid and antibiotics. Laboratory investigations revealed hemoglobin of 13.8 g/dL, total leukocyte count 13,000/mm3 with 80% neutrophils, 17% lymphocytes, 2% monocytes and 165000/mm3 platelets. The blood sugar was 94 mg/dL, blood urea 35 mg/dL, S. creatinine 1.0 mg/dL, AST 25 IU/L, ALT 20 IU/L, S.LDH 230 IU/L and total protein was 6.9 g/dL with 4.3 g/dL albumin. Serum immunoglobulin's IgG, IgA, IgM and CD4-T cell count were within normal range. He was tested non-reactive for HIV 1 and 2 and negative for malaria parasite test. Mantoux skin test was also negative.
Sputum samples were examined for the presence of bacteria, fungus, mycobacterium and nocardia with Grams staining, Ziehl-Neelsen (ZN) staining, and modified acid-fast stains (kinyon stain). Sputum culture was done for these organisms according to their specific culture media. Microscopic examination of sputum smear stained with ZN and modified ZN staining showed of 4-6 μ, circular and acid-fast structures [Figure 1]. These structures were identified as oocysts of cryptosporidium parvum. Modified ZN staining of stool smear also showed a lot of cryptosporidium oocysts [Figure 2]. The presence of acid-fast structures of cryptosporidium oocysts were confirmed on repeat modified ZN staining of sputum and stool sample after 2 days. No pathogenic bacteria including mycobacterium tuberculosis were grown in culture. Blood and urine culture were sterile for any pathogenic bacteria. Chest X-ray PA view revealed right lower zone consolidation [Figure 3b]. After conformation of cryptosporidium infection, he was treated with nitazoxanide for 3 days. He became asymptomatic with complete resolution of opacities on chest X-ray after treatment [Figure 3a] Oocysts were no longer detected in stool and sputum.
Figure 1.
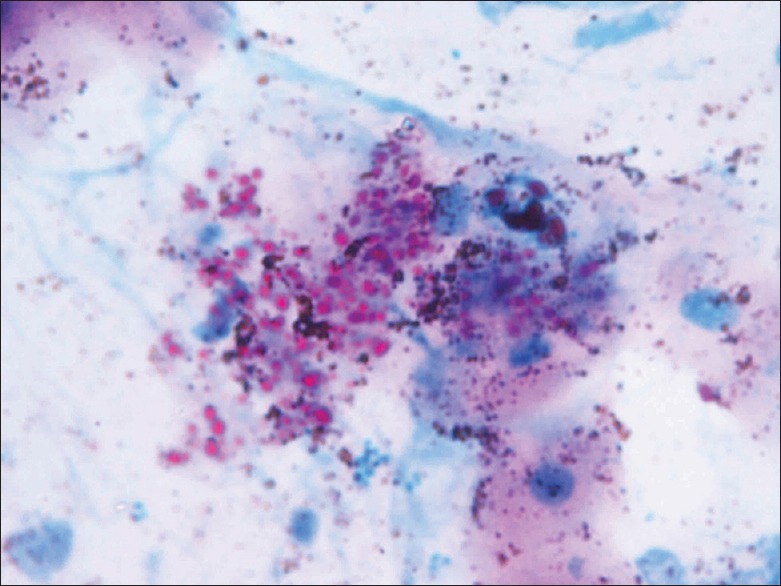
Cryptosporidium in sputum on modified ZN staining ×100
Figure 2.
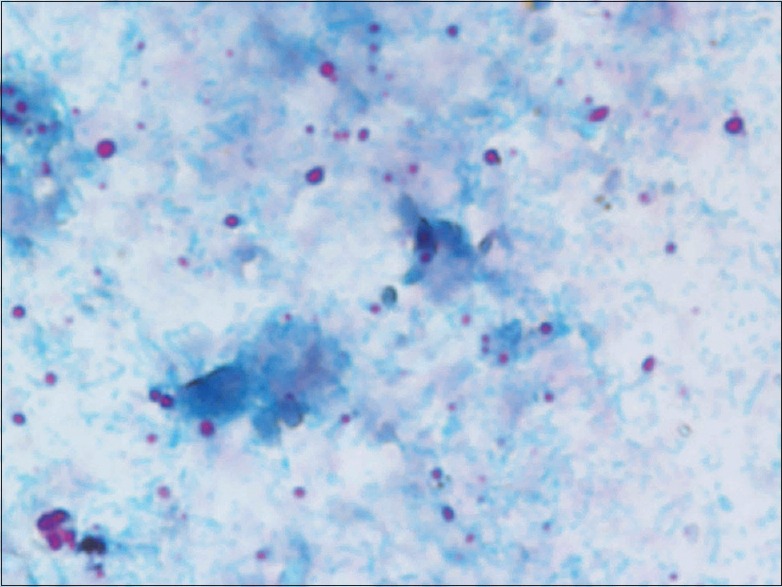
Cryptosporidium in stool on modified ZN staining
Figure 3.

(a) Chest X-ray showing consolidation patch on right lower zone before treatment (b) Complete resolution of opacities on chest X-ray after treatment with nitazoxanide
DISCUSSION
Transmission of Cryptosporidium occurs through the fecal/oral route after the ingestion of occysts (Infective stage of C. parvum). Ingestion can occur via person-to-person, zoonotic, waterborne, food-borne and airborne contact.[5] Cryptosporidium usually infect small gastrointestinal tract epithelium, multiplies within the macrophages and causes diarrheal diseases. Theses spores can migrate to the whole gastrointestinal tract, respiratory epithelium, and biliary tract. Severity of diseases depends on the immunity of the patients. In immunocompetent individuals rapid clearance of the organism is responsible for asymptomatic and self-limiting disease.[6] Immunocompromised individuals are prone for severe and fatal disease. Extra-intestinal manifestations are also common in these individuals. Most common extra-intestinal manifestations are bile tract infections which can lead to acalculous cholecystitis or papillary stenosis and pancreatitis. Lung infections and middle ear infections were also found.[4,7] A case of pulmonary cryptosporidiosis in a HIV-negative immunocompetent child who was receiving corticosteroids has been reported.[8]
The pulmonary cryptosporidiosis rarely reported and commonly associated with diarrhea. The pathogenesis of lung disease is not fully understood.[9] The lung diseases can occur due to the inhalation of spores or migration of oocysts from gastrointestinal tract through circulating phagocytes. The common presenting symptoms of pulmonary cryptosporidiosis are non-specific and typically include chronic cough, fever, and dyspnea. Radiological changes may or may not occur.[9,10]
Our patient presented because of fever, cough and breathlessness and had diarrhea after 5 days. He was a farmer. Thus we assumed that inhalation of spore or ingestion of contaminated food or water might be the route of transmission of cryptosporidium. There is a possibility of hematogenous spread of transmission of oocysts through circulating phagocytes to the gastrointestinal tract, other than ingestion of contaminated food or water for intestinal symptoms. He was treated successfully with nitazoxanide and loperamide and he became asymptomatic with normal chest X-ray and no evidence of oocysts on the sputum and stool staining after 5 days of treatment. Proceeding of respiratory symptoms to diarrhea after cryptosporidium infection in an immunocompetent host along with lung consolidation and good response to nitazoxanide makes this case rarer.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cama VA, Bern C, Roberts J, Cabrera L, Sterling CR, Ortega Y, et al. Cryptosporidium species and subtypes and clinical manifestations in children, Peru. Emerg Infect Dis. 2008;14:1567–74. doi: 10.3201/eid1410.071273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clavel A, Arnal AC, Sánchez EC, Cuesta J, Letona S, Amiguet JA, et al. Respiratory cryptosporidiosis: Case series and review of the literature. Infection. 1996;24:341–6. doi: 10.1007/BF01716076. [DOI] [PubMed] [Google Scholar]
- 3.Brea Hernando AJ, Bandrés Franco E, Mosquera Lozano JD, Lantero Benedito M, Ezquerra Lezcano M. Pulmonary cryptosporidiosis and AIDS: Presentation of a case and review of the literature. Ann Med Intern. 1993;10:232–6. [PubMed] [Google Scholar]
- 4.Chen XM, Keithly JS, Paya CV, LaRusso NF. Cryptosporodiosis. N Engl J Med. 2002;346:1723–31. doi: 10.1056/NEJMra013170. [DOI] [PubMed] [Google Scholar]
- 5.Thompson RC, Olson ME, Zhu G, Enomoto S, Abrahamsen MS, Hijjawi NS. Cryptosporidium and cryptosporidiosis. Adv Parasitol. 2005;59:77–158. doi: 10.1016/S0065-308X(05)59002-X. [DOI] [PubMed] [Google Scholar]
- 6.Wolska-Kusnierz B, Bajer A, Caccio S, Heropolitanska-Pliszka E, Bernatowska E, Socha P, et al. Cryptosporidium infection in patients with primary immunodeficiencies. J Pediatr Gastroenterol Nutr. 2007;45:458–64. doi: 10.1097/MPG.0b013e318054b09b. [DOI] [PubMed] [Google Scholar]
- 7.Clark DP. New insights into human cryptosporidiosis. Clin Microbiol Rev. 1999;12:554–63. doi: 10.1128/cmr.12.4.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shrikhande SN, Chande CA, Shegokar VR, Powar RM. Pulmonary cryptosporidiosis in HIV negative, immunocompromised host. Indian J Pathol Microbiol. 2009;52:267–8. doi: 10.4103/0377-4929.48942. [DOI] [PubMed] [Google Scholar]
- 9.Corti M, Villafañe MF, Muzzio E, Bava J, Abuín JC, Palmieri OJ. Pulmonary cryptosporidiosis in AIDS patients. Rev Argent Microbiol. 2008;40:106–8. [PubMed] [Google Scholar]
- 10.Dupont C, Bougnoux ME, Turner L, Rouveix E, Dorra M. Microbiological findings about pulmonary cryptosporidiosis in two AIDS patients. J Clin Microbiol. 1996;34:227–9. doi: 10.1128/jcm.34.1.227-229.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]


